Profit versus Quality: The Enigma of Scientific Wellness
Abstract
1. Introduction
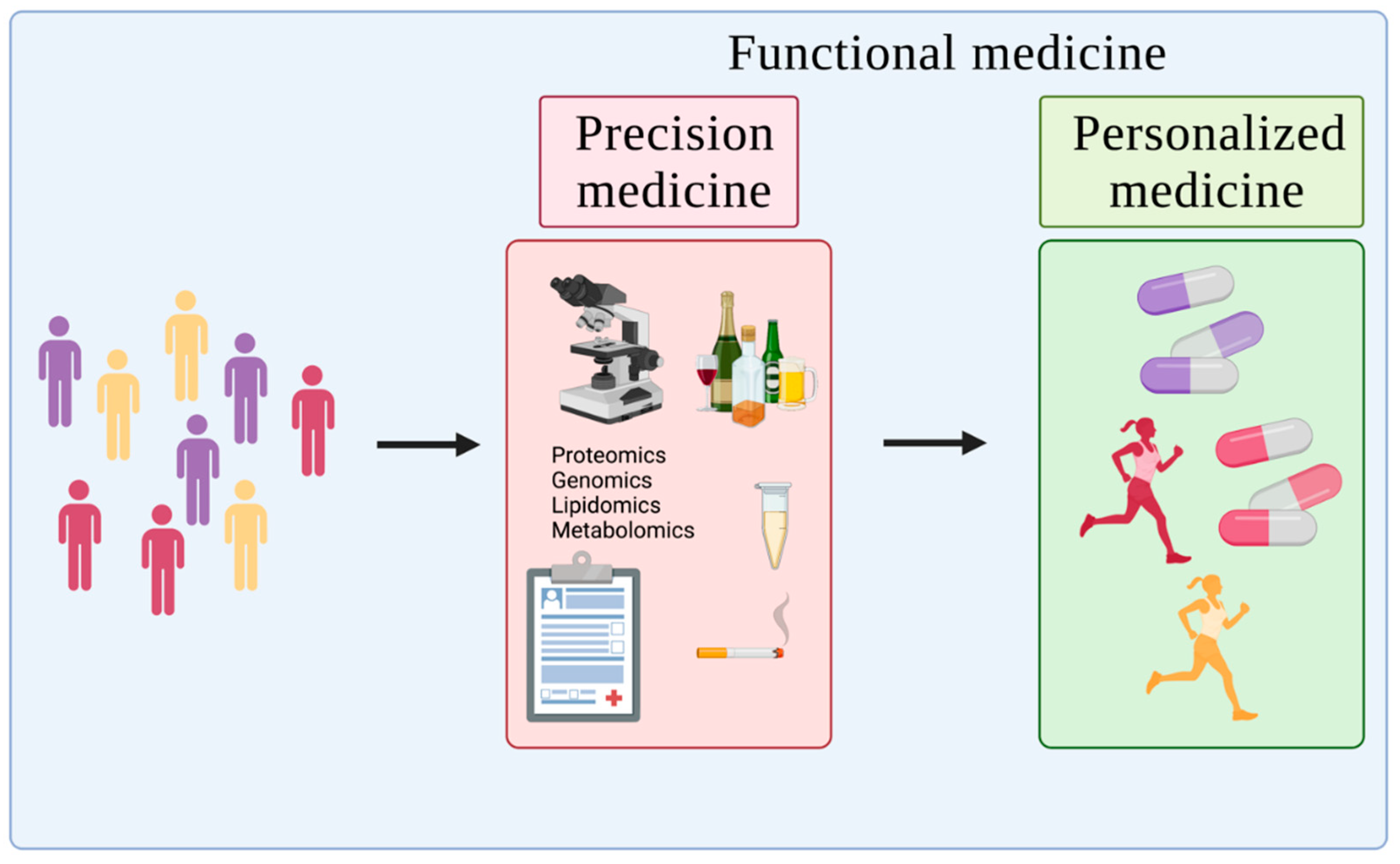
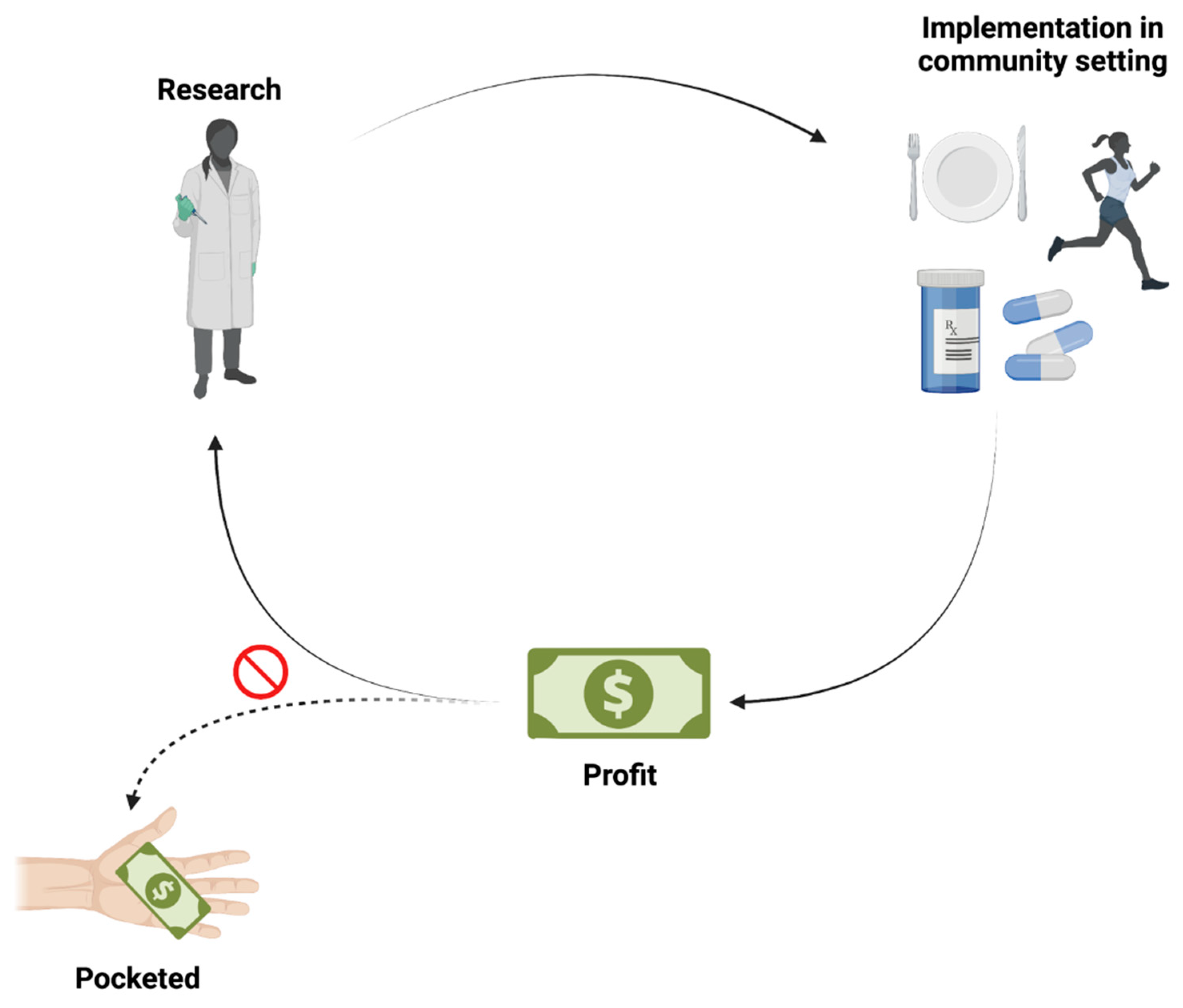
2. Current Strategies
2.1. Research-Based Ventures (Voluntary Participants)
2.2. Business Ventures (Paying Clients)
3. Lessons Learned
4. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Barlow, F.K. Nature vs. nurture is nonsense: On the necessity of an integrated genetic, social, developmental, and personality psychology. Aust. J. Psychol. 2019, 71, 68–79. [Google Scholar] [CrossRef]
- Nazha, B.; Mishra, M.; Pentz, R.; Owonikoko, T.K. Enrollment of racial minorities in clinical trials: Old problem assumes new urgency in the age of immunotherapy. Am. Soc. Clin. Oncol. Educ. Book 2019, 39, 3–10. [Google Scholar] [CrossRef]
- Jackson, S.E.; Llewellyn, C.H.; Smith, L. The obesity epidemic—Nature via nurture: A narrative review of high-income countries. SAGE Open Med. 2020, 8, 2050312120918265. [Google Scholar] [CrossRef] [PubMed]
- Tistarelli, N.; Fagnani, C.; Troianiello, M.; Stazi, M.A.; Adriani, W. The nature and nurture of ADHD and its comorbidities: A narrative review on twin studies. Neurosci. Biobehav. Rev. 2020, 109, 63–77. [Google Scholar] [CrossRef] [PubMed]
- Brom, B. Functional medicine: How dysfunction leads to disease. S. Afr. Fam. Pract. 2011, 53, 540–544. [Google Scholar] [CrossRef][Green Version]
- Bland, J. Defining function in the functional medicine model. Integr. Med. 2017, 16, 22–25. [Google Scholar]
- Mirnezami, R.; Nicholson, J.; Darzi, A. Preparing for precision medicine. N. Engl. J. Med. 2012, 366, 489–491. [Google Scholar] [CrossRef]
- National Research Council. The National Academies Collection: Reports funded by National Institutes of Health. In Toward Precision Medicine: Building a Knowledge Network for Biomedical Research and a New Taxonomy of Disease; National Academies Press: Washington, DC, USA, 2011. [Google Scholar]
- Jameson, J.L.; Longo, D.L. Precision medicine—Personalized, problematic, and promising. N. Engl. J. Med. 2015, 372, 2229–2234. [Google Scholar] [CrossRef]
- Vogenberg, F.R.; Isaacson Barash, C.; Pursel, M. Personalized medicine: Part 1: Evolution and development into theranostics. Pharm. Ther. 2010, 35, 560–576. [Google Scholar]
- Senn, S. Statistical pitfalls of personalized medicine. Nature 2018, 563, 619–621. [Google Scholar] [CrossRef]
- Antonovsky, A. Studying Health Instead of Disease. In Health, Stress, and Coping, 1st ed.; Jossey-Bass: San Francisco, CA, USA, 1979; pp. 12–37. [Google Scholar]
- Kaeberlein, M. How healthy is the healthspan concept? Geroscience 2018, 40, 361–364. [Google Scholar] [CrossRef] [PubMed]
- Hood, L. P4 medicine and scientific wellness: Catalyzing a revolution in 21st century medicine. Mol. Front. J. 2017, 1, 132–137. [Google Scholar] [CrossRef]
- Price, N.D.; Magis, A.T.; Earls, J.C.; Glusman, G.; Levy, R.; Lausted, C.; McDonald, D.T.; Kusebauch, U.; Moss, C.L.; Zhou, Y.; et al. A wellness study of 108 individuals using personal, dense, dynamic data clouds. Nat. Biotechnol. 2017, 35, 747–756. [Google Scholar] [CrossRef] [PubMed]
- Maxmen, A. Google spin-off deploys wearable electronics for huge health study. Nature 2017, 547, 13–14. [Google Scholar] [CrossRef]
- Senior, M. ‘Scientific wellness’ searches for a business model. Nat. Biotechnol. 2019, 37, 705–706. [Google Scholar] [CrossRef]
- Chen, Z.; Chen, J.; Collins, R.; Guo, Y.; Peto, R.; Wu, F.; Li, L. China Kadoorie Biobank of 0.5 million people: Survey methods, baseline characteristics and long-term follow-up. Int. J. Epidemiol. 2011, 40, 1652–1666. [Google Scholar] [CrossRef] [PubMed]
- Lv, J.; Chen, W.; Sun, D.; Li, S.; Millwood, I.Y.; Smith, M.; Guo, Y.; Bian, Z.; Yu, C.; Zhou, H.; et al. Gender-specific association between tobacco smoking and central obesity among 0.5 million Chinese people: The China Kadoorie Biobank Study. PLoS ONE 2015, 10, e0124586. [Google Scholar] [CrossRef]
- Du, H.; Li, L.; Bennett, D.; Yang, L.; Guo, Y.; Key, T.J.; Bian, Z.; Chen, Y.; Walters, R.G.; Millwood, I.Y.; et al. Fresh fruit consumption and all-cause and cause-specific mortality: Findings from the China Kadoorie Biobank. Int. J. Epidemiol. 2017, 46, 1444–1455. [Google Scholar] [CrossRef]
- Song, X.; Wu, J.; Yu, C.; Dong, W.; Lv, J.; Guo, Y.; Bian, Z.; Yang, L.; Chen, Y.; Chen, Z.; et al. Association between multiple comorbidities and self-rated health status in middle-aged and elderly Chinese: The China Kadoorie Biobank study. BMC Public Health 2018, 18, 744. [Google Scholar] [CrossRef]
- Project Baseline by Verily. Available online: https://www.projectbaseline.com (accessed on 11 October 2021).
- Arges, K.; Assimes, T.; Bajaj, V.; Balu, S.; Bashir, M.R.; Beskow, L.; Blanco, R.; Califf, R.; Campbell, P.; Carin, L.; et al. The Project Baseline Health Study: A step towards a broader mission to map human health. NPJ Digit. Med. 2020, 3, 84. [Google Scholar] [CrossRef]
- Wong, C.A.; Hernandez, A.F.; Califf, R.M. Return of research results to study participants: Uncharted and untested. JAMA 2018, 320, 435–436. [Google Scholar] [CrossRef]
- deCODE Genetics. Available online: https://www.decode.com (accessed on 12 October 2021).
- Somalogic. Available online: https://somalogic.com (accessed on 12 October 2021).
- deCODE Genetics, and Amgen Subsidiary, and SomaLogic Announce Collaboration to Perform Large-Scale Protein Analysis of up to 40,000 Human Samples. Available online: https://somalogic.com/news_press_releases/decode-genetics-an-amgen-subsidiary-and-somalogic-announce-collaboration-to-perform-large-scale-protein-analysis-of-up-to-40000-human-samples/ (accessed on 8 October 2021).
- Styrkarsdottir, U.; Lund, S.H.; Saevarsdottir, S.; Magnusson, M.I.; Gunnarsdottir, K.; Norddahl, G.L.; Frigge, M.L.; Ivarsdottir, E.V.; Bjornsdottir, G.; Holm, H.; et al. The CRTAC1 protein in plasma is associated with osteoarthritis and predicts progression to joint replacement: A large-scale proteomics scan in Iceland. Arthritis Rheumatol. 2021, 73, 2025–2034. [Google Scholar] [CrossRef]
- Research Institute for Aging. Available online: https://the-ria.ca (accessed on 8 October 2021).
- The Precision Medicine Initiative. Available online: https://www.nih.gov/sites/default/files/research-training/initiatives/pmi/pmi-infographic.pdf (accessed on 8 October 2021).
- Ramirez, A.H.; Gebo, K.A.; Harris, P.A. Progress with the All of Us research program: Opening access for researchers. JAMA 2021, 325, 2441–2442. [Google Scholar] [CrossRef]
- The Human Project. Available online: https://www.thehumanproject.org (accessed on 1 October 2021).
- Introducing the Kavli HUMAN Project. Available online: https://www.psychologicalscience.org/publications/observer/obsonline/introducing-the-kavli-human-project.html (accessed on 8 October 2021).
- Rutkin, A. Tracking the health of 10,000 New Yorkers. New Sci. 2015, 228, 20. [Google Scholar] [CrossRef]
- World Urbanization Prospects. Available online: https://population.un.org/wup/ (accessed on 12 October 2021).
- Buchholz, K. How Was the World’s Urban Population Changed from 1950 to Today? Available online: https://www.weforum.org/agenda/2020/11/global-continent-urban-population-urbanisation-percent/ (accessed on 4 November 2021).
- iCarbonX. Available online: https://www.icarbonx.com/en/index.html (accessed on 2 November 2021).
- Cyranoski, D. Jun Wang’s iCarbonX heads consortium using AI in health and wellness. Nat. Biotechnol. 2017, 35, 103–104. [Google Scholar] [CrossRef] [PubMed]
- Abbasi, J. 23andMe, big data, and the genetics of depression. JAMA 2017, 317, 14–16. [Google Scholar] [CrossRef] [PubMed]
- 23andMe Agrees to Acquire Lemonaid Health. Available online: https://www.globenewswire.com/news-release/2021/10/22/2319017/0/en/23andMe-Agrees-to-Acquire-Lemonaid-Health.html (accessed on 25 October 2021).
- Lemonaid Health. Available online: https://www.lemonaidhealth.com (accessed on 25 October 2021).
- Health Nucleus by Human Longevity Inc. Available online: https://www.healthnucleus100plus.com (accessed on 8 October 2021).
- 100+ by Health Nucleus. Available online: https://www.healthnucleus100plus.com/pages/brnst (accessed on 4 November 2021).
- Cross, R. ‘Scientific wellnes’ study divides researchers. Science 2017, 357, 345. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Abascal, F.; Juan, D.; Jungreis, I.; Martinez, L.; Rigau, M.; Rodriguez, J.M.; Vazquez, J.; Tress, M.L. Loose ends: Almost one in five human genes still have unresolved coding status. Nucleic Acids Res. 2018, 46, 7070–7084. [Google Scholar] [CrossRef] [PubMed]
- Loos, R.J.F. From nutrigenomics to personalizing diets: Are we ready for precision medicine? Am. J. Clin. Nutr. 2019, 109, 1–2. [Google Scholar] [CrossRef] [PubMed]
- Peisch, S.F.; Van Blarigan, E.L.; Chan, J.M.; Stampfer, M.J.; Kenfield, S.A. Prostate cancer progression and mortality: A review of diet and lifestyle factors. World J. Urol. 2017, 35, 867–874. [Google Scholar] [CrossRef]
- Jakimovski, D.; Weinstock-Guttman, B.; Gandhi, S.; Guan, Y.; Hagemeier, J.; Ramasamy, D.P.; Fuchs, T.A.; Browne, R.W.; Bergsland, N.; Dwyer, M.G.; et al. Dietary and lifestyle factors in multiple sclerosis progression: Results from a 5-year longitudinal MRI study. J. Neurol. 2019, 266, 866–875. [Google Scholar] [CrossRef]
- Paul, K.C.; Chuang, Y.-H.; Shih, I.F.; Keener, A.; Bordelon, Y.; Bronstein, J.M.; Ritz, B. The association between lifestyle factors and Parkinson’s disease progression and mortality. Mov. Disord. 2019, 34, 58–66. [Google Scholar] [CrossRef] [PubMed]
- Langan, S.P.; Grosicki, G.J. Exercise is medicine…and the dose matters. Front. Physiol. 2021, 12, 660818. [Google Scholar] [CrossRef] [PubMed]
- Pape, S.E.; Baksh, R.A.; Startin, C.; Hamburg, S.; Hithersay, R.; Strydom, A. The association between physical activity and CAMDEX-DS changes prior to the onset of Alzheimer’s disease in Down Syndrome. J. Clin. Med. 2021, 10, 1882. [Google Scholar] [CrossRef]
- Bland, J. Arivale Is Gone but Not Forgotten: What Did We Learn? Medium 2019. Available online: https://medium.com/@jeffreyblandphd/arivale-is-gone-but-not-forgotten-what-did-we-learn-6c37142f5f80 (accessed on 12 October 2021).
- Stein, D. Are You Suffering from B.S.O.S? Available online: https://salesandmarketing.com/are-you-suffering-bsos/ (accessed on 12 October 2021).
- Smith, C. Your SOS: How to handle the Shiny Object Syndrome. Rough Notes 2015, 158, 70–72. [Google Scholar]
- Genetic Information Privacy. Available online: https://www.eff.org/issues/genetic-information-privacy (accessed on 3 November 2021).
- Brodwin, E. After You Spit into a Tube for a DNA Test like 23andMe, Experts Say You Shouldn’t Assume Your Data Will Stay Private Forever. Available online: https://www.businessinsider.com/privacy-security-risks-genetic-testing-23andme-ancestry-dna-2019-2 (accessed on 3 November 2021).
- GEDmatch. Available online: https://www.gedmatch.com (accessed on 3 November 2021).
- Erlich, Y.; Shor, T.; Pe’er, I.; Carmi, S. Identity inference of genomic data using long-range familial searches. Science 2018, 362, 690–694. [Google Scholar] [CrossRef]
- Segert, J.; Nathan, A. Understanding Ownership and Privacy of Genetic Data; Harvard University, The Graduate School of Arts and Sciences: Cambridge, MA, USA, 2018; Available online: https://sitn.hms.harvard.edu/flash/2018/understanding-ownership-privacy-genetic-data/ (accessed on 3 November 2021).
- Dankar, F.K.; Ptitsyn, A.; Dankar, S.K. The development of large-scale de-identified biomedical databases in the age of genomics—Principles and challenges. Hum. Genom. 2018, 12, 19. [Google Scholar] [CrossRef]
- Slavich, G.M. Life stress and health: A review of conceptual issues and recent findings. Teach. Psychol. 2016, 43, 346–355. [Google Scholar] [CrossRef]
- Febbraio, M.A. Health benefits of exercise—More than meets the eye! Nat. Rev. Endocrinol. 2017, 13, 72–74. [Google Scholar] [CrossRef] [PubMed]
- Pietromonaco, P.R.; Collins, N.L. Interpersonal mechanisms linking close relationships to health. Am. Psychol. 2017, 72, 531–542. [Google Scholar] [CrossRef] [PubMed]
- Muscaritoli, M. The impact of nutrients on mental health and well-being: Insights from the literature. Front. Nutr. 2021, 8, 656290. [Google Scholar] [CrossRef] [PubMed]
- Kujawa, C. Before ‘Raw Water,’ Radium Water Was the craze—And then People Died. Chic. Trib. 2018. Available online: https://www.chicagotribune.com/opinion/commentary/ct-perspec-flash-radium-elixir-fad-cure-cocktails-0304-20180220-story.html (accessed on 12 October 2021).
- Shapiro, N.L.; Loberg, K. Hype: A Doctor’s Guide to Medical Myths, Exaggerated Claims and Bad Advice—How to Tell What’s Real and What’s Not, 1st ed.; St. Martin’s Press: New York, NY, USA, 2018. [Google Scholar]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Carbonara, K.; MacNeil, A.J.; O’Leary, D.D.; Coorssen, J.R. Profit versus Quality: The Enigma of Scientific Wellness. J. Pers. Med. 2022, 12, 34. https://doi.org/10.3390/jpm12010034
Carbonara K, MacNeil AJ, O’Leary DD, Coorssen JR. Profit versus Quality: The Enigma of Scientific Wellness. Journal of Personalized Medicine. 2022; 12(1):34. https://doi.org/10.3390/jpm12010034
Chicago/Turabian StyleCarbonara, Katrina, Adam J. MacNeil, Deborah D. O’Leary, and Jens R. Coorssen. 2022. "Profit versus Quality: The Enigma of Scientific Wellness" Journal of Personalized Medicine 12, no. 1: 34. https://doi.org/10.3390/jpm12010034
APA StyleCarbonara, K., MacNeil, A. J., O’Leary, D. D., & Coorssen, J. R. (2022). Profit versus Quality: The Enigma of Scientific Wellness. Journal of Personalized Medicine, 12(1), 34. https://doi.org/10.3390/jpm12010034






