Endocrine Aspects of ICU-Hospitalized COVID-19 Patients
Abstract
1. Introduction
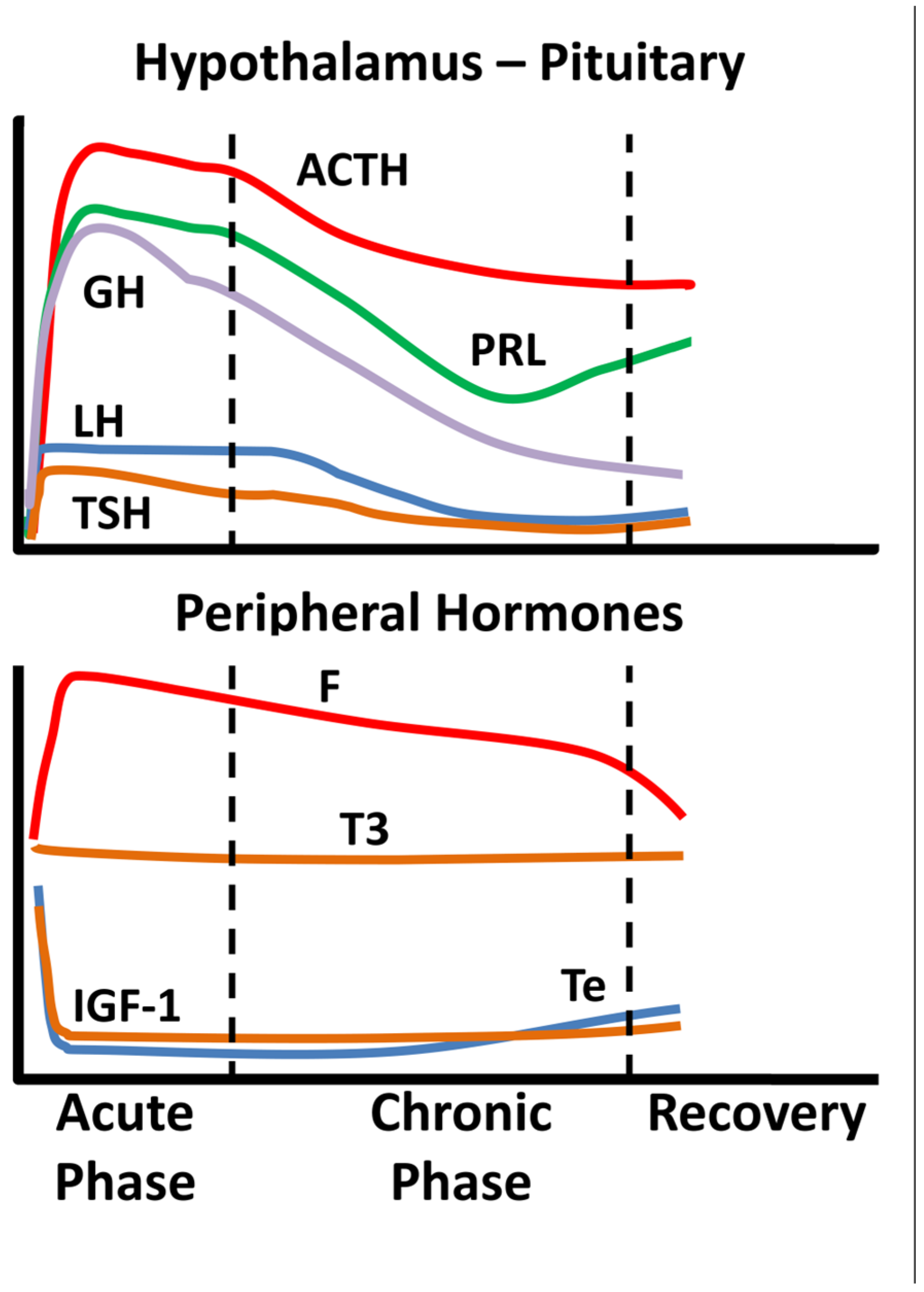
2. Non-COVID-19 Critical Illness
3. Endocrine Aspects of SARS-CoV-1 Infection
4. Endocrine Aspects of SARS-CoV-2 Infection
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Langouche, L.; Van den Berghe, G. Hypothalamic-pituitary hormones during critical illness: A dynamic neuroendocrine response. Handb. Clin. Neurol. 2014, 124, 115–126. [Google Scholar] [CrossRef]
- Mechanick, J.I.; Brett, E.M. Endocrine and metabolic issues in the management of the chronically critically ill patient. Crit. Care Clin. 2002, 18, 619–641, viii. [Google Scholar] [CrossRef]
- Mechanick, J.I.; Nierman, D.M. Gonadal steroids in critical illness. Crit. Care Clin. 2006, 22, 87–103, vii. [Google Scholar] [CrossRef]
- Van den Berghe, G. On the Neuroendocrinopathy of Critical Illness. Perspectives for Feeding and Novel Treatments. Am. J. Respir. Crit. Care Med. 2016, 194, 1337–1348. [Google Scholar] [CrossRef]
- Van den Berghe, G. Adrenal function/dysfunction in critically ill patients: A concise narrative review of recent novel insights. J. Anesth. 2021, 35, 903–910. [Google Scholar] [CrossRef]
- Vassiliou, A.G.; Floros, G.; Jahaj, E.; Stamogiannos, G.; Gennimata, S.; Vassiliadi, D.A.; Tsagarakis, S.; Tzanela, M.; Ilias, I.; Orfanos, S.E.; et al. Decreased glucocorticoid receptor expression during critical illness. Eur. J. Clin. Invest. 2019, 49, e13073. [Google Scholar] [CrossRef]
- Vassiliou, A.G.; Stamogiannos, G.; Jahaj, E.; Botoula, E.; Floros, G.; Vassiliadi, D.A.; Ilias, I.; Tsagarakis, S.; Tzanela, M.; Orfanos, S.E.; et al. Longitudinal evaluation of glucocorticoid receptor alpha/beta expression and signalling, adrenocortical function and cytokines in critically ill steroid-free patients. Mol. Cell. Endocrinol. 2020, 501, 110656. [Google Scholar] [CrossRef]
- Ilias, I. Novel appearance of hyperglycemia/diabetes, associated with COVID-19. World J. Virol 2022, 11, 111–112. [Google Scholar] [CrossRef]
- Marik, P.E.; Bellomo, R. Stress hyperglycemia: An essential survival response! Crit. Care 2013, 17, 305. [Google Scholar] [CrossRef]
- Nylén, E.S.; Seam, N.; Khosla, R. Endocrine markers of severity and prognosis in critical illness. Crit. Care Clin. 2006, 22, 161–179, viii. [Google Scholar] [CrossRef]
- Wang, W.; Ye, Y.; Yao, Z.; Li, H.; Sun, L.; Wang, A.; Wang, Z.; Liu, J.; Li, Z.; Guo, X.; et al. Evaluation and observation of serum throid hormone and parathyroid hormone in patients with severe acute respiratory syndrome. J. Chin. Anti-Tubercul. Assoc. 2003, 25, 232–234. [Google Scholar]
- Wei, L.; Sun, S.; Xu, C.H.; Zhang, J.; Xu, Y.; Zhu, H.; Peh, S.C.; Korteweg, C.; McNutt, M.A.; Gu, J. Pathology of the thyroid in severe acute respiratory syndrome. Hum. Pathol. 2007, 38, 95–102. [Google Scholar] [CrossRef]
- Ye, Y.; Wang, W.; Yao, Z.; Li, H.; Sun, L.; Wang, A.; Wang, Z.; Li, Z.; Guo, X.; Chen, H.; et al. Change in Hormones of Related Sexual Function in Patients with Severe Acute Respiretory Syndrome. Labeled Immunoass. Clin. Med. 2004, 11, 63–65. [Google Scholar]
- Ding, Y.; He, L.; Zhang, Q.; Huang, Z.; Che, X.; Hou, J.; Wang, H.; Shen, H.; Qiu, L.; Li, Z.; et al. Organ distribution of severe acute respiratory syndrome (SARS) associated coronavirus (SARS-CoV) in SARS patients: Implications for pathogenesis and virus transmission pathways. J. Pathol. 2004, 203, 622–630. [Google Scholar] [CrossRef]
- Leow, M.K.; Kwek, D.S.; Ng, A.W.; Ong, K.C.; Kaw, G.J.; Lee, L.S. Hypocortisolism in survivors of severe acute respiratory syndrome (SARS). Clin. Endocrinol. (Oxf.) 2005, 63, 197–202. [Google Scholar] [CrossRef]
- Yang, J.K.; Lin, S.S.; Ji, X.J.; Guo, L.M. Binding of SARS coronavirus to its receptor damages islets and causes acute diabetes. Acta Diabetol. 2010, 47, 193–199. [Google Scholar] [CrossRef]
- Scappaticcio, L.; Maiorino, M.I.; Iorio, S.; Camponovo, C.; Piccardo, A.; Bellastella, G.; Docimo, G.; Esposito, K.; Trimboli, P. Thyroid surgery during the COVID-19 pandemic: Results from a systematic review. J. Endocrinol. Invest. 2022, 45, 181–188. [Google Scholar] [CrossRef]
- Scappaticcio, L.; Pitoia, F.; Esposito, K.; Piccardo, A.; Trimboli, P. Impact of COVID-19 on the thyroid gland: An update. Rev. Endocr. Metab. Disord. 2021, 22, 803–815. [Google Scholar] [CrossRef]
- Speer, G.; Somogyi, P. Thyroid complications of SARS and coronavirus disease 2019 (COVID-19). Endocr. J. 2021, 68, 129–136. [Google Scholar] [CrossRef]
- Bonakdaran, S.; Layegh, P.; Hasani, S.; Afkhamizadeh, M.; Khorasani, Z.M.; Mohebbi, M.; Vojouhi, S.; Mousavi, Z.; Aboutorabi, R.B.; Mehrad-Majd, H.; et al. The Prognostic Role of Metabolic and Endocrine Parameters for the Clinical Severity of COVID-19. Dis. Markers 2022, 2022, 5106342. [Google Scholar] [CrossRef]
- Sparano, C.; Zago, E.; Morettini, A.; Nozzoli, C.; Yannas, D.; Adornato, V.; Caldini, E.; Vaudo, M.; Maggi, M.; Petrone, L. Euthyroid sick syndrome as an early surrogate marker of poor outcome in mild SARS-CoV-2 disease. J. Endocrinol. Invest. 2022, 45, 837–847. [Google Scholar] [CrossRef]
- Beltrão, F.E.L.; Beltrão, D.C.A.; Carvalhal, G.; Brito, A.D.S.; Capistrano, K.; Bastos, I.H.A.; Hecht, F.; Daltro, C.; Bianco, A.C.; Gonçalves, M.; et al. Thyroid Hormone Levels During Hospital Admission Inform Disease Severity and Mortality in COVID-19 Patients. Thyroid 2021, 31, 1639–1649. [Google Scholar] [CrossRef]
- Baldelli, R.; Nicastri, E.; Petrosillo, N.; Marchioni, L.; Gubbiotti, A.; Sperduti, I.; Di Giacinto, P.; Rizza, L.; Rota, F.; Franco, M.; et al. Thyroid dysfunction in COVID-19 patients. J. Endocrinol. Invest. 2021, 44, 2735–2739. [Google Scholar] [CrossRef]
- Campi, I.; Bulgarelli, I.; Dubini, A.; Perego, G.B.; Tortorici, E.; Torlasco, C.; Torresani, E.; Rocco, L.; Persani, L.; Fugazzola, L. The spectrum of thyroid function tests during hospitalization for SARS COV-2 infection. Eur. J. Endocrinol. 2021, 184, 699–709. [Google Scholar] [CrossRef]
- Gong, J.; Wang, D.K.; Dong, H.; Xia, Q.S.; Huang, Z.Y.; Zhao, Y.; Chen, X.; Yuan, F.; Li, J.B.; Lu, F.E. Prognostic significance of low TSH concentration in patients with COVID-19 presenting with non-thyroidal illness syndrome. BMC Endocr. Disord. 2021, 21, 111. [Google Scholar] [CrossRef]
- Muller, I.; Cannavaro, D.; Dazzi, D.; Covelli, D.; Mantovani, G.; Muscatello, A.; Ferrante, E.; Orsi, E.; Resi, V.; Longari, V.; et al. SARS-CoV-2-related atypical thyroiditis. Lancet Diabetes Endocrinol. 2020, 8, 739–741. [Google Scholar] [CrossRef]
- Vassiliadi, D.A.; Ilias, I.; Pratikaki, M.; Jahaj, E.; Vassiliou, A.G.; Detsika, M.; Ampelakiotou, K.; Koulenti, M.; Manolopoulos, K.N.; Tsipilis, S.; et al. Thyroid hormone alterations in critically and non-critically ill patients with SARS-CoV-2 infection. Endocr. Connect. 2021, 10, 646–655. [Google Scholar] [CrossRef]
- Mourouzis, I.; Apostolaki, V.; Trikas, A.; Kokkinos, L.; Alexandrou, N.; Avdikou, M.; Giannoulopoulou, M.; Vassi, A.; Tseti, I.; Pantos, C. The Potential of Thyroid Hormone Therapy in Severe COVID-19: Rationale and Preliminary Evidence. Int J Environ Res. Public Health 2022, 19, 8063. [Google Scholar] [CrossRef]
- Güven, M.; Gültekin, H. Could serum total cortisol level at admission predict mortality due to coronavirus disease 2019 in the intensive care unit? A prospective study. Sao Paulo Med. J. 2021, 139, 398–404. [Google Scholar] [CrossRef]
- Mao, Y.; Xu, B.; Guan, W.; Xu, D.; Li, F.; Ren, R.; Zhu, X.; Gao, Y.; Jiang, L. The Adrenal Cortex, an Underestimated Site of SARS-CoV-2 Infection. Front. Endocrinol. (Lausanne) 2020, 11, 593179. [Google Scholar] [CrossRef]
- Vassiliou, A.G.; Athanasiou, N.; Keskinidou, C.; Jahaj, E.; Tsipilis, S.; Zacharis, A.; Botoula, E.; Diamantopoulos, A.; Ilias, I.; Vassiliadi, D.A.; et al. Increased Glucocorticoid Receptor Alpha Expression and Signaling in Critically Ill Coronavirus Disease 2019 Patients. Crit. Care Med. 2021, 49, 2131–2136. [Google Scholar] [CrossRef]
- Arnold, C.G.; Libby, A.; Vest, A.; Hopkinson, A.; Monte, A.A. Immune mechanisms associated with sex-based differences in severe COVID-19 clinical outcomes. Biol. Sex. Differ. 2022, 13, 7. [Google Scholar] [CrossRef]
- Tokatli, M.R.; Sisti, L.G.; Marziali, E.; Nachira, L.; Rossi, M.F.; Amantea, C.; Moscato, U.; Malorni, W. Hormones and Sex-Specific Medicine in Human Physiopathology. Biomolecules 2022, 12, 413. [Google Scholar] [CrossRef]
- Di Stasi, V.; Rastrelli, G.; Inglese, F.; Beccaria, M.; Garuti, M.; Di Costanzo, D.; Spreafico, F.; Cervi, G.; Greco, G.F.; Pecoriello, A.; et al. Higher testosterone is associated with increased inflammatory markers in women with SARS-CoV-2 pneumonia: Preliminary results from an observational study. J. Endocrinol. Invest. 2022, 45, 639–648. [Google Scholar] [CrossRef]
- Zheng, S.; Zou, Q.; Zhang, D.; Yu, F.; Bao, J.; Lou, B.; Xie, G.; Lin, S.; Wang, R.; Chen, W.; et al. Serum level of testosterone predicts disease severity of male COVID-19 patients and is related to T-cell immune modulation by transcriptome analysis. Clin. Chim. Acta 2022, 524, 132–138. [Google Scholar] [CrossRef]
- Schroeder, M.; Schaumburg, B.; Mueller, Z.; Parplys, A.; Jarczak, D.; Roedl, K.; Nierhaus, A.; de Heer, G.; Grensemann, J.; Schneider, B.; et al. High estradiol and low testosterone levels are associated with critical illness in male but not in female COVID-19 patients: A retrospective cohort study. Emerg. Microbes Infect. 2021, 10, 1807–1818. [Google Scholar] [CrossRef]
- Lanser, L.; Burkert, F.R.; Thommes, L.; Egger, A.; Hoermann, G.; Kaser, S.; Pinggera, G.M.; Anliker, M.; Griesmacher, A.; Weiss, G.; et al. Testosterone Deficiency Is a Risk Factor for Severe COVID-19. Front. Endocrinol. (Lausanne) 2021, 12, 694083. [Google Scholar] [CrossRef]
- Salonia, A.; Pontillo, M.; Capogrosso, P.; Gregori, S.; Tassara, M.; Boeri, L.; Carenzi, C.; Abbate, C.; Cignoli, D.; Ferrara, A.M.; et al. Severely low testosterone in males with COVID-19: A case-control study. Andrology 2021, 9, 1043–1052. [Google Scholar] [CrossRef]
- Ilias, I.; Pratikaki, M.; Diamantopoulos, A.; Jahaj, E.; Mourelatos, P.; Athanasiou, N.; Tsipilis, S.; Zacharis, A.; Vassiliou, A.G.; Vassiliadi, D.A.; et al. Testosterone, free, bioavailable and total, in patients with COVID-19. Minerva Endocrinol. (Torino) 2022, 47, 111–116. [Google Scholar] [CrossRef]
- Hazrati, E.; Gholami, M.; Farahani, R.H.; Ghorban, K.; Ghayomzadeh, M.; Rouzbahani, N.H. The effect of IGF-1 plasma concentration on COVID-19 severity. Microb. Pathog. 2022, 164, 105416. [Google Scholar] [CrossRef]
- Ilias, I.; Diamantopoulos, A.; Botoula, E.; Athanasiou, N.; Zacharis, A.; Tsipilis, S.; Jahaj, E.; Vassiliou, A.G.; Vassiliadi, D.A.; Kotanidou, A.; et al. COVID-19 and Growth Hormone/Insulin-Like Growth Factor 1: Study in Critically and Non-Critically Ill Patients. Front. Endocrinol. (Lausanne) 2021, 12, 644055. [Google Scholar] [CrossRef]
- Herrera-Quintana, L.; Gamarra-Morales, Y.; Vázquez-Lorente, H.; Molina-López, J.; Castaño-Pérez, J.; Machado-Casas, J.F.; Coca-Zúñiga, R.; Pérez-Villares, J.M.; Planells, E. Bad Prognosis in Critical Ill Patients with COVID-19 during Short-Term ICU Stay regarding Vitamin D Levels. Nutrients 2021, 13, 1988. [Google Scholar] [CrossRef]
- Campi, I.; Gennari, L.; Merlotti, D.; Mingiano, C.; Frosali, A.; Giovanelli, L.; Torlasco, C.; Pengo, M.F.; Heilbron, F.; Soranna, D.; et al. Vitamin D and COVID-19 severity and related mortality: A prospective study in Italy. BMC Infect. Dis. 2021, 21, 566. [Google Scholar] [CrossRef]
- Chiodini, I.; Gatti, D.; Soranna, D.; Merlotti, D.; Mingiano, C.; Fassio, A.; Adami, G.; Falchetti, A.; Eller-Vainicher, C.; Rossini, M.; et al. Vitamin D Status and SARS-CoV-2 Infection and COVID-19 Clinical Outcomes. Front. Public Health 2021, 9, 736665. [Google Scholar] [CrossRef]
- Hurst, E.A.; Mellanby, R.J.; Handel, I.; Griffith, D.M.; Rossi, A.G.; Walsh, T.S.; Shankar-Hari, M.; Dunning, J.; Homer, N.Z.; Denham, S.G.; et al. Vitamin D insufficiency in COVID-19 and influenza A, and critical illness survivors: A cross-sectional study. BMJ Open 2021, 11, e055435. [Google Scholar] [CrossRef]
- Chen, J.; Mei, K.; Xie, L.; Yuan, P.; Ma, J.; Yu, P.; Zhu, W.; Zheng, C.; Liu, X. Low vitamin D levels do not aggravate COVID-19 risk or death, and vitamin D supplementation does not improve outcomes in hospitalized patients with COVID-19: A meta-analysis and GRADE assessment of cohort studies and RCTs. Nutr. J. 2021, 20, 89. [Google Scholar] [CrossRef]
- Jevalikar, G.; Mithal, A.; Singh, A.; Sharma, R.; Farooqui, K.J.; Mahendru, S.; Dewan, A.; Budhiraja, S. Lack of association of baseline 25-hydroxyvitamin D levels with disease severity and mortality in Indian patients hospitalized for COVID-19. Sci. Rep. 2021, 11, 6258. [Google Scholar] [CrossRef]
- Butler-Laporte, G.; Nakanishi, T.; Mooser, V.; Morrison, D.R.; Abdullah, T.; Adeleye, O.; Mamlouk, N.; Kimchi, N.; Afrasiabi, Z.; Rezk, N.; et al. Vitamin D and COVID-19 susceptibility and severity in the COVID-19 Host Genetics Initiative: A Mendelian randomization study. PLoS Med. 2021, 18, e1003605. [Google Scholar] [CrossRef]
- Martineau, A.R.; Cantorna, M.T. Vitamin D for COVID-19: Where are we now? Nat. Rev. Immunol. 2022. [CrossRef]
- Quesada-Gomez, J.M.; Lopez-Miranda, J.; Entrenas-Castillo, M.; Casado-Díaz, A.; Nogues, Y.S.X.; Mansur, J.L.; Bouillon, R. Vitamin D Endocrine System and COVID-19: Treatment with Calcifediol. Nutrients 2022, 14, 2716. [Google Scholar] [CrossRef]
- Cromer, S.J.; Colling, C.; Schatoff, D.; Leary, M.; Stamou, M.I.; Selen, D.J.; Putman, M.S.; Wexler, D.J. Newly diagnosed diabetes vs. pre-existing diabetes upon admission for COVID-19: Associated factors, short-term outcomes, and long-term glycemic phenotypes. J. Diabetes Its Complicat. 2022, 36, 108145. [Google Scholar] [CrossRef]
- Ilias, I.; Diamantopoulos, A.; Pratikaki, M.; Botoula, E.; Jahaj, E.; Athanasiou, N.; Tsipilis, S.; Zacharis, A.; Vassiliou, A.G.; Vassiliadi, D.A.; et al. Glycemia, Beta-Cell Function and Sensitivity to Insulin in Mildly to Critically Ill COVID-19 Patients. Medicina (Kaunas) 2021, 57, 68. [Google Scholar] [CrossRef]
- Rubino, F.; Amiel, S.A.; Zimmet, P.; Alberti, G.; Bornstein, S.; Eckel, R.H.; Mingrone, G.; Boehm, B.; Cooper, M.E.; Chai, Z.; et al. New-Onset Diabetes in COVID-19. N. Engl. J. Med. 2020, 383, 789–790. [Google Scholar] [CrossRef]
- Battaglini, D.; Lopes-Pacheco, M.; Castro-Faria-Neto, H.C.; Pelosi, P.; Rocco, P.R.M. Laboratory Biomarkers for Diagnosis and Prognosis in COVID-19. Front. Immunol. 2022, 13, 857573. [Google Scholar] [CrossRef]
| Affected Axis | |
|---|---|
| Hypothalamic–pituitary–thyroid | Low TSH, low T3 [11]; Extensive thyroid gland damage [12]; Diminished pituitary staining for TSH [13] |
| Hypothalamic–pituitary–growth | Diminished pituitary staining for GH [13] |
| Hypothalamic–pituitary–adrenal | Low F [11]; Diminished pituitary staining for ACTH [13] |
| Hypothalamic–pituitary–gonadal | Low E2 [11]; Elevated FSH, elevated LH [11]; Increased pituitary staining for FSH, LH [13] |
| Hypothalamo-prolactin | Elevated PRL [11]; Increased pituitary staining for PRL [13] |
| Glucose-insulin | Acute onset transient diabetes/hyperglycemia [16] |
| Affected Axis | |
|---|---|
| Hypothalamic–pituitary–thyroid | Low T3 or free T3, low free T4 and low TSH [20,21,22,23,24,25]; NTIS or Thyrotoxicosis [27] |
| Hypothalamic–pituitary–growth | Low IGF-1 [40,41]; Low IGF-1 and low GH associated with worse prognosis [41] |
| Hypothalamic–pituitary–adrenal | High [29] or low F [30] |
| Hypothalamic–pituitary–gonadal | In women with high Te: worse prognosis [34]; In men: high total Te [35] or lower Te than control patients [36,37,38]; low free Te and bioavailable Te [39], high E2 [36] |
| Glucose-insulin | Acute onset transient diabetes/hyperglycemia [51]; Impaired beta cell function [52] |
| Vitamin D | Low (OH)25-vitamin-D3 [42,43,44,45] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Diamantopoulos, A.; Dimopoulou, I.; Mourelatos, P.; Vassiliou, A.G.; Vassiliadi, D.-A.; Kotanidou, A.; Ilias, I. Endocrine Aspects of ICU-Hospitalized COVID-19 Patients. J. Pers. Med. 2022, 12, 1703. https://doi.org/10.3390/jpm12101703
Diamantopoulos A, Dimopoulou I, Mourelatos P, Vassiliou AG, Vassiliadi D-A, Kotanidou A, Ilias I. Endocrine Aspects of ICU-Hospitalized COVID-19 Patients. Journal of Personalized Medicine. 2022; 12(10):1703. https://doi.org/10.3390/jpm12101703
Chicago/Turabian StyleDiamantopoulos, Aristidis, Ioanna Dimopoulou, Panagiotis Mourelatos, Alice G Vassiliou, Dimitra-Argyro Vassiliadi, Anastasia Kotanidou, and Ioannis Ilias. 2022. "Endocrine Aspects of ICU-Hospitalized COVID-19 Patients" Journal of Personalized Medicine 12, no. 10: 1703. https://doi.org/10.3390/jpm12101703
APA StyleDiamantopoulos, A., Dimopoulou, I., Mourelatos, P., Vassiliou, A. G., Vassiliadi, D.-A., Kotanidou, A., & Ilias, I. (2022). Endocrine Aspects of ICU-Hospitalized COVID-19 Patients. Journal of Personalized Medicine, 12(10), 1703. https://doi.org/10.3390/jpm12101703








