Vitiligo—Thyroid Disease Association: When, in Whom, and Why Should It Be Suspected? A Systematic Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategies
2.2. Laboratory Tests Used in Reviewed Studies
2.3. Interventions
2.4. Data Extraction
3. Results
4. Discussion
4.1. Temporal Association
4.2. Characteristics of Age Groups
4.3. Particular Features of the Body Distribution of Vitiligo according to Autoimmune Thyroid Pathology
4.4. Prognosis of the Association between Vitiligo, Autoimmune Thyroid Pathologies, and Oncological Treatment
5. Conclusions
- Autoimmune thyroid disease is more common among people with NSV than among the general population. Women with vitiligo more frequently presented autoimmune pathologies than men, with a higher prevalence of autoimmune thyroiditis.
- Screening for thyroid pathologies is particularly recommended for older patients with a family history of thyroid pathologies. The most common antibodies in vitiligo patients are anti-thyroid antibodies (ATPO, anti-Tg). Screening of asymptomatic patients together with early treatment of the underlying pathology leads to better results in terms of the prognosis of the pathology and the evolution of the patients compared to subjects who were not screened beforehand and presented to the doctor with an already-clinically-manifested pathology.
- Anti-TPO antibodies are a sensitive way to detect subclinical forms of autoimmune thyroiditis early. ATPO titers do not seem to correlate with the extent of vitiligo or a particular subtype of vitiligo. On the other hand, the percentage of total body surface area affected by vitiligo was found to be significantly higher in the presence of thyroid pathology, which, in turn, is more common among women.
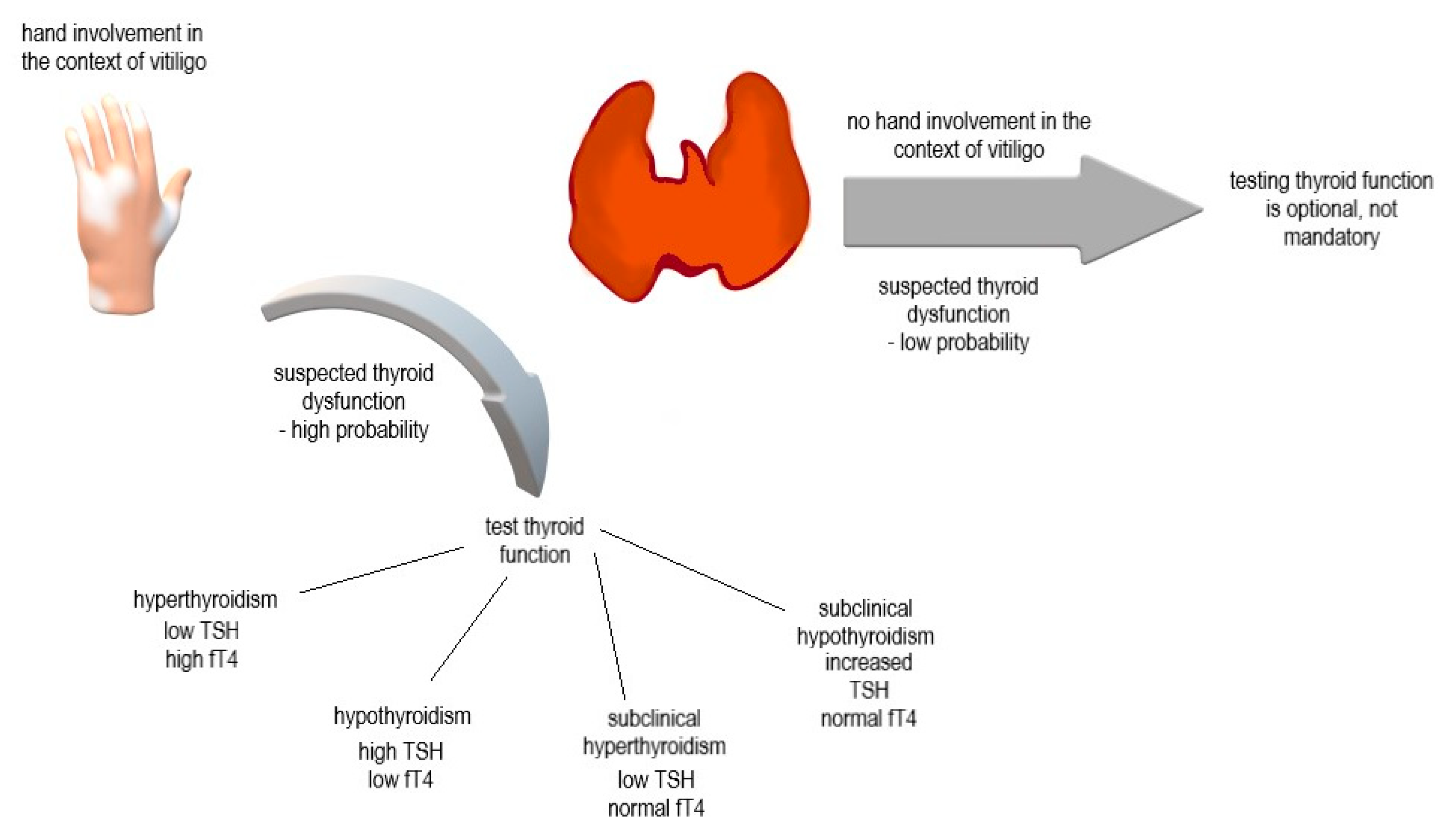
- Patients with coexisting thyroid pathologies have a predisposition to developing acral vitiligo and depigmentation of the wrists. The association between concomitant thyroid dysfunction and depigmentation of the hands is so strong that the absence of depigmented macules on the hands may exclude the coexistence of autoimmune thyroid pathology. Taken together, autoimmune thyroid pathologies appear to be the only coexisting autoimmune or inflammatory diseases in vitiligo patients to show a pattern of distribution. Although the frequency of acral involvement in patients with associated autoimmune pathologies is higher, the mechanism by which thyroid pathology influences this distribution pattern remains incompletely elucidated. One possible explanation is that these areas are more prone to the Koebner phenomenon, which, in patients with associated autoimmune pathologies, can occur through a loss of peripheral tolerance and a resulting increase in the inflammatory response. These non-specific stimuli most likely initiate an immune response that causes the recruitment of CD8+ lymphocytes directed against melanocytes.
- Vitiligo tends to precede the onset of thyroid pathology, and patients who lack other associated autoimmune or inflammatory pathologies but have a positive family history of these pathologies tend to have an early onset of vitiligo.
- The chances of repigmentation among patients with vitiligo and associated autoimmune pathologies are not statistically significant compared to the chances among patients without associated autoimmune pathologies.
- Both autoimmune thyroiditis and vitiligo can be considered immune adverse reactions during antitumor therapy, and both are positive prognostic factors for therapeutic response and survival.
- Vitiligo should be considered an integrative pathology with which other autoimmune pathologies may be associated. This framework should form the basis of clinical reasoning and guide relevant screening modalities in order to detect the onset of other diseases as early as possible. This process should be understood as reciprocal so that more attention is given to the skin in order to detect possible depigmented macules in patients with associated autoimmune polyglandular syndromes, pernicious anemia, rheumatological pathologies, alopecia areata, or thyroiditis of an autoimmune etiology.
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bergqvist, C.; Ezzedine, K. Vitiligo: A review. Dermatology 2020, 236, 571–592. [Google Scholar]
- Ferrari, S.M.; Fallahi, P.; Santaguida, G.; Virili, C.; Ruffilli, I.; Ragusa, F.; Centanni, M.; Antonelli, A. Circulating CXCL10 is increased in non-segmental vitiligo, in presence or absence of autoimmune thyroiditis. Autoimmun. Rev. 2017, 16, 946–950. [Google Scholar] [CrossRef]
- Kundu, R.V.; Mhlaba, J.M.; Rangel, S.M.; Le Poole, I.C. The convergence theory for vitiligo: A reappraisal. Exp. Dermatol. 2019, 28, 647–655. [Google Scholar] [CrossRef]
- Bú, E.A.D.; dos Santos, V.M.; Lima, K.S.; Pereira, C.R.; de Alexandre, M.E.S.; Bezerra, V.A.D.S. Neuroticism, stress, and rumination in anxiety and depression of people with Vitiligo: An explanatory model. Acta Psychol. 2022, 227, 103613. [Google Scholar] [CrossRef]
- Kussainova, A.; Kassym, L.; Akhmetova, A.; Glushkova, N.; Sabirov, U.; Adilgozhina, S.; Tuleutayeva, R.; Semenova, Y. Vitiligo and anxiety: A systematic review and meta-analysis. PLoS ONE 2020, 15, e0241445. [Google Scholar] [CrossRef]
- Ezzedine, K.; Diallo, A.; Léauté-Labrèze, C.; Seneschal, J.; Boniface, K.; Cario-André, M.; Prey, S.; Ballanger, F.; Boralevi, F.; Jouary, T.; et al. Pre- vs. post-pubertal onset of vitiligo: Multivariate analysis indicates atopic diathesis association in pre-pubertal onset vitiligo. Br. J. Dermatol. 2012, 167, 490–495. [Google Scholar] [CrossRef]
- Olejek, A.; Gabriel, I.; Bilska-Janosik, A.; Kozak-Darmas, I.; Kawczyk-Krupka, A. ALA—Photodynamic treatment in Lichen sclerosus—Clinical and immunological outcome focusing on the assesment of antinuclear antibodies. Photodiagnosis Photodyn. Ther. 2017, 18, 128–132. [Google Scholar] [CrossRef]
- Forsea, A.M.; Mihai, C.; Predescu, T.; Tudose, I.; Margaritescu, I.; Giurcaneanu, C. Polyglandular autoimmune syndrome associated with multiple autoimmune conditions and atopic dermatitis—An unusual manifestation of a polyautoimmunity phenotype. Acta Endocrinol. 2017, 13, 106–110. [Google Scholar]
- Skov, J.; Eriksson, D.; Kuja-Halkola, R.; Höijer, J.; Gudbjörnsdottir, S.; Svensson, A.-M.; Magnusson, P.; Ludvigsson, J.F.; Kämpe, O.; Bensing, S. Co-aggregation and heritability of organ-specific autoimmunity: A population-based twin study. Eur. J. Endocrinol. 2020, 182, 473–480. [Google Scholar] [CrossRef]
- Liu, Y.-H.; Chen, C.-C.; Yang, C.-M.; Chen, Y.-J.; Tsai, F.-J. Dual Effect of a Polymorphism in the Macrophage Migration Inhibitory Factor Gene Is Associated with New-Onset Graves Disease in a Taiwanese Chinese Population. PLoS ONE 2014, 9, e92849. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Syst. Rev. 2021, 10, 89. [Google Scholar]
- Freeman-Keller, M.; Kim, Y.; Cronin, H.; Richards, A.; Gibney, G.; Weber, J.S. Nivolumab in Resected and Unresectable Metastatic Melanoma: Characteristics of Immune-Related Adverse Events and Association with Outcomes. Clin. Cancer Res. 2016, 22, 886–894. [Google Scholar] [CrossRef]
- Curti, B.; Daniels, G.A.; McDermott, D.F.; Clark, J.I.; Kaufman, H.L.; Logan, T.F.; Singh, J.; Kaur, M.; Luna, T.L.; Gregory, N.; et al. Improved survival and tumor control with interleukin-2 is associated with the development of immune-related adverse events: Data from the proclaim(sm) registry. J. Immunother. Cancer 2017, 5, 102. [Google Scholar]
- Alkhateeb, A.; Fain, P.R.; Thody, A.; Bennett, D.; Spritz, R.A. Epidemiology of Vitiligo and Associated Autoimmune Diseases in Caucasian Probands and Their Families. Pigment. Cell Res. 2003, 16, 208–214. [Google Scholar] [CrossRef]
- Blomhoff, A.; Kemp, E.H.; Gawkrodger, D.J.; Weetman, A.P.; Husebye, E.S.; Akselsen, H.E.; Lie, B.A.; Undlien, D.E. CTLA4 polymorphisms are associated with vitiligo, in patients with concomitant autoimmune diseases. Pigment Cell Res. 2005, 18, 55–58. [Google Scholar] [CrossRef]
- Li, J.; Yan, M.; Zhang, Y.; Feng, C.; Wang, H.; Wang, C.; Sun, L. Meta-analysis of the association between NLRP1 polymorphisms and the susceptibility to vitiligo and associated autoimmune diseases. Oncotarget 2017, 8, 88179–88188. [Google Scholar] [CrossRef]
- Birlea, S.A.; Fain, P.R.; Spritz, R.A. A Romanian Population Isolate With High Frequency of Vitiligo and Associated Autoimmune Diseases. Arch. Dermatol. 2008, 144, 310–316. [Google Scholar] [CrossRef]
- Yazdanpanah, M.J.; Seyedi Noghabi, S.A.; Taghavi, M.; Afzal Aghaee, M.; Zabolinejad, N. Comparison of Autoimmune Thyroid Disease in Patients With Progressive and Stable Vitiligo. J. Cutan. Med. Surg. 2016, 20, 135–138. [Google Scholar] [CrossRef]
- Tanioka, M.; Yamamoto, Y.; Katoh, M.; Takahashi, K.; Miyachi, Y. Vitiligo vulgaris and autoimmune diseases in japan: A report from vitiligo clinic in kyoto university hospital. Dermato-Endocrinology 2009, 1, 43–45. [Google Scholar]
- Narita, T.; Oiso, N.; Fukai, K.; Kabashima, K.; Kawada, A.; Suzuki, T. Generalized vitiligo and associated autoimmune diseases in japanese patients and their families. Allergol. Int. 2011, 60, 505–508. [Google Scholar] [CrossRef]
- Gill, L.; Zarbo, A.; Isedeh, P.; Jacobsen, G.; Lim, H.W.; Hamzavi, I. Comorbid autoimmune diseases in patients with vitiligo: A cross-sectional study. J. Am. Acad. Dermatol. 2016, 74, 295–302. [Google Scholar] [CrossRef]
- Bae, J.M.; Lee, J.H.; Yun, J.S.; Han, B.; Han, T.Y. Vitiligo and overt thyroid diseases: A nationwide population-based study in Korea. J. Am. Acad. Dermatol. 2017, 76, 871–878. [Google Scholar] [CrossRef]
- van Geel, N.; Speeckaert, M.; Brochez, L.; Lambert, J.; Speeckaert, R. Clinical profile of generalized vitiligo patients with associated autoimmune/autoinflammatory diseases. J. Eur. Acad. Dermatol. Venereol. 2014, 28, 741–746. [Google Scholar] [CrossRef]
- Yuan, J.; Sun, C.; Jiang, S.; Lu, Y.; Zhang, Y.; Gao, X.-H.; Wu, Y.; Chen, H.-D. The Prevalence of Thyroid Disorders in Patients With Vitiligo: A Systematic Review and Meta-Analysis. Front. Endocrinol. 2018, 9, 803. [Google Scholar] [CrossRef]
- Nunes, D.H.; Esser, L.M. Vitiligo epidemiological profile and the association with thyroid disease. An. Bras. Dermatol. 2011, 86, 241–248. [Google Scholar]
- Hegedüs, L.; Heidenheim, M.; Gervil, M.; Hjalgrim, H.; Høier-Madsen, M. High frequency of thyroid dysfunction in patients with vitiligo. Acta Derm.-Venereol. 1994, 74, 120–123. [Google Scholar]
- Kroon, M.; Joore, I.; Wind, B.; Leloup, M.; Wolkerstorfer, A.; Luiten, R.; Bos, J.; Geskus, R.; Van Der Veen, J. Low yield of routine screening for thyroid dysfunction in asymptomatic patients with vitiligo. Br. J. Dermatol. 2012, 166, 532–538. [Google Scholar] [CrossRef]
- Ingordo, V.; Cazzaniga, S.; Raone, B.; Digiuseppe, M.D.; Musumeci, M.L.; Fai, D.; Pellegrino, M.; Pezzarossa, E.; Di Lernia, V.; Battarra, V.C.; et al. Circulating Autoantibodies and Autoimmune Comorbidities in Vitiligo Patients: A Multicenter Italian Study. Dermatology 2014, 228, 240–249. [Google Scholar] [CrossRef]
- Vanderpump, M.P.J.; Tunbrldge, W.M.G.; French, J.M.; Appleton, D.; Bates, D.; Clark, F.; Evans, J.G.; Hasan, D.M.; Rodgers, H.; Tunbridge, F.; et al. The incidence of thyroid disorders in the community: A twenty-year follow-up of the Whickham Survey. Clin. Endocrinol. 1995, 43, 55–68. [Google Scholar] [CrossRef]
- Dash, R.; Mohapatra, A.; Manjunathswamy, B.S. Anti-Thyroid Peroxidase Antibody in Vitiligo: A Prevalence Study. J. Thyroid Res. 2015, 2015, 192736. [Google Scholar] [CrossRef]
- Daneshpazhooh, M.; G, M.M.; Behjati, J.; Akhyani, M.; Robati, R.M. Anti-thyroid peroxidase antibody and vitiligo: A controlled study. BMC Dermatol. 2006, 6, 3. [Google Scholar] [CrossRef][Green Version]
- Patel, S.; Rauf, A.; Khan, H.; Meher, B.R.; Hassan, S.S.U. A holistic review on the autoimmune disease vitiligo with emphasis on the causal factors. Biomed. Pharmacother. 2017, 92, 501–508. [Google Scholar] [CrossRef]
- Laberge, G.; Mailloux, C.M.; Gowan, K.; Holland, P.; Bennett, D.; Fain, P.R.; Spritz, R.A. Early disease onset and increased risk of other autoimmune diseases in familial generalized vitiligo. Pigment Cell Res. 2005, 18, 300–305. [Google Scholar] [CrossRef]
- Kroon, M.W.; Vrijman, C.; Chandeck, C.; Wind, B.S.; Wolkerstorfer, A.; Luiten, R.M.; Bos, J.D.; Geskus, R.B.; van Trotsenburg, P.; van der Veen, J.W. High Prevalence of Autoimmune Thyroiditis in Children and Adolescents with Vitiligo. Horm. Res. Paediatr. 2013, 79, 137–144. [Google Scholar] [CrossRef]
- Li, D.; Liang, G.; Calderone, R.; Bellanti, J.A. Vitiligo and hashimoto’s thyroiditis: Autoimmune diseases linked by clinical presentation, biochemical commonality, and autoimmune/oxidative stress-mediated toxicity pathogenesis. Med. Hypotheses 2019, 128, 69–75. [Google Scholar]
- Prindaville, B.; Rivkees, S.A. Incidence of vitiligo in children with graves’ disease and hashimoto’s thyroiditis. Int. J. Pediatr. Endocrinol. 2011, 2011, 18. [Google Scholar]
- Yang, Y.; Lin, X.; Fu, W.; Luo, X.; Kang, K. An approach to the correlation between vitiligo and autoimmune thyroiditis in Chinese children. Clin. Exp. Dermatol. 2010, 35, 706–710. [Google Scholar] [CrossRef]
- Troshina, E.A.; Volnukhin, V.A.; Petrov, V.A.; Nuralieva, N.F.; Yukina, M.Y.; Orlova, E.M.; Frigo, N.V. The prevalence of autoimmune endocrine diseases in vitiligo patients. Ter. Arkhiv 2020, 92, 88–96. [Google Scholar] [CrossRef]
- Nicolaidou, E.; Antoniou, C.; Miniati, A.; Lagogianni, E.; Matekovits, A.; Stratigos, A.; Katsambas, A. Childhood- and later-onset vitiligo have diverse epidemiologic and clinical characteristics. J. Am. Acad. Dermatol. 2012, 66, 954–958. [Google Scholar] [CrossRef]
- Cho, S.B.; Kim, J.H.; Cho, S.; Park, J.M.; Park, Y.K.; Oh, S.H. Vitiligo in children and adolescents: Association with thyroid dysfunction. J. Eur. Acad. Dermatol. Venereol. 2011, 25, 64–67. [Google Scholar] [CrossRef]
- Fernandes, N.C.; Campos, M.M. Childhood vitiligo and thyroid disease. An. Bras. Dermatol. 2009, 84, 200–202. [Google Scholar]
- Speeckaert, R.; van Geel, N. Distribution patterns in generalized vitiligo. J. Eur. Acad. Dermatol. Venereol. 2014, 28, 755–762. [Google Scholar] [CrossRef]
- Nejad, S.B.; Qadim, H.H.; Nazeman, L.; Fadaii, R.; Goldust, M. Frequency of Autoimmune Diseases in Those Suffering from Vitiligo in Comparison with Normal Population. Pak. J. Biol. Sci. 2013, 16, 570–574. [Google Scholar] [CrossRef]
- Lazzeri, L.; Colucci, R.; Cammi, A.; Dragoni, F.; Moretti, S. Adult Onset Vitiligo: Multivariate Analysis Suggests the Need for a Thyroid Screening. BioMed Res. Int. 2016, 2016, 8065765. [Google Scholar] [CrossRef]
- Bystryn, J.-C.; Naughton, G.K. The significance of vitiligo antibodies. J. Dermatol. 1985, 12, 1–9. [Google Scholar] [CrossRef]
- Francisco, G.; Rao, B.K.; Victor, F.C. Two reports of malignant melanoma arising within a new vitiligo-like depigmented patch. JAAD Case Rep. 2018, 4, 573–575. [Google Scholar] [CrossRef]
- Pradhan, V.; Patwardhan, M.; Thakkar, V.; Kharkar, V.; Khopkar, U.; Ghosh, K.; Weetman, A.; Gawkrodger, D.; Kemp, E.H. Vitiligo patients from India (Mumbai) show differences in clinical, demographic and autoantibody profiles compared to patients in western countries. J. Eur. Acad. Dermatol. Venereol. 2013, 27, 279–286. [Google Scholar] [CrossRef]
- Galeone, M.; Colucci, R.; Dragoni, F.; Moretti, S. Can environmental factors contribute in triggering vitiligo and associated autoimmune thyroid diseases? Possible connection to the chernobyl nuclear accident. G. Ital. Dermatol. Venereol. 2018, 153, 729–730. [Google Scholar]
- Khan, S.; Gerber, D.E. Autoimmunity, checkpoint inhibitor therapy and immune-related adverse events: A review. Semin. Cancer Biol. 2020, 64, 93–101. [Google Scholar] [CrossRef]
- Lommerts, J.E.; Bekkenk, M.W.; Luiten, R.M. Vitiligo induced by immune checkpoint inhibitors in melanoma patients: An expert opinion. Expert Opin. Drug Saf. 2021, 20, 883–888. [Google Scholar] [CrossRef]
- Wang, J.-R.; Yu, K.-J.; Juan, W.-H.; Yang, C.-H. Metastatic malignant melanoma associated with vitiligo-like depigmentation. Clin. Exp. Dermatol. 2009, 34, 209–211. [Google Scholar] [CrossRef]
- Merimsky, O.; Shoenfeld, Y.; Yecheskel, G.; Chaitchik, S.; Azizi, E.; Fishman, P. Vitiligo- and melanoma-associated hypopigmentation: A similar appearance but a different mechanism. Cancer Immunol. Immunother. 1994, 38, 411–416. [Google Scholar]
- Farinazzo, E.; Zelin, E.; Agozzino, M.; Papa, G.; Pizzichetta, M.A.; di Meo, N.; Zalaudek, I. Regression of nevi, vitiligo-like depigmentation and halo phenomenon may indicate response to immunotherapy and targeted therapy in melanoma. Melanoma Res. 2021, 31, 582–585. [Google Scholar] [CrossRef]
- Hofs, T.; Zugehor, M.; Morenz, J. Melanocyte antibodies in idiopathic vitiligo (author’s transl). Dermatol. Mon. 1981, 167, 685–692. [Google Scholar]
- Hertz, K.C.; Gazze, L.A.; Kirkpatrick, C.H.; Katz, S.I. Autoimmune vitiligo: Detection of antibodies to melanin-producing cells. N. Engl. J. Med. 1977, 297, 634–637. [Google Scholar]
- Failla, C.M.; Carbone, M.L.; Fortes, C.; Pagnanelli, G.; D’Atri, S. Melanoma and Vitiligo: In Good Company. Int. J. Mol. Sci. 2019, 20, 5731. [Google Scholar] [CrossRef]
- Ranawaka, R. An observational study of alopecia areata in Sri Lankan adult patients. Ceylon Med. J. 2014, 59, 128. [Google Scholar] [CrossRef]
- Rork, J.F.; Rashighi, M.; Harris, J.E. Understanding autoimmunity of vitiligo and alopecia areata. Curr. Opin. Pediatr. 2016, 28, 463–469. [Google Scholar] [CrossRef]
- Attili, V.R.; Attili, S.K. Acral vitiligo and lichen sclerosus—Association or a distinct pattern?: A clinical and histopathological review of 15 cases. Indian J. Dermatol. 2015, 60, 519. [Google Scholar] [CrossRef]
- Baldini, E.; Odorisio, T.; Sorrenti, S.; Catania, A.; Tartaglia, F.; Carbotta, G.; Pironi, D.; Rendina, R.; D’Armiento, E.; Persechino, S.; et al. Vitiligo and Autoimmune Thyroid Disorders. Front. Endocrinol. 2017, 8, 290. [Google Scholar] [CrossRef]
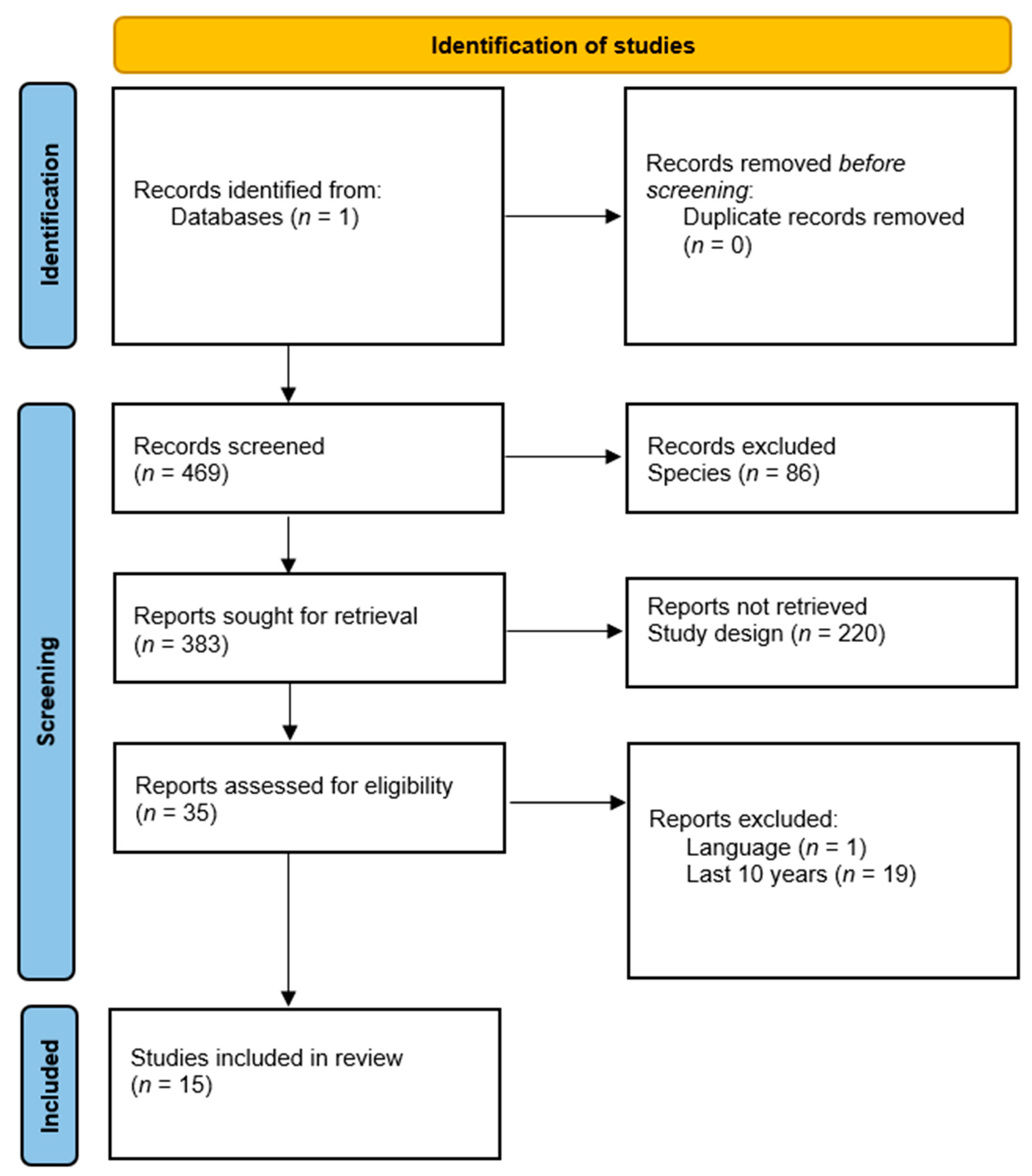
| Parameter Used | Inclusion Criteria | Exclusion Criteria |
|---|---|---|
| Language | English, French, Romanian, and Italian | Any language not already listed |
| Access | Free access to the full text | Access to the full text, financially conditional |
| Species | Human subjects | Any species other than Human |
| Type of Study | Observational, cohort, case-control, single-center or multicenter randomized studies | Review, meta-analysis, systematic review, case report studies |
| Publication period | Studies published in the last 10 years (2012–2022) | Studies published before 2012 |
| Duplicate | No | Yes |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chivu, A.M.; Bălășescu, E.; Pandia, L.D.; Nedelcu, R.I.; Brînzea, A.; Turcu, G.; Antohe, M.; Ion, D.A. Vitiligo—Thyroid Disease Association: When, in Whom, and Why Should It Be Suspected? A Systematic Review. J. Pers. Med. 2022, 12, 2048. https://doi.org/10.3390/jpm12122048
Chivu AM, Bălășescu E, Pandia LD, Nedelcu RI, Brînzea A, Turcu G, Antohe M, Ion DA. Vitiligo—Thyroid Disease Association: When, in Whom, and Why Should It Be Suspected? A Systematic Review. Journal of Personalized Medicine. 2022; 12(12):2048. https://doi.org/10.3390/jpm12122048
Chicago/Turabian StyleChivu, Ana Maria, Elena Bălășescu, Larisa Diana Pandia, Roxana Ioana Nedelcu, Alice Brînzea, Gabriela Turcu, Mihaela Antohe, and Daniela Adriana Ion. 2022. "Vitiligo—Thyroid Disease Association: When, in Whom, and Why Should It Be Suspected? A Systematic Review" Journal of Personalized Medicine 12, no. 12: 2048. https://doi.org/10.3390/jpm12122048
APA StyleChivu, A. M., Bălășescu, E., Pandia, L. D., Nedelcu, R. I., Brînzea, A., Turcu, G., Antohe, M., & Ion, D. A. (2022). Vitiligo—Thyroid Disease Association: When, in Whom, and Why Should It Be Suspected? A Systematic Review. Journal of Personalized Medicine, 12(12), 2048. https://doi.org/10.3390/jpm12122048










