Differences in Health-Related Quality of Life and Physical Condition of Two Community-Based Exercise Programs in Subjects with Cardiovascular Risk Factors: A Prospective Observational Cohort Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Community-Based Exercise Programs
2.3. Outcome Measures
2.4. Health-Related Quality of Life (HRQL)
2.5. Physical Condition
2.6. Satisfaction with the Program
2.7. Statistical Analysis
3. Results
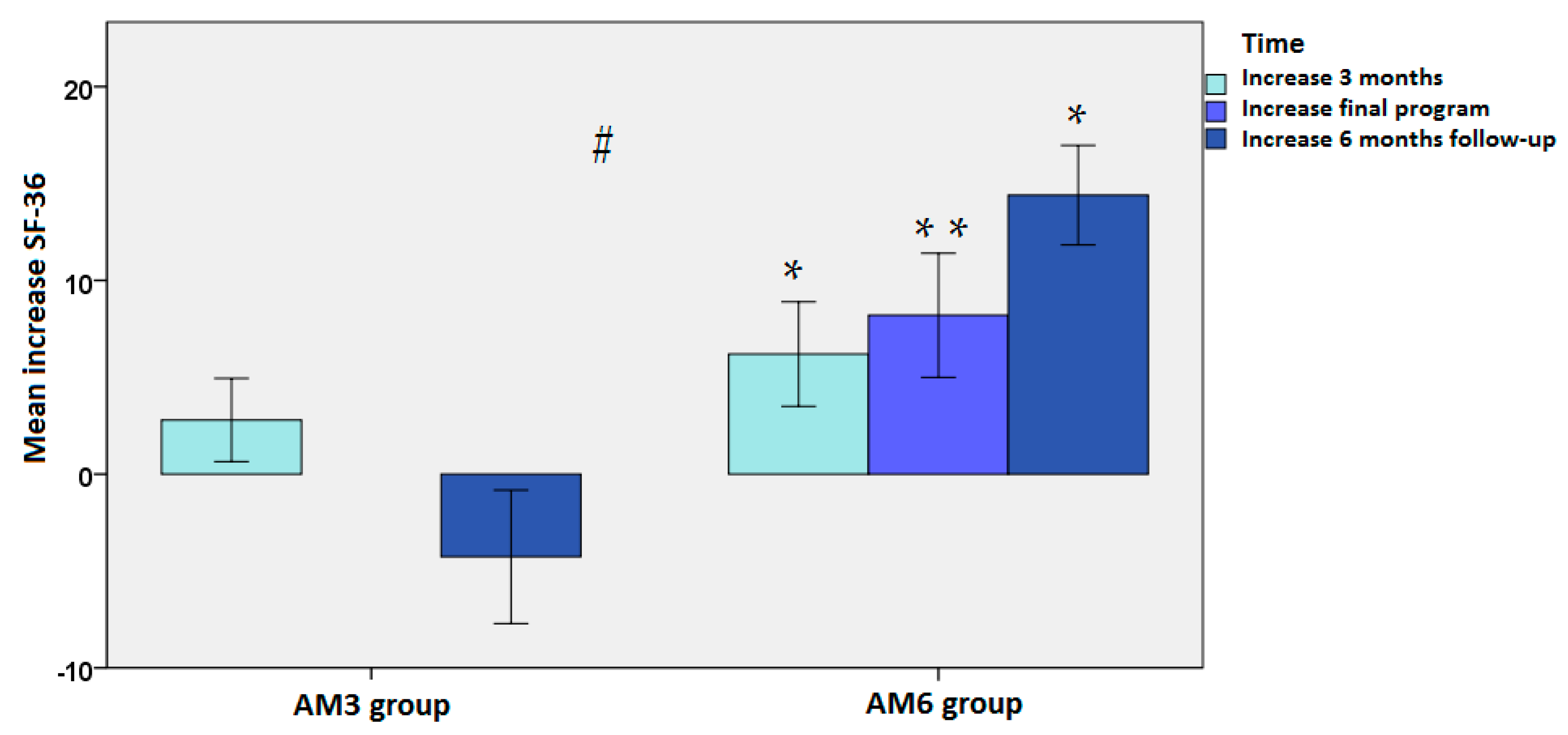
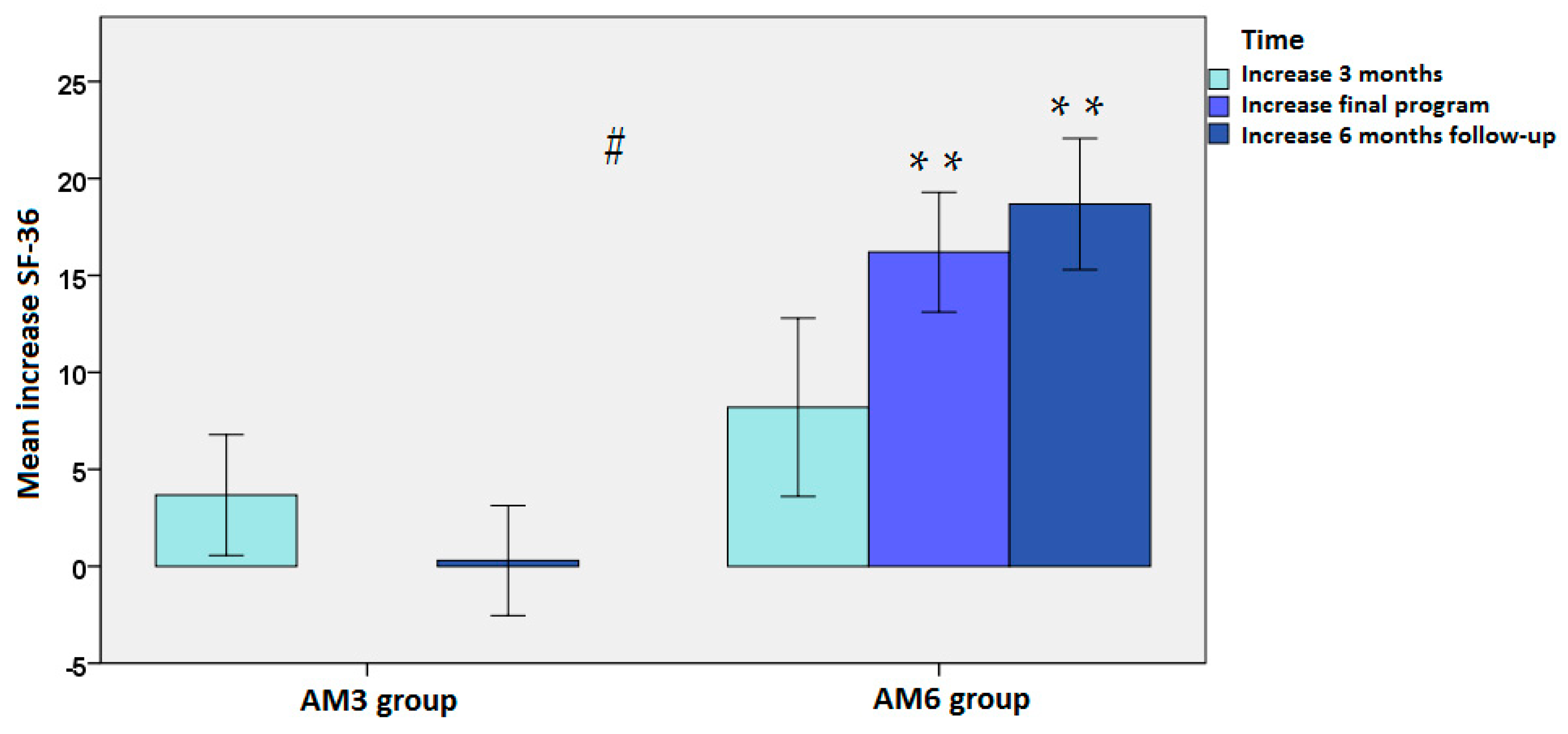
3.1. Changes in HRQL
3.2. Changes in Physical Condition
3.3. Participants’ Satisfaction
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Marquez, D.X.; Aguiñaga, S.; Vásquez, P.M.; Conroy, D.E.; Erickson, K.I.; Hillman, C.; Stillman, C.M.; Ballard, R.M.; Sheppard, B.B.; Petruzzello, S.J.; et al. A systematic review of physical activity and quality of life and well-being. Transl. Behav. Med. 2020, 10, 1098–1109. [Google Scholar] [CrossRef]
- Vagetti, G.C.; Barbosa Filho, V.C.; Moreira, N.B.; Oliveira, V.D.; Mazzardo, O.; Campos, W.D. Association between physical activity and quality of life in the elderly: A systematic review, 2000–2012. Braz. J. Psychiatry 2014, 36, 76–88. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pucci, G.C.; Rech, C.R.; Fermino, R.C.; Reis, R.S. Association between physical activity and quality of life in adults. Rev. Saude Publica 2012, 46, 166–179. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bize, R.; Johnson, J.A.; Plotnikoff, R.C. Physical activity level and health-related quality of life in the general adult population: A systematic review. Prev. Med. 2007, 45, 401–415. [Google Scholar] [CrossRef] [PubMed]
- Lavie, C.J.; Ozemek, C.; Carbone, S.; Katzmarzyk, P.T.; Blair, S.N. Sedentary behavior, exercise, and cardiovascular health. Circ. Res. 2019, 124, 799–815. [Google Scholar] [CrossRef]
- Cheng, W.; Zhang, Z.; Cheng, W.; Yang, C.; Diao, L.; Liu, W. Associations of leisure-time physical activity with cardiovascular mortality: A systematic review and meta-analysis of 44 prospective cohort studies. Eur. J. Prev. Cardiol. 2018, 25, 1864–1872. [Google Scholar] [CrossRef]
- Colberg, S.R.; Sigal, R.J.; Fernhall, B.; Regensteiner, J.G.; Blissmer, B.J.; Rubin, R.R.; Chasan-Taber, L.; Albright, A.L.; Braun, B. American College of Sports Medicine; American Diabetes Association. Exercise and type 2 diabetes: The American College of Sports Medicine and the American Diabetes Association: Joint position statement. Diabetes Care 2010, 33, e147–e167. [Google Scholar] [CrossRef] [Green Version]
- Brown, J.C.; Winters-Stone, K.; Lee, A.; Schmitz, K.H. Cancer, physical activity, and exercise. Compr. Physiol. 2012, 2, 2775–2809. [Google Scholar] [CrossRef] [Green Version]
- McTiernan, A.; Friedenreich, C.M.; Katzmarzyk, P.T.; Powell, K.E.; Macko, R.; Buchner, D.; Pescatello, L.S.; Bloodgood, B.; Tennant, B.; Vaux-Bjerke, A.; et al. Physical activity in cancer prevention and survival: A systematic review. Med. Sci. Sports Exerc. 2019, 51, 1252–1261. [Google Scholar] [CrossRef]
- Rezende, L.F.M.; Sá, T.H.; Markozannes, G.; Rey-López, J.P.; Lee, I.M.; Tsilidis, K.K.; Ioannidis, J.P.A.; Eluf-Neto, J. Physical activity and cancer: An umbrella review of the literature including 22 major anatomical sites and 770 000 cancer cases. Br. J. Sports Med. 2018, 52, 826–833. [Google Scholar] [CrossRef]
- Schmitt, N.M.; Schmitt, J.; Dören, M. The role of physical activity in the prevention of osteoporosis in postmenopausal women-An update. Maturitas 2009, 63, 34–38. [Google Scholar] [CrossRef] [PubMed]
- Borer, K.T. Physical activity in the prevention and amelioration of osteoporosis in women: Interaction of mechanical, hormonal and dietary factors. Sports Med. 2005, 35, 779–830. [Google Scholar] [CrossRef] [PubMed]
- Penedo, F.J.; Dahn, J.R. Exercise and well-being: A review of mental and physical health benefits associated with physical activity. Curr. Opin. Psychiatry 2005, 18, 189–193. [Google Scholar] [CrossRef]
- Lawton, E.; Brymer, E.; Clough, P.; Denovan, A. The relationship between the physical activity environment, nature relatedness, anxiety, and the psychological well-being benefits of regular exercisers. Front. Psychol. 2017, 8, 1058. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.P.; Chastin, S.; Chou, R.; et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 2020, 54, 1451–1462. [Google Scholar] [CrossRef]
- Bock, C.; Jarczok, M.N.; Litaker, D. Community-based efforts to promote physical activity: A systematic review of interventions considering mode of delivery, study quality and population subgroups. J. Sci. Med. Sport 2014, 17, 276–282. [Google Scholar] [CrossRef] [PubMed]
- Moore, M.; Warburton, J.; O’Halloran, P.D.; Shields, N.; Kingsley, M. Effective community-based physical activity interventions for older adults living in rural and regional areas: A systematic review. J. Aging Phys. Act. 2016, 24, 158–167. [Google Scholar] [CrossRef]
- Müller, A.M.; Khoo, S. Non-face-to-face physical activity interventions in older adults: A systematic review. Int. J. Behav. Nutr. Phys. Act. 2014, 11, 35. [Google Scholar] [CrossRef] [Green Version]
- Cooper, J.; Murphy, J.; Woods, C.; Van Nassau, F.; McGrath, A.; Callaghan, D.; Carroll, P.; Kelly, P.; Murphy, N.; Murphy, M.; et al. Barriers and facilitators to implementing community-based physical activity interventions: A qualitative systematic review. Int. J. Behav. Nutr. Phys. Act. 2021, 18, 118. [Google Scholar] [CrossRef]
- Arija, V.; Villalobos, F.; Pedret, R.; Vinuesa, A.; Timón, M.; Basora, T.; Aguas, D.; Basora, J. Pas-a-Pas research group. Effectiveness of a physical activity program on cardiovascular disease risk in adult primary health-care users: The “Pas-a-Pas” community intervention trial. BMC Public Health 2017, 17, 576. [Google Scholar] [CrossRef]
- Lawlor, E.R.; Bradley, D.T.; Cupples, M.E.; Tully, M.A. The effect of community-based interventions for cardiovascular disease secondary prevention on behavioural risk factors. Prev. Med. 2018, 114, 24–38. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hassen, H.Y.; Ndejjo, R.; Musinguzi, G.; Van Geertruyden, J.P.; Abrams, S.; Bastiaens, H. Effectiveness of community-based cardiovascular disease prevention interventions to improve physical activity: A systematic review and meta-regression. Prev. Med. 2021, 153, 106797. [Google Scholar] [CrossRef] [PubMed]
- Mendes, R.; Sousa, N.; Reis, V.M.; Themudo-Barata, J.L. Implementing low-cost, community-based exercise programs for middle-aged and older patients with type 2 diabetes: What are the benefits for glycemic control and cardiovascular risk? Int. J. Environ. Res. Public Health 2017, 149, 1057. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Farag, N.H.; Moore, W.E.; Thompson, D.M.; Kobza, C.E.; Abbott, K.; Eichner, J.E. Evaluation of a community-based participatory physical activity promotion project: Effect on cardiovascular disease risk profiles of school employees. BMC Public Health 2010, 10, 313. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- López-Román, F.J.; Tornel-Miñarro, F.I.; Delsors-Merida-Nicolich, E.; Fernández-López, L.; Martínez-Ros, M.T.; García Sánchez, E.; López-Santiago, A. Feasibility of implementing a preventive physical exercise programme recommended by general practitioners in cardiovascular risk patients: A pre-post comparison study. Eur. J. Gen. Pract. 2020, 26, 71–78. [Google Scholar] [CrossRef] [PubMed]
- García-Sánchez, E.; Rubio-Arias, J.Á.; Ávila-Gandía, V.; López-Román, F.J.; Menarguez-Puche, J.F. Effects of two community-based exercise programs on adherence, cardiometabolic markers, and body composition in older people with cardiovascular risk factors: A prospective observational cohort study. J. Pers. Med. 2020, 10, 176. [Google Scholar] [CrossRef] [PubMed]
- Alonso, J.; Prieto, L.; Antó, J.M. The Spanish version of the SF-36 Health Survey (the SF-36 health questionnaire): An instrument for measuring clinical results. Med. Clin. 1995, 104, 771–776. [Google Scholar]
- Kline, G.M.; Porcari, J.P.; Hintermeister, R.; Freedson, P.S.; Ward, A.; McCarron, R.F.; Ross, J.; Rippe, J.M. Estimation of VO2max from a one-mile track walk, gender, age, and body weight. Med. Sci. Sports Exerc. 1987, 19, 253–259. [Google Scholar] [CrossRef]
- Stockbrugger, B.A.; Haennel, R.G. Validity and reliability of a medicine ball explosive power test. J. Strength Cond. Res. 2001, 15, 431–438. [Google Scholar]
- Baltaci, G.; Un, N.; Tunay, V.; Besler, A.; Gerçeker, S. Comparison of three different sit and reach tests for measurement of hamstring flexibility in female university students. Br. J. Sports Med. 2003, 37, 59–61. [Google Scholar] [CrossRef] [Green Version]
- Walaszek, R.; Chwała, W.; Walaszek, K.; Burdacki, M.; Błaszczuk, J. Evaluation of the accuracy of the postural stability measurement with the Y-Balance Test based on the levels of the biomechanical parameters. Acta Bioeng. Biomech. 2017, 19, 121–128. [Google Scholar] [PubMed]
- Zhao, R.; Bu, W.; Chen, Y.; Chen, X. The dose-response associations of sedentary time with chronic diseases and the risk for all-cause mortality affected by different health status: A systematic review and meta-analysis. J. Nutr. Health Aging 2020, 24, 63–70. [Google Scholar] [CrossRef] [PubMed]
- Troeschel, A.N.; Hartman, T.J.; Flanders, W.D.; Akinyemiju, T.; Judd, S.; Bostick, R.M. A novel evolutionary-concordance lifestyle score is inversely associated with all-cause, all-cancer, and all-cardiovascular disease mortality risk. Eur. J. Nutr. 2021, 60, 3485–3497. [Google Scholar] [CrossRef] [PubMed]
- Miller, K.J.; Mesagno, C.; McLaren, S.; Grace, F.; Yates, M.; Gomez, R. Exercise, mood, self-efficacy, and social support as predictors of depressive symptoms in older adults: Direct and interaction effects. Front. Psychol. 2019, 10, 2145. [Google Scholar] [CrossRef] [Green Version]
- Pereira de Lima, M.; Conopca, S., Jr.; Miyabara, R.; Romeiro, G.; Campos, L.A.; Baltatu, O.C. Cardiovascular and quality of life outcomes of a 3-month physical exercise program in two Brazilian communities. Front. Med. 2020, 7, 568796. [Google Scholar] [CrossRef]
- Tsai, J.C.; Yang, H.Y.; Wang, W.H.; Hsieh, M.H.; Chen, P.T.; Kao, C.C.; Kao, P.F.; Wang, C.H.; Chan, P. The beneficial effect of regular endurance exercise training on blood pressure and quality of life in patients with hypertension. Clin. Exp. Hypertens. 2004, 26, 255–265. [Google Scholar] [CrossRef]
- Bradley, S.M.; Michos, E.D.; Miedema, M.D. Physical activity, fitness, and cardiovascular health. Insights from publications in JAMA Network Open. JAMA Netw. Open 2019, 2, e198343. [Google Scholar] [CrossRef]

| Variables | ACTIVA Murcia Community-Based Exercise Program | p Value | |
|---|---|---|---|
| AM3 (3 Months) (n = 51) | AM6 (Six Months) (n = 42) | ||
| Age, years, mean ± SD | 59.2 ± 7.4 | 59.4 ± 8.9 | 0.948 |
| Sex, % women | 82.4 | 71.4 | 0.210 |
| Weight, kg, mean ± SD | 78.7 ± 16.0 | 75.9 ± 13.5 | 0.477 |
| Body mass index (BMI), kg/m2, mean ± SD | 30.6 ± 5.3 | 29.5 ± 4.3 | 0.659 |
| Cardiovascular risk factors, % | |||
| Hypertension | 62.7 | 66.7 | 0.694 |
| Dyslipidemia | 78.4 | 76.2 | 0.797 |
| Obesity, BMI ≥ 30 kg/m2 | 51.0 | 52.4 | 0.893 |
| Overweight, BMI ≥ 25 and < 30 kg/m2 | 49.0 | 47.6 | 0.893 |
| Prediabetes | 39.2 | 35.7 | 0.728 |
| Current smoker | 9.8 | 7.1 | 0.648 |
| ACTIVA Murcia Programs | Physical Functioning | Social Functioning | Role Physical | Role Emotional | Mental Health | Energy/ Vitality | Bodily Pain | General Health | Health Transition |
|---|---|---|---|---|---|---|---|---|---|
| AM3 (n = 51) | |||||||||
| Baseline | 79.4 ± 17.6 | 79.4 ± 19.7 | 83.1 ± 34.7 | 78.4 ± 40.1 | 69.3 ± 17.4 | 56.0 ± 22.6 | 68.8 ± 24.9 | 54.9 ± 17.4 | 44.8 ± 18.2 |
| 3 months | 82.2 ± 18.0 | 84.2 ± 19.3 | 78.7 ± 37.5 | 85.3 ± 34.0 | 71.8 ± 14.3 | 59.7 ± 16.5 | 71.6 ± 22.9 | 60.0 ± 16.3 | 28.7 ± 19.6 * |
| 6 months follow-up | 75.1 ± 21.3 | 79.4 ± 18.7 | 77.9 ± 37.3 | 67.6 ± 43.0 | 67.6 ± 16.4 | 56.3 ± 18.6 | 70.2 ± 22.7 | 57.3 ± 15.1 | 40.4 ± 19.5 |
| AM6 (n = 42) | |||||||||
| Baseline | 66.9 ± 20.6 | 80.7 ± 18.8 | 64.5 ± 39.6 | 56.9 ± 48.6 | 65.5 ± 25.2 | 50.4 ± 25.0 | 60.7 ± 26.5 | 54.4 ± 20.6 | 46.9 ± 27.9 |
| 3 months | 73.9 ± 17.9 * | 82.3 ± 18.0 | 70.8 ± 38.1 | 69.4 ± 43.9 | 69.2 ± 23.8 | 59.2 ± 22.6 | 69.5 ± 21.9 | 55.3 ± 16.9 | 38.5 ± 20.8 |
| 6 months | 77.3 ± 14.8 * | 84.9 ± 16.5 | 71.9 ± 38.5 | 70.8 ± 42.1 | 74.5 ± 21.6 * | 67.3 ± 20.3 * | 75.2 ± 21.3 * | 60.0 ± 20.3 | 28.1 ± 22.5 * |
| 6 months follow-up | 80.8 ± 17.8 * | 82.8 ± 22.4 | 81.2 ± 36.3 | 79.2 ± 36.5 | 76.0 ± 17.1 * | 69.5 ± 19.5 * | 74.0 ± 26.9 * | 63.9 ± 18.9 * | 20.8 ± 14.1 * |
| AM3 vs. AM6 | |||||||||
| Baseline | p = 0.021 | p = 0.824 | p = 0.076 | p = 0.10 | p = 0.556 | p = 0.565 | p = 0.334 | p = 0.956 | p = 0.756 |
| 3 months | p = 0.712 | p = 0.892 | p = 0.987 | p = 0.233 | p = 0.872 | p = 0.887 | p = 0.899 | p = 0.589 | p = 0.08 |
| 6 months follow-up | p = 0.003 | p = 0.534 | p = 0.256 | p = 0.211 | p = 0.037 | p = 0.009 | p = 0.121 | p = 0.049 | p = 0.001 |
| Final AM3 vs. AM6 | p = 0.081 | p = 0.823 | p = 0.898 | p = 0.342 | p = 0.675 | p = 0.048 | p = 0.433 | p = 0.709 | p = 0.821 |
| ACTIVA Murcia Programs | VO2 Max mL/kg/min | Body Strength m | Flexibility cm | Balance Number of Mistakes |
|---|---|---|---|---|
| AM3 (n = 51) | ||||
| Baseline | 23.7 ± 9.4 | 4.55 ± 0.10 | 0.17 ± 7.48 | 2.51 ± 3.85 |
| 3 months | 27.7 ± 9.0 * | 5.07 ± 0.93 * | 5.00 ± 6.96 * | 1.18 ± 2.43 * |
| AM6 (n = 42) | ||||
| Baseline | 28.6 ± 10.9 | 4.89 ± 1.16 | 3.53 ± 5.92 | 2.62 ± 3.09 |
| 3 months | 30.9 ± 9.8 | 5.00 ± 1.23 | 6.78 ± 4.73 | 2.03 ± 2.39 |
| 6 months | 41.1 ± 11.4 * | 5.18 ± 1.03 * | 9.57 ± 4.93 * | 0.85 ± 1.35 * |
| AM3 vs. AM6 | ||||
| Baseline | p = 0.081 | p = 0.213 | p = 0.067 | p = 0.938 |
| 3 months | p = 0.879 | p = 0.023 | p = 0.689 | p = 0.126 |
| Final AM3 vs. AM6 | p = 0.001 | p = 0.078 | p = 0.046 | p = 0.412 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
García-Sánchez, E.; Ávila-Gandía, V.; López-Román, F.J.; Rubio-Arias, J.Á.; Menarguez-Puche, J.F. Differences in Health-Related Quality of Life and Physical Condition of Two Community-Based Exercise Programs in Subjects with Cardiovascular Risk Factors: A Prospective Observational Cohort Study. J. Pers. Med. 2022, 12, 1894. https://doi.org/10.3390/jpm12111894
García-Sánchez E, Ávila-Gandía V, López-Román FJ, Rubio-Arias JÁ, Menarguez-Puche JF. Differences in Health-Related Quality of Life and Physical Condition of Two Community-Based Exercise Programs in Subjects with Cardiovascular Risk Factors: A Prospective Observational Cohort Study. Journal of Personalized Medicine. 2022; 12(11):1894. https://doi.org/10.3390/jpm12111894
Chicago/Turabian StyleGarcía-Sánchez, Esther, Vicente Ávila-Gandía, F. Javier López-Román, Jacobo Á. Rubio-Arias, and Juan F. Menarguez-Puche. 2022. "Differences in Health-Related Quality of Life and Physical Condition of Two Community-Based Exercise Programs in Subjects with Cardiovascular Risk Factors: A Prospective Observational Cohort Study" Journal of Personalized Medicine 12, no. 11: 1894. https://doi.org/10.3390/jpm12111894
APA StyleGarcía-Sánchez, E., Ávila-Gandía, V., López-Román, F. J., Rubio-Arias, J. Á., & Menarguez-Puche, J. F. (2022). Differences in Health-Related Quality of Life and Physical Condition of Two Community-Based Exercise Programs in Subjects with Cardiovascular Risk Factors: A Prospective Observational Cohort Study. Journal of Personalized Medicine, 12(11), 1894. https://doi.org/10.3390/jpm12111894







