Impact of Frailty on the Relationship between Blood Pressure and Cardiovascular Diseases and Mortality in Young-Old Adults
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Source and Study Subjects
2.2. BP Measurements
2.3. Physical Function Test
2.4. Study Endpoints
2.5. Covariates
2.6. Statistical Analyses
3. Results
3.1. Baseline Characteristics
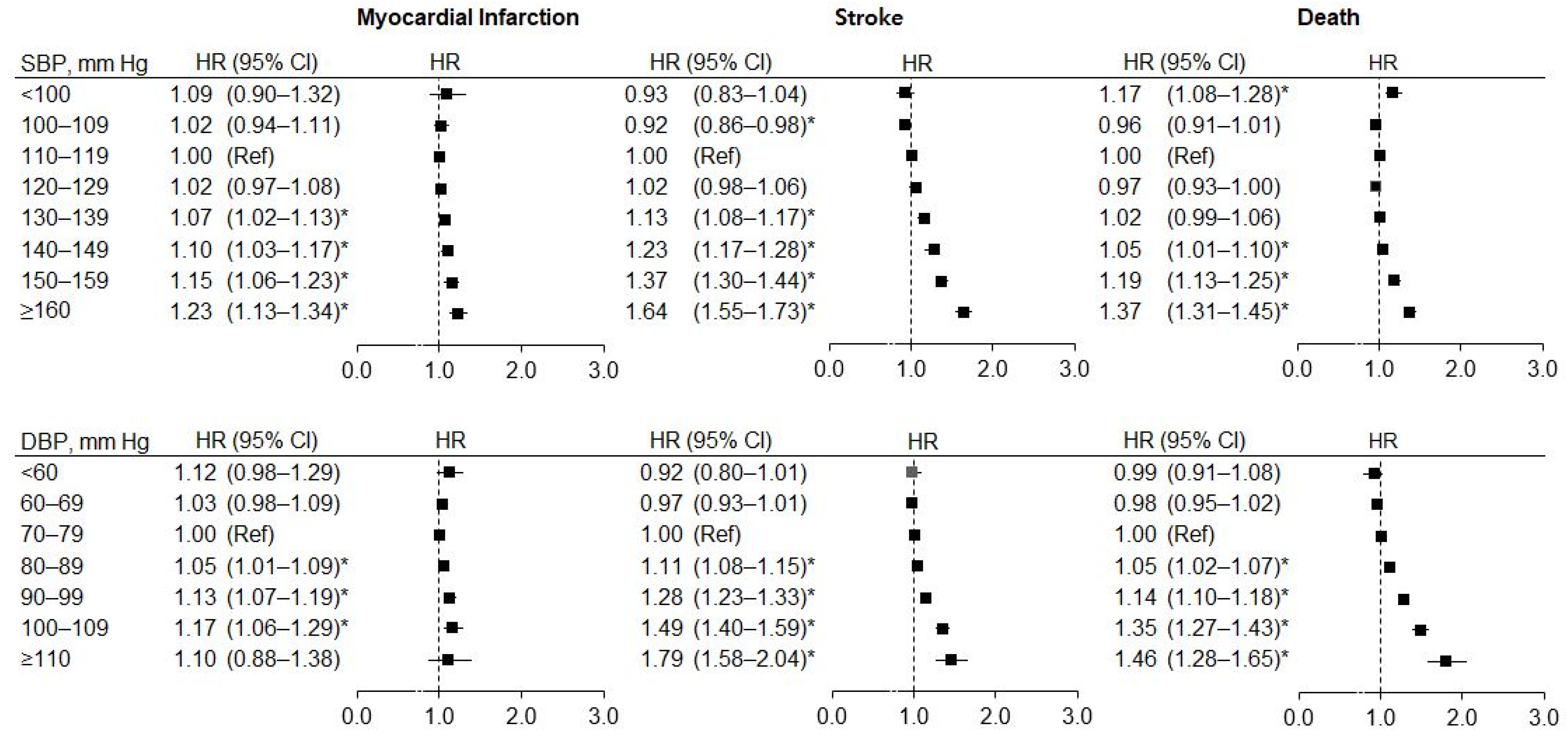
3.2. Risk of MI, Stroke, and Mortality by BP in all Subjects
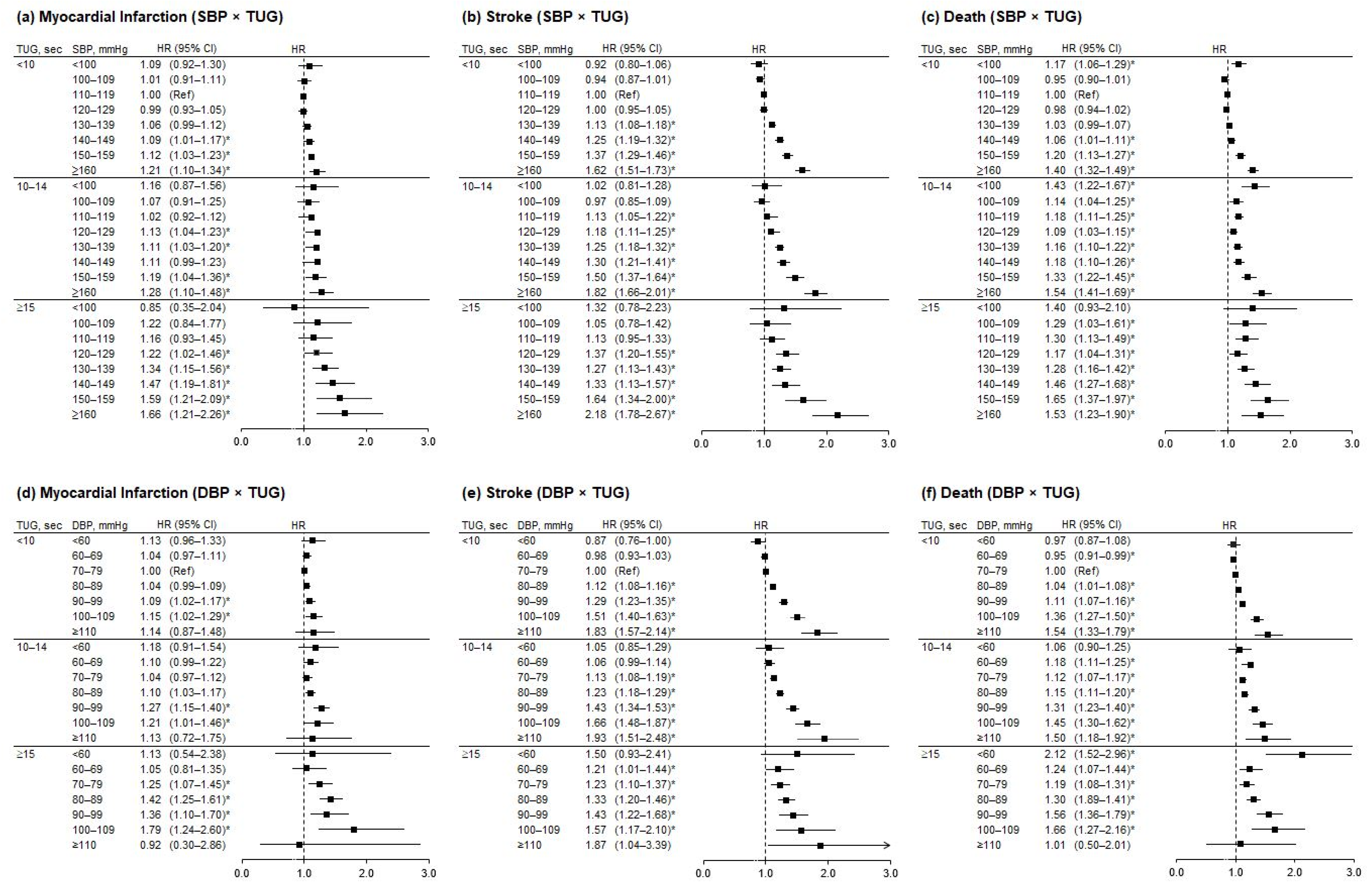
3.3. Risk of MI, Stroke, and Mortality by BP and TUG Results
3.4. Risk of MI, Stroke, and Mortality by BP within a Group Stratified by TUG Results
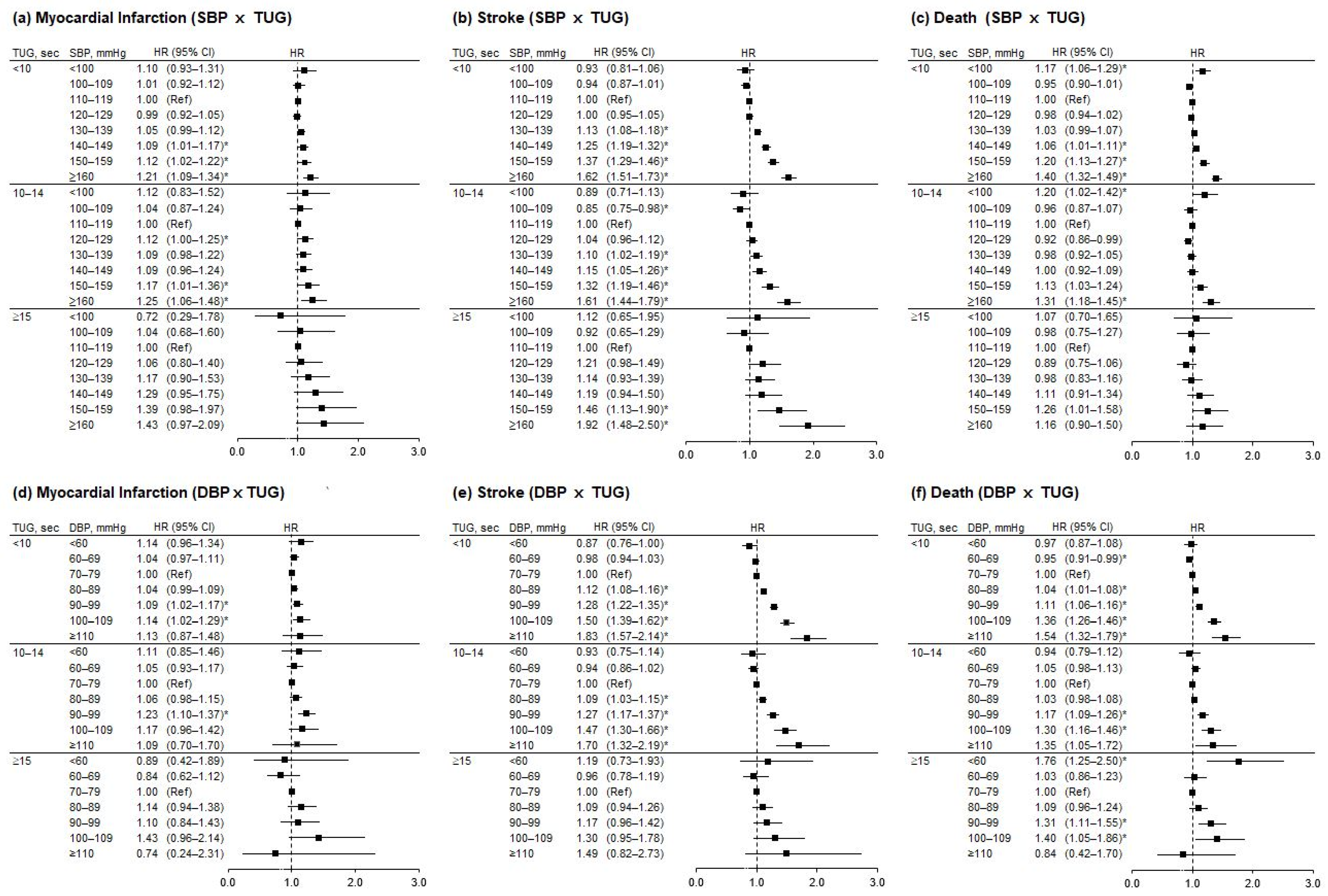
3.5. Risk of MI, Stroke, and Mortality by BP and TUG Stratified by Antihypertensive Treatment
4. Discussion
4.1. Frailty and Cardiovascular Diseases (CVDs)
4.2. Blood Pressure Goals
4.3. Elevated BP and CVDs
4.4. Treated and Untreated High BP and Outcomes
4.5. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gutierrez-Misis, A.; Sanchez-Santos, M.T.; Banegas, J.R.; Castell, M.V.; Gonzalez-Montalvo, J.I.; Otero, A. Walking speed and high blood pressure mortality risk in a Spanish elderly population. J. Hum. Hypertens. 2015, 29, 566–572. [Google Scholar] [CrossRef] [PubMed]
- Matsuzawa, Y.; Konishi, M.; Akiyama, E.; Suzuki, H.; Nakayama, N.; Kiyokuni, M.; Sumita, S.; Ebina, T.; Kosuge, M.; Hibi, K.; et al. Association between gait speed as a measure of frailty and risk of cardiovascular events after myocardial infarction. J. Am. Coll. Cardiol. 2013, 61, 1964–1972. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Odden, M.C.; Covinsky, K.E.; Neuhaus, J.M.; Mayeda, E.R.; Peralta, C.A.; Haan, M.N. The association of blood pressure and mortality differs by self-reported walking speed in older Latinos. J. Gerontol. Ser. A 2012, 67, 977–983. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Odden, M.C.; Peralta, C.A.; Haan, M.N.; Covinsky, K.E. Rethinking the association of high blood pressure with mortality in elderly adults: The impact of frailty. Arch. Intern. Med. 2012, 172, 1162–1168. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Peralta, C.A.; Katz, R.; Newman, A.B.; Psaty, B.M.; Odden, M.C. Systolic and diastolic blood pressure, incident cardiovascular events, and death in elderly persons: The role of functional limitation in the Cardiovascular Health Study. Hypertension 2014, 64, 472–480. [Google Scholar] [CrossRef] [Green Version]
- Post Hospers, G.; Smulders, Y.M.; Maier, A.B.; Deeg, D.J.; Muller, M. Relation between blood pressure and mortality risk in an older population: Role of chronological and biological age. J. Intern. Med. 2015, 277, 488–497. [Google Scholar] [CrossRef] [Green Version]
- Ravindrarajah, R.; Hazra, N.C.; Hamada, S.; Charlton, J.; Jackson, S.H.D.; Dregan, A.; Gulliford, M.C. Systolic Blood Pressure Trajectory, Frailty, and All-Cause Mortality >80 Years of Age: Cohort Study Using Electronic Health Records. Circulation 2017, 135, 2357–2368. [Google Scholar] [CrossRef] [Green Version]
- Wu, C.; Smit, E.; Peralta, C.A.; Sarathy, H.; Odden, M.C. Functional Status Modifies the Association of Blood Pressure with Death in Elders: Health and Retirement Study. J. Am. Geriatr. Soc. 2017, 65, 1482–1489. [Google Scholar] [CrossRef]
- Beckett, N.; Peters, R.; Tuomilehto, J.; Swift, C.; Sever, P.; Potter, J.; McCormack, T.; Forette, F.; Gil-Extremera, B.; Dumitrascu, D.; et al. Immediate and late benefits of treating very elderly people with hypertension: Results from active treatment extension to Hypertension in the Very Elderly randomised controlled trial. BMJ 2011, 344, d7541. [Google Scholar] [CrossRef] [Green Version]
- Beckett, N.S.; Peters, R.; Fletcher, A.E.; Staessen, J.A.; Liu, L.; Dumitrascu, D.; Stoyanovsky, V.; Antikainen, R.L.; Nikitin, Y.; Anderson, C.; et al. Treatment of hypertension in patients 80 years of age or older. N. Engl. J. Med. 2008, 358, 1887–1898. [Google Scholar] [CrossRef] [Green Version]
- Group, S.R.; Wright, J.T., Jr.; Williamson, J.D.; Whelton, P.K.; Snyder, J.K.; Sink, K.M.; Rocco, M.V.; Reboussin, D.M.; Rahman, M.; Oparil, S.; et al. A Randomized Trial of Intensive versus Standard Blood-Pressure Control. N. Engl. J. Med. 2015, 373, 2103–2116. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Zhang, S.; Deng, Y.; Wu, S.; Ren, J.; Sun, G.; Yang, J.; Jiang, Y.; Xu, X.; Wang, T.D.; et al. Trial of Intensive Blood-Pressure Control in Older Patients with Hypertension. N. Engl. J. Med. 2021, 385, 1268–1279. [Google Scholar] [CrossRef] [PubMed]
- Warwick, J.; Falaschetti, E.; Rockwood, K.; Mitnitski, A.; Thijs, L.; Beckett, N.; Bulpitt, C.; Peters, R. No evidence that frailty modifies the positive impact of antihypertensive treatment in very elderly people: An investigation of the impact of frailty upon treatment effect in the HYpertension in the Very Elderly Trial (HYVET) study, a double-blind, placebo-controlled study of antihypertensives in people with hypertension aged 80 and over. BMC Med. 2015, 13, 78. [Google Scholar] [CrossRef] [Green Version]
- Giffin, A.; Madden, K.M.; Hogan, D.B. Blood Pressure Targets for Older Patients-Do Advanced Age and Frailty Really Not Matter? Can. Geriatr. J. 2020, 23, 205–209. [Google Scholar] [CrossRef]
- Podsiadlo, D.; Richardson, S. The timed “Up & Go”: A test of basic functional mobility for frail elderly persons. J. Am. Geriatr. Soc. 1991, 39, 142–148. [Google Scholar] [CrossRef]
- Savva, G.M.; Donoghue, O.A.; Horgan, F.; O’Regan, C.; Cronin, H.; Kenny, R.A. Using timed up-and-go to identify frail members of the older population. J. Gerontol. Ser. A 2013, 68, 441–446. [Google Scholar] [CrossRef]
- Jung, H.W.; Kim, S.; Jang, I.Y.; Shin, D.W.; Lee, J.E.; Won, C.W. Screening Value of Timed Up and Go Test for Frailty and Low Physical Performance in Korean Older Population: The Korean Frailty and Aging Cohort Study (KFACS). Ann. Geriatr. Med. Res. 2020, 24, 259–266. [Google Scholar] [CrossRef]
- Dumurgier, J.; Elbaz, A.; Ducimetiere, P.; Tavernier, B.; Alperovitch, A.; Tzourio, C. Slow walking speed and cardiovascular death in well functioning older adults: Prospective cohort study. BMJ 2009, 339, b4460. [Google Scholar] [CrossRef] [Green Version]
- Veronese, N.; Cereda, E.; Stubbs, B.; Solmi, M.; Luchini, C.; Manzato, E.; Sergi, G.; Manu, P.; Harris, T.; Fontana, L.; et al. Risk of cardiovascular disease morbidity and mortality in frail and pre-frail older adults: Results from a meta-analysis and exploratory meta-regression analysis. Ageing Res. Rev. 2017, 35, 63–73. [Google Scholar] [CrossRef] [Green Version]
- Chun, S.; Shin, D.W.; Han, K.; Jung, J.H.; Kim, B.; Jung, H.W.; Son, K.Y.; Lee, S.P.; Lee, S.C. The Timed Up and Go test and the ageing heart: Findings from a national health screening of 1,084,875 community-dwelling older adults. Eur. J. Prev. Cardiol. 2021, 28, 213–219. [Google Scholar] [CrossRef]
- Masoli, J.A.H.; Delgado, J.; Pilling, L.; Strain, D.; Melzer, D. Blood pressure in frail older adults: Associations with cardiovascular outcomes and all-cause mortality. Age Ageing 2020, 49, 807–813. [Google Scholar] [CrossRef] [PubMed]
- Antikainen, R.; Jousilahti, P.; Tuomilehto, J. Systolic blood pressure, isolated systolic hypertension and risk of coronary heart disease, strokes, cardiovascular disease and all-cause mortality in the middle-aged population. J. Hypertens. 1998, 16, 577–583. [Google Scholar] [CrossRef] [PubMed]
- Kannel, W.B. Blood pressure as a cardiovascular risk factor: Prevention and treatment. JAMA 1996, 275, 1571–1576. [Google Scholar] [CrossRef] [PubMed]
- Mattace-Raso, F.U.; van der Cammen, T.J.; van Popele, N.M.; van der Kuip, D.A.; Schalekamp, M.A.; Hofman, A.; Breteler, M.M.; Witteman, J.C. Blood pressure components and cardiovascular events in older adults: The Rotterdam study. J. Am. Geriatr. Soc. 2004, 52, 1538–1542. [Google Scholar] [CrossRef]
- Nielsen, W.B.; Vestbo, J.; Jensen, G.B. Isolated systolic hypertension as a major risk factor for stroke and myocardial infarction and an unexploited source of cardiovascular prevention: A prospective population-based study. J. Hum. Hypertens. 1995, 9, 175–180. [Google Scholar]
- Cruickshank, J.M. Coronary flow reserve and the J curve relation between diastolic blood pressure and myocardial infarction. BMJ 1988, 297, 1227–1230. [Google Scholar] [CrossRef] [Green Version]
- Li, J.; Somers, V.K.; Gao, X.; Chen, Z.; Ju, J.; Lin, Q.; Mohamed, E.A.; Karim, S.; Xu, H.; Zhang, L. Evaluation of Optimal Diastolic Blood Pressure Range Among Adults With Treated Systolic Blood Pressure Less Than 130 mm Hg. JAMA Netw. Open 2021, 4, e2037554. [Google Scholar] [CrossRef]
- Boutitie, F.; Gueyffier, F.; Pocock, S.; Fagard, R.; Boissel, J.P.; INDANA Project Steering Committee. J-shaped relationship between blood pressure and mortality in hypertensive patients: New insights from a meta-analysis of individual-patient data. Ann. Intern. Med. 2002, 136, 438–448. [Google Scholar] [CrossRef]
| MI, Stroke, or Death | |||
|---|---|---|---|
| Characteristics | No (n = 670,001) | Yes (n = 38,963) | p-Value |
| Sex | <0.0001 | ||
| Male | 302,784 (45.2) | 20,914 (53.7) | |
| Female | 367,217 (54.8) | 18,049 (46.3) | |
| Income | <0.0001 | ||
| Basic Livelihood Security recipients | 21,452 (3.2) | 2114 (5.4) | |
| Q1 (low) | 166,615 (24.9) | 10,120 (26.0) | |
| Q2 (low-middle) | 129,312 (19.3) | 7739 (19.86) | |
| Q3 (high-middle) | 179,599 (26.8) | 10,329 (26.5) | |
| Q4 (high) | 173,023 (25.8) | 8661 (22.2) | |
| Smoking | <0.0001 | ||
| None | 472,141 (70.5) | 24,198 (62.1) | |
| Past | 110,171 (16.4) | 6198 (15.9) | |
| Current | 87,689 (13.1) | 8567 (22.0) | |
| Drink | <0.0001 | ||
| None | 475,137 (70.9) | 26,682 (68.5) | |
| Mild | 167,022 (24.9) | 10,067 (25.8) | |
| Heavy | 27,842 (4.2) | 2214 (5.7) | |
| Regular exercise (yes) | 313,320 (46.8) | 16,289 (41.8) | <0.0001 |
| Antihypertensive drugs | 270,767 (40.4) | 19,176 (49.2) | <0.0001 |
| Diabetes mellitus | 120,441 (18.0) | 10,662 (27.4) | <0.0001 |
| eGFR, mL/min/1.73 m2 | |||
| Mean, SD | 83.7 ± 30.3 | 82.05 ± 32.66 | <0.0001 |
| <30 | 4949 (0.7) | 440 (1.1) | |
| 30–59 | 70,110 (10.5) | 5189 (13.3) | |
| ≥60 | 594,942 (88.8) | 33,334 (85.6) | <0.0001 |
| COPD | 85,691 (12.8) | 5,939 (15.2) | <0.0001 |
| BMI (kg/m2) | 24.3 ± 3.0 | 24.4 ± 3.1 | <0.0001 |
| Hemoglobin | 13.6 ± 1.4 | 13.8 ± 1.5 | <0.0001 |
| Fasting blood glucose, mg/dL | 102.8 ± 24.8 | 108.5 ± 33.8 | <0.0001 |
| Systolic blood pressure, mmHg | 128.4 ± 15.4 | 130.7 ± 16.3 | <0.0001 |
| Diastolic blood pressure, mmHg | 77.9 ± 9.7 | 79.0 ± 10.2 | <0.0001 |
| Total cholesterol, mg/dL | 199.2 ± 37.9 | 200.2 ± 39.7 | <0.0001 |
| HDL-cholesterol, mg/dL | 54.2 ± 17.0 | 52.7 ± 18.7 | <0.0001 |
| LDL-cholesterol, mg/dL | 118.7 ± 40.8 | 118.7 ± 41.2 | 0.8 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chun, S.; Han, K.; Lee, S.; Cho, M.-H.; Jeong, S.-M.; Jung, H.-W.; Son, K.-Y.; Shin, D.-W.; Lee, S.-C. Impact of Frailty on the Relationship between Blood Pressure and Cardiovascular Diseases and Mortality in Young-Old Adults. J. Pers. Med. 2022, 12, 418. https://doi.org/10.3390/jpm12030418
Chun S, Han K, Lee S, Cho M-H, Jeong S-M, Jung H-W, Son K-Y, Shin D-W, Lee S-C. Impact of Frailty on the Relationship between Blood Pressure and Cardiovascular Diseases and Mortality in Young-Old Adults. Journal of Personalized Medicine. 2022; 12(3):418. https://doi.org/10.3390/jpm12030418
Chicago/Turabian StyleChun, Sohyun, Kyungdo Han, Seungwoo Lee, Mi-Hee Cho, Su-Min Jeong, Hee-Won Jung, Ki-Young Son, Dong-Wook Shin, and Sang-Chol Lee. 2022. "Impact of Frailty on the Relationship between Blood Pressure and Cardiovascular Diseases and Mortality in Young-Old Adults" Journal of Personalized Medicine 12, no. 3: 418. https://doi.org/10.3390/jpm12030418
APA StyleChun, S., Han, K., Lee, S., Cho, M.-H., Jeong, S.-M., Jung, H.-W., Son, K.-Y., Shin, D.-W., & Lee, S.-C. (2022). Impact of Frailty on the Relationship between Blood Pressure and Cardiovascular Diseases and Mortality in Young-Old Adults. Journal of Personalized Medicine, 12(3), 418. https://doi.org/10.3390/jpm12030418








