Real-World Impact of a Pharmacogenomics-Enriched Comprehensive Medication Management Program
Abstract
:1. Introduction
2. Methods
2.1. Program Description
2.2. Genetic Testing
2.3. Medication Action Plan
2.4. Evaluation of the Program
2.5. Economic Data Analysis
3. Results
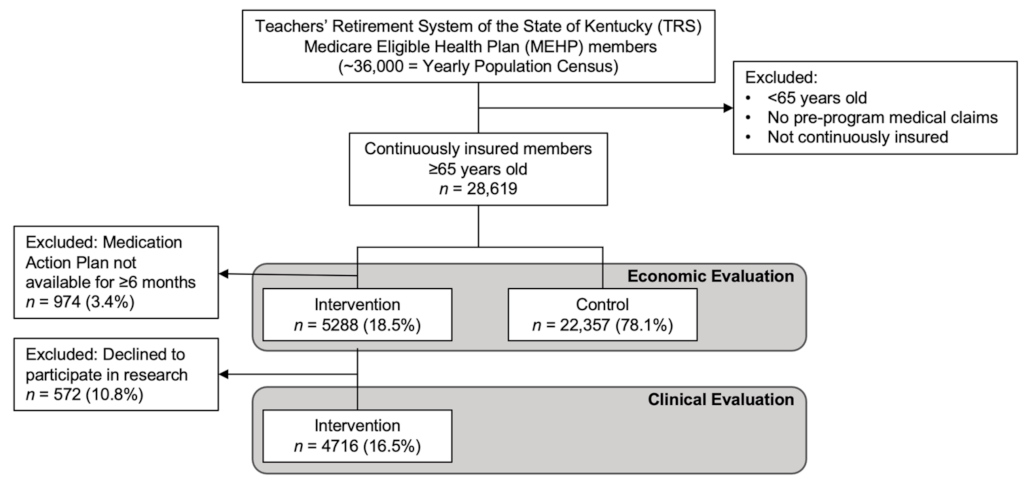
3.1. Retrospective Study: Intervention and Control Assignments
3.2. Demographic Data
3.3. Medication Action Plan
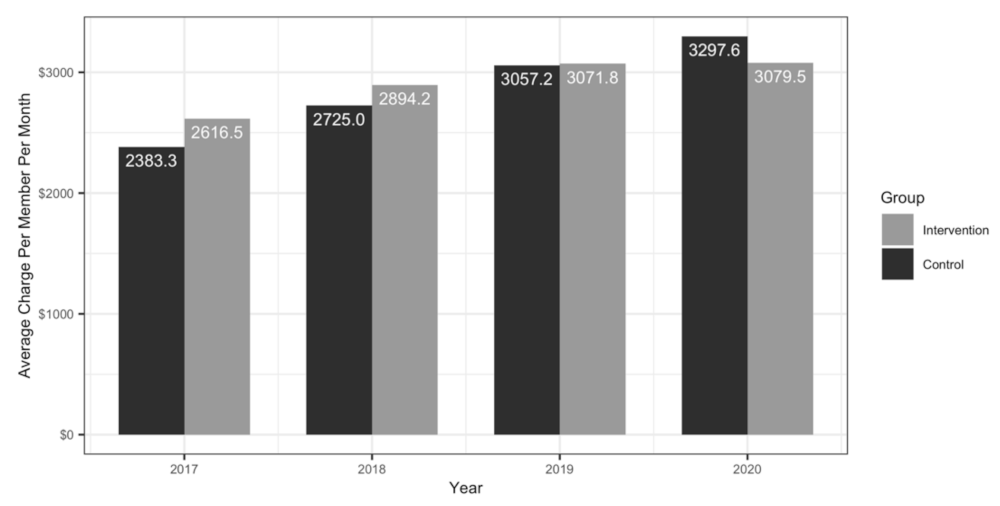
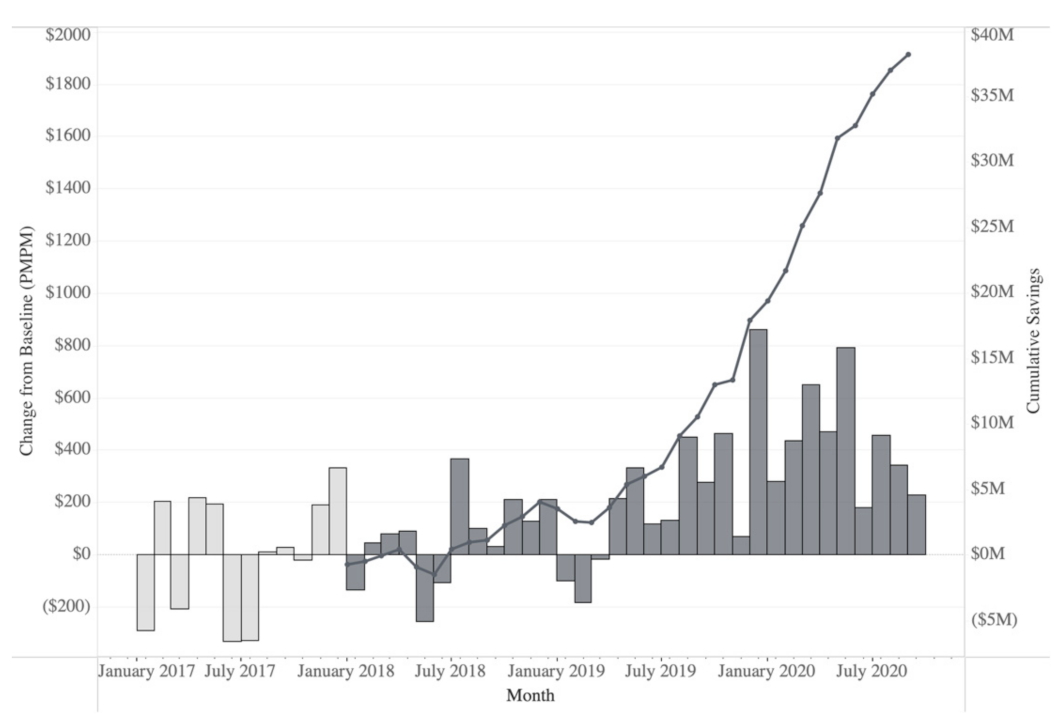
3.4. Economic Outcomes
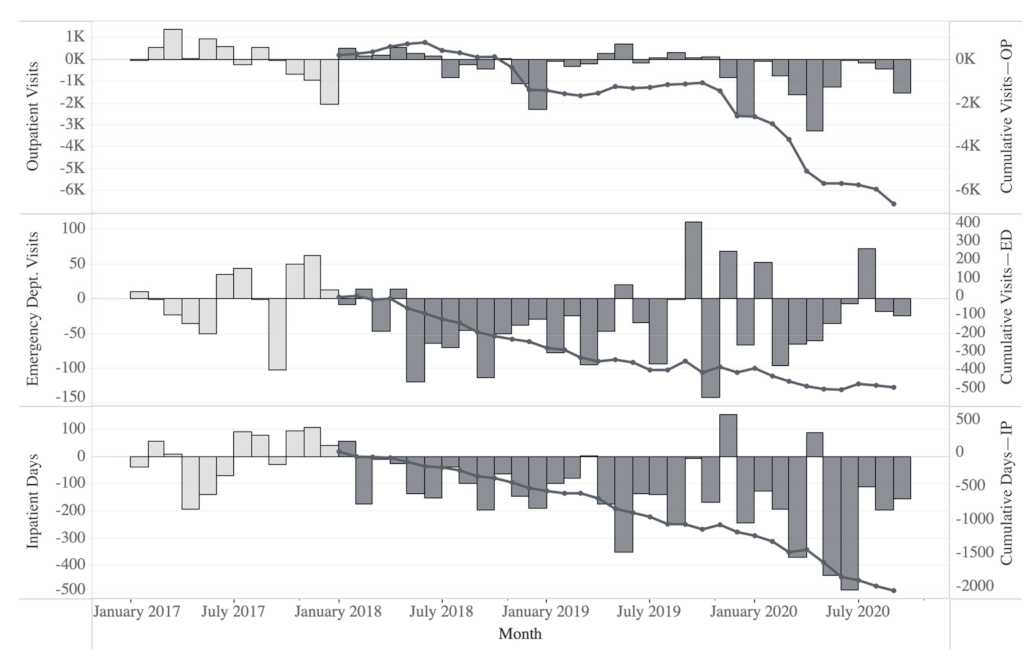
3.5. Healthcare Resource Utilization
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- U.S. Food and Drug Administration (FDA). Table of Pharmacogenomic Biomarkers in Drug Labeling. Available online: https://www.fda.gov/drugs/science-and-research-drugs/table-pharmacogenomic-biomarkers-drug-labeling (accessed on 11 November 2021).
- Roden, D.M.; McLeod, H.L.; Relling, M.V.; Williams, M.S.; Mensah, G.A.; Peterson, J.F.; Van Driest, S.L. Pharmacogenomics. Lancet 2019, 394, 521–532. [Google Scholar] [CrossRef]
- Meaddough, E.L.; Sarasua, S.M.; Fasolino, T.K.; Farrell, C.L. The impact of pharmacogenetic testing in patients exposed to polypharmacy: A scoping review. Pharmacogenom. J. 2021, 21, 409–422. [Google Scholar] [CrossRef] [PubMed]
- Orlando, L.A.; Voils, C.; Horowitz, C.R.; Myers, R.A.; Arwood, M.J.; Cicali, E.J.; McDonough, C.W.; Pollin, T.I.; Guan, Y.; Levy, K.D.; et al. IGNITE network: Response of patients to genomic medicine interventions. Mol. Genet. Genom. Med. 2019, 7, e636. [Google Scholar] [CrossRef]
- Aboelbaha, S.; Zolezzi, M.; Elewa, H. Effect of Pharmacogenetic-Based Decision Support Tools in Improving Depression Outcomes: A Systematic Review. Neuropsychiatr. Dis. Treat. 2021, 17, 2397–2419. [Google Scholar] [CrossRef] [PubMed]
- Haga, S.B.; Mills, R.; Moaddeb, J.; Liu, Y.; Voora, D. Independent Community Pharmacists’ Experience in Offering Pharmacogenetic Testing. Pharmgenom. Pers. Med. 2021, 14, 877–886. [Google Scholar] [CrossRef] [PubMed]
- Hayashi, M.; Hamdy, D.A.; Mahmoud, S.H. Applications for pharmacogenomics in pharmacy practice: A scoping review. Res. Soc. Adm. Pharm. 2021, in press. [Google Scholar] [CrossRef] [PubMed]
- David, V.; Fylan, B.; Bryant, E.; Smith, H.; Sagoo, G.S.; Rattray, M. An Analysis of Pharmacogenomic-Guided Pathways and Their Effect on Medication Changes and Hospital Admissions: A Systematic Review and Meta-Analysis. Front. Genet. 2021, 12, 698148. [Google Scholar] [CrossRef]
- Berm, E.J.; Looff, M.; Wilffert, B.; Boersma, C.; Annemans, L.; Vegter, S.; Boven, J.F.; Postma, M.J. Economic Evaluations of Pharmacogenetic and Pharmacogenomic Screening Tests: A Systematic Review. Second Update of the Literature. PLoS ONE 2016, 11, e0146262. [Google Scholar] [CrossRef]
- Miteva-Marcheva, N.N.; Ivanov, H.Y.; Dimitrov, D.K.; Stoyanova, V.K. Application of pharmacogenetics in oncology. Biomark. Res. 2020, 8, 32. [Google Scholar] [CrossRef]
- Fragoulakis, V.; Roncato, R.; Fratte, C.D.; Ecca, F.; Bartsakoulia, M.; Innocenti, F.; Toffoli, G.; Cecchin, E.; Patrinos, G.P.; Mitropoulou, C. Estimating the Effectiveness of DPYD Genotyping in Italian Individuals Suffering from Cancer Based on the Cost of Chemotherapy-Induced Toxicity. Am. J. Hum. Genet. 2019, 104, 1158–1168. [Google Scholar] [CrossRef] [Green Version]
- Bousman, C.A.; Arandjelovic, K.; Mancuso, S.G.; Eyre, H.A.; Dunlop, B.W. Pharmacogenetic tests and depressive symptom remission: A meta-analysis of randomized controlled trials. Pharmacogenomics 2019, 20, 37–47. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van Schaik, R.H.N.; Muller, D.J.; Serretti, A.; Ingelman-Sundberg, M. Pharmacogenetics in Psychiatry: An Update on Clinical Usability. Front. Pharmacol. 2020, 11, 575540. [Google Scholar] [CrossRef]
- Tanner, J.A.; Davies, P.E.; Overall, C.C.; Grima, D.; Nam, J.; Dechairo, B.M. Cost-effectiveness of combinatorial pharmacogenomic testing for depression from the Canadian public payer perspective. Pharmacogenomics 2020, 21, 521–531. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jarvis, J.P.; Peter, A.P.; Shaman, J.A. Consequences of CYP2D6 Copy-Number Variation for Pharmacogenomics in Psychiatry. Front. Psychiatry 2019, 10, 432. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Islam, F.; Men, X.; Yoshida, K.; Zai, C.C.; Muller, D.J. Pharmacogenetics-Guided Advances in Antipsychotic Treatment. Clin. Pharmacol. Ther. 2021, 110, 582–588. [Google Scholar] [CrossRef]
- Brown, L.C.; Lorenz, R.A.; Li, J.; Dechairo, B.M. Economic Utility: Combinatorial Pharmacogenomics and Medication Cost Savings for Mental Health Care in a Primary Care Setting. Clin. Ther. 2017, 39, 592–602.e1. [Google Scholar] [CrossRef] [Green Version]
- Perlis, R.H.; Mehta, R.; Edwards, A.M.; Tiwari, A.; Imbens, G.W. Pharmacogenetic testing among patients with mood and anxiety disorders is associated with decreased utilization and cost: A propensity-score matched study. Depress. Anxiety 2018, 35, 946–952. [Google Scholar] [CrossRef]
- Carrascal-Laso, L.; Franco-Martin, M.A.; Marcos-Vadillo, E.; Ramos-Gallego, I.; Garcia-Berrocal, B.; Mayor-Toranzo, E.; Sanchez-Iglesias, S.; Lorenzo, C.; Sevillano-Jimenez, A.; Sanchez-Martin, A.; et al. Economic Impact of the Application of a Precision Medicine Model (5SPM) on Psychotic Patients. Pharmgenom. Pers. Med. 2021, 14, 1015–1025. [Google Scholar] [CrossRef]
- Chang, W.C.; Tanoshima, R.; Ross, C.J.D.; Carleton, B.C. Challenges and Opportunities in Implementing Pharmacogenetic Testing in Clinical Settings. Annu. Rev. Pharmacol. Toxicol. 2021, 61, 65–84. [Google Scholar] [CrossRef]
- Chanfreau-Coffinier, C.; Hull, L.E.; Lynch, J.A.; DuVall, S.L.; Damrauer, S.M.; Cunningham, F.E.; Voight, B.F.; Matheny, M.E.; Oslin, D.W.; Icardi, M.S.; et al. Projected Prevalence of Actionable Pharmacogenetic Variants and Level A Drugs Prescribed Among US Veterans Health Administration Pharmacy Users. JAMA Netw. Open 2019, 2, e195345. [Google Scholar] [CrossRef]
- Eichmeyer, J.; Rogers, S.; Formea, C.M.; Giri, J.; Jones, J.S.; Schnettler, E.; Schmidlen, T.; Glogowski, E.; Kurz, R.N. PARC report: A perspective on the state of clinical pharmacogenomics testing. Pharmacogenomics 2020, 21, 809–820. [Google Scholar] [CrossRef] [PubMed]
- CMM in Primary Care Research Team. The Patient Care Process for Delivering Comprehensive Medication Management (CMM): Optimizing Medication Use in Patient-Centered, Team-Based Care Settings. Available online: http://www.accp.com/cmm_care_process (accessed on 11 November 2021).
- Patient-Centered Primary Care Collaborative. Integrating Comprehensive Medication Management to Optimize Patient Outcomes. Available online: www.pcpcc.org/sites/default/files/media/medmanagement.pdf (accessed on 11 November 2021).
- Santos, B.D.; Nascimento, M.; de Oliveira, G.C.B.; Nascimento, Y.A.; Mambrini, J.V.M.; Cid, A.S.; Piovesan, T.G.C.; Fernandes, L.B.; Martins, U.C.M.; Neves, C.M.; et al. Clinical Impact of a Comprehensive Medication Management Service in Primary Health Care. J. Pharm. Pract. 2021, 34, 265–271. [Google Scholar] [CrossRef] [PubMed]
- Tripicchio, K.; Urick, B.; Easter, J.; Ozawa, S. Making the economic value proposition for pharmacist comprehensive medication management (CMM) in primary care: A conceptual framework. Res. Soc. Adm. Pharm. 2020, 16, 1416–1421. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McFarland, M.S.; Buck, M.L.; Crannage, E.; Armistead, L.T.; Ourth, H.; Finks, S.W.; McClurg, M.R.; writing on behalf of the Get the Medications Right. Assessing the Impact of Comprehensive Medication Management on Achievement of the Quadruple. Aim. Am. J. Med. 2021, 134, 456–461. [Google Scholar] [CrossRef] [PubMed]
- Sutton, R.T.; Pincock, D.; Baumgart, D.C.; Sadowski, D.C.; Fedorak, R.N.; Kroeker, K.I. An overview of clinical decision support systems: Benefits, risks, and strategies for success. NPJ Digit. Med. 2020, 3, 17. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, K.; Magness, J.W.; Nelson, R.; Baron, V.; Brixner, D.I. Clinical Utility of Pharmacogenetic Testing and a Clinical Decision Support Tool to Enhance the Identification of Drug Therapy Problems through Medication Therapy Management in Polypharmacy Patients. J. Manag. Care Spec. Pharm. 2018, 24, 1250–1259. [Google Scholar] [CrossRef]
- Brown, J.T.; Bishop, J.R.; Schneiderhan, M.E. Using pharmacogenomics and therapeutic drug monitoring to guide drug selection and dosing in outpatient mental health comprehensive medication management. Ment. Health Clin. 2020, 10, 254–258. [Google Scholar] [CrossRef]
- Haidar, C.E.; Petry, N.; Oxencis, C.; Douglas, J.S.; Hoffman, J.M. ASHP Statement on the Pharmacist’s Role in Clinical Pharmacogenomics. Am. J. Health Syst. Pharm. 2021. [Google Scholar] [CrossRef]
- Empey, P.E.; Pratt, V.M.; Hoffman, J.M.; Caudle, K.E.; Klein, T.E. Expanding evidence leads to new pharmacogenomics payer coverage. Genet. Med. 2021, 23, 830–832. [Google Scholar] [CrossRef]
- Relling, M.V.; Klein, T.E. CPIC: Clinical Pharmacogenetics Implementation Consortium of the Pharmacogenomics Research Network. Clin. Pharmacol. Ther. 2011, 89, 464–467. [Google Scholar] [CrossRef]
- Gaedigk, A.; Ingelman-Sundberg, M.; Miller, N.A.; Leeder, J.S.; Whirl-Carrillo, M.; Klein, T.E. The Pharmacogene Variation (PharmVar) Consortium: Incorporation of the Human Cytochrome P450 (CYP) Allele Nomenclature Database. Clin. Pharmacol. Ther. 2018, 103, 399–401. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sherry, S.T.; Ward, M.; Sirotkin, K. dbSNP-database for single nucleotide polymorphisms and other classes of minor genetic variation. Genome Res. 1999, 9, 677–679. [Google Scholar] [CrossRef] [PubMed]
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C.R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef]
- Centers for Medicare & Medicaid Services. Place of Service Code Set. Available online: https://www.cms.gov/Medicare/Coding/place-of-service-codes/Place_of_Service_Code_Set (accessed on 21 September 2021).
- Kentucky Department of Education. Kentucky Education Facts. Available online: https://education.ky.gov/comm/edfacts/Pages/default.aspx (accessed on 12 January 2022).
- Kentucky Department of Education. Certification. Available online: https://education.ky.gov/teachers/NxGenProf/pages/certification.aspx (accessed on 12 January 2022).
- Gharani, N.; Keller, M.A.; Stack, C.B.; Hodges, L.M.; Schmidlen, T.J.; Lynch, D.E.; Gordon, E.S.; Christman, M.F. The Coriell personalized medicine collaborative pharmacogenomics appraisal, evidence scoring and interpretation system. Genome Med. 2013, 5, 93. [Google Scholar] [CrossRef] [Green Version]
- U.S. Food and Drug Administration (FDA). Table of Pharmacogenetic Associations. Available online: https://www.fda.gov/medical-devices/precision-medicine/table-pharmacogenetic-associations (accessed on 12 November 2021).
- Zajic, S.C.; Jarvis, J.P.; Zhang, P.; Rajula, K.D.; Brangan, A.; Brenner, R.; Dempsey, M.P.; Christman, M.F. Individuals with CYP2C8 and CYP2C9 reduced metabolism haplotypes self-adjusted ibuprofen dose in the Coriell Personalized Medicine Collaborative. Pharmacogenet. Genom. 2019, 29, 49–57. [Google Scholar] [CrossRef]
- Theken, K.N.; Lee, C.R.; Gong, L.; Caudle, K.E.; Formea, C.M.; Gaedigk, A.; Klein, T.E.; Agundez, J.A.G.; Grosser, T. Clinical Pharmacogenetics Implementation Consortium (CPIC) Guideline for CYP2C9 and Nonsteroidal Anti-inflammatory Drugs. Clin. Pharmacol. Ther. 2020, 108, 191–200. [Google Scholar] [CrossRef]
- Lima, J.J.; Thomas, C.D.; Barbarino, J.; Desta, Z.; Van Driest, S.L.; El Rouby, N.; Johnson, J.A.; Cavallari, L.H.; Shakhnovich, V.; Thacker, D.L.; et al. Clinical Pharmacogenetics Implementation Consortium (CPIC) Guideline for CYP2C19 and Proton Pump Inhibitor Dosing. Clin. Pharmacol. Ther. 2020, 109, 1417–1423. [Google Scholar] [CrossRef]

| Population Characteristics for Pre-Program Period | |||
|---|---|---|---|
| Variables | Intervention (n = 5288) | Control (n = 22,357) | p-Value |
| Age in Years, avg (SD) | 73.7 (5.7) | 74.0 (6.2) | 0.0007 |
| 65–74, n (%) | 3249 (61%) | 13,382 (60%) | <0.0001 |
| 75–84 | 1696 (32%) | 6849 (31%) | |
| ≥85 | 343 (6%) | 2126 (10%) | |
| Sex, n (%) | |||
| Female | 3523 (67%) | 14,893 (67%) | 1 |
| Male | 1765 (33%) | 7464 (33%) | |
| Charlson Comorbidity Index, avg (SD) | 3.6 (1.4) | 3.6 (1.5) | 1 |
| 0–2, n (%) | 1113 (21%) | 4789 (21%) | 0.3509 |
| 3–4 | 3144 (59%) | 13,056 (58%) | |
| 5+ | 1031 (19%) | 4512 (20%) | |
| Number of Medications, avg (SD) | 13.0 (8.4) | 11.9 (8.3) | <0.0001 |
| 0, n (%) | 79 (1%) | 584 (3%) | <0.0001 |
| 1–2 | 223 (4%) | 1281 (6%) | |
| 3–4 | 429 (8%) | 1997 (9%) | |
| 5–7 | 786 (15%) | 3788 (17%) | |
| 8–10 | 904 (17%) | 3703 (17%) | |
| 11+ | 2867 (54%) | 11,004 (49%) | |
| Risks Associated with Pre-Intervention Regimens | |
|---|---|
| Identified Risk | n (%) |
| AGS Beers Criteria® | 4232 (90%) |
| Drug–Drug Interaction | 4083 (87%) |
| ADR (FDA Black Box) | 3978 (84%) |
| Genetic | 3110 (66%) |
| Anticholinergic Burden | 2645 (56%) |
| Lifestyle | 1171 (25%) |
| Contraindication | 9 (0%) |
| Total Interventions (MAPs) | 4716 (100%) |
| Pharmacist Recommendations (MAPs) | |
|---|---|
| Actionable MAPs n (%) | 3228 |
| Monitor * | 2545 (78.8%) |
| Future Concern † | 714 (22.1%) |
| Discontinue Medication | 502 (15.6%) |
| Modify Prescription | 461 (14.3%) |
| Initiate New Medication | 398 (12.3%) |
| Healthcare Resource Utilization (Intervention Group) | |||
|---|---|---|---|
| Place of Service | HRU Events | ||
| Expected * | Actual | % Avoided | |
| Outpatient | 315,058 | 309,126 | 1.9% |
| Emergency Department | 7129 | 6644 | 6.8% |
| Inpatient | 13,340 | 11,351 | 14.9% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jarvis, J.P.; Peter, A.P.; Keogh, M.; Baldasare, V.; Beanland, G.M.; Wilkerson, Z.T.; Kradel, S.; Shaman, J.A. Real-World Impact of a Pharmacogenomics-Enriched Comprehensive Medication Management Program. J. Pers. Med. 2022, 12, 421. https://doi.org/10.3390/jpm12030421
Jarvis JP, Peter AP, Keogh M, Baldasare V, Beanland GM, Wilkerson ZT, Kradel S, Shaman JA. Real-World Impact of a Pharmacogenomics-Enriched Comprehensive Medication Management Program. Journal of Personalized Medicine. 2022; 12(3):421. https://doi.org/10.3390/jpm12030421
Chicago/Turabian StyleJarvis, Joseph P., Arul Prakasam Peter, Murray Keogh, Vince Baldasare, Gina M. Beanland, Zachary T. Wilkerson, Steven Kradel, and Jeffrey A. Shaman. 2022. "Real-World Impact of a Pharmacogenomics-Enriched Comprehensive Medication Management Program" Journal of Personalized Medicine 12, no. 3: 421. https://doi.org/10.3390/jpm12030421
APA StyleJarvis, J. P., Peter, A. P., Keogh, M., Baldasare, V., Beanland, G. M., Wilkerson, Z. T., Kradel, S., & Shaman, J. A. (2022). Real-World Impact of a Pharmacogenomics-Enriched Comprehensive Medication Management Program. Journal of Personalized Medicine, 12(3), 421. https://doi.org/10.3390/jpm12030421






