Body Image and Body Mass Index Influence on Psychophysical Well-Being in Bariatric Patients: A Cross-Sectional Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Procedures
2.2. Measures
2.3. Statistical Analyses
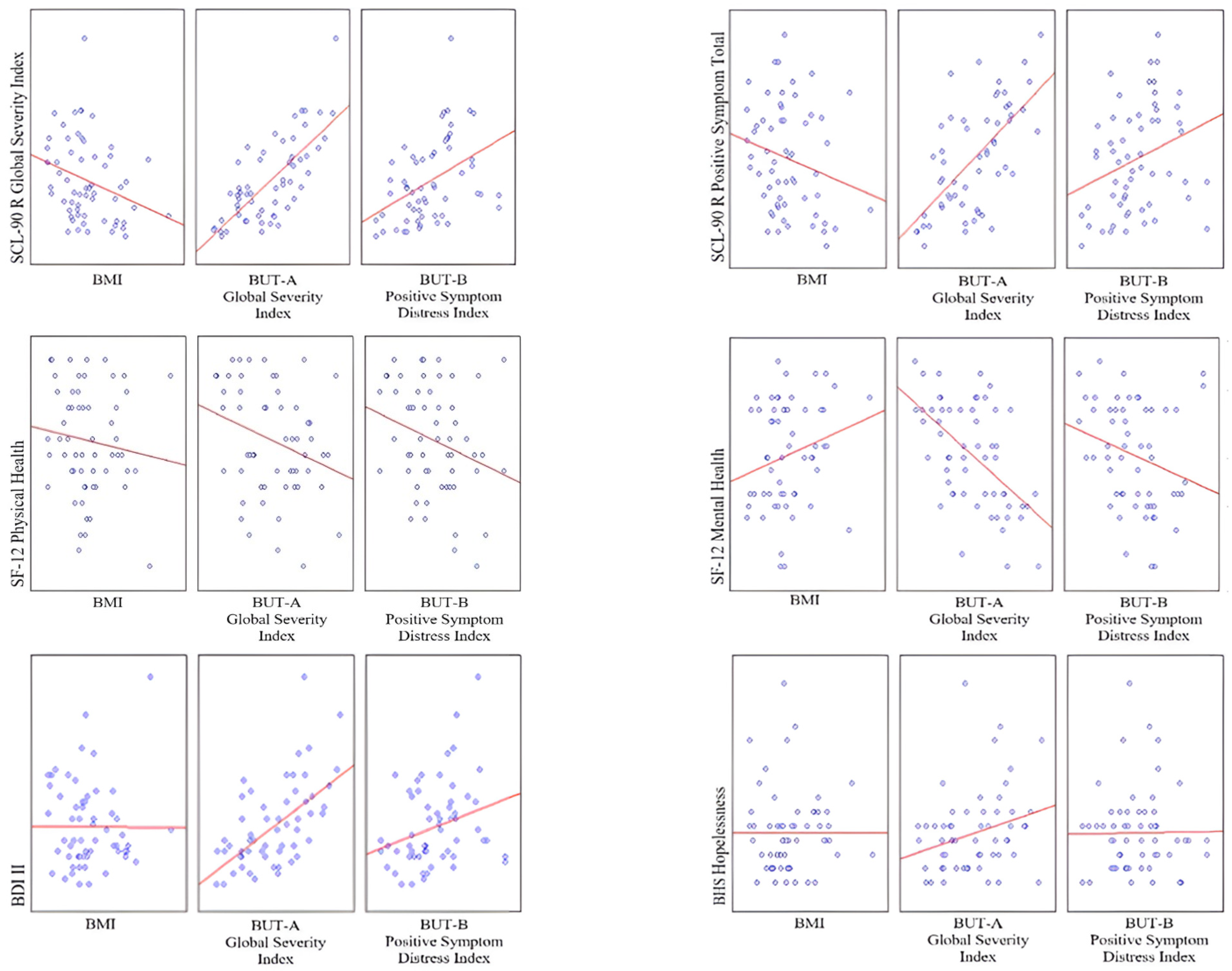
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- De Luca, M.; Angrisani, L.; Himpens, J.; Busetto, L.; Scopinaro, N.; Weiner, R.; Sartori, A.; Stier, C.; Lakdawala, M.; Bhasker, A.G.; et al. Indications for Surgery for Obesity and Weight-Related Diseases: Position Statements from the International Federation for the Surgery of Obesity and Metabolic Disorders (IFSO). Obes. Surg. 2016, 26, 1659–1696. [Google Scholar] [CrossRef] [PubMed]
- Di Lorenzo, N.; Antoniou, S.A.; Batterham, R.L.; Busetto, L.; Godoroja, D.; Iossa, A.; Carrano, F.M.; Agresta, F.; Alarçon, I.; Azran, C.; et al. Clinical practice guidelines of the European Association for Endoscopic Surgery (EAES) on bariatric surgery: Update 2020 endorsed by IFSO-EC, EASO and ESPCOP. Surg. Endosc. 2020, 34, 2332–2358. [Google Scholar] [CrossRef] [PubMed]
- Husky, M.M.; Mazure, C.M.; Ruffault, A.; Flahault, C.; Kovess-Masfety, V. Differential Associations Between Excess Body Weight and Psychiatric Disorders in Men and Women. J. Women’s Health 2018, 27, 183–190. [Google Scholar] [CrossRef] [PubMed]
- Lai, C.; Aceto, P.; Santucci, F.R.; Pierro, L.; Petrucci, I.; Cacioppo, M.; Castelnuovo, G.; Sollazzi, L.; Bellantone, R.; Raffaelli, M. Preoperative psychological characteristics affecting mid-term outcome after bariatric surgery: A follow-up study. EWD 2021, 26, 585–590. [Google Scholar] [CrossRef] [PubMed]
- Cohn, I.; Raman, J.; Sui, Z. Patient motivations and expectations prior to bariatric surgery: A qualitative systematic review. Obes. Rev. 2019, 20, 1608–1618. [Google Scholar] [CrossRef] [PubMed]
- Wilson, R.E.; Latner, J.D.; Hayashi, K. More than just body weight: The role of body image in psychological and physical functioning. Body Image 2013, 10, 644–647. [Google Scholar] [CrossRef] [PubMed]
- Spirou, D.; Raman, J.; Smith, E. Psychological outcomes following surgical and endoscopic bariatric procedures: A systematic review. Obes. Rev. 2020, 21, e12998. [Google Scholar] [CrossRef]
- Szmulewicz, A.; Wanis, K.N.; Gripper, A.; Angriman, F.; Hawel, J.; Elnahas, A.; Alkhamesi, N.A.; Schlachta, C.M. Mental health quality of life after bariatric surgery: A systematic review and meta-analysis of randomized clinical trials. Clin. Obes. 2019, 9, e12290. [Google Scholar] [CrossRef]
- Monpellier, V.M.; Antoniou, E.E.; Aarts, E.O.; Janssen, I.M.C.; Jansen, A.T.M. Improvement of Health-Related Quality of Life After Roux-en-Y Gastric Bypass Related to Weight Loss. Obes. Surg. 2017, 27, 1168–1173. [Google Scholar] [CrossRef] [PubMed]
- Cash, T.F.; Pruzinsky, T. Body Images: Development, Deviance, and Change; Guilford: New York, NY, USA, 1990. [Google Scholar]
- Watson, C.; Riazi, A.; Ratcliffe, D. Exploring the Experiences of Women Who Develop Restrictive Eating Behaviours after Bariatric Surgery. Obes. Surg. 2020, 30, 2131–2139. [Google Scholar] [CrossRef]
- Sarwer, D.B.; Wadden, T.A.; Moore, R.H.; Eisenberg, M.H.; Raper, S.E.; Williams, N.N. Changes in quality of life and body image after gastric bypass surgery. Surg. Obes. Relat. Dis. 2010, 6, 608–614. [Google Scholar] [CrossRef] [PubMed]
- Song, P.; Patel, N.B.; Gunther, S.; Li, C.S.; Liu, Y.; Lee, C.Y.; Kludt, N.A.; Patel, K.B.; Ali, M.R.; Wong, M.S. Body Image & Quality of Life: Changes with Gastric Bypass and Body Contouring. Ann. Plast. Surg. 2016, 76, S216–S221. [Google Scholar] [PubMed]
- Perdue, T.O.; Schreier, A.; Neil, J.; Carels, R.; Swanson, M. A Concept Analysis of Disturbed Body Image in Bariatric Surgery Patients. Int. J. Nurs. Knowl. 2020, 31, 74–81. [Google Scholar] [CrossRef] [PubMed]
- Felske, A.N.; Williamson, T.M.; Scurrey, S.R.M.; Telfer, J.A.; Campbell, T.S.; Rash, J.A. The Influence of Weight-Related Self-Esteem and Symptoms of Depression on Shape and Weight Concerns and Weight-Loss 12 Months After Bariatric Surgery. Obes. Surg. 2021, 31, 1062–1072. [Google Scholar] [CrossRef] [PubMed]
- de Meireles, A.J.; Carlin, A.M.; Bonham, A.J.; Cassidy, R.; Ross, R.; Stricklen, A.; Finks, J.; Ghaferi, A.A. A Longitudinal Analysis of Variation in Psychological Well-being and Body Image in Patients Before and After Bariatric Surgery. Ann. Surg. 2020, 271, 885–890. [Google Scholar] [CrossRef]
- Mento, C.; Silvestri, M.C.; Muscatello, M.; Rizzo, A.; Celebre, L.; Cedro, C.; Zoccali, R.A.; Navarra, G.; Bruno, A. The role of body image in obese identity changes post bariatric surgery. Eat. Weight Disord. 2022, 27, 1269–1278. [Google Scholar] [CrossRef]
- Chen, E.Y.; Fettich, K.C.; Tierney, M.; Cummings, H.; Berona, J.; Weissman, J.; Ward, A.; Christensen, K.; Southward, M.; Gordon, K.H.; et al. Factors associated with suicide ideation in severely obese bariatric surgery-seeking individuals. Suicide Life-Threat. Behav. 2012, 42, 541–549. [Google Scholar] [CrossRef]
- Gaudrat, B.; Andrieux, S.; Florent, V.; Rousseau, A. Psychological characteristics of patients seeking bariatric treatment versus those seeking medical treatment for obesity: Is bariatric surgery a last best hope? Eat. Weight Disord. 2021, 26, 949–961. [Google Scholar] [CrossRef]
- Derogatis, L.R.; Lipman, R.S.; Covi, L. SCL-90: An outpatient psychiatric rating scale—Preliminary report. Psychopharmacol. Bull. 1973, 9, 13–28. [Google Scholar]
- Prunas, A.; Sarno, I.; Preti, E.; Madeddu, F.; Perugini, M. Psychometric properties of the Italian version of the SCL-90-R: A study on a large community sample. Eur. Psychiatry 2012, 27, 591–597. [Google Scholar] [CrossRef]
- Cuzzolaro, M.; Vetrone, G.; Marano, G.; Garfinkel, P.E. The Body Uneasiness Test (BUT): Development and validation of a new body image assessment scale. Eat. Weight Disord. 2006, 11, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Ware, J., Jr.; Kosinski, M.; Keller, S.D. A 12-Item Short-Form Health Survey: Construction of scales and preliminary tests of reliability and validity. Med. Care 1996, 34, 220–233. [Google Scholar] [CrossRef]
- Apolone, G.; Mosconi, P. The Italian SF-36 Health Survey: Translation, validation and norming. J. Clin. Epidemiol. 1998, 51, 1025–1036. [Google Scholar] [CrossRef]
- Beck, A.T.; Steer, R.A.; Ball, R.; Ranieri, W. Comparison of Beck Depression Inventories-IA and -II in psychiatric outpatients. J. Personal. Assess. 1996, 67, 588–597. [Google Scholar] [CrossRef] [PubMed]
- Sica, C.; Ghisi, M. The Italian versions of the Beck Anxiety Inventory and the Beck Depression Inventory-II: Psychometric properties and discriminant power. In Leading-Edge Psychological Tests and Testing Research; Lange, M.A., Ed.; Nova Science Publishers: New York, NY, USA, 2007; pp. 27–50. [Google Scholar]
- Beck, A.T.; Weissman, A.; Lester, D.; Trexler, L. The measurement of pessimism: The hopelessness scale. J. Consult. Clin. Psychol. 1974, 42, 861–865. [Google Scholar] [CrossRef] [PubMed]
- Pompili, M.; Iliceto, P.; Lester, D.; Innamorati, M.; Girardi, P.; Tatarelli, R. BHS Beck Hopelessness Scale: Manuale; Giunti, O.S., Ed.; Organizzazioni Speciali: Firenze, Italy, 2009. [Google Scholar]
- Faul, F.; Erdfelder, E.; Lang, A.G.; Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef]
- Bennett, B.L.; Grilo, C.M.; Alperovich, M.; Ivezaj, V. Body Image Concerns and Associated Impairment Among Adults Seeking Body Contouring Following Bariatric Surgery. Aesthet. Surg. J. 2022, 42, 275–282. [Google Scholar] [CrossRef]
- Rosner, B. Fundamentals of Biostatistics, 7th ed.; Brooks/Cole: Boston, MA, USA, 2011. [Google Scholar]
- Dotse, J. Relationship between body image satisfaction and psychological well-being: The impact of Africentric values. J. Soc. Sci. Stud. 2015, 2, 320–342. [Google Scholar] [CrossRef]
- Geller, S.; Dahan, S.; Levy, S.; Goldzweig, G.; Hamdan, S.; Abu-Abeid, S. Body Image and Emotional Eating as Predictors of Psychological Distress Following Bariatric Surgery. Obes. Surg. 2020, 30, 1417–1423. [Google Scholar] [CrossRef]
- Abilés, V.; Rodríguez-Ruiz, S.; Abilés, J.; Mellado, C.; García, A.; Pérez de la Cruz, A.; Fernández-Santaella, M.C. Psychological characteristics of morbidly obese candidates for bariatric surgery. Obes. Surg. 2010, 20, 161–167. [Google Scholar] [CrossRef]
- Kubik, J.F.; Gill, R.S.; Laffin, M.; Karmali, S. The impact of bariatric surgery on psychological health. J. Obes. 2013, 2013, 837989. [Google Scholar] [CrossRef]
- Cash, T.F. Body image: Past, present, and future. Body Image 2004, 1, 1–5. [Google Scholar] [CrossRef]
- Cuzzolaro, M.; Fassino, S. Body Image, Eating, and Weight, 1st ed.; Springer: Cham, Switzerland, 2018. [Google Scholar]
- Latner, J.D.; Wilson, R.E. Obesity and body image in adulthood. In Body Image: A Handbook of Science, Practice, and Prevention; Cash, T.F., Smolak, L., Eds.; The Guilford Press: New York, NY, USA, 2011; pp. 189–197. [Google Scholar]
- Wang, R.; Wu, M.J.; Ma, X.Q.; Zhao, Y.F.; Yan, X.Y.; Gao, Q.B.; He, J. Body mass index and health-related quality of life in adults: A population based study in five cities of China. Eur. J. Public Health 2012, 22, 497–502. [Google Scholar] [CrossRef] [PubMed]
- Audureau, E.; Pouchot, J.; Coste, J. Gender-Related Differential Effects of Obesity on Health-Related Quality of Life via Obesity-Related Comorbidities: A Mediation Analysis of a French Nationwide Survey. Circ. Cardiovasc. Qual. Outcomes 2016, 9, 246–256. [Google Scholar] [CrossRef]
| Mean | SD | N(%) (n = 59) | |
|---|---|---|---|
| Weight | 115.62 | 22.89 | |
| BMI baseline Class I (30.0–34.9) Class II (35.0–39.9) Class III (>40.0) | 41.96 | 5.38 | 6(10.2%) 15(25.4%) 38(64.4%) |
| Education Primary School Secondary School University | 35(59.3%) 17(28.9%) 7(11.8%) | ||
| Work Student Employed Unemployed Retired | 4(6.9%) 28(47.3%) 26(44.1%) 1(1.7%) | ||
| Marital Status Single Married Separated Widowed | 20(33.9%) 32(54.2%) 6(10.2%) 1(1.7%) | ||
| SCL-90-R SCL- 90-R GSI SCL-90-R PST | 66.06 60.48 | 17.80 12.37 | |
| BUT-A BUT-A GSI BUT-A Weight Phobia BUT-A Body Image Concern BUT-A Avoidance BUT-A Compulsive Self-monitoring BUT-A Depersonalisation | 1.86 2.32 2.85 1.36 1.00 1.40 | 1.07 1.25 1.29 1.22 0.84 1.29 | |
| BUT-B BUT-B PST BUT-PSDI | 14.12 2.75 | 8.91 0.95 | |
| SF-12 Total Physical Health Mental Health | 33.20 13.93 19.27 | 6.63 3.37 4.34 | |
| BDI II | 10.59 | 7.72 | |
| BHS | 3.54 | 2.86 |
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 | 21 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Gender | — | ||||||||||||||||||||
| 2. Weight | −0.75 *** | — | |||||||||||||||||||
| 3. BMI | −0.56 *** | 0.85 *** | — | ||||||||||||||||||
| 4. Marital Status | −0.00 | 0.03 | 0.10 | — | |||||||||||||||||
| 5. Work | 0.19 | −0.14 | −0.10 | −0.20 | — | ||||||||||||||||
| 6. Education | 0.35 ** | −0.34 ** | −0.40 ** | −0.40 *** | 0.09 | — | |||||||||||||||
| 7. BUT-A GSI | 0.12 | −0.11 | −0.16 | 0.17 | −0.17 | 0.08 | — | ||||||||||||||
| 8. BUT-A Weight Phobia | 0.09 | −0.16 | −0.19 | 0.13 | −0.08 | 0.00 | 0.91 *** | — | |||||||||||||
| 9. BUT-A Body Image Concern | 0.08 | −0.01 | −0.09 | 0.17 | −0.12 | 0.07 | 0.92 *** | 0.84 *** | — | ||||||||||||
| 10. BUT-A Avoidance | 0.08 | −0.02 | −0.06 | 0.05 | −0.18 | 0.09 | 0.84 *** | 0.65 *** | 0.71 *** | — | |||||||||||
| 11. BUT-A Compulsive Self-monitoring | 0.07 | −0.23 | −0.28 * | 0.14 | −0.13 | 0.15 | 0.73 *** | 0.68 *** | 0.57 *** | 0.49 *** | — | ||||||||||
| 12. BUT-A Depersonalisation | 0.20 | −0.14 | −0.15 | 0.23 | −0.30 * | 0.07 | 0.83 *** | 0.63 *** | 0.67 *** | 0.76 *** | 0.56 *** | — | |||||||||
| 13. BUT-B PST | 0.16 | −0.11 | −0.16 | −0.15 | −0.05 | 0.26 * | 0.54 *** | 0.42 *** | 0.45 *** | 0.53 *** | 0.48 *** | 0.51 *** | — | ||||||||
| 14. BUT-B PSDI | 0.05 | −0.01 | 0.04 | 0.18 | −0.08 | −0.07 | 0.56 *** | 0.53 *** | 0.57 *** | 0.41 *** | 0.39 ** | 0.41 *** | 0.203 | — | |||||||
| 15. SCL−90-R GSI | 0.18 | −0.19 | −0.29 * | 0.07 | −0.15 | 0.06 | 0.73 *** | 0.63 *** | 0.59 *** | 0.73 *** | 0.53 *** | 0.70 *** | 0.611 *** | 0.42 *** | — | ||||||
| 16. SCL−90R PST | 0.15 | −0.08 | −0.21 | 0.10 | −0.20 | 0.00 | 0.65 *** | 0.56 *** | 0.52 *** | 0.65 *** | 0.42 *** | 0.64 *** | 0.565 *** | 0.29 * | 0.92 *** | — | |||||
| 17. SF−12 Physical Health | −0.10 | −0.00 | −0.12 | −0.14 | −0.03 | 0.13 | −0.29 * | −0.23 | −0.25 | −0.31 * | −0.26 * | −0.20 | −0.176 | −0.27 * | −0.39 ** | −0.44 *** | — | ||||
| 18. SF−12 Mental Health | −0.27 * | 0.22 | 0.23 | −0.03 | −0.01 | −0.10 | −0.56 *** | −0.48 *** | −0.45 *** | −0.63 *** | −0.34 ** | −0.48 *** | −0.548 *** | −0.26 * | −0.69 *** | −0.65 *** | 0.47 *** | — | |||
| 19. SF−12 Total Score | −0.23 | 0.14 | 0.09 | −0.09 | −0.02 | −0.00 | −0.51 *** | −0.43 *** | −0.42 *** | −0.57 *** | −0.35 ** | −0.42 *** | −0.448 *** | −0.30 * | −0.65 *** | −0.65 *** | 0.82 *** | 0.89 *** | — | ||
| 20. BDI II | 0.16 | 0.01 | −0.00 | 0.24 | −0.14 | −0.09 | 0.58 *** | 0.46 *** | 0.49 *** | 0.61 *** | 0.41 *** | 0.57 *** | 0.398 ** | 0.28 * | 0.67 *** | 0.65 *** | −0.49 *** | −0.64 *** | −0.67 *** | — | |
| 21. BHS | −0.09 | 0.05 | 0.00 | 0.02 | −0.04 | −0.14 | 0.27 * | 0.23 | 0.22 | 0.39 ** | 0.07 | 0.23 | −0.020 | 0.01 | 0.38 ** | 0.39 ** | −0.20 | −0.38 ** | −0.35 ** | 0.38 ** | — |
| Outcome: SCL-90 R GSI | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Step 1 | Step 2 | ||||||||
| B | β | p | B | β | p | ||||
| Independent Variables | BMI | −0.030 | −0.288 | 0.027 | −0.018 | −0.180 | 0.053 | ||
| BUT-A GSI | 0.361 | 0.673 | <0.001 | ||||||
| BUT-B PSDI | 0.031 | 0.054 | 0.623 | ||||||
| Model | R | 0.288 | 0.754 | ||||||
| Summary | R2 | 0.083 | 0.568 | ||||||
| Adjusted R2 | 0.067 | 0.544 | |||||||
| F | 5.15 | 24.08 | |||||||
| Sig. of the model | 0.027 | <0.001 | |||||||
| F2 | 0.090 | 1.314 | |||||||
| R2 change | 0.485 | ||||||||
| Outcome: SCL-90 R PST | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Step 1 | Step 2 | ||||||||
| B | β | p | B | β | p | ||||
| Independent Variables | BMI | −0.766 | −0.215 | 0.101 | −0.363 | −0.102 | 0.332 | ||
| BUT-A GSI | 12.551 | 0.675 | <0.001 | ||||||
| BUT-B PSDI | −1.667 | −0.083 | 0.508 | ||||||
| Model | R | 0.215 | 0.659 | ||||||
| Summary | R2 | 0.046 | 0.434 | ||||||
| Adjusted R2 | 0.030 | 0.403 | |||||||
| F | 2.77 | 14.05 | |||||||
| Sig. of the model | 0.101 | <0.001 | |||||||
| F2 | 0.048 | 0.767 | |||||||
| R2 change | 0.387 | ||||||||
| Outcome: SF-12 Physical Health | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Step 1 | Step 2 | ||||||||
| B | β | p | B | β | p | ||||
| Independent Variables | BMI | −0.076 | −0.122 | 0.358 | −0.097 | −0.156 | 0.236 | ||
| BUT-A GSI | −0.786 | −0.240 | 0.131 | ||||||
| BUT-B PSDI | −0.456 | −0.128 | 0.410 | ||||||
| Model | R | 0.122 | 0.349 | ||||||
| Summary | R2 | 0.015 | 0.122 | ||||||
| Adjusted R2 | −0.002 | 0.074 | |||||||
| F | 0.858 | 2.551 | |||||||
| Sig. of the model | 0.358 | 0.065 | |||||||
| F2 | 0.015 | 0.139 | |||||||
| R2 change | 0.107 | ||||||||
| Outcome: SF-12 Mental Health | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Step 1 | Step 2 | Step 3 | |||||||||||
| B | β | p | B | β | p | B | β | p | |||||
| Independent Variables | BMI | 0.186 | 0.231 | 0.078 | 0.110 | 0.137 | 0.231 | 0.021 | 0.027 | 0.841 | |||
| BUT-A GSI | −2.373 | −0.563 | <0.001 | −2.394 | −0.568 | <0.001 | |||||||
| BUT-B PSDI | 0.240 | 0.052 | 0.699 | 0.318 | 0.069 | 0.606 | |||||||
| GENDER | −1.908 | −0.193 | 0.151 | ||||||||||
| Model Summary | R | 0.231 | 0.576 | 0.597 | |||||||||
| R2 | 0.053 | 0.331 | 0.357 | ||||||||||
| Adjusted R2 | 0.036 | 0.295 | 0.309 | ||||||||||
| F | 3.21 | 9.09 | 7.49 | ||||||||||
| Sig. of the model | 0.078 | <0.001 | <0.001 | ||||||||||
| F2 | 0.056 | 0.495 | 0.555 | ||||||||||
| R2 change | 0.278 | 0.025 | |||||||||||
| Outcome: BDI II | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Step 1 | Step 2 | ||||||||
| B | β | p | B | β | p | ||||
| Independent Variables | BMI | −0.007 | −0.005 | 0.972 | 0.151 | 0.105 | 0.347 | ||
| BUT-A GSI | 4.895 | 0.653 | <0.001 | ||||||
| BUT-B PSDI | −0.761 | −0.093 | 0.483 | ||||||
| Model | R | 0.005 | 0.595 | ||||||
| Summary | R2 | 0.020 | 0.354 | ||||||
| Adjusted R2 | −0.017 | 0.319 | |||||||
| F | 0.001 | 10.068 | |||||||
| Sig. of the model | 0.972 | <0.001 | |||||||
| F2 | 0.020 | 0.548 | |||||||
| R2 change | 0.354 | ||||||||
| Outcome: BHS | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Step 1 | Step 2 | ||||||||
| B | β | p | B | β | p | ||||
| Independent Variables | BMI | 0.001 | 0.002 | 0.989 | 0.041 | 0.077 | 0.561 | ||
| BUT-A GSI | 1.123 | 0.404 | 0.013 | ||||||
| BUT-B PSDI | −0.651 | −0.216 | 0.172 | ||||||
| Model Summary | R | 0.002 | 0.327 | ||||||
| R2 | 0.000 | 0.107 | |||||||
| Adjusted R2 | −0.017 | 0.058 | |||||||
| F | 0.059 | 2.19 | |||||||
| Sig. of the model | 0.989 | 0.099 | |||||||
| F2 | 0.000 | 0.120 | |||||||
| R2 change | 0.107 | ||||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Campedelli, V.; Ciacchella, C.; Veneziani, G.; Meniconzi, I.; Paone, E.; Silecchia, G.; Lai, C. Body Image and Body Mass Index Influence on Psychophysical Well-Being in Bariatric Patients: A Cross-Sectional Study. J. Pers. Med. 2022, 12, 1597. https://doi.org/10.3390/jpm12101597
Campedelli V, Ciacchella C, Veneziani G, Meniconzi I, Paone E, Silecchia G, Lai C. Body Image and Body Mass Index Influence on Psychophysical Well-Being in Bariatric Patients: A Cross-Sectional Study. Journal of Personalized Medicine. 2022; 12(10):1597. https://doi.org/10.3390/jpm12101597
Chicago/Turabian StyleCampedelli, Virginia, Chiara Ciacchella, Giorgio Veneziani, Irene Meniconzi, Emanuela Paone, Gianfranco Silecchia, and Carlo Lai. 2022. "Body Image and Body Mass Index Influence on Psychophysical Well-Being in Bariatric Patients: A Cross-Sectional Study" Journal of Personalized Medicine 12, no. 10: 1597. https://doi.org/10.3390/jpm12101597
APA StyleCampedelli, V., Ciacchella, C., Veneziani, G., Meniconzi, I., Paone, E., Silecchia, G., & Lai, C. (2022). Body Image and Body Mass Index Influence on Psychophysical Well-Being in Bariatric Patients: A Cross-Sectional Study. Journal of Personalized Medicine, 12(10), 1597. https://doi.org/10.3390/jpm12101597







