Circulating Tumor Cell Detection during Neoadjuvant Chemotherapy to Predict Early Response in Locally Advanced Oropharyngeal Cancers: A Prospective Pilot Study
Abstract
1. Introduction
2. Materials and Methods
3. Results
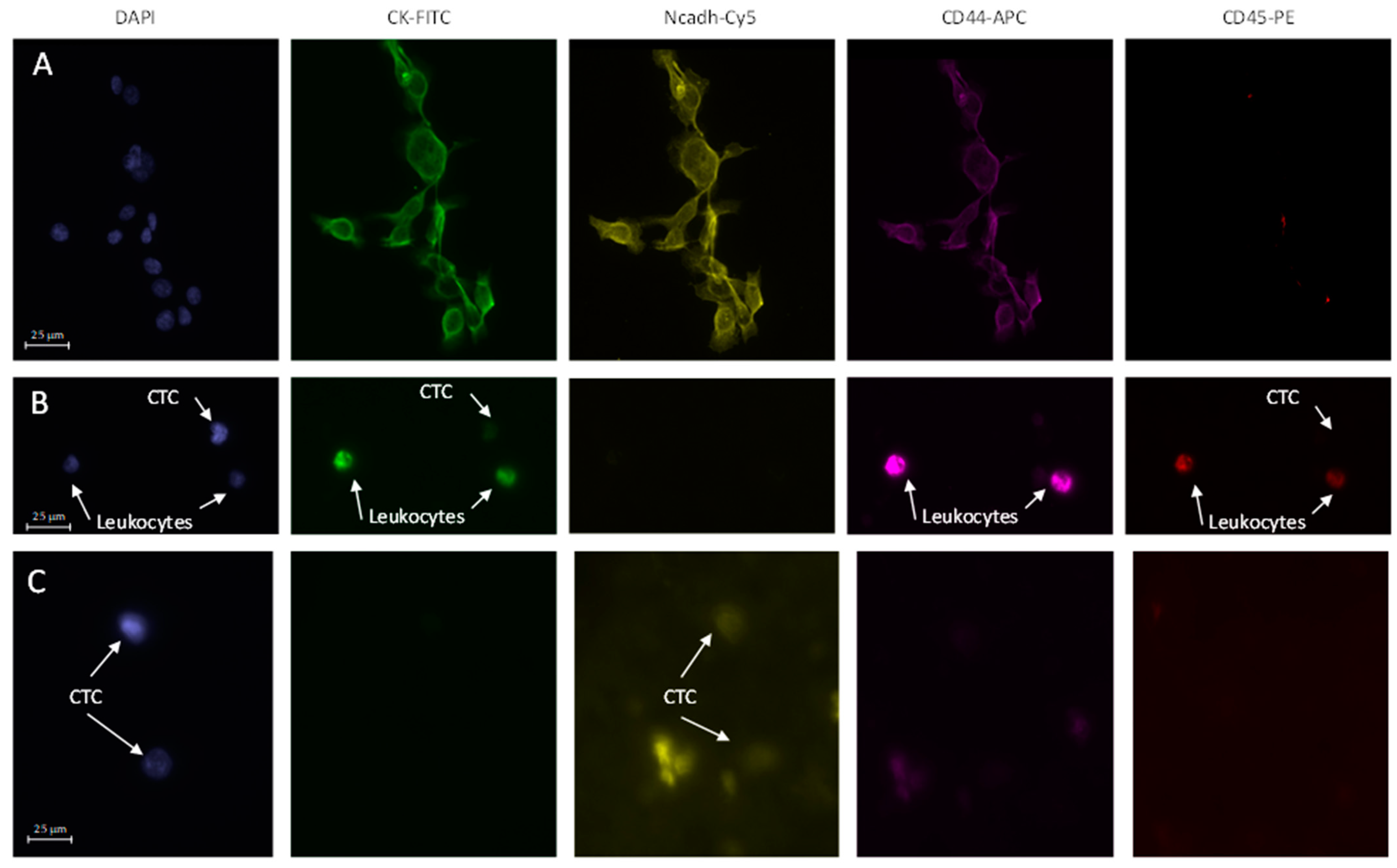
3.1. Counting and Characterization of CTCs
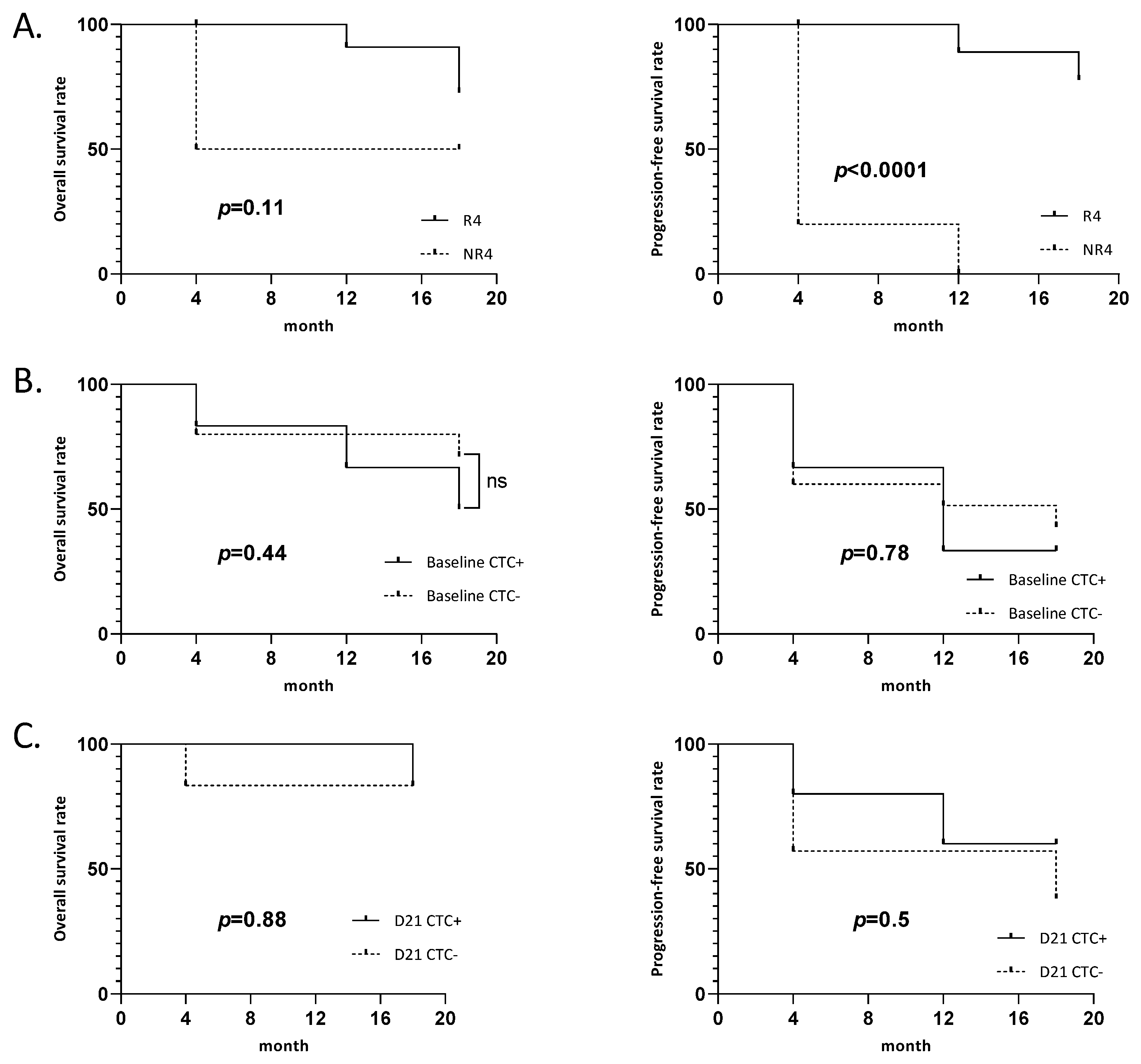
3.2. Association between the Presence of CTCs at Baseline or Day21 and the Survival Rate
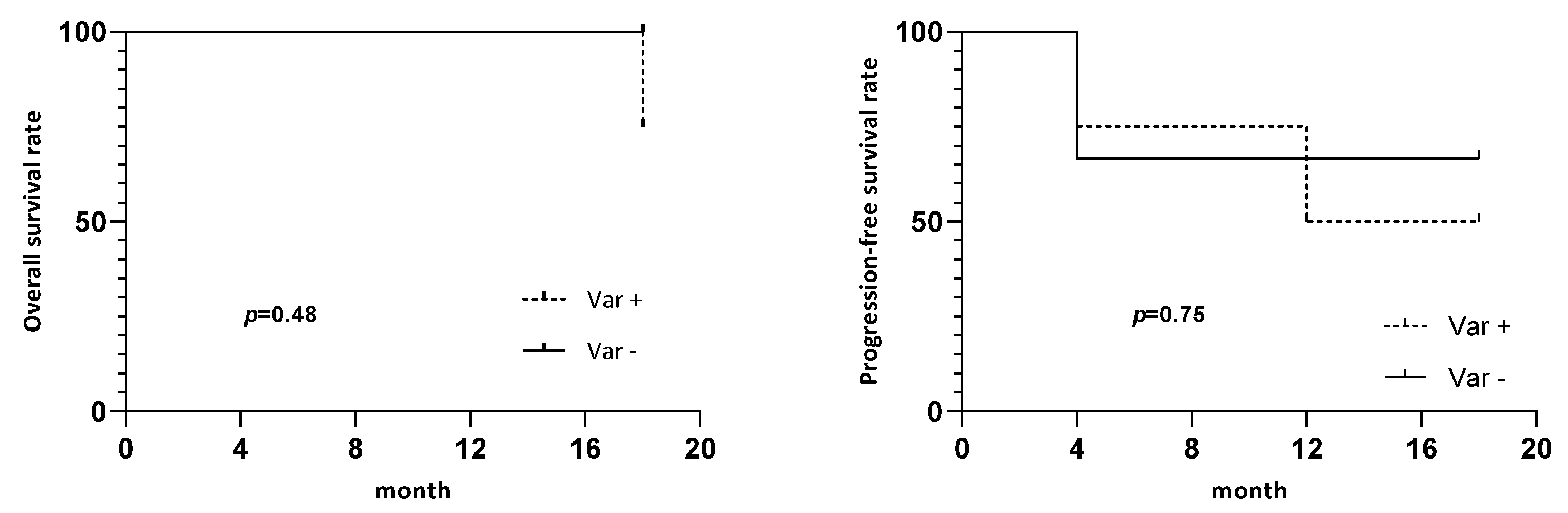
3.3. Variation in the Number of CTCs between Baseline and D21 and the Survival Rate
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ferlay, J.; Soerjomataram, I.; Dikshit, R.; Eser, S.; Mathers, C.; Rebelo, M.; Parkin, D.M.; Forman, D.; Bray, F. Cancer incidence and mortality worldwide: Sources, methods and major patterns in GLOBOCAN 2012. Int. J. Cancer 2015, 136, E359–E386. [Google Scholar] [CrossRef] [PubMed]
- Takes, R.P.; Rinaldo, A.; Silver, C.E.; Haigentz, M.; Woolgar, J.A.; Triantafyllou, A.; Mondin, V.; Paccagnella, D.; de Bree, R.; Shaha, A.R.; et al. Distant metastases from head and neck squamous cell carcinoma. Part I. Basic aspects. Oral Oncol. 2012, 48, 775–779. [Google Scholar] [CrossRef] [PubMed]
- Routray, S.; Mohanty, N. Cancer stem cells accountability in progression of head and neck squamous cell carcinoma: The most recent trends! Mol. Biol. Int. 2014, 2014, 375325. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Yoshida, G.J.; Saya, H. Molecular pathology underlying the robustness of cancer stem cells. Regen. Ther. 2021, 17, 38–50. [Google Scholar] [CrossRef] [PubMed]
- Lianidou, E.S.; Markou, A.; Strati, A. The Role of CTCs as Tumor Biomarkers. Adv. Exp. Med. Biol. 2015, 867, 341–367. [Google Scholar] [CrossRef]
- Galletti, G.; Portella, L.; Tagawa, S.T.; Kirby, B.J.; Giannakakou, P.; Nanus, D.M. Circulating tumor cells in prostate cancer diagnosis and monitoring: An appraisal of clinical potential. Mol. Diagn. Ther. 2014, 18, 389–402. [Google Scholar] [CrossRef]
- Giordano, A.; Egleston, B.L.; Hajage, D.; Bland, J.; Hortobagyi, G.N.; Reuben, J.M.; Pierga, J.-Y.; Cristofanilli, M.; Bidard, F.-C. Establishment and validation of circulating tumor cell-based prognostic nomograms in first-line metastatic breast cancer patients. Clin. Cancer Res. 2013, 19, 1596–1602. [Google Scholar] [CrossRef]
- Tsai, W.-S.; Chen, J.-S.; Shao, H.-J.; Wu, J.-C.; Lai, J.-M.; Lu, S.-H.; Hung, T.-F.; Chiu, Y.-C.; You, J.-F.; Hsieh, P.-S.; et al. Circulating Tumor Cell Count Correlates with Colorectal Neoplasm Progression and Is a Prognostic Marker for Distant Metastasis in Non-Metastatic Patients. Sci. Rep. 2016, 6, 24517. [Google Scholar] [CrossRef]
- Zou, K.; Yang, S.; Zheng, L.; Wang, S.; Xiong, B. Prognostic Role of the Circulating Tumor Cells Detected by Cytological Methods in Gastric Cancer: A Meta-Analysis. Biomed. Res. Int. 2016, 2016, 2765464. [Google Scholar] [CrossRef]
- Bozec, A.; Ilie, M.; Dassonville, O.; Long, E.; Poissonnet, G.; Santini, J.; Chamorey, E.; Ettaiche, M.; Chauvière, D.; Peyrade, F.; et al. Significance of circulating tumor cell detection using the CellSearch system in patients with locally advanced head and neck squamous cell carcinoma. Eur. Arch. Oto-Rhino-Laryngol. 2013, 270, 2745–2749. [Google Scholar] [CrossRef]
- Grisanti, S.; Almici, C.; Consoli, F.; Buglione, M.; Verardi, R.; Bolzoni-Villaret, A.; Bianchetti, A.; Ciccarese, C.; Mangoni, M.; Ferrari, L.; et al. Circulating tumor cells in patients with recurrent or metastatic head and neck carcinoma: Prognostic and predictive significance. PLoS ONE 2014, 9, e103918. [Google Scholar] [CrossRef] [PubMed]
- Inhestern, J.; Oertel, K.; Stemmann, V.; Schmalenberg, H.; Dietz, A.; Rotter, N.; Veit, J.; Görner, M.; Sudhoff, H.; Junghanß, C.; et al. Prognostic Role of Circulating Tumor Cells during Induction Chemotherapy Followed by Curative Surgery Combined with Postoperative Radiotherapy in Patients with Locally Advanced Oral and Oropharyngeal Squamous Cell Cancer. PLoS ONE 2015, 10, e0132901. [Google Scholar] [CrossRef] [PubMed]
- Jatana, K.R.; Balasubramanian, P.; Lang, J.C.; Yang, L.; Jatana, C.A.; White, E.; Agrawal, A.; Ozer, E.; Schuller, D.E.; Teknos, T.N.; et al. Significance of circulating tumor cells in patients with squamous cell carcinoma of the head and neck: Initial results. Arch. Otolaryngol. Head Neck Surg. 2010, 136, 1274–1279. [Google Scholar] [CrossRef]
- Winter, S.C.; Stephenson, S.-A.; Subramaniam, S.K.; Paleri, V.; Ha, K.; Marnane, C.; Krishnan, S.; Rees, G. Long term survival following the detection of circulating tumour cells in head and neck squamous cell carcinoma. BMC Cancer 2009, 9, 424. [Google Scholar] [CrossRef] [PubMed]
- Tang, K.D.; Vasani, S.; Taheri, T.; Walsh, L.J.; Hughes, B.G.M.; Kenny, L.; Punyadeera, C. An Occult HPV-Driven Oropharyngeal Squamous Cell Carcinoma Discovered Through a Saliva Test. Front. Oncol. 2020, 10, 408. [Google Scholar] [CrossRef] [PubMed]
- Ekanayake Weeramange, C.; Liu, Z.; Hartel, G.; Li, Y.; Vasani, S.; Langton-Lockton, J.; Kenny, L.; Morris, L.; Frazer, I.; Tang, K.D.; et al. Salivary High-Risk Human Papillomavirus (HPV) DNA as a Biomarker for HPV-Driven Head and Neck Cancers. J. Mol. Diagn. 2021, 23, 1334–1342. [Google Scholar] [CrossRef] [PubMed]
- Hodgkinson, C.L.; Morrow, C.J.; Li, Y.; Metcalf, R.L.; Rothwell, D.G.; Trapani, F.; Polanski, R.; Burt, D.J.; Simpson, K.L.; Morris, K.; et al. Tumorigenicity and genetic profiling of circulating tumor cells in small-cell lung cancer. Nat. Med. 2014, 20, 897–903. [Google Scholar] [CrossRef]
- Moncharmont, C.; Guy, J.-B.; Wozny, A.-S.; Gilormini, M.; Battiston-Montagne, P.; Ardail, D.; Beuve, M.; Alphonse, G.; Simoëns, X.; Rancoule, C.; et al. Carbon ion irradiation withstands cancer stem cells’ migration/invasion process in Head and Neck Squamous Cell Carcinoma (HNSCC). Oncotarget 2016, 7, 47738–47749. [Google Scholar] [CrossRef]
- Kulasinghe, A.; Zhou, J.; Kenny, L.; Papautsky, I.; Punyadeera, C. Capture of Circulating Tumour Cell Clusters Using Straight Microfluidic Chips. Cancers 2019, 11, 89. [Google Scholar] [CrossRef]
- Kulasinghe, A.; Schmidt, H.; Perry, C.; Whitfield, B.; Kenny, L.; Nelson, C.; Warkiani, M.E.; Punyadeera, C. A Collective Route to Head and Neck Cancer Metastasis. Sci. Rep. 2018, 8, 746. [Google Scholar] [CrossRef]
- Moussavi-Harami, S.F.; Wisinski, K.B.; Beebe, D.J. Circulating Tumor Cells in Metastatic Breast Cancer: A Prognostic and Predictive Marker. J. Patient Cent. Res. Rev. 2014, 1, 85–92. [Google Scholar] [CrossRef] [PubMed]
- Kapeleris, J.; Kulasinghe, A.; Warkiani, M.E.; Vela, I.; Kenny, L.; O’Byrne, K.; Punyadeera, C. The Prognostic Role of Circulating Tumor Cells (CTCs) in Lung Cancer. Front. Oncol. 2018, 8, 311. [Google Scholar] [CrossRef] [PubMed]
- Poveda, A.; Kaye, S.B.; McCormack, R.; Wang, S.; Parekh, T.; Ricci, D.; Lebedinsky, C.A.; Tercero, J.C.; Zintl, P.; Monk, B.J. Circulating tumor cells predict progression free survival and overall survival in patients with relapsed/recurrent advanced ovarian cancer. Gynecol. Oncol. 2011, 122, 567–572. [Google Scholar] [CrossRef]
- Zhang, X.; Li, H.; Yu, X.; Li, S.; Lei, Z.; Li, C.; Zhang, Q.; Han, Q.; Li, Y.; Zhang, K.; et al. Analysis of Circulating Tumor Cells in Ovarian Cancer and Their Clinical Value as a Biomarker. Cell Physiol. Biochem. 2018, 48, 1983–1994. [Google Scholar] [CrossRef] [PubMed]
- Buglione, M.; Grisanti, S.; Almici, C.; Mangoni, M.; Polli, C.; Consoli, F.; Verardi, R.; Costa, L.; Paiar, F.; Pasinetti, N.; et al. Circulating Tumour Cells in locally advanced head and neck cancer: Preliminary report about their possible role in predicting response to non-surgical treatment and survival. Eur. J. Cancer 2012, 48, 3019–3026. [Google Scholar] [CrossRef] [PubMed]
- Balasubramanian, P.; Lang, J.C.; Jatana, K.R.; Miller, B.; Ozer, E.; Old, M.; Schuller, D.E.; Agrawal, A.; Teknos, T.N.; Summers, T.A.; et al. Multiparameter analysis, including EMT markers, on negatively enriched blood samples from patients with squamous cell carcinoma of the head and neck. PLoS ONE 2012, 7, e42048. [Google Scholar] [CrossRef] [PubMed]
- Kulasinghe, A.; Hughes, B.G.M.; Kenny, L.; Punyadeera, C. An update: Circulating tumor cells in head and neck cancer. Expert Rev. Mol. Diagn. 2019, 19, 1109–1115. [Google Scholar] [CrossRef] [PubMed]
- Kulasinghe, A.; Kenny, L.; Perry, C.; Thiery, J.-P.; Jovanovic, L.; Vela, I.; Nelson, C.; Punyadeera, C. Impact of label-free technologies in head and neck cancer circulating tumour cells. Oncotarget 2016, 7, 71223–71234. [Google Scholar] [CrossRef]
- Garrel, R.; Mazel, M.; Perriard, F.; Vinches, M.; Cayrefourcq, L.; Guigay, J.; Digue, L.; Aubry, K.; Alfonsi, M.; Delord, J.-P.; et al. Circulating Tumor Cells as a Prognostic Factor in Recurrent or Metastatic Head and Neck Squamous Cell Carcinoma: The CIRCUTEC Prospective Study. Clin. Chem. 2019, 65, 1267–1275. [Google Scholar] [CrossRef]
- Wang, H.-M.; Wu, M.-H.; Chang, P.-H.; Lin, H.-C.; Liao, C.-D.; Wu, S.-M.; Hung, T.-M.; Lin, C.-Y.; Chang, T.-C.; Tzu-Tsen, Y.; et al. The change in circulating tumor cells before and during concurrent chemoradiotherapy is associated with survival in patients with locally advanced head and neck cancer. Head Neck 2019, 41, 2676–2687. [Google Scholar] [CrossRef]
| Patients’ Characteristics | Number of Patients | n CTC+ at Baseline | p-Value |
|---|---|---|---|
| Age (years) | |||
| <65 | 16 (76.2%) | 5 | 1 |
| >65 | 5 (23.8%) | 1 | |
| Gender | |||
| Male | 18 (85.7%) | 5 | 1 |
| Female | 3 (14.3%) | 1 | |
| T stage | |||
| T2 | 2 (9.5%) | 0 | 0.57 |
| T3 | 8 (38.1%) | 3 | |
| T4 | 11 (52.4%) | 3 | |
| N stage | |||
| N0 | 3 (14.3%) | 2 | 0.18 |
| N+ | 18 (85.7%) | 4 | |
| Tobacco | |||
| Exposed | 19 (90.5%) | 6 | 1 |
| None | 2 (9.5%) | 0 | |
| Alcohol | |||
| Exposed | 7 (33.3%) | 3 | 0.29 |
| None | 14 (61.9%) | 3 | |
| HPV status | |||
| Positive | 5 (23.8%) | 0 | |
| Negative | 13 (61.9%) | 4 | 0.12 |
| Unknown | 3 (14.3%) | 2 |
| Patients | Baseline (Number of Cells) | Day 21 (Number of Cells) | Variation | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Epithelial | Mesenchymal | Stem Cell | Undefined | CTC/ mL | Epithelial | Mesenchymal | Stem Cell | Undefined | CTC/ mL | |||
| DCF | #1 | 0 | 1 | 0 | 2 | 0.315 | 0 | 0 | 0 | 0 | 0 | - |
| #2 | 0 | 1 | 0 | 2 | 0.255 | 1 | 1 | 0 | 20 * | 1.505 | + | |
| #3 | 0 | 0 | 0 | 1 | 0.190 | 0 | 0 | 0 | 6 | 0.315 | + | |
| #4 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | = | |
| #5 | 0 | 0 | 0 | 0 | 0 | 0 | 3 | 1 | 15 | 1.190 | + | |
| #6 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | = | |
| #7 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | = | |
| #14° | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 38 * | 2.375 | + | |
| #15° | 0 | 0 | 0 | 3 | 0.880 | 0 | 0 | 0 | 1 | 0.055 | - | |
| #16° | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | = | |
| #17° | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | = | |
| #18° | 0 | 0 | 0 | 0 | 0 | / | / | / | / | / | NA | |
| mDCF | #8 | 0 | 0 | 0 | 0 | 0 | / | / | / | / | / | NA |
| #9 | 0 | 0 | 0 | 0 | 0 | / | / | / | / | / | NA | |
| #10 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | = | |
| #11 | 0 | 0 | 0 | 0 | 0 | / | / | / | / | / | NA | |
| #12 | 1 | 0 | 0 | 1 | 0.125 | / | / | / | / | / | NA | |
| #13 | 0 | 0 | 0 | 0 | 0 | / | / | / | / | / | NA | |
| #19° | 0 | 0 | 0 | 0 | 0 | / | / | / | / | / | NA | |
| #20° | 1 | 1 | 0 | 8 | 3.335 | / | / | / | / | / | NA | |
| #21° | 0 | 0 | 0 | 0 | 0 | / | / | / | / | / | NA | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gauthier, A.; Philouze, P.; Lauret, A.; Alphonse, G.; Malesys, C.; Ardail, D.; Payen, L.; Céruse, P.; Wozny, A.-S.; Rodriguez-Lafrasse, C. Circulating Tumor Cell Detection during Neoadjuvant Chemotherapy to Predict Early Response in Locally Advanced Oropharyngeal Cancers: A Prospective Pilot Study. J. Pers. Med. 2022, 12, 445. https://doi.org/10.3390/jpm12030445
Gauthier A, Philouze P, Lauret A, Alphonse G, Malesys C, Ardail D, Payen L, Céruse P, Wozny A-S, Rodriguez-Lafrasse C. Circulating Tumor Cell Detection during Neoadjuvant Chemotherapy to Predict Early Response in Locally Advanced Oropharyngeal Cancers: A Prospective Pilot Study. Journal of Personalized Medicine. 2022; 12(3):445. https://doi.org/10.3390/jpm12030445
Chicago/Turabian StyleGauthier, Arnaud, Pierre Philouze, Alexandra Lauret, Gersende Alphonse, Céline Malesys, Dominique Ardail, Léa Payen, Philippe Céruse, Anne-Sophie Wozny, and Claire Rodriguez-Lafrasse. 2022. "Circulating Tumor Cell Detection during Neoadjuvant Chemotherapy to Predict Early Response in Locally Advanced Oropharyngeal Cancers: A Prospective Pilot Study" Journal of Personalized Medicine 12, no. 3: 445. https://doi.org/10.3390/jpm12030445
APA StyleGauthier, A., Philouze, P., Lauret, A., Alphonse, G., Malesys, C., Ardail, D., Payen, L., Céruse, P., Wozny, A.-S., & Rodriguez-Lafrasse, C. (2022). Circulating Tumor Cell Detection during Neoadjuvant Chemotherapy to Predict Early Response in Locally Advanced Oropharyngeal Cancers: A Prospective Pilot Study. Journal of Personalized Medicine, 12(3), 445. https://doi.org/10.3390/jpm12030445






