Effects of Implementing Personalized Health Education in Ambulatory Care on Cardiovascular Risk Factors, Compliance and Satisfaction with Treatment
Abstract
1. Introduction
2. Methods
- Age ≥ 18 years,
- Psychophysical state of health, which promises compliance with medical recommendations,
- Treatment for up to 4 weeks with acetylsalicylic acid at a dose of 100 mg.
- Chronic mental illnesses,
- Alcohol and/or drug addiction,
- Contraindications to the use of drugs containing acetylsalicylic acid.
3. Statistical Analysis
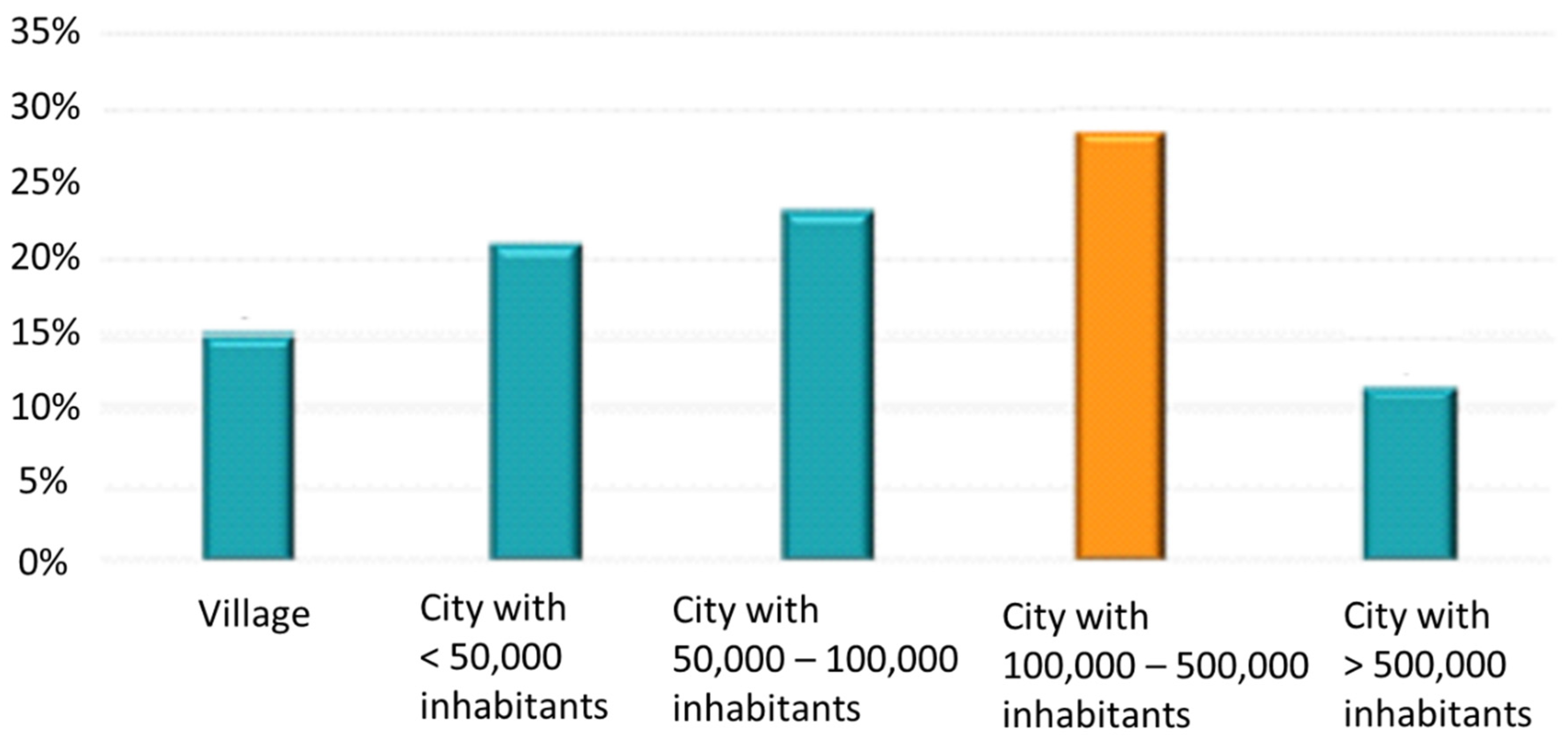
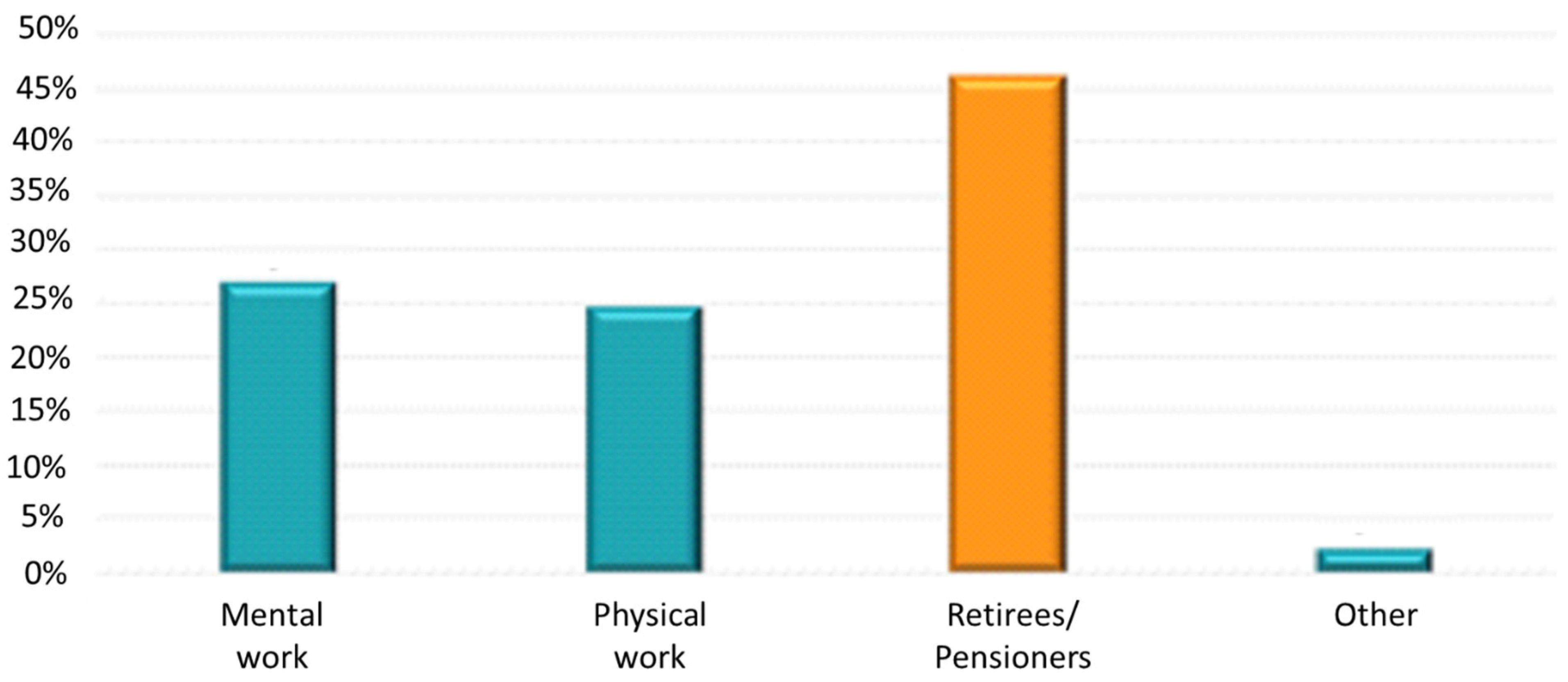
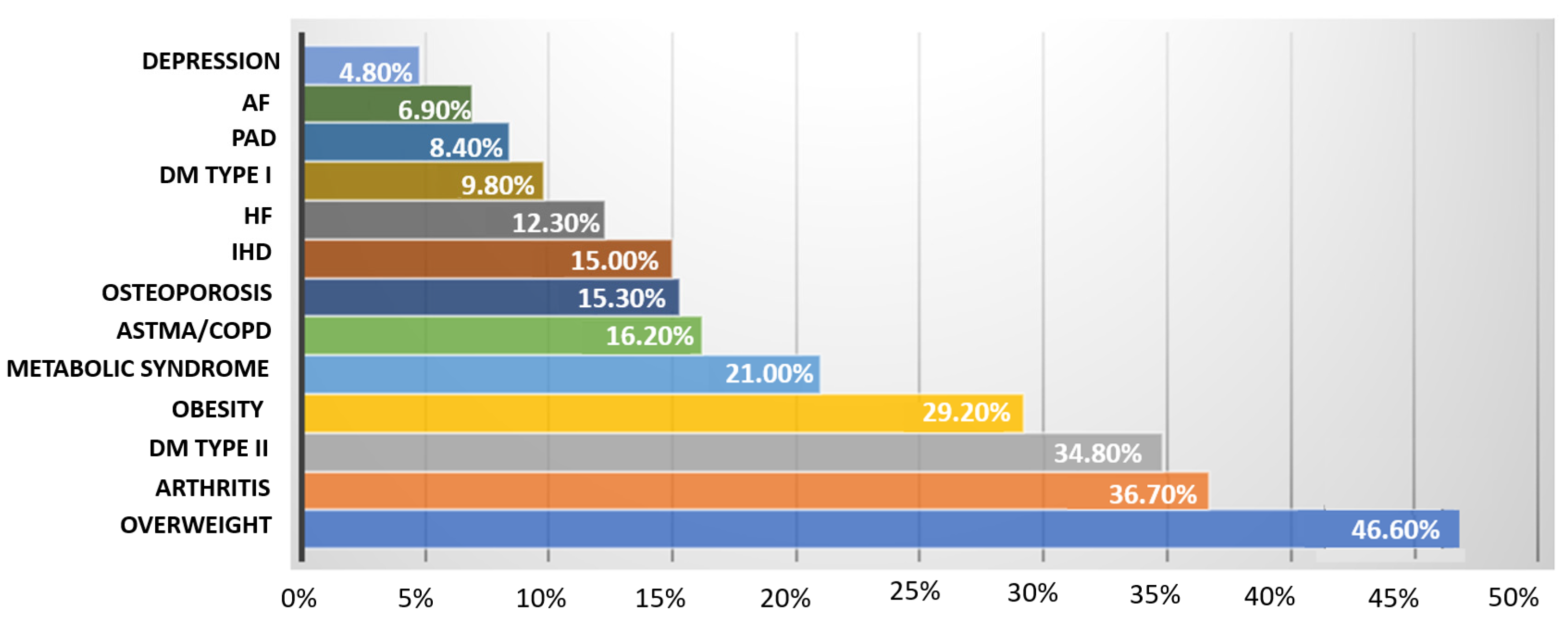
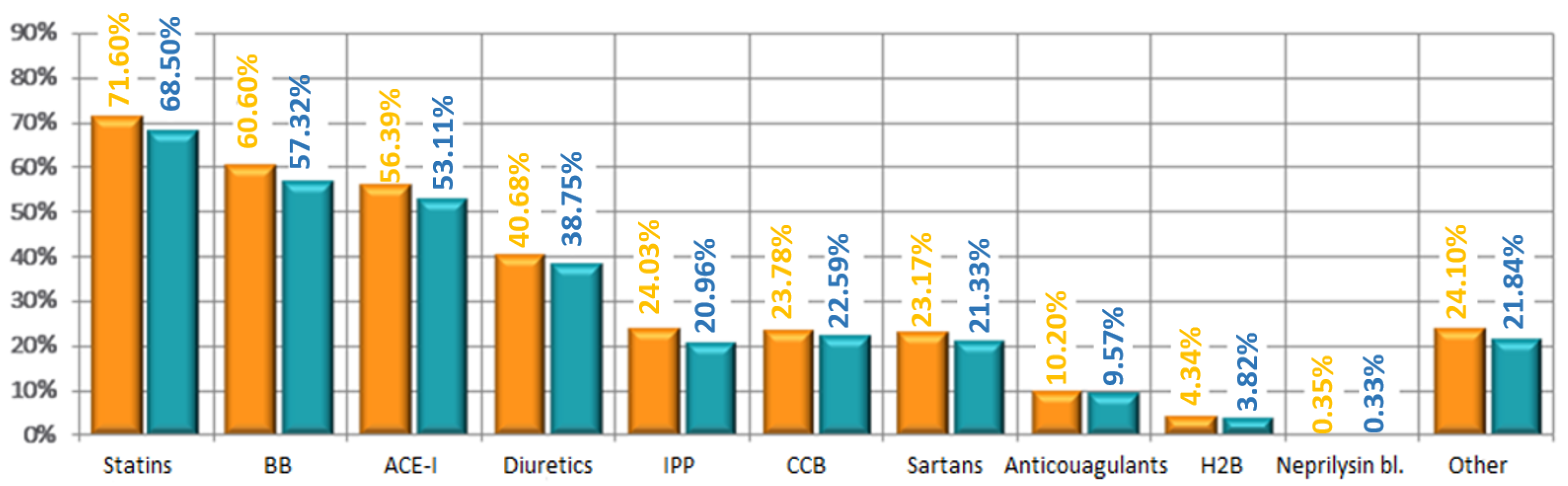
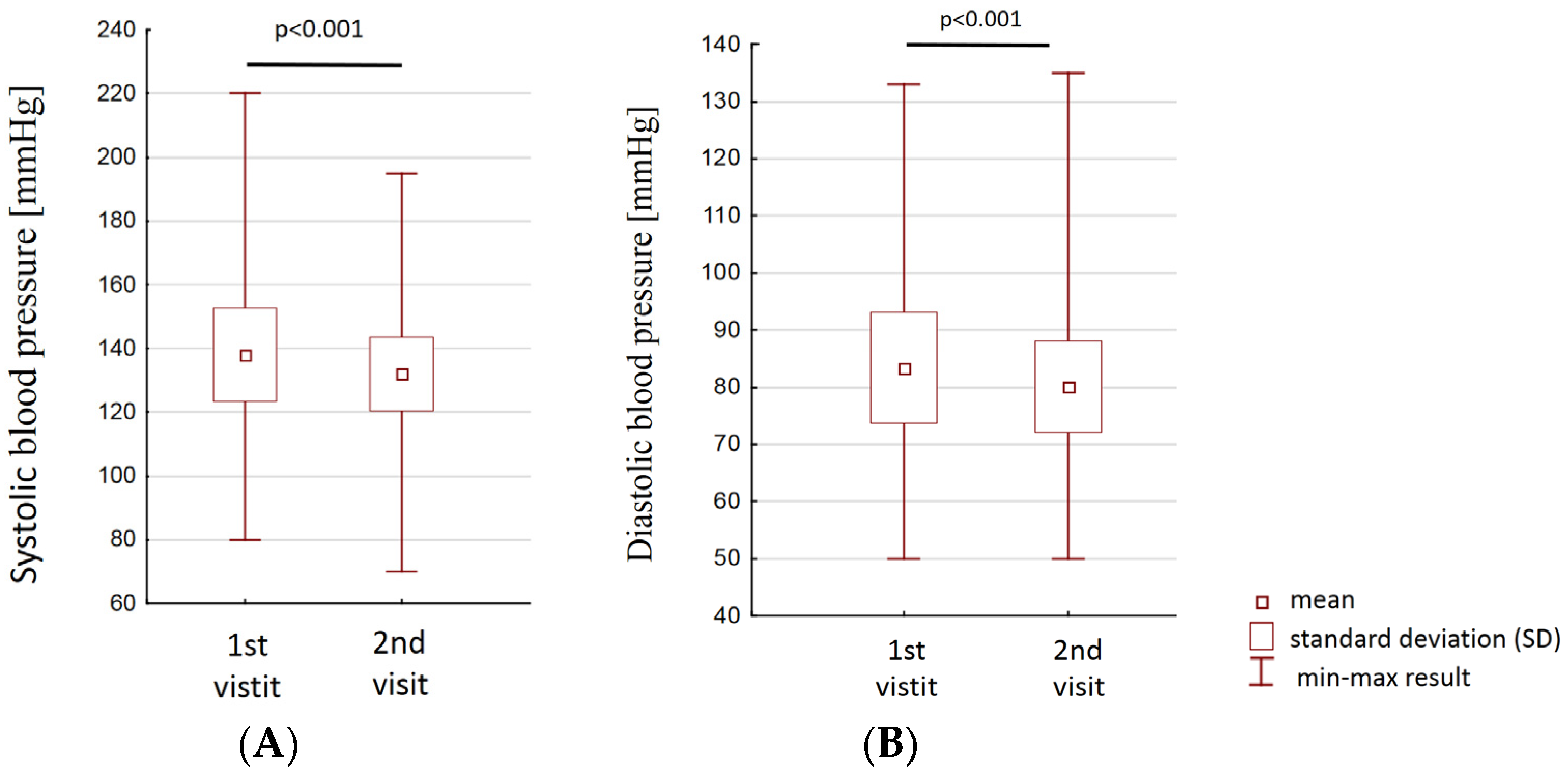
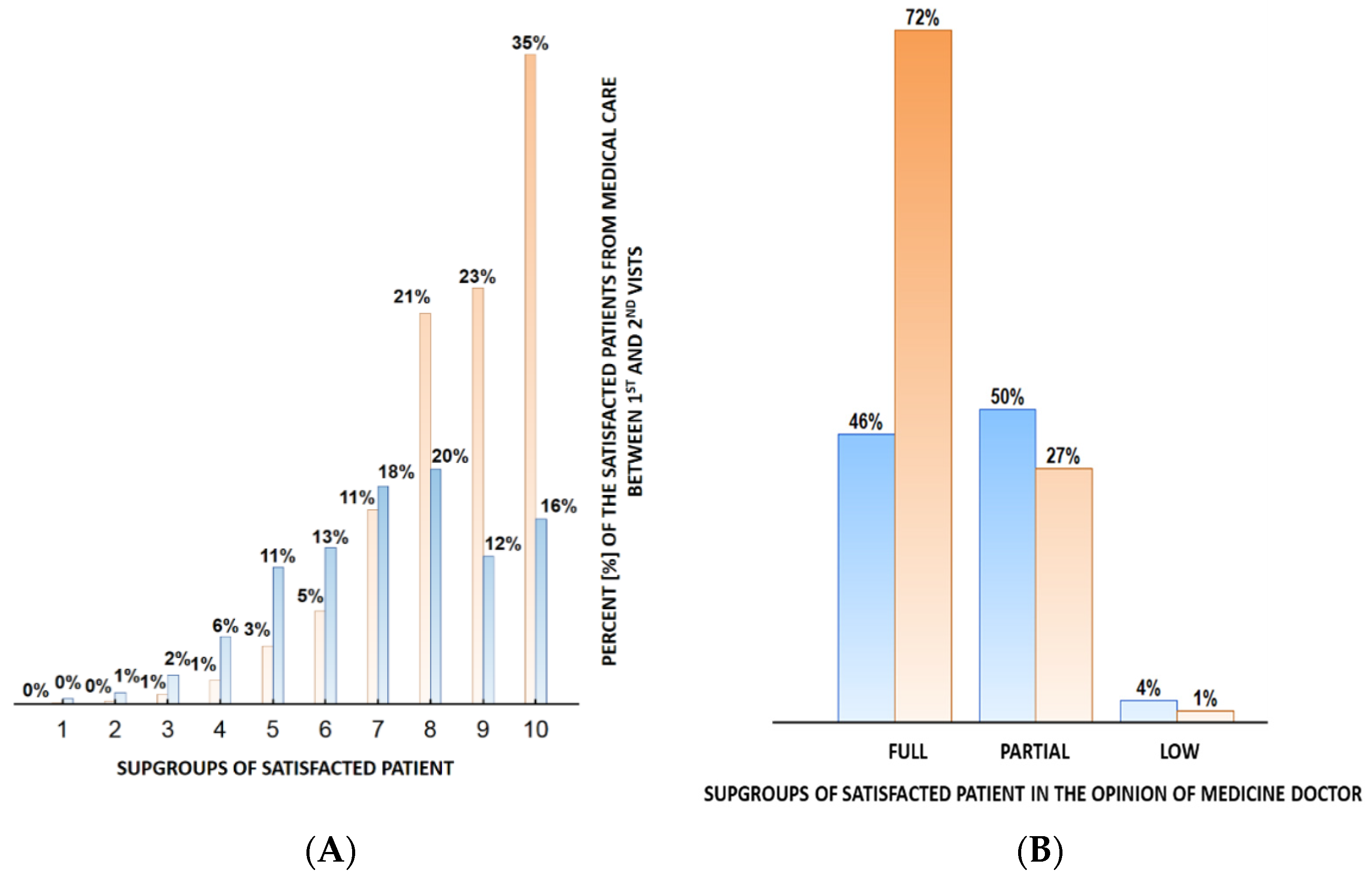
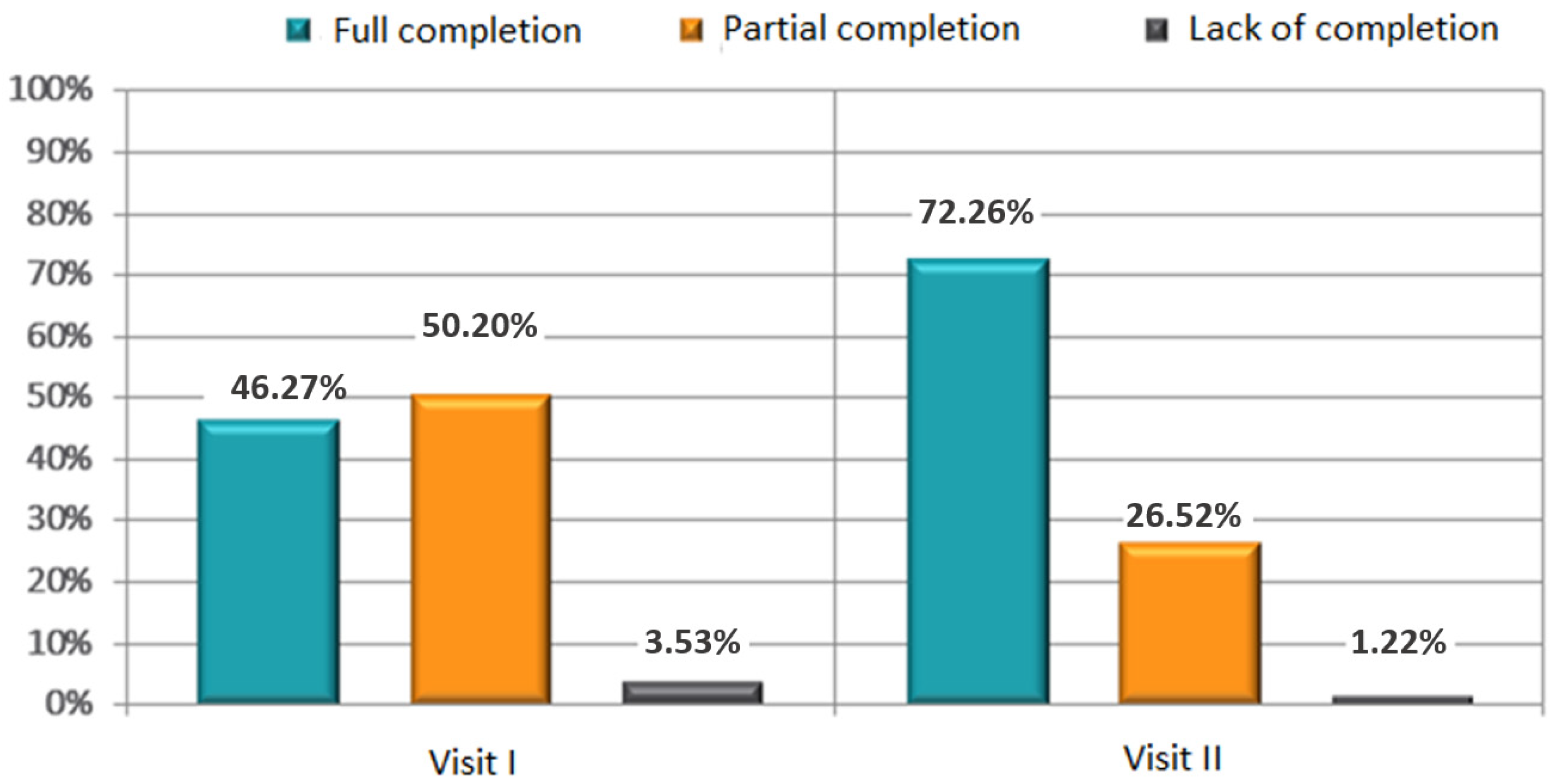
4. Results
5. Factors Influencing Medical Adherence to Lifestyle Modification
5.1. Physical Activity
5.2. Body Weight-Diet Reduction
5.3. Limiting Alcohol Consumption
5.4. Smoking
6. Discussion
7. Limitations of the Study
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Townsend, N.; Wilson, L.; Bhatnagar, P.; Wickramasinghe, K.; Rayner, M.; Nichols, M. Cardiovascular disease in Europe: Epidemiological update 2016. Eur. Heart J. 2016, 37, 3232–3245. [Google Scholar] [CrossRef] [PubMed]
- Members, T.F.; Piepoli, M.F.; Hoes, A.W.; Agewall, S.; Albus, C.; Brotons, C.; Catapano, A.L.; Cooney, M.T.; Corrà, U.; Cosyns, B.; et al. 2016 European on cardiovascular disease prevention in clinical practice: The Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts): Developed with the special contribution of the European Association for Cardiovascular Prevention and Rehabilitation (EACPR). Eur. J. Prev. Cardiol. 2016, 23, NP1–NP96. [Google Scholar]
- Kukkonen-Harjula, K.T.; Borg, P.T.; Nenonen, A.M.; Fogelholm, M.G. Effects of a weight maintenance program with or without exercise on the metabolic syndrome: A randomized trial in obese men. Prev. Med. 2005, 41, 784–790. [Google Scholar] [CrossRef] [PubMed]
- Esposito, K.; Marfella, R.; Ciotola, M.; Di Palo, C.; Giugliano, F.; Giugliano, G.; D’Armiento, M.; D’Andrea, F.; Giugliano, D. Effect of a Mediterranean-style diet on endothelial dysfunction and markers of vascular inflammation in the metabolic syndrome: A randomized trial. JAMA 2004, 292, 1440–1446. [Google Scholar] [CrossRef] [PubMed]
- Saboya, P.P.; Bodanese, L.C.; Zimmermann, P.R.; Gustavo AD, S.; Macagnan, F.E.; Feoli, A.P.; Oliveira MD, S. Lifestyle intervention on metabolic syndrome and its impact on quality of life: A randomized controlled trial. Arq. Bras. Cardiol. 2017, 108, 60–69. [Google Scholar] [CrossRef]
- Whelton, P.K.; Carey, R.M.; Aronow, W.S.; Casey, D.E., Jr.; Collins, K.J.; Dennison Himmelfarb, C.; DePalma, S.M.; Gidding, S.; Jamerson, K.A.; Jones, D.W.; et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: Executive Summary: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 2018, 71, 1269–1324. [Google Scholar]
- Sacks, F.M.; Svetkey, L.P.; Vollmer, W.M.; Appel, L.J.; Bray, G.A.; Harsha, D.; Obarzanek, E.; Conlin, P.R.; Miller, E.R.; Simons-Morton, D.G.; et al. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH-sodium collaborative research group. N. Engl. J. Med. 2001, 344, 3–10. [Google Scholar] [CrossRef]
- Perk, J.; De Backer, G.; Gohlke, H.; Graham, I.; Reiner, Ž.; Verschuren, M.; Albus, C.; Benlian, P.; Boysen, G.; Cifkova, R.; et al. European Guidelines on cardiovascular disease prevention in clinical practice (version 2012).The Fifth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of nine societies and by invited experts). Eur. Heart J. 2012, 33, 1635–1701. [Google Scholar]
- Cosentino, F.; Grant, P.J.; Aboyans, V.; Bailey, C.J.; Ceriello, A.; Delgado, V.; Federici, M.; Filippatos, G.; Grobbee, D.E.; Hansen, T.B.; et al. 2019 ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD. Eur. Heart J. 2020, 41, 255–323. [Google Scholar] [CrossRef]
- Mach, F.; Baigent, C.; Catapano, A.L.; Koskinas, K.C.; Casula, M.; Badimon, L.; Chapman, M.J.; De Backer, G.G.; Delgado, V.; Ference, B.A.; et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: Lipid modification to reduce cardiovascular risk. Eur. Heart J. 2020, 41, 111–188. [Google Scholar] [CrossRef]
- Filippou, C.D.; Tsioufis, C.P.; Thomopoulos, C.G.; Mihas, C.C.; Dimitriadis, K.S.; Sotiropoulou, L.I.; Chrysochoou, C.A.; Nihoyannopoulos, P.I.; Tousoulis, D.M. Dietary Approaches to Stop Hypertension (DASH) diet and blood pressure reduction in adults with and without hypertension: A systematic review and meta-analysis of randomized controlled trials. Adv. Nutr. 2020, 11, 1150–1160. [Google Scholar] [CrossRef]
- Sinnadurai, S.; Sowa, P.; Jankowski, P.; Gasior, Z.; Kosior, D.A.; Haberka, M.; Czarnecka, D.; Pająk, A.; Setny, M.; Jamiołkowski, J.; et al. Recollection of physician information about risk factor and lifestyle changes in chronic coronary syndrome patients. Int. J. Environ. Res. Public Health 2022, 19, 6416. [Google Scholar] [CrossRef] [PubMed]
- Piovesan, C.H.; Gustavo, A.; Macagnan, F.E.; Saboya, P.P.; Oliveira, M.D.S.; Bodanese, L.C.; Ludwig, M.W.B.; Closs, V.E.; Feoli, A.M.P. The effect of different interventions for lifestyle modifications on the number of diagnostic criteria and clinical aspects of metabolic syndrome. Metab. Syndr. Relat. Disord. 2021, 19, 8–17. [Google Scholar] [CrossRef]
- Oh, E.G.; Bang, S.Y.; Hyun, S.S.; Kim, S.H.; Chu, S.H.; Jeon, J.Y.; Im, J.A.; Lee, M.K.; Lee, J.E. Effects of a 6-month lifestyle modification intervention on the cardiometabolic risk factors and health-related qualities of life in women with metabolic syndrome. Metabolism 2010, 59, 1035–1043. [Google Scholar] [CrossRef] [PubMed]
- Eriksson, K.M.; Westborg, C.J.; Eliasson, M.C. A randomized trial of lifestyle intervention in primary healthcare for the modification of cardiovascular risk factors. Scand. J. Public Health 2006, 34, 453–461. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.H.; Chiang, S.L.; Tzeng, W.C.; Chiang, L.C. Systematic review of impact of lifestyle-modification programs on metabolic risks and patient-reported outcomes in adults with metabolic syndrome. Worldviews Evid.-Based Nurs. 2014, 11, 361–368. [Google Scholar] [CrossRef]
- Yamamoto, R.; Kawamura, T.; Wakai, K.; Ichihara, Y.; Anno, T.; Mizuno, Y.; Yokoi, M.; Ohta, T.; Lguchi, A.; Ohno, Y. Favorable life-style modification and attenuation of cardiovascular risk factors. Jpn. Circ. J. 1999, 63, 184–188. [Google Scholar] [CrossRef][Green Version]
- Lee, Y.M.; Kim, R.B.; Lee, H.J.; Kim, K.; Shin, M.H.; Park, H.K.; Ahn, S.K.; Kim, S.Y.; Lee, Y.H.; Kim, B.G.; et al. Relationships among medication adherence, lifestyle modification, and health-related quality of life in patients with acute myocardial infarction: A cross-sectional study. Health Qual. Life Outcomes 2018, 16, 100. [Google Scholar] [CrossRef]
- Villafuerte, F.U.; Cànaves, J.L.; Montalvo, P.L.; Sancho, M.L.M.; Oliver, B.O.; Flores, P.B.; Mantolan, A.E.; Bordoy, P.J.; Ruiz, R.T.; Hernández, R.A. Effectiveness of a multifactorial intervention, consisting of self-management of antihypertensive medication, self-measurement of blood pressure, hypocaloric and low sodium diet, and physical exercise, in patients with uncontrolled hypertension taking 2 or more antihypertensive drugs: The MEDICHY study. Medicine (Baltimore) 2020, 99, e19769. [Google Scholar]
- Brinks, J.; Fowler, A.; Franklin, B.A.; Dulai, J. Lifestyle Modification in Secondary Prevention: Beyond Pharmacotherapy. Am. J. Lifestyle Med. 2017, 11, 137–152. [Google Scholar] [CrossRef]
- Khaw, K.T.; Wareham, N.; Bingham, S.; Welch, A.; Luben, R.; Day, N. Combined impact of health behaviours and mortality in men and women: The EPIC-Norfolk prospective population study. PLoS Med. 2008, 5, e12. [Google Scholar]

| Mean | SD | 95% CI | ||
|---|---|---|---|---|
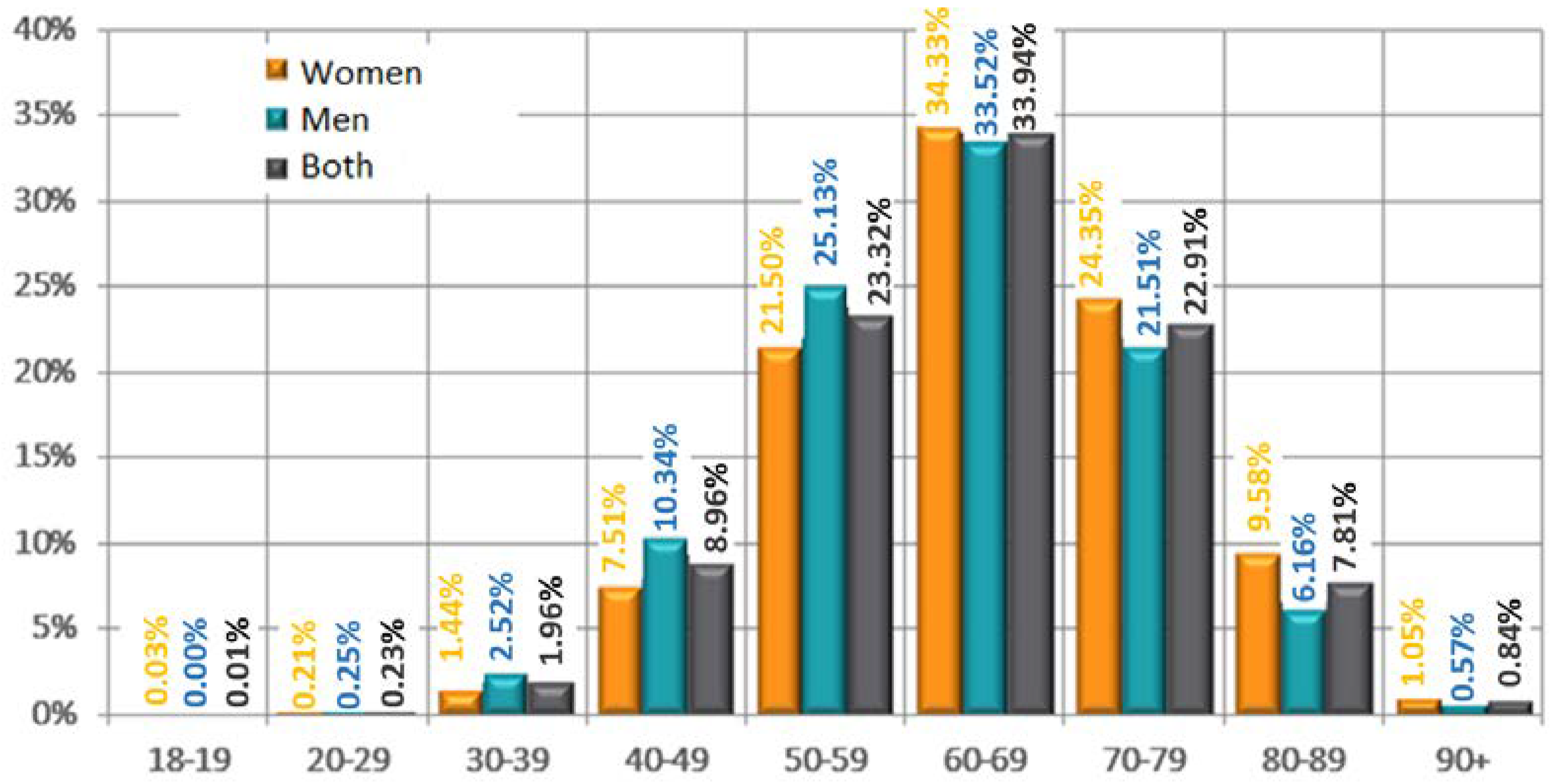
| Age (years) | Women | 65.11 | 11.29 | 64.76–65.47 |
| Men | 62.69 | 11.23 | 62.34–63.04 | |
| Both | 63.89 | 11.32 | 63.63–64.14 | |
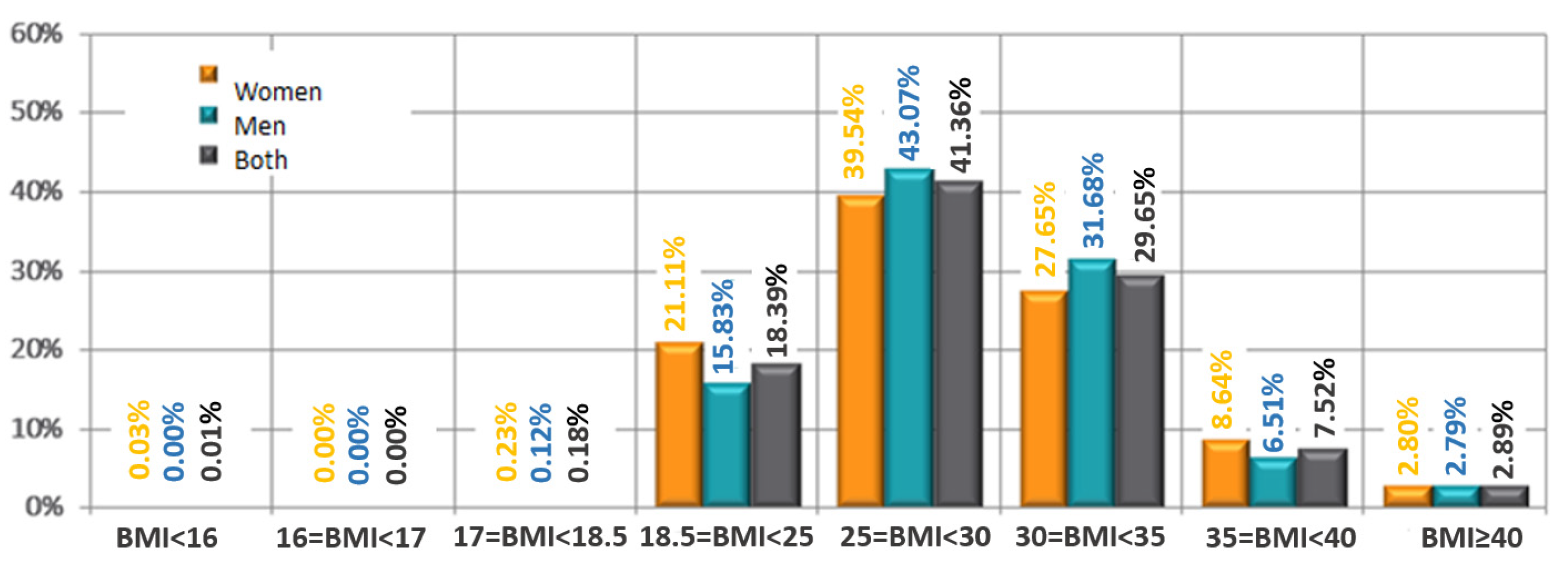
| BMI (kg/m2) | Women | 29.00 | 4.91 | 28.85–29.16 |
| Men | 29.32 | 4.49 | 29.18–29.46 | |
| Both | 29.17 | 4.70 | 29.06–29.27 |
| Blood Pressure The First Visit | Women Mean (±SD) | Men Mean (±SD) | p |
|---|---|---|---|
| Systolic | 136.91 | 139.01 | <0.0001 |
| (mmHg) | (14.74) | (14.58) | |
| Diastolic | 82.47 | 84.26 | <0.0001 |
| (mmHg) | (9.73) | (9.69) |
| Lipid Fraction | 1st Visit Mean (±SD) | 2nd Visit Mean (±SD) | p |
|---|---|---|---|
| Total cholesterol | 209 (±76) | 196 (±41) | <0.001 |
| LDL-cholesterol | 121(±48) | 111(±34) | <0.001 |
| HDL-Cholesterol | 55 (±28) | 55 (±24) | 0.436 |
| Triglicerydes | 154 (±81) | 140 (±55) | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bielecka-Dabrowa, A.; Lewek, J.; Sakowicz, A.; Paduszyńska, A.; Dąbrowa, M.; Orszulak-Michalak, D.; Banach, M.; CARDIOPLUS Investigators. Effects of Implementing Personalized Health Education in Ambulatory Care on Cardiovascular Risk Factors, Compliance and Satisfaction with Treatment. J. Pers. Med. 2022, 12, 1583. https://doi.org/10.3390/jpm12101583
Bielecka-Dabrowa A, Lewek J, Sakowicz A, Paduszyńska A, Dąbrowa M, Orszulak-Michalak D, Banach M, CARDIOPLUS Investigators. Effects of Implementing Personalized Health Education in Ambulatory Care on Cardiovascular Risk Factors, Compliance and Satisfaction with Treatment. Journal of Personalized Medicine. 2022; 12(10):1583. https://doi.org/10.3390/jpm12101583
Chicago/Turabian StyleBielecka-Dabrowa, Agata, Joanna Lewek, Agata Sakowicz, Aleksandra Paduszyńska, Marek Dąbrowa, Daria Orszulak-Michalak, Maciej Banach, and CARDIOPLUS Investigators. 2022. "Effects of Implementing Personalized Health Education in Ambulatory Care on Cardiovascular Risk Factors, Compliance and Satisfaction with Treatment" Journal of Personalized Medicine 12, no. 10: 1583. https://doi.org/10.3390/jpm12101583
APA StyleBielecka-Dabrowa, A., Lewek, J., Sakowicz, A., Paduszyńska, A., Dąbrowa, M., Orszulak-Michalak, D., Banach, M., & CARDIOPLUS Investigators. (2022). Effects of Implementing Personalized Health Education in Ambulatory Care on Cardiovascular Risk Factors, Compliance and Satisfaction with Treatment. Journal of Personalized Medicine, 12(10), 1583. https://doi.org/10.3390/jpm12101583









