Endotracheal Intubation Using C-MAC Video Laryngoscope vs. Direct Laryngoscope While Wearing Personal Protective Equipment
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
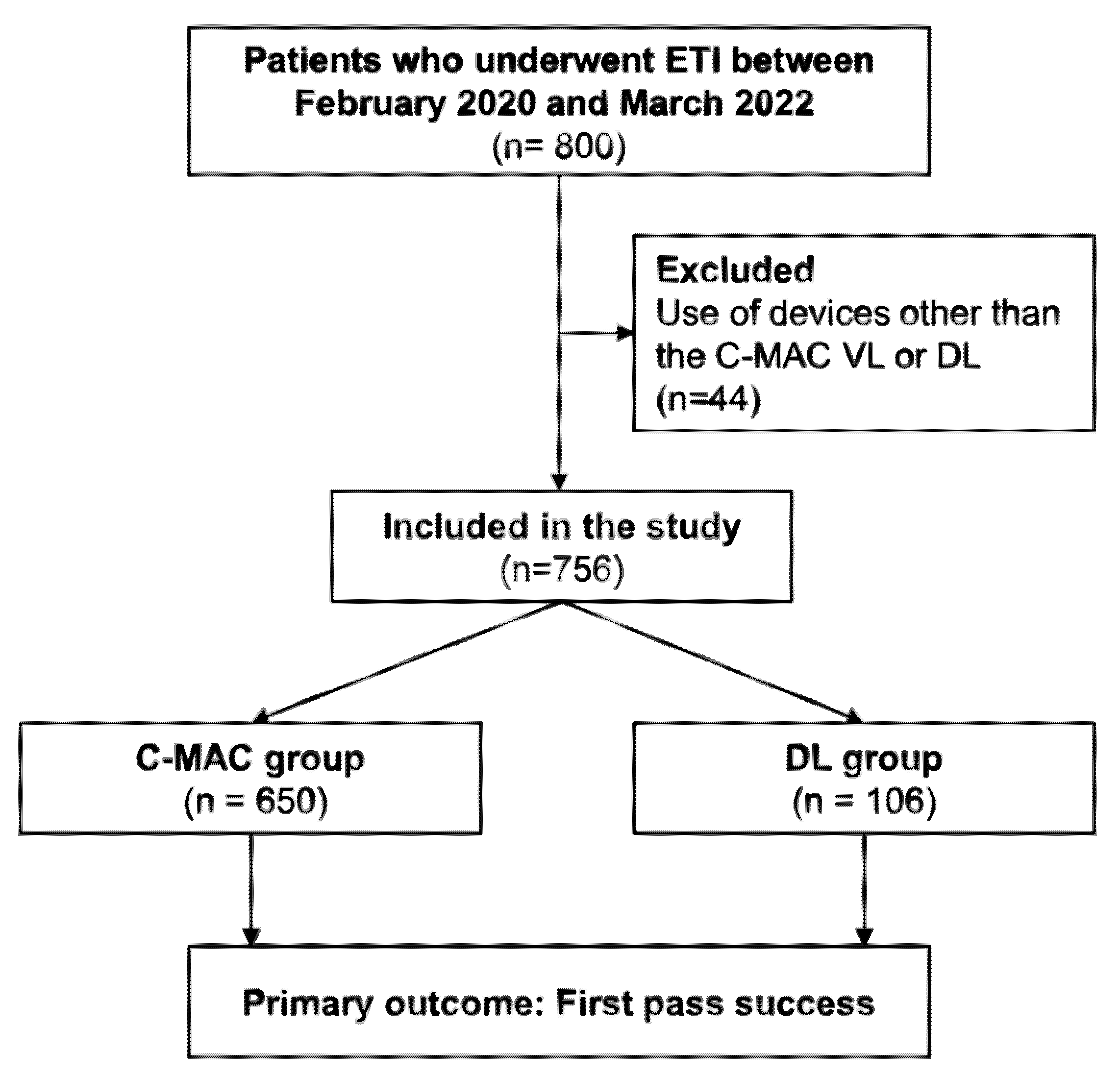
2.2. Study Population
2.3. Data Collection
2.4. Definitions
2.5. Primary and Secondary Outcomes
2.6. Statistical Analysis
3. Results
3.1. Baseline Characteristics of Patients and ETI Procedures
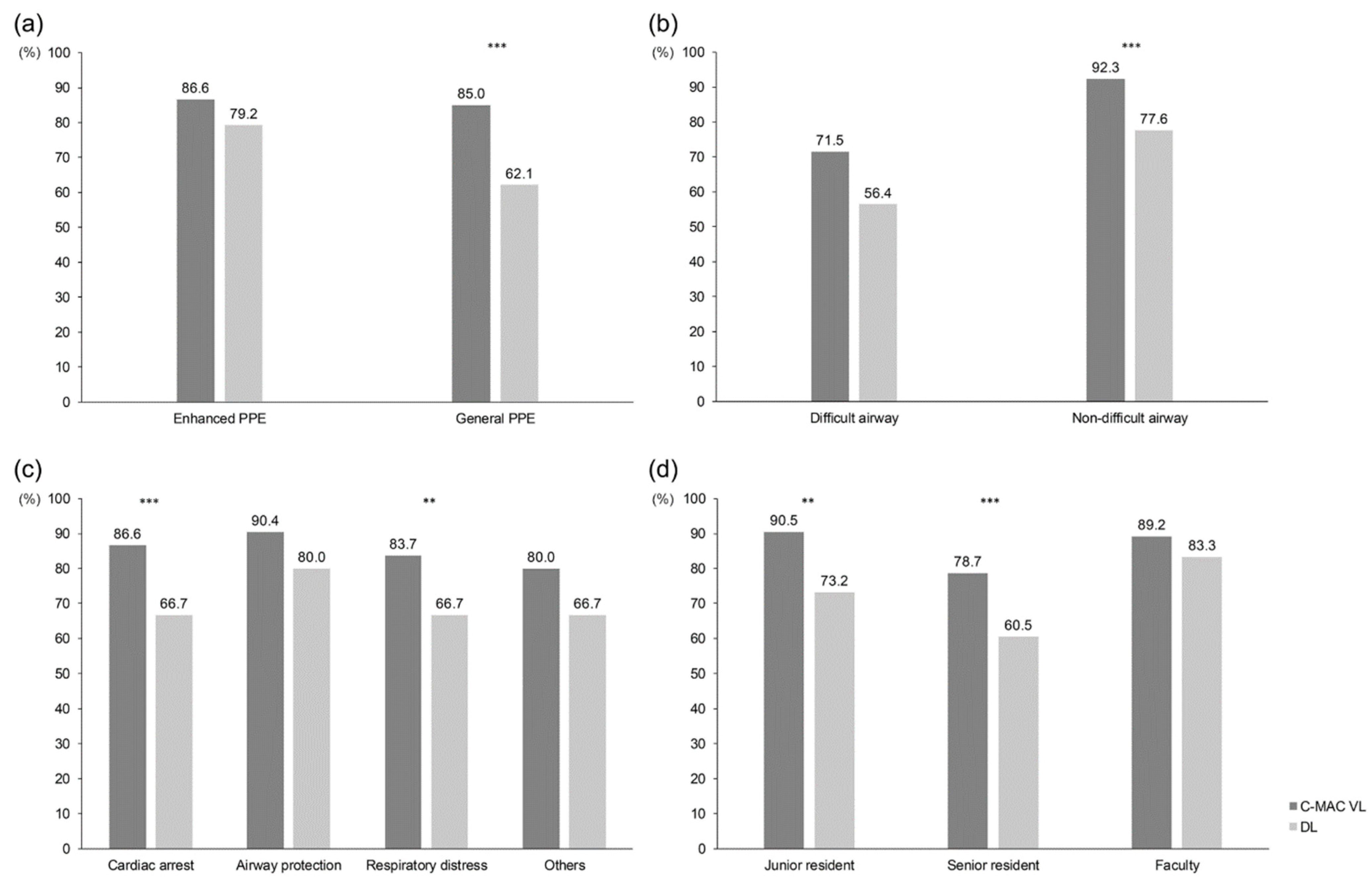
3.2. Primary and Secondary Outcomes
3.3. Multivariable Analysis for Factors Associated with FPS
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A

References
- World Health Organization. WHO Coronavirus (COVID-19) Dashboard. 2022. Available online: https://covid19.who.int (accessed on 1 August 2022).
- Hickey, S.; Mathews, K.S.; Siller, J.; Sueker, J.; Thakore, M.; Ravikumar, D.; E Olmedo, R.; McGreevy, J.; Kohli-Seth, R.; Carr, B.; et al. Rapid deployment of an emergency department-intensive care unit for the COVID-19 pandemic. Clin. Exp. Emerg. Med. 2020, 7, 319–325. [Google Scholar] [CrossRef] [PubMed]
- Ko, H.-Y.; Park, J.-E.; Jeong, D.-U.; Shin, T.-G.; Sim, M.-S.; Jo, I.-J.; Lee, G.-T.; Hwang, S.-Y. Impact of Personal Protective Equipment on Out-of-Hospital Cardiac Arrest Resuscitation in Coronavirus Pandemic. Medicina 2021, 57, 1291. [Google Scholar] [CrossRef] [PubMed]
- Meyerowitz, E.A.; Richterman, A. SARS-CoV-2 Transmission and Prevention in the Era of the Delta Variant. Infect. Dis. Clin. N. Am. 2022, 36, 267–293. [Google Scholar] [CrossRef] [PubMed]
- Leal, J.; Farkas, B.; Mastikhina, L.; Flanagan, J.; Skidmore, B.; Salmon, C.; Dixit, D.; Smith, S.; Tsekrekos, S.; Lee, B.; et al. Risk of transmission of respiratory viruses during aerosol-generating medical procedures (AGMPs) revisited in the COVID-19 pandemic: A systematic review. Antimicrob. Resist. Infect. Control 2022, 11, 102. [Google Scholar] [CrossRef] [PubMed]
- Orser, B.A. Recommendations for Endotracheal Intubation of COVID-19 Patients. Anesth. Analg. 2020, 130, 1109–1110. [Google Scholar] [CrossRef] [PubMed]
- Foley, L.J.; Urdaneta, F.; Berkow, L.; Aziz, M.F.; Baker, P.A.; Jagannathan, N.; Rosenblatt, W.; Straker, T.M.; Wong, D.T.; Hagberg, C.A. Difficult Airway Management in Adult Coronavirus Disease 2019 Patients: Statement by the Society of Airway Management. Anesth. Analg. 2021, 133, 876–890. [Google Scholar] [CrossRef]
- Sanfilippo, F.; Tigano, S.; La Rosa, V.; Morgana, A.; Murabito, P.; Oliveri, F.; Longhini, F.; Astuto, M. Tracheal intubation while wearing personal protective equipment in simulation studies: A systematic review and meta-analysis with trial-sequential analysis. Braz. J. Anesthesiol. 2022, 72, 291–301. [Google Scholar] [CrossRef] [PubMed]
- Gadek, L.; Szarpak, L.; Konge, L.; Dabrowski, M.; Telecka-Gadek, D.; Maslanka, M.; Drela, W.L.; Jachowicz, M.; Iskrzycki, L.; Bialka, S.; et al. Direct vs. Video-Laryngoscopy for Intubation by Paramedics of Simulated COVID-19 Patients under Cardiopulmonary Resuscitation: A Randomized Crossover Trial. J. Clin. Med. 2021, 10, 5740. [Google Scholar] [CrossRef] [PubMed]
- Shin, D.H.; Choi, P.C.; Na, J.U.; Cho, J.H.; Han, S.K. Utility of the Pentax-AWS in performing tracheal intubation while wearing chemical, biological, radiation and nuclear personal protective equipment: A randomised crossover trial using a manikin. Emerg. Med. J. 2013, 30, 527–531. [Google Scholar] [CrossRef] [PubMed]
- Yousif, S.; Machan, J.T.; Alaska, Y.; Suner, S. Airway Management in Disaster Response: A Manikin Study Comparing Direct and Video Laryngoscopy for Endotracheal Intubation by Prehospital Providers in Level C Personal Protective Equipment. Prehospital Disaster Med. 2017, 32, 352–356. [Google Scholar] [CrossRef] [PubMed]
- Goh, Q.; Lie, S.; Tan, Z.; Tan, P.; Ng, S.; Abdullah, H. Time to intubation with McGrath™ videolaryngoscope versus direct laryngoscope in powered air-purifying respirator: A randomised controlled trial. Singap. Med. J. 2021; online ahead of print. [Google Scholar]
- Jeon, J.; Han, C.; Kim, T.; Lee, S. Evolution of Responses to COVID-19 and Epidemiological Characteristics in South Korea. Int. J. Environ. Res. Public Health 2022, 19, 4056. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.; Shin, T.; Park, J.; Lee, G.; Kim, Y.; Lee, S.; Kim, S.; Hwang, N.; Hwang, S. Impact of Personal Protective Equipment on the First-Pass Success of Endotracheal Intubation in the ED: A Propensity-Score-Matching Analysis. J. Clin. Med. 2021, 10, 1060. [Google Scholar] [CrossRef] [PubMed]
- Hwang, S.Y.; Park, J.H.; Yoon, H.; Cha, W.C.; Jo, I.J.; Sim, M.S.; Song, K.J.; Woo, H.J.; Jeong, S.G.; Shin, T.G. Quality Improvement Program Outcomes for Endotracheal Intubation in the Emergency Department. J. Patient Saf. 2018, 14, e83–e88. [Google Scholar] [CrossRef] [PubMed]
- Hansel, J.; Rogers, A.M.; Lewis, S.R.; Cook, T.M.; Smith, A.F. Videolaryngoscopy versus direct laryngoscopy for adults undergoing tracheal intubation. Cochrane Database Syst. Rev. 2022, 4, Cd011136. [Google Scholar] [PubMed]
- De Carvalho, C.C.; da Silva, D.M.; Lemos, V.M.; Dos Santos, T.G.B.; Agra, I.C.; Pinto, G.M.; Ramos, I.B.; Costa, Y.S.C.; Santos Neto, J.M. Videolaryngoscopy vs. direct Macintosh laryngoscopy in tracheal intubation in adults: A ranking systematic review and network meta-analysis. Anaesthesia 2022, 77, 326–338. [Google Scholar] [CrossRef] [PubMed]
- Scott Taylor, R.; Pitzer, M.; Goldman, G.; Czysz, A.; Simunich, T.; Ashurst, J. Comparison of intubation devices in level C personal protective equipment: A cadaveric study. Am. J. Emerg. Med. 2018, 36, 922–925. [Google Scholar] [CrossRef] [PubMed]
| Total (n = 756) | C-MAC Group (n = 650) | DL Group (n = 106) | p-Value | |
|---|---|---|---|---|
| Patient age (years) | 66.1 ± 15.0 | 66.3 ± 15.0 | 65.1 ± 15.2 | 0.445 |
| Patient sex (male) | 475 (62.8) | 413 (63.5) | 62 (58.5) | 0.374 |
| Patient BMI (kg/m2) | 22.8 ± 4.0 | 22.9 ± 4.0 | 22.3 ± 3.9 | 0.102 |
| Patient BMI | 0.194 | |||
| Normal weight (18.5–24.9 kg/m2) | 484 (64.0) | 418 (64.3) | 66 (62.3) | |
| Underweight (<18.5 kg/m2) | 92 (12.2) | 73 (11.2) | 19 (17.9) | |
| Pre-obese (25.0–29.9 kg/m2) | 140 (18.5) | 125 (19.2) | 15 (14.2) | |
| Obese (≥30.0 kg/m2) | 40 (5.3) | 34 (5.2) | 6 (5.7) | |
| PPE level | 0.737 | |||
| General | 425 (56.2) | 367 (56.5) | 58 (54.7) | |
| Enhanced | 331 (43.8) | 283 (43.5) | 48 (45.3) | |
| Anticipated difficult airway | 246 (32.5) | 207 (31.8) | 39 (36.8) | 0.370 |
| Intubation indication | 0.001 | |||
| Cardiac arrest | 279 (36.9) | 231 (35.5) | 48 (45.3) | |
| Airway protection | 129 (17.1) | 104 (16.0) | 25 (23.6) | |
| Respiratory distress | 322 (42.6) | 295 (45.4) | 27 (25.5) | |
| Other | 26 (3.4) | 20 (3.1) | 6 (5.7) | |
| Method for ETI | 0.135 | |||
| Crash approach * | 284 (37.6) | 235 (36.2) | 49 (46.2) | |
| RSI | 395 (52.2) | 348 (53.5) | 47 (44.3) | |
| Other | 77 (10.2) | 67 (10.3) | 10 (9.4) | |
| Level of intubator † | 0.736 | |||
| Junior resident | 296 (39.2) | 258 (39.7) | 38 (35.8) | |
| Senior resident | 383 (50.7) | 327 (50.3) | 56 (52.8) | |
| Faculty | 77 (10.2) | 65 (10.0) | 12 (11.3) | |
| Sedatives (n = 434) | 0.719 | |||
| Ketamine | 117 (27.0) | 106 (27.5) | 11 (22.4) | |
| Etomidate | 289 (66.6) | 253 (65.7) | 36 (73.5) | |
| Other ‡ | 27 (6.2) | 25 (6.5) | 2 (4.1) | |
| NMBAs (n = 404) | 0.768 | |||
| Succinylcholine | 146 (36.1) | 130 (36.6) | 16 (32.7) | |
| Rocuronium | 246 (60.9) | 214 (60.3) | 32 (65.3) | |
| Other § | 12 (3.0) | 11 (3.1) | 1 (2.0) |
| Total (n = 756) | C-MAC Group (n = 650) | DL Group (n = 106) | p-Value | |
|---|---|---|---|---|
| Success rate | ||||
| First-pass success rate | 631 (83.5) | 557 (85.7) | 74 (69.8) | <0.001 |
| Multiple attempts * | 37 (4.9) | 27 (4.2) | 10 (9.4) | 0.036 |
| Glottic view | ||||
| C-L grade III or IV, (%) | 62 (8.2) | 41 (6.3) | 21 (19.8) | <0.001 |
| Complications | ||||
| Any complications | 120 (15.9) | 105 (16.2) | 15 (14.2) | 0.601 |
| Esophageal intubation | 8 (1.1) | 5 (0.8) | 3 (2.8) | 0.054 |
| Unrecognized EI † | 0 (0.0) | 0 (0.0) | 0 (0.0) | - |
| Dental injury | 3 (0.4) | 2 (0.3) | 1 (0.9) | 0.334 |
| Post-intubation hypotension ‡ | 64 (8.5) | 56 (8.6) | 8 (7.5) | 0.714 |
| Post-intubation hypoxemia ‡ | 23 (3.0) | 19 (2.9) | 4 (3.8) | 0.636 |
| Vomiting ‡ | 1 (0.1) | 1 (0.2) | 0 (0.0) | 0.686 |
| Agitation ‡ | 21 (2.8) | 20 (3.1) | 1 (0.9) | 0.215 |
| Cardiac arrest | 14 (1.9) | 13 (2.0) | 1 (0.9) | 0.454 |
| Univariable | Multivariable | |||
|---|---|---|---|---|
| Parameter | OR (95% CI) | p-Value | OR (95% CI) | p-Value |
| Device, C-MAC VL (vs. DL) | 2.58 (1.60–4.11) | <0.001 | 2.81 (1.68–4.71) | <0.001 |
| PPE | ||||
| General PPE | (ref) | (ref) | ||
| Enhanced PPE | 1.30 (0.88–1.93) | 0.185 | 1.25 (0.81–1.93) | 0.312 |
| BMI, kg/m2 | ||||
| Normal weight (18.5–24.9) | ||||
| Underweight (<18.5) | 0.79 (0.44–1.43) | 0.438 | 0.88 0.46–1.70) | 0.703 |
| Pre-obese (25.0–29.9) | 0.52 (0.33–0.82) | 0.005 | 0.60 (0.37–1.00) | 0.050 |
| Obese (≥30.0) | 0.94 (0.38–2.33) | 0.897 | 2.06 (0.78–5.45) | 0.146 |
| Anticipated difficult airway | 0.24 (0.16–0.35) | <0.001 | 0.22 (0.14–0.33) | <0.001 |
| Intubation indication | ||||
| Cardiac arrest | (ref) | (ref) | ||
| Non-cardiac arrest | 1.04 (0.70–1.54) | 0.860 | 1.68 (1.04–2.71) | 0.033 |
| Level of intubator | ||||
| Junior resident (1st, 2nd) | (ref) | (ref) | ||
| Senior resident (3rd, 4th) | 2.26 (1.51–3.43) | <0.001 | 2.29 (1.43–3.66) | 0.001 |
| EM Faculty | 2.34 (1.16–5.24) | 0.025 | 3.43 (1.51–7.77) | 0.003 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, D.S.; Jeong, D.; Park, J.E.; Lee, G.T.; Shin, T.G.; Chang, H.; Kim, T.; Lee, S.U.; Yoon, H.; Cha, W.C.; et al. Endotracheal Intubation Using C-MAC Video Laryngoscope vs. Direct Laryngoscope While Wearing Personal Protective Equipment. J. Pers. Med. 2022, 12, 1720. https://doi.org/10.3390/jpm12101720
Kim DS, Jeong D, Park JE, Lee GT, Shin TG, Chang H, Kim T, Lee SU, Yoon H, Cha WC, et al. Endotracheal Intubation Using C-MAC Video Laryngoscope vs. Direct Laryngoscope While Wearing Personal Protective Equipment. Journal of Personalized Medicine. 2022; 12(10):1720. https://doi.org/10.3390/jpm12101720
Chicago/Turabian StyleKim, Da Saem, Daun Jeong, Jong Eun Park, Gun Tak Lee, Tae Gun Shin, Hansol Chang, Taerim Kim, Se Uk Lee, Hee Yoon, Won Chul Cha, and et al. 2022. "Endotracheal Intubation Using C-MAC Video Laryngoscope vs. Direct Laryngoscope While Wearing Personal Protective Equipment" Journal of Personalized Medicine 12, no. 10: 1720. https://doi.org/10.3390/jpm12101720
APA StyleKim, D. S., Jeong, D., Park, J. E., Lee, G. T., Shin, T. G., Chang, H., Kim, T., Lee, S. U., Yoon, H., Cha, W. C., Sim, Y. J., Park, S. Y., & Hwang, S. Y. (2022). Endotracheal Intubation Using C-MAC Video Laryngoscope vs. Direct Laryngoscope While Wearing Personal Protective Equipment. Journal of Personalized Medicine, 12(10), 1720. https://doi.org/10.3390/jpm12101720






