Influence of Pregnancy on the Occurrence of Lumbar Spine Pain in Polish Women: A Retrospective Study
Abstract
:1. Introduction
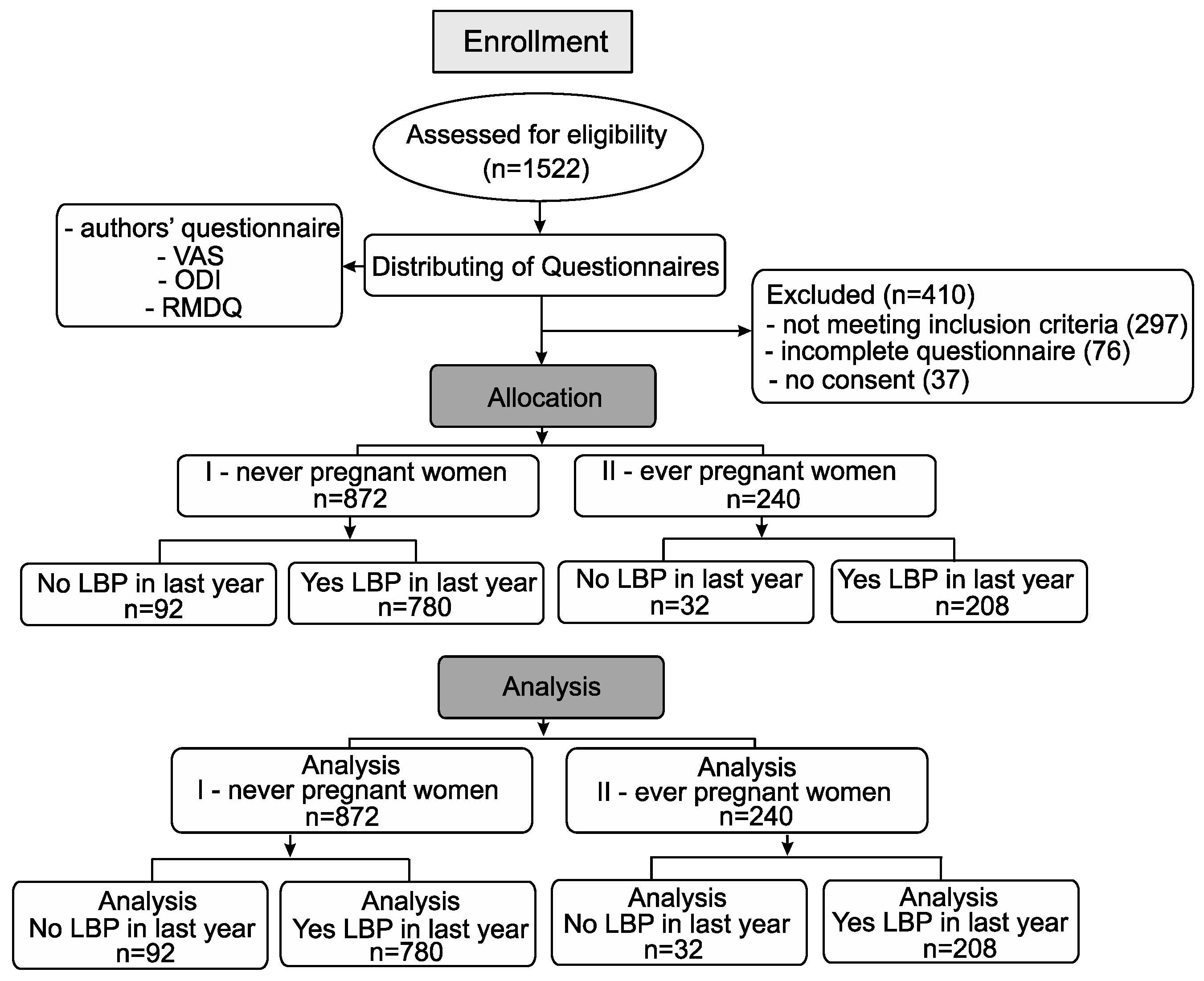
2. Materials and Methods
- history of surgery of the spine in the lumbar region,
- the presence of cancer,
- spine deformities (e.g., scoliosis),
- osteoporosis,
- multiple sclerosis,
- fractures or any abnormalities in the pelvic area,
- inflammations,
- pregnancy while completing the questionnaire,
- less than a year passed since last pregnancy,
- refusal to participate in research.
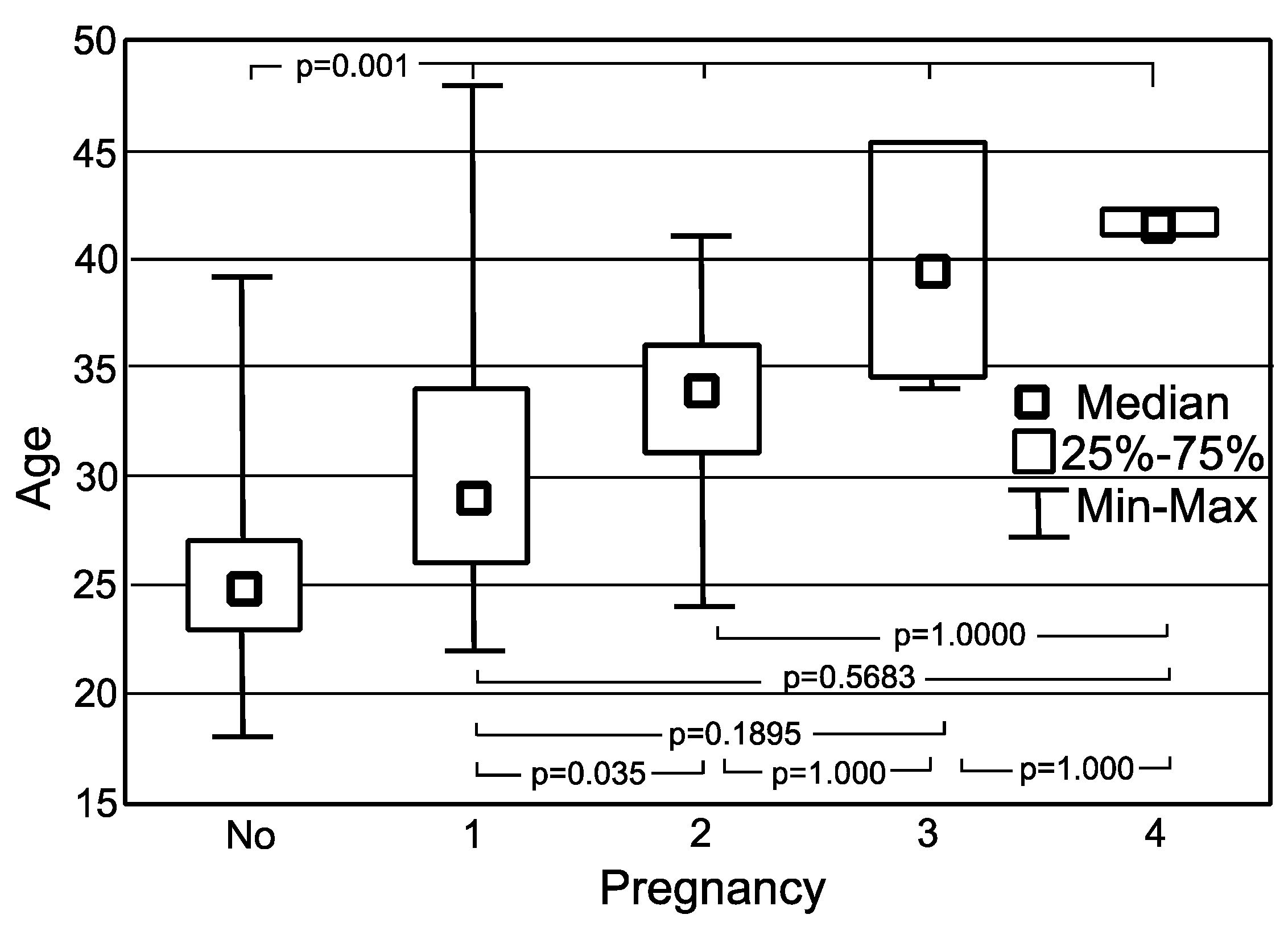
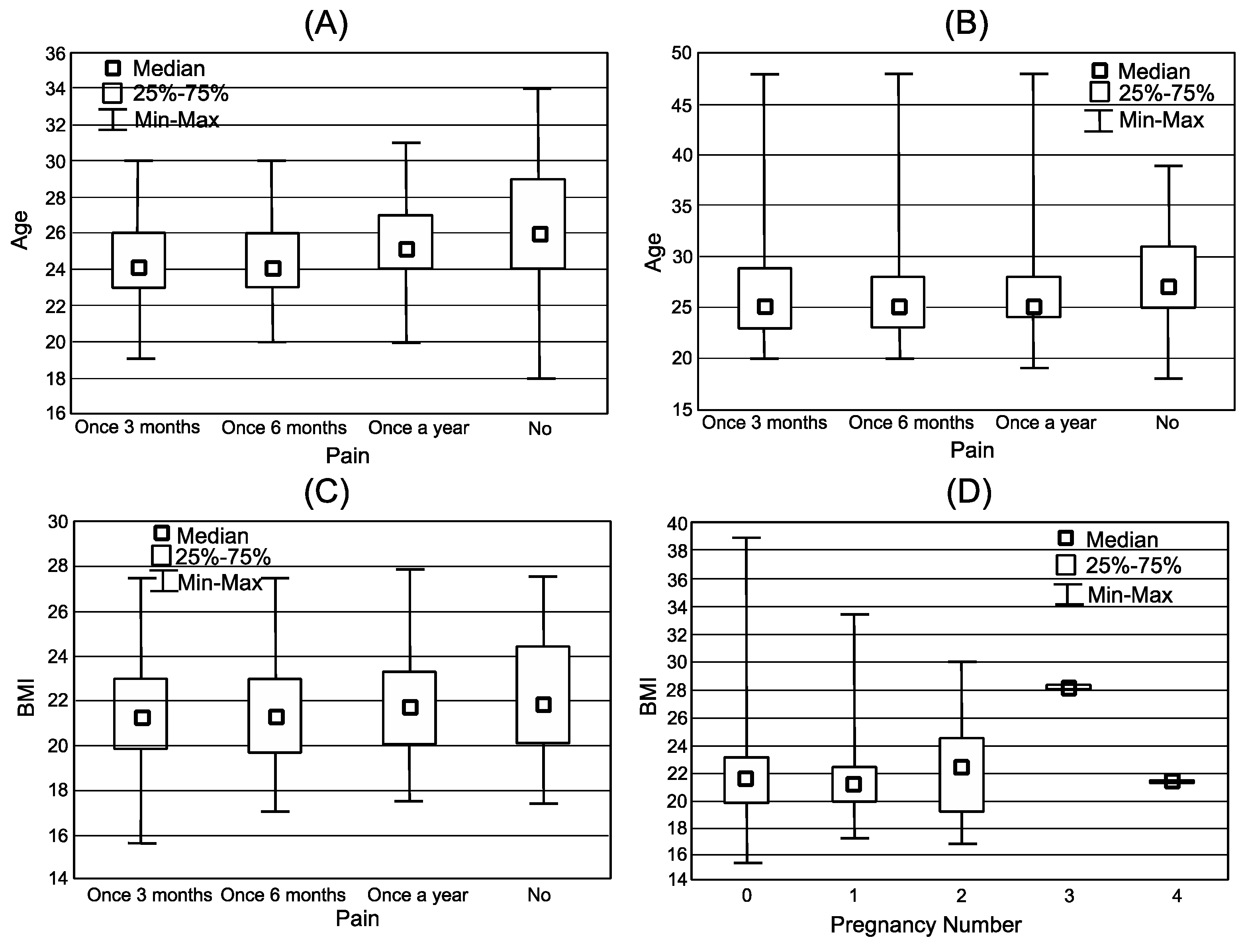
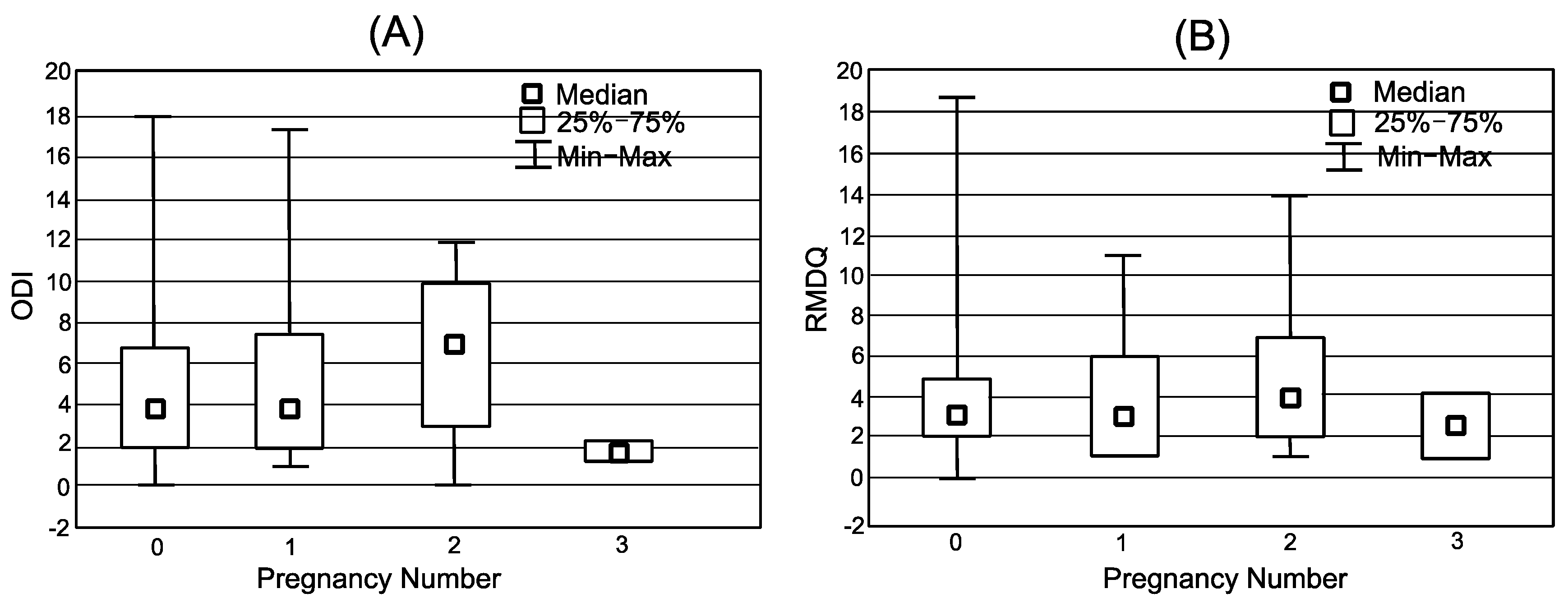
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hoy, D.; Bain, C.; Williams, G.; March, L.; Brooks, P.; Blyth, F.; Woolf, A.; Vos, T.; Buchbinder, R. A systematic review of the global prevalence of low back pain. Arthritis Rheum. 2012, 64, 2028–2037. [Google Scholar] [CrossRef]
- Glowinski, S.; Krzyzynski, T. Modelling of the ejection process in a symmetrical flight. J. Theor. Appl. Mech. 2013, 51, 775–785. [Google Scholar]
- World Health Organization. The Global Burden of Disease: 2004 Update; World Health Organization: Geneva, Switzerland, 2008. [Google Scholar]
- Hartvigsen, J.; Hancock, M.J.; Kongsted, A.; Louw, Q.; Ferreira, M.L.; Genevay, S.; Woolf, A. What low back pain is and why we need to pay attention. Lancet 2018, 391, 2356–2367. [Google Scholar] [CrossRef] [Green Version]
- Institute for Health Metrics and Evaluation. Available online: http://www.healthdata.org/gbd/data (accessed on 15 September 2021).
- Wu, A.; March, L.; Zheng, X.; Huang, J.; Wang, X.; Zhao, J.; Blyth, F.M.; Smith, E.; Buchbinder, R.; Hoy, D. Global low back pain prevalence and years lived with disability from 1990 to 2017: Estimates from the Global Burden of Disease Study. Ann. Transl. Med. 2020, 8, 299. [Google Scholar] [CrossRef]
- Chen, L.; Ferreira, M.L.; Beckenkamp, P.R.; Caputo, E.L.; Feng, S.; Ferreira, P.H. Comparative Efficacy and Safety of Conservative Care for Pregnancy-Related Low Back Pain: A Systematic Review and Network Meta-analysis. Phys. Ther. 2021, 101, pzaa200. [Google Scholar] [CrossRef] [PubMed]
- Riley, J.L., III; Robinson, M.E.; Wise, E.A.; Price, D. A meta-analytic review of pain perception across the menstrual cycle. Pain 1999, 81, 225–235. [Google Scholar] [CrossRef]
- Bryndal, A.; Majchrzycki, M.; Grochulska, A.; Glowinski, S.; Seremak-Mrozikiewicz, A. Risk factors associated with low back pain among a group of 1510 pregnant women. J. Pers. Med. 2020, 10, 51. [Google Scholar] [CrossRef] [PubMed]
- Ostgaard, H.C.; Andersson, G.B.J.; Karlsson, K. Prevalence of back pain in pregnancy. Spine 1991, 16, 549Y552. [Google Scholar] [CrossRef]
- Sakamoto, A.; Nakagawa, H.; Nakagawa, H.; Gamada, K. Effect of Exercise with a Pelvic Realignment Device on Low-Back and Pelvic Girdle Pain After Childbirth: A Randomized Control Study. J. Rehabil. Med. 2018, 50, 914–919. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Komatsu, R.; Ando, K.; Flood, P.D. Factors associated with persistent pain after childbirth: A narrative review. Br. J. Anaesth. 2020, 124, 117–130. [Google Scholar] [CrossRef] [Green Version]
- Matsuda, N.; Kitagaki, K.; Perrein, E.; Tsuboi, Y.; Ebina, A.; Kondo, Y.; Ono, R. Association between excessive weight gain during pregnancy and persistent low back and pelvic pain after delivery. Spine 2020, 45, 319–324. [Google Scholar] [CrossRef] [PubMed]
- Noren, L.; Ostgaard, S.; Johansson, G. Lumbar back and posterior pelvic pain during pregnancy: A 3-year follow-up. Eur. Spine J. 2002, 11, 267–271. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Koyanagi, A.; Stickley, A.; Garin, N.; Miret, M.; Ayuso-Mateos, J.L.; Leonardi, M.; Haro, J.M. The association between obesity and back pain in nine countries: A cross-sectional study. BMC Public Health 2015, 15, 123. [Google Scholar] [CrossRef] [PubMed]
- Shiri, R.; Karppinen, J.; Leino-Arjas, P.; Solovieva, S.; Viikari-Juntura, E. The Association between Obesity and Low Back Pain: A Meta-Analysis. Am. J. Epidemiol. 2009, 171, 135–154. [Google Scholar] [CrossRef] [Green Version]
- Bailey, A. Risk factors for low back pain in women. Menopause 2009, 16, 3–4. [Google Scholar] [CrossRef]
- Carlson, H.L.; Carlson, N.L.; Pasternak, B.A.; Balderston, K.D. Understanding and managing the back pain of pregnancy. Curr. Womens Health Rep. 2003, 3, 65–71. [Google Scholar]
- Kent, P.; Lauridsen, H.H. Managing Missing Scores on the Roland Morris Disability Questionnaire. Spine 2011, 36, 1878–1884. [Google Scholar] [CrossRef]
- Carlsson, A.M. Assessment of chronic pain. I. Aspects of the reliability and validity of the visual analogue scale. Pain 1983, 16, 87–101. [Google Scholar] [CrossRef] [PubMed]
- Roland, M.O.; Morris, R.W. A study of the natural history of back pain. Part 1: Development of a reliable and sensitive measure of disability in low back pain. Spine J. 1983, 8, 141–144. [Google Scholar] [CrossRef]
- Miekisiak, G.; Kollataj, M.; Dobrogowski, J.; Kloc, W.; Libionka, W.; Banach, M.; Latka, D.; Sobolewski, T.; Sulewski, A.; Nowakowski, A.; et al. Validation and Cross-Cultural Adaptation of the Polish Version of the Oswestry Disability Index. Spine 2013, 38, 237–243. [Google Scholar] [CrossRef]
- Quintero Rodriguez, C.; Troynikov, O. The Effect of Maternity Support Garments on Alleviation of Pains and Discomforts during Pregnancy: A Systematic Review. J. Pregnancy 2019, 2019, 2163790. [Google Scholar] [CrossRef]
- Sehmbi, H.; D’Souza, R.; Bhatia, A. Low Back Pain in Pregnancy: Investigations, Management, and Role of Neuraxial Analgesia and Anaesthesia: A Systematic Review. Gynecol. Obstet. Investig. 2017, 82, 417–436. [Google Scholar] [CrossRef] [PubMed]
- Opara, J.; Szary, S.; Kucharz, E. Polish Cultural Adaptation of the Roland-Morris Questionnaire for Evaluation of Quality of Life in Patients with Low Back Pain. Spine 2006, 31, 2744–2746. [Google Scholar] [CrossRef] [PubMed]
- Statistica. Available online: https://www.statsoft.pl (accessed on 10 November 2020).
- de Campos, T.F.; Maher, C.G.; Fuller, J.T.; Steffens, D.; Attwell, S.; Hancock, M.J. Prevention strategies to reduce future impact of low back pain: A systematic review and meta-analysis. Br. J. Sports Med. 2021, 55, 468–476. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, C.; Alburquerque-Sendín, F. Effectiveness of physical therapy for pregnancy-related low back and/or pelvic pain after delivery: A systematic review. Physiother. Theory Pract. 2012, 6, 419–431. [Google Scholar] [CrossRef]
- Wiezer, M.; Hage-Fransen, M.A.H.; Otto, A.; Wieffer-Platvoet, M.S.; Slotman, M.H.; Nijhuis-Van der Sanden, M.W.G.; Pool-Goudzwaard, A.L. Risk factors for pelvic girdle pain postpartum and pregnancy related low back pain postpartum; A systematic review and meta-analysis. Musculoskelet. Sci. Pract. 2020, 48, 102154. [Google Scholar] [CrossRef] [PubMed]
- Pennick, V.; Liddle, S.D. Interventions for Preventing and Treating Pelvic and Back Pain in Pregnancy. Cochrane Database Syst. Rev. 2013, 8, CD001139. [Google Scholar] [CrossRef]
- Kristiansson, P.; Svärdsudd, K.; von Schoultz, B. Serum relaxin, symphyseal pain, and back pain during pregnancy. Am. J. Obstet. Gynecol. 1996, 175, 1342–1347. [Google Scholar] [CrossRef]
- Mens, J.M.; Vleeming, A.; Stoeckart, R.; Stam, H.J.; Snijders, C.J. Understanding peripartum pelvic pain. Implications of a patient survey. Spine 1996, 21, 1363–1369; discussion 1369–1370. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mogren, I.M.; Pohjanen, A.I. Low back pain and pelvic pain during pregnancy: Prevalence and risk factors. Spine 2005, 30, 983–991. [Google Scholar] [CrossRef]
- Toktaş, Z.O.; Ekşi, M.Ş.; Yılmaz, B.; Demir, M.K.; Özgen, S.; Kılıç, T.; Konya, D. Association of collagen I, IX and vitamin D receptor gene polymorphisms with radiological severity of intervertebral disc degeneration in Southern European Ancestor. Eur. Spine J. 2015, 24, 2432–2441. [Google Scholar] [CrossRef] [PubMed]
- Kawaguchi, Y.; Kanamori, M.; Ishihara, H.; Ohmori, K.; Matsui, H.; Kimura, T. The association of lumbar disc disease with vitamin-D receptor gene polymorphism. J. Bone Joint Surg. Am. 2002, 84, 2022–2028. [Google Scholar] [CrossRef] [PubMed]
| All Group n = 1112 | I Never Pregnant Woman n = 872 | II Ever Pregnant Woman n = 240 | p-Value | |
|---|---|---|---|---|
| Age (years) | 26.7 (4.8) | 25.3 (3.3) | 31.8 (5.8) | 0.0000 1 |
| 18.0–48.0 | 18.0–39.0 | 22.0–48.0 | ||
| 25.0 | 25.0 | 31.0 | ||
| [26.4; 26.9] | [25.0; 25.5] | [31.1; 32.5] | ||
| Height (cm) | 167.6 (6.1) | 167.6 (6.0) | 167.8 (6.5) | 0.9781 1 |
| 152.0–185.0 | 152.0–185.0 | 157.0–185.0 | ||
| 167.0 | 167.0 | 168.0 | ||
| [167.3; 168.0] | [167.2; 168.0] | [167.0; 168.6] | ||
| Weight (kg) | 61.6 (10.2) | 61.3 (10.1) | 62.5 (10.4) | 0.0912 1 |
| 40.0–119.0 | 40.0–119.0 | 45.0–100.0 | ||
| 60.0 | 60.0 | 60.0 | ||
| [61.0; 62.2] | [60.6; 62.0] | [61.2; 63.8] | ||
| BMI (kg/m2) | 21.9 (3.0) | 21.8 (2.9) | 22.2 (3.2) | 0.2558 1 |
| 15.6–39.0 | 15.6–39.0 | 17.0–33.4 | ||
| 21.5 | 21.5 | 21.4 | ||
| [21.7; 22.0] | [21.6; 22.0] | [21.7; 22.6] |
| All Group n = 1112 | Never-Pregnant n = 872 | Ever-Pregnant n = 240 | |||
|---|---|---|---|---|---|
| Occurrence of low back pain in last year (%) | No | 124 (11%) | 92 (11%) | 32 (13%) | |
| Yes | 988 (89%) | 780 (89%) | 208 (87%) | ||
| Pain frequency (%) | No | 124 (11%) | 92 (11%) | 32 (13%) | |
| Yes—once a year | 272 (24%) | 219 (25%) | 53 (22%) | ||
| Yes—once per 6 months | 274 (25%) | 210 (24%) | 64 (27%) | ||
| Yes—once per 3 months | 442 (40%) | 351 (40%) | 91 (38%) | ||
| Occurrence of low back pain | The pain nature (%) | constant | 73 (18%) | 44 (15%) | 29(23%) |
| temporary | 191 (46%) | 137 (47%) | 54 (44%) | ||
| local | 112 (27%) | 79 (27%) | 33 (27%) | ||
| radiating | 36 (9%) | 28 (10%) | 8 (6%) | ||
| other | 4 (1%) | 4 (1%) | 0 (0%) | ||
| Time of occurrence of pain symptoms (%) | in the morning | 83 (15%) | 44 (12%) | 39 (23%) | |
| during the day | 259 (48%) | 184 (48%) | 75 (44%) | ||
| in the night | 66 (12%) | 66 (12%) | 30 (18%) | ||
| after exercise | 137 (25%) | 137 (25%) | 26 (15%) | ||
| Activities essential in everyday life, the performance of which is difficult due to pain (%) | bending down | 112 (14%) | 68 (12%) | 44 (15%) | |
| lying down sleeping | 80 (10%) | 60 (11%) | 80 (28%) | ||
| seating | 163 (21%) | 133 (24%) | 30 (10%) | ||
| standing | 118 (21%) | 91 (16%) | 27 (9%) | ||
| walking | 105 (13%) | 70 (12%) | 35 (12%) | ||
| physical activity | 87 (11%) | 57 (10%) | 30 (10%) | ||
| lifting | 130 (16%) | 84 (15%) | 46 (16%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bryndal, A.; Glowinski, S.; Majchrzycki, M. Influence of Pregnancy on the Occurrence of Lumbar Spine Pain in Polish Women: A Retrospective Study. J. Pers. Med. 2022, 12, 357. https://doi.org/10.3390/jpm12030357
Bryndal A, Glowinski S, Majchrzycki M. Influence of Pregnancy on the Occurrence of Lumbar Spine Pain in Polish Women: A Retrospective Study. Journal of Personalized Medicine. 2022; 12(3):357. https://doi.org/10.3390/jpm12030357
Chicago/Turabian StyleBryndal, Aleksandra, Sebastian Glowinski, and Marian Majchrzycki. 2022. "Influence of Pregnancy on the Occurrence of Lumbar Spine Pain in Polish Women: A Retrospective Study" Journal of Personalized Medicine 12, no. 3: 357. https://doi.org/10.3390/jpm12030357
APA StyleBryndal, A., Glowinski, S., & Majchrzycki, M. (2022). Influence of Pregnancy on the Occurrence of Lumbar Spine Pain in Polish Women: A Retrospective Study. Journal of Personalized Medicine, 12(3), 357. https://doi.org/10.3390/jpm12030357







