Markers for the Prediction of Probably Sarcopenia in Middle-Aged Individuals
Abstract
1. Introduction
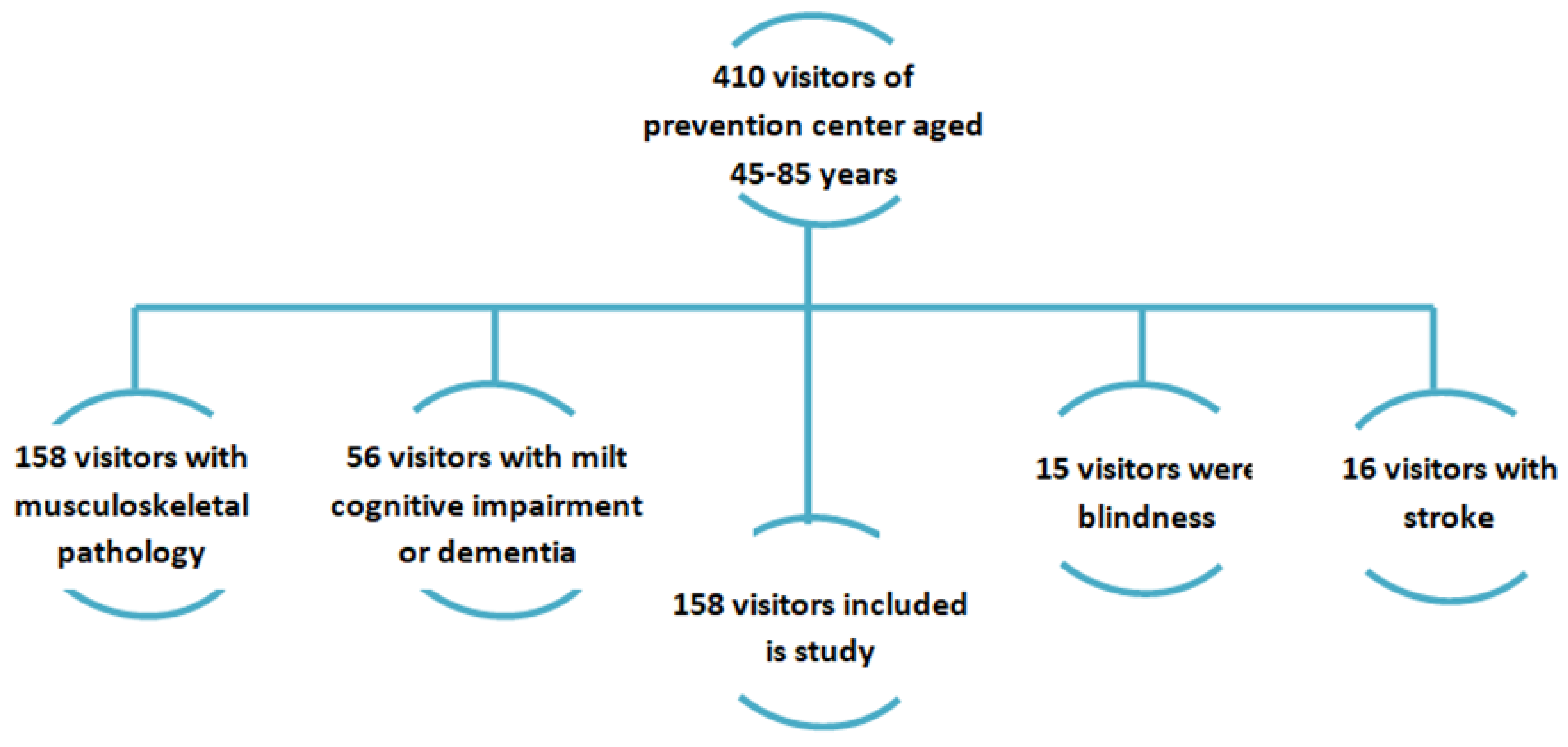
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- United Nations News Service Section. UN News Centre Opening Remarks at Press Event on Day of Seven Billion; UN News Service Section: New York, NY, USA, 2011. [Google Scholar]
- Grigorieva, I.I.; Raskina, T.A.; Letaeva, M.V.; Malyshenko, O.S.; Averkieva, Y.V.; Masenko, V.L.; Kokov, A.N. Sarcopenia: Features of pathogenesis and diagnosis. Fundam. Clin. Med. 2019, 4, 105–116. [Google Scholar] [CrossRef]
- Shafiee, G.; Keshtkar, A.; Soltani, A.; Ahadi, Z.; Larijani, B.; Heshmat, R. Prevalence of sarcopenia in the world: A systematic review and meta- analysis of general population studies. J. Diabetes Metab. Disord. 2017, 16, 21. [Google Scholar] [CrossRef] [PubMed]
- Cruz-Jentoft, A.J.; Bahat, G.; Bauer, J.; Boirie, Y.; Bruyère, O.; Cederholm, T.; Cooper, C.; Landi, F.; Rolland, Y.; Sayer, A.A.; et al. Writing Group for the European Working Group on Sarcopenia in Older People 2 (EWGSOP2), and the Extended Group for EWGSOP2. Sarcopenia: Revised European consensus on definition and diagnosis. Age Ageing 2019, 48, 16–31. [Google Scholar] [CrossRef] [PubMed]
- Bogat, S.V. The prevalence of sarcopenia in patients of older age groups. Gerontology 2014, 3, 305–310. (In Russian) [Google Scholar]
- Bischoff-Ferrari, H.A.; Orav, J.E.; Kanis, J.A.; Rizzoli, R.; Schlögl, M.; Staehelin, H.B.; Willett, W.C.; Dawson-Hughes, B. Comparative performance of current definitions of sarcopenia against the prospective incidence of falls among community-dwelling seniors age 65 and older. Osteoporos. Int. 2015, 26, 2793–2802. [Google Scholar] [CrossRef]
- Misnikova, I.V.; Kovaleva, Y.A.; Klimina, N.A. Sarkopenic obesity. Russ. Med. J. 2017, 25, 24–29. (In Russian) [Google Scholar]
- Nipp, R.D.; Fuchs, G.; El-Jawahri, A.; Mario, J.; Troschel, F.M.; Greer, J.A.; Gallagher, E.R.; Jackson, V.A.; Kambadakone, A.; Hong, T.S.; et al. Sarcopenia is Associated with Quality of Life and Depression in Patients with Advanced Cancer. Oncologist 2018, 23, 97–104. [Google Scholar] [CrossRef]
- Morville, T.; Sahl, R.E.; Trammell, S.A.; Svenningsen, J.S.; Gillum, M.P.; Helge, J.W.; Clemmensen, C. Divergent effects of resistance and endurance exercise on plasma bile acids, FGF19, and FGF21 in humans. JCI Insight 2018, 3, e122737. [Google Scholar] [CrossRef]
- Sanchis-Gomar, F.; Pareja-Galeano, H.; Santos-Lozano, A.; Garatachea, N.; Fiuza-Luces, C.; Venturini, L.; Ricevuti, G.; Lucia, A.; Emanuele, E. A preliminary candidate approach identifies the combination of chemerin, fetuin-A, and fibroblast growth factors 19 and 21 as a potential biomarker panel of successful aging. Age 2015, 37, 42. [Google Scholar] [CrossRef]
- Yamakage, H.; Tanaka, M.; Inoue, T.; Odori, S.; Kusakabe, T.; Satoh-Asahara, N. Effects of dapagliflozin on the serum levels of fibroblast growth factor 21 and myokines and muscle mass in Japanese patients with type 2 diabetes: A randomized, controlled trial. J. Diabetes Investig. 2020, 11, 653–661. [Google Scholar] [CrossRef]
- Zeng, Y.; Nie, C.; Min, J.; Liu, X.; Li, M.; Chen, H.; Xu, H.; Wang, M.; Ni, T.; Li, Y.; et al. Novel loci and pathways significantly associated with longevity. Sci Rep. 2016, 6, 21243. [Google Scholar] [CrossRef] [PubMed]
- Di Marco, S.; Mazroui, R.; Dallaire, P.; Chittur, S.; Tenenbaum, S.A.; Radzioch, D.; Marette, A.; Gallouzi, I.-E. NF-κB-mediated MyoD decay during muscle wasting requires nitric oxide synthase mRNA stabilization, HuR protein, and nitric oxide release. Mol. Cell. Biol. 2005, 25, 6533–6545. [Google Scholar] [CrossRef] [PubMed]
- Hall, D.T.; Ma, J.F.; Marco, S.D.; Di Marco, S.; Gallouzi, I.-E. Inducible nitric oxide synthase (iNOS) in muscle wasting syndrome, sarcopenia, and cachexia. Aging 2011, 3, 702–715. [Google Scholar] [CrossRef] [PubMed]
- Coggan, A.R.; Racette, S.B.; Thies, D.; Peterson, L.R.; Stratford, R.E., Jr. Simultaneous Pharmacokinetic Analysis of Nitrate and its Reduced Metabolite, Nitrite, Following Ingestion of Inorganic Nitrate in a Mixed Patient Population. Pharm. Res. 2020, 37, 235. [Google Scholar] [CrossRef] [PubMed]
- Barrera, G.; Pizzimenti, S.; Daga, M.; Dianzani, C.; Arcaro, A.; Cetrangolo, G.P.; Giordano, G.; Cucci, M.A.; Graf, M.; Gentile, F. Lipid Peroxidation-Derived Aldehydes, 4-Hydroxynonenal and Malondialdehyde in Aging-Related Disorders. Antioxidants 2018, 7, 102. [Google Scholar] [CrossRef]
- Standley, R.A.; Distefano, G.; Pereira, S.L.; Tian, M.; Kelly, O.J.; Coen, P.M.; Deutz, N.E.P.; Wolfe, R.R.; Goodpaster, B.H. Effects of β-hydroxy-β-methylbutyrate on skeletal muscle mitochondrial content and dynamics, and lipids after 10 days of bed rest in older adults. J. Appl. Physiol. 2017, 123, 1092–1100. [Google Scholar] [CrossRef]
- Lu, Y.; Niti, M.; Yap, K.B.; Tan, C.T.Y.; Nyunt, M.S.Z.; Feng, L.; Tan, B.Y.; Chan, G.; Khoo, S.A.; Chan, S.M.; et al. Effects of multi-domain lifestyle interventions on sarcopenia measures and blood biomarkers: Secondary analysis of a randomized controlled trial of community-dwelling pre-frail and frail older adults. Aging 2021, 13, 9330–9347. [Google Scholar] [CrossRef]
- Krzymińska-Siemaszko, R.; Fryzowicz, A.; Czepulis, N.; Kaluźniak-Szymanowska, A.; Dworak, L.B.; Wieczorowska-Tobis, K. The impact of the age range of young healthy reference population on the cut-off points for low muscle mass necessary for the diagnosis of sarcopenia. Eur. Rev. Med. Pharmacol. Sci. 2019, 23, 4321–4332. [Google Scholar] [CrossRef]
- Chen, L.-K.; Woo, J.; Assantachai, P.; Auyeung, T.-W.; Chou, M.-Y.; Iijima, K.; Jang, H.C.; Kang, L.; Kim, M.; Kim, S.; et al. Asian Working Group for Sarcopenia: 2019 Consensus Update on Sarcopenia Diagnosis and Treatment. J. Am. Med. Dir. Assoc. 2020, 21, 300–307.e2. [Google Scholar] [CrossRef]
- Shahar, S.; Kamaruddin, N.S.; Badrasawi, M.; Sakian, N.I.; Manaf, Z.A.; Yassin, Z.; Joseph, L. Effectiveness of exercise and protein supplementation intervention on body composition, functional fitness, and oxidative stress among elderly Malays with sarcopenia. Clin. Interv. Aging 2013, 8, 1365–1375. [Google Scholar] [CrossRef]
- Soysal, P.; Smith, L.; Isik, A.T. Validation of population-based cut-offs for low muscle mass and strength. Eur. Geriatr. Med. 2020, 11, 713–714. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.X.; Li, J.; Chen, C.; Yin, T.; Wang, Q.A.; Li, X.X.; Wang, F.X.; Zhao, J.H.; Zhao, Y.; Zhang, Y.H. Reference values of skeletal muscle mass, fat mass and fat-to-muscle ratio for rural middle age and older adults in western China. Arch. Gerontol. Geriatr. 2021, 95, 104389. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.; Park, K.S.; Yoo, J.I. Associations between the quality of life in sarcopenia measured with the SarQoL® and nutritional status. Health Qual. Life Outcomes 2021, 19, 28. [Google Scholar] [CrossRef] [PubMed]
- Krzymińska-Siemaszko, R.; Deskur-Śmielecka, E.; Styszyński, A.; Wieczorowska-Tobis, K. Polish Translation and Validation of the Mini Sarcopenia Risk Assessment (MSRA) Questionnaire to Assess Nutritional and Non-Nutritional Risk Factors of Sarcopenia in Older Adults. Nutrients 2021, 13, 1061. [Google Scholar] [CrossRef] [PubMed]
- Vandewoude, M.F.J.; Alish, C.J.; Sauer, A.C.; Hegazi, R.A. Malnutrition-sarcopenia syndrome: Is this the future of nutrition screening and assessment for older adults? J. Aging Res. 2012, 2012, 651570. [Google Scholar] [CrossRef]
- Suetta, C.; Haddock, B.; Alcazar, J.; Noerst, T.; Hansen, O.M.; Ludvig, H.; Kamper, R.S.; Schnohr, P.; Prescott, E.; Andersen, L.L.; et al. The Copenhagen Sarcopenia Study: Lean mass, strength, power, and physical function in a Danish cohort aged 20–93 years. J. Cachexia Sarcopenia Muscle 2019, 10, 1316–1329. [Google Scholar] [CrossRef] [PubMed]
- Geerinck, A.; Bruyère, O.; Locquet, M.; Reginster, J.Y.; Beaudart, C. Evaluation of the Responsiveness of the SarQoL® Questionnaire, a Patient-Reported Outcome Measure Specific to Sarcopenia. Adv. Ther. 2018, 35, 1842–1858. [Google Scholar] [CrossRef]
- Verreijen, A.M.; Engberink, M.F.; Memelink, R.G.; van der Plas, S.E.; Visser, M.; Weijs, P.J. Effect of a high protein diet and/or resistance exercise on the preservation of fat free mass during weight loss in overweight and obese older adults: A randomized controlled trial. Nutr. J. 2017, 16, 10. [Google Scholar] [CrossRef]
- Yamaguchi, T. Updates on Lifestyle-Related Diseases and Bone Metabolism. The metabolic syndrome and bone metabolism. Clin. Calcium 2014, 24, 1599–1604. [Google Scholar]
- Hernández-Martínez, P.; Olmos, J.M.; Llorca, J.; Hernández, J.L.; González-Macías, J. Sarcopenic osteoporosis, sarcopenic obesity, and sarcopenic osteoporotic obesity in the Camargo cohort (Cantabria, Spain). Arch. Osteoporos. 2022, 17, 105. [Google Scholar] [CrossRef]
- Roh, E.; Hwang, S.Y.; Yoo, H.J.; Baik, S.H.; Cho, B.; Park, Y.S.; Kim, H.J.; Lee, S.-G.; Kim, B.J.; Jang, H.C.; et al. Association of plasma FGF21 levels with muscle mass and muscle strength in a national multicentre cohort study: Korean Frailty and Aging Cohort Study. Age Ageing 2021, 50, 1971–1978. [Google Scholar] [CrossRef] [PubMed]
- Kawashima, M.; Miyakawa, M.; Sugiyama, M.; Miyoshi, M.; Arakawa, T. Unloading during skeletal muscle regeneration retards iNOS-expressing macrophage recruitment and perturbs satellite cell accumulation. Histochem. Cell Biol. 2020, 154, 355–367. [Google Scholar] [CrossRef] [PubMed]
- Bulatova, I.A.; Shchekotova, A.P.; Krivtsov, A.V.; Ulitina, P.V.; Larionova, G.G.; Paducheva, S.V. Significance of malondialdehyde and glutathione transferase in assessing liver damage and monitoring therapy in chronic hepatitis. Fundam. Res. 2014, 4, 246–251. [Google Scholar]
- Sim, M.; Lewis, J.R.; Blekkenhorst, L.C.; Bondonno, C.P.; Devine, A.; Zhu, K.; Peeling, P.; Prince, R.L.; Hodgson, J.M. Dietary nitrate intake is associated with muscle function in older women. J. Cachexia Sarcopenia Muscle 2019, 10, 601–610. [Google Scholar] [CrossRef]
- Valenzuela, P.L.; Morales, J.S.; Emanuele, E.; Pareja-Galeano, H.; Lucia, A. Supplements with purported effects on muscle mass and strength. Eur. J. Nutr. 2019, 58, 2983–3008. [Google Scholar] [CrossRef]
- Córdova, A.; Caballero-García, A.; Noriega-González, D.; Bello, H.J.; Pons, A.; Roche, E. Nitric-Oxide-Inducing Factors on Vitamin D Changes in Older People Susceptible to Suffer from Sarcopenia. Int. J. Environ. Res. Public Health 2022, 19, 5938. [Google Scholar] [CrossRef]
- Pin, F.; Beltrà, M.; Garcia-Castillo, L.; Pardini, B.; Birolo, G.; Matullo, G.; Penna, F.; Guttridge, D.; Costelli, P. Extracellular vesicles derived from tumor cells as a trigger of energy crisis in the skeletal muscle. J. Cachexia Sarcopenia Muscle 2022, 13, 481–494. [Google Scholar] [CrossRef]
- Kawamoto, R.; Kohara, K.; Katoh, T.; Kusunoki, T.; Ohtsuka, N.; Abe, M.; Kumagi, T.; Miki, T. Changes in oxidized low-density lipoprotein cholesterol are associated with changes in handgrip strength in Japanese community-dwelling persons. Endocrine 2015, 48, 871–877. [Google Scholar] [CrossRef]
- Petyaev, I.M.; Klochkov, V.A.; Chalyk, N.E.; Pristensky, D.V.; Chernyshova, M.P.; Kyle, N.H.; Bashmakov, Y.K. Markers of Hypoxia and Oxidative Stress in Aging Volunteers Ingesting Lycosomal Formulation of Dark Chocolate Containing Astaxanthin. J. Nutr. Health Aging 2018, 22, 1092–1098. [Google Scholar] [CrossRef]
- Wang, S.; Zhou, H.; Zhao, C.; He, H. Effect of Exercise Training on Body Composition and Inflammatory Cytokine Levels in Overweight and Obese Individuals: A Systematic Review and Network Meta-Analysis. Front. Immunol. 2022, 13, 921085. [Google Scholar] [CrossRef]
| Parameters | Women | p | Men | p | ||
|---|---|---|---|---|---|---|
| Main Group (n = 118) | Control Group (n = 28) | Main Group (n = 47) | Control Group (n = 28) | |||
| Age, years | 54 [48–65] | 55 [48–66] | 0.453 | 53 [49–59] | 52 [47–56.5] | 0.534 |
| Body mass index kg/m2 | 28.5 [25.1–31.8] | 28.5 [25.1–31.8] | 0.285 | 28.5 [25.1–31.8] | 28.5 [25.1–31.8] | 0.285 |
| Waist-to-hip ratio | 0.97 [0.93–1.01] | 0.96 [0.9–1.02] | 0.435 | 0.94 [0.8–1.02] | 0.95 [0.8–1.05] | 0.435 |
| Right hand, kg | 24 [19–31] | 40 [38–53] | 0.001 | 17 [15–24] | 35 [27–39] | 0.001 |
| Left hand, kg | 23 [19–29] | 38 [33–51] | 0.001 | 15 [13–22] | 33 [25–36] | 0.001 |
| Gait speed, m/s | 0.95 [0.8–1.25] | 1.15 [0.8–1.4] | <0.001 | 1.0 [0.9–1.3] | 1.2 [0.9–1.5] | <0.001 |
| Glycemia, mmol/L | 4.9 [4.6–5.3] | 4.95 [4.6–5.3] | 0.834 | 4.7 [4.3–5.2] | 4.5 [4.2–5.0] | 0.745 |
| Options | Main Group | Control Group | p |
|---|---|---|---|
| SarQol | 80.54 [67.89–86.895] | 78.03 [63.81–89.19] | 0.833 |
| HADS (anaxiety) | 4 [2–7] | 4 [2–6] | 0.108 |
| HADS (depression) | 4 [2–6] | 3 [1–5] | 0.142 |
| SF36, physical component | 55 [49–59] | 56 [50–60] | 0.228 |
| SF36, psychological component | 45 [42–48] | 46 [43–49] | 0.499 |
| Parameters | Women | p | Men | p | ||
|---|---|---|---|---|---|---|
| Main Group (n = 118) | Control Group (n = 28) | Main Group (n = 47) | Control Group (n = 28) | |||
| Body fat mass (kg) | 28 [25.1–36] | 26.5 [20.65–35] | 0.011 | 30 [26.1–38] | 26.5 [20.65–35] | 0.002 |
| Body fat percentage (%) | 35.9 [35.4–41.3] | 33.7 [29.85–40.1] | 0.0001 | 39.7 [35.6–44.8] | 35.1 [29.7–40.5] | 0.0001 |
| Visceral fat area (cm2) | 144.2 [128.3–176.1] | 129.1 [92.2–169.25] | 0.002 | 154.7 [128.3–198.4] | 132.3 [95.3–183.5] | 0.002 |
| Skeletal muscle mass (kg2) | 25.5 [23.4–27.9] | 28.6 [22.9–33.3] | 0.043 | 23.2 [21.4–27.4] | 26.4 [22.5–34.1] | 0.003 |
| Appendicular muscle mass (m2) | 6.7 [5.9–7.3] | 7.8 [6.5–8.9] | <0.001 | 6.4 [5.85–7.1] | 7.6 [6.3–8.5] | <0.001 |
| Protein content | 8.9 [8.1–10.0] | 9.5 [8.25–11.6] | 0.048 | 8.4 [7.5–9.4] | 9.3 [8.25–11.6] | 0.002 |
| Minerals | 3.1 [2.8–3.4] | 3.9 [2.9–4.0] | 0.03 | 3.0 [2.5–3.5] | 3.6 [2.8–3.9] | 0.044 |
| Metabolites | Main Group (F = M = 47) | Control Group (F = M = 28) | p |
|---|---|---|---|
| Fibroblast growth factor 21 ng/L | 263.8 [251.4–274.8] | 267 [246.5–273.5] | 0.80 |
| Nitrates, mmol/L | 0.21 [0.21–0.355] | 0.105 [0.07–0.14] | 0.05 |
| Malondialdehyde (MDA), µmol/L | 290.32 [260.97–290.32] | 147.42 [78.06–216.77] | 0.76 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Samoilova, Y.G.; Matveeva, M.V.; Khoroshunova, E.A.; Kudlay, D.A.; Oleynik, O.A.; Spirina, L.V. Markers for the Prediction of Probably Sarcopenia in Middle-Aged Individuals. J. Pers. Med. 2022, 12, 1830. https://doi.org/10.3390/jpm12111830
Samoilova YG, Matveeva MV, Khoroshunova EA, Kudlay DA, Oleynik OA, Spirina LV. Markers for the Prediction of Probably Sarcopenia in Middle-Aged Individuals. Journal of Personalized Medicine. 2022; 12(11):1830. https://doi.org/10.3390/jpm12111830
Chicago/Turabian StyleSamoilova, Yulia G., Mariia V. Matveeva, Ekaterina A. Khoroshunova, Dmitry A. Kudlay, Oxana A. Oleynik, and Liudmila V. Spirina. 2022. "Markers for the Prediction of Probably Sarcopenia in Middle-Aged Individuals" Journal of Personalized Medicine 12, no. 11: 1830. https://doi.org/10.3390/jpm12111830
APA StyleSamoilova, Y. G., Matveeva, M. V., Khoroshunova, E. A., Kudlay, D. A., Oleynik, O. A., & Spirina, L. V. (2022). Markers for the Prediction of Probably Sarcopenia in Middle-Aged Individuals. Journal of Personalized Medicine, 12(11), 1830. https://doi.org/10.3390/jpm12111830







