Comparative Evaluation of the Prognosis of Septic Shock Patients from Before to After the Onset of the COVID-19 Pandemic: A Retrospective Single-Center Clinical Analysis
Abstract
:1. Introduction
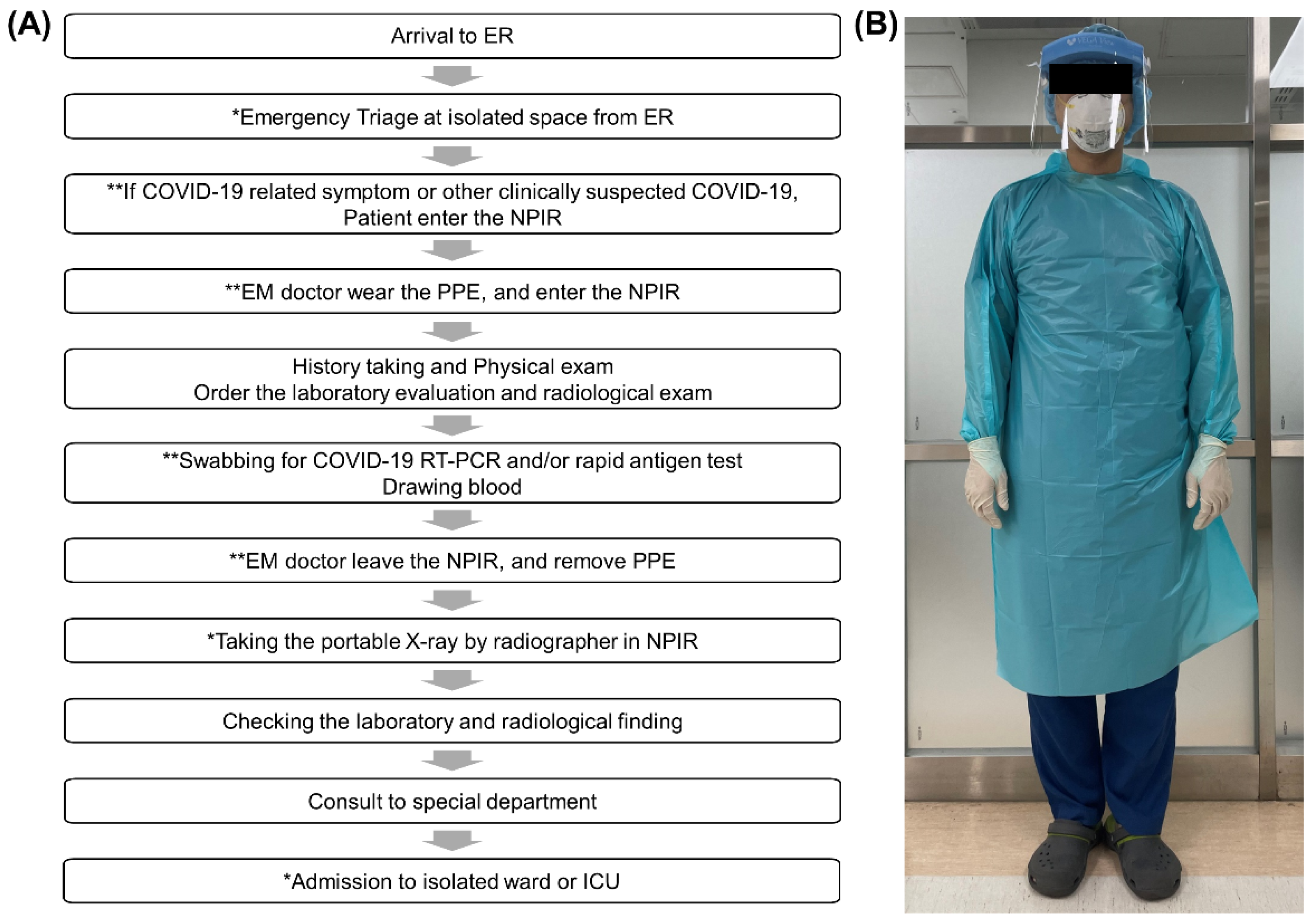
2. Materials and Methods
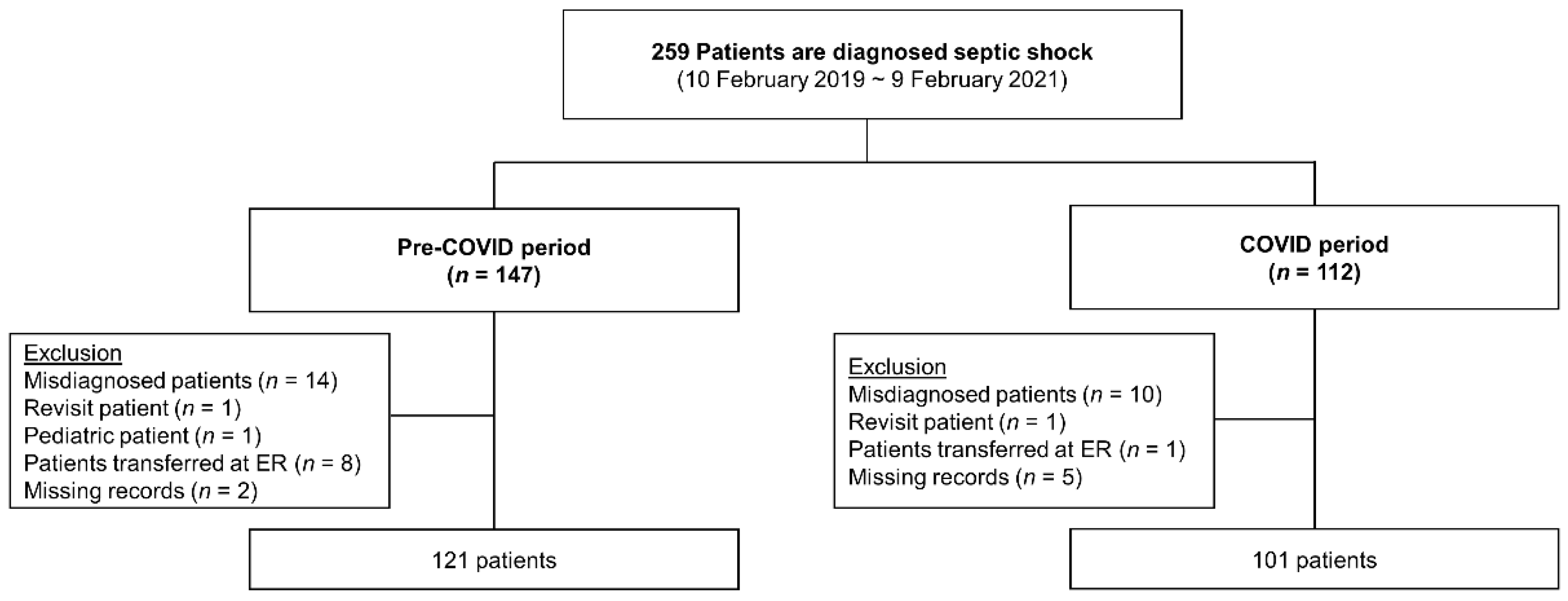
2.1. Study Design and Population
2.2. Data Collection and Outcome Measurement
2.3. Statistical Analysis
2.4. Ethics Statement
3. Results
3.1. Baseline Characteristics
3.2. Clinical Characteristics
3.3. Outcomes
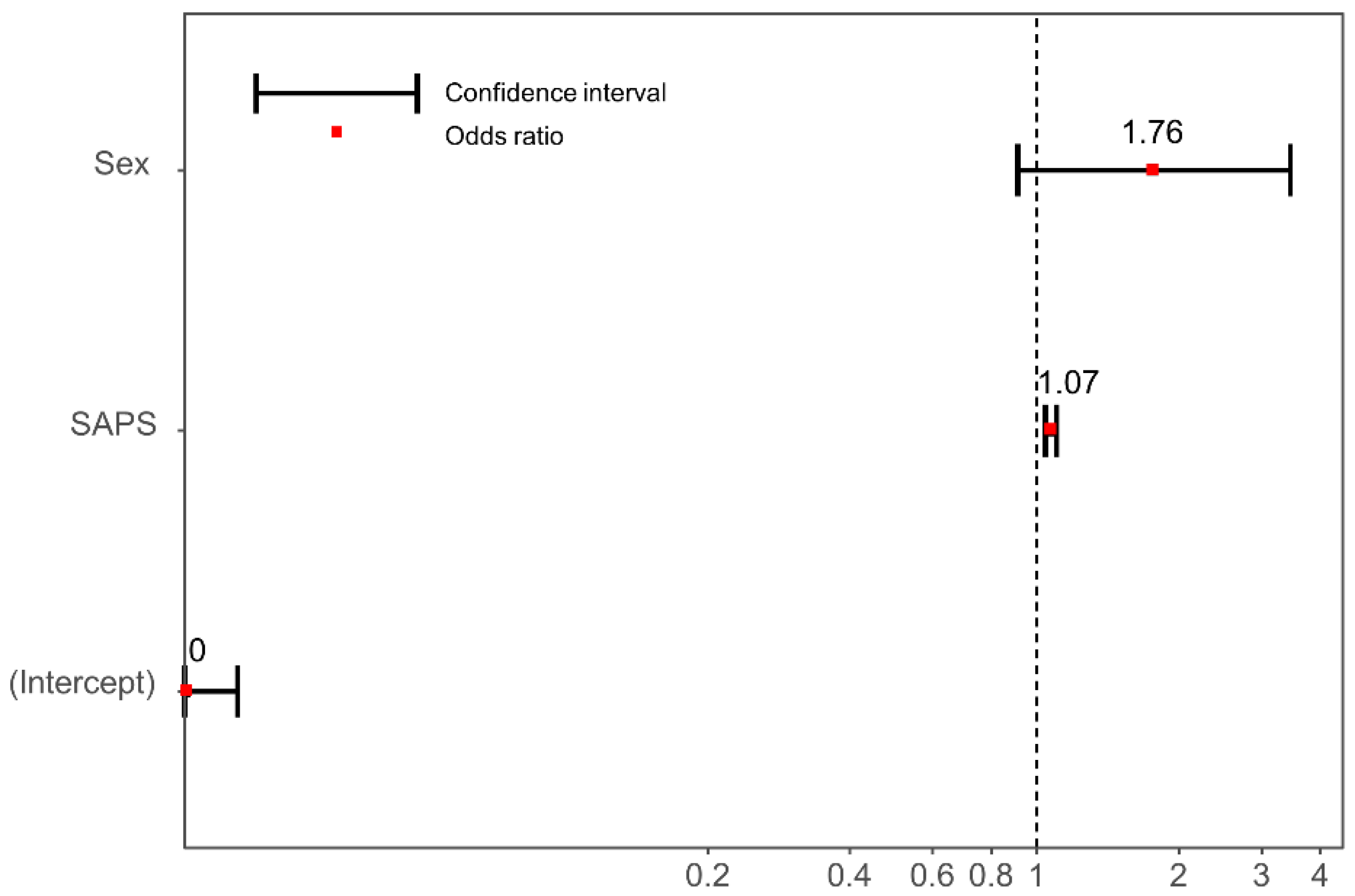
3.4. Multivariable Logistic Regression to Identify Independent Risk Factors of Mortality
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Zhu, N.; Zhang, D.; Wang, W.; Li, X.; Yang, B.; Song, J.; Zhao, X.; Huang, B.; Shi, W.; Lu, R.; et al. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N. Engl. J. Med. 2020, 382, 727–733. [Google Scholar] [CrossRef] [PubMed]
- Korea Disease Control and Prevention Agency. Coronavirus Disease-19, Republic of Korea. Available online: http://ncov.mohw.go.kr/en/ (accessed on 12 June 2020).
- Korea Disease Control and Prevention Agency. COVID-19 Report. Available online: http://ncov.mohw.go.kr/en/tcmBoardView.do?brdId=12&brdGubun=125&dataGubun=&ncvContSeq=1278&contSeq=1278&board_id=&gubun (accessed on 22 November 2021).
- Choi, A.; Kim, H.Y.; Cho, A.; Noh, J.; Park, I.; Chung, H.S. Efficacy of a four-tier infection response system in the emergency department during the coronavirus disease-2019 outbreak. PLoS ONE 2021, 16, e0256116. [Google Scholar] [CrossRef] [PubMed]
- Mafham, M.M.; Spata, E.; Goldacre, R.; Gair, D.; Curnow, P.; Bray, M.; Hollings, S.; Roebuck, C.; Gale, C.P.; A Mamas, M.; et al. COVID-19 pandemic and admission rates for and management of acute coronary syndromes in England. Lancet 2020, 396, 381–389. [Google Scholar] [CrossRef]
- Lange, S.J.; Ritchey, M.D.; Goodman, A.B.; Dias, T.; Twentyman, E.; Fuld, J.; Schieve, L.A.; Imperatore, G.; Benoit, S.R.; Kite-Powell, A.; et al. Potential indirect effects of the COVID-19 pandemic on use of emergency departments for acute life-threatening conditions—United States, January–May 2020. Am. J. Transplant. 2020, 20, 2612–2617. [Google Scholar] [CrossRef] [PubMed]
- Masroor, S. Collateral damage of COVID-19 pandemic: Delayed medical care. J. Card. Surg. 2020, 35, 1345–1347. [Google Scholar] [CrossRef] [PubMed]
- Sung, C.-W.; Lu, T.-C.; Fang, C.-C.; Huang, C.-H.; Chen, W.-J.; Chen, S.-C.; Tsai, C.-L. Impact of COVID-19 pandemic on emergency department services acuity and possible collateral damage. Resuscitation 2020, 153, 185–186. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.E.; Ro, Y.S.; Ryoo, H.W.; Moon, S. Impact of temporary closures of emergency departments during the COVID-19 outbreak on clinical outcomes for emergency patients in a metropolitan area. Am. J. Emerg. Med. 2021, 47, 35–41. [Google Scholar] [CrossRef] [PubMed]
- De Rosa, S.; Spaccarotella, C.; Basso, C.; Calabrò, M.P.; Curcio, A.; Filardi, P.P.; Mancone, M.; Mercuro, G.; Muscoli, S.; Nodari, S.; et al. Reduction of hospitalizations for myocardial infarction in Italy in the COVID-19 era. Eur. Heart J. 2020, 41, 2083–2088. [Google Scholar] [CrossRef] [PubMed]
- Meza, H.T.; Gil, L.; Saldaña, A.S.; Martínez-Zabaleta, M.; Juez, P.D.L.R.; Martínez, E.L.-C.; Apilánez, M.C.; Isasi, M.H.; Enguita, J.M.; Alfonso, M.D.L.; et al. Impact of COVID-19 outbreak on ischemic stroke admissions and in-hospital mortality in North-West Spain. Int. J. Stroke 2020, 15, 755–762. [Google Scholar] [CrossRef] [PubMed]
- Evans, L.; Rhodes, A.; Alhazzani, W.; Antonelli, M.; Coopersmith, C.M.; French, C.; Machado, F.R.; Mcintyre, L.; Ostermann, M.; Prescott, H.C.; et al. Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock 2021. Crit. Care Med. 2021, 49, e1063–e1143. [Google Scholar] [CrossRef] [PubMed]
- Korea Disease Control and Prevention Agency. Infectious Disease Alert Level. C. Korea and C. f. D. C. Prevention. Available online: http://ncov.mohw.go.kr/tcmBoardView.do?brdId=3&brdGubun=31&dataGubun=&ncvContSeq=583&contSeq=583&board_id=311&gubun=ALL (accessed on 22 November 2021).
- World Health Organization. Clinical management of severe acute respiratory infection when novel coronavirus (2019-nCoV) infection is suspected: Interim guidance, 28 January 2020, Geneva. 2020. Available online: https://apps.who.int/iris/handle/10665/330893 (accessed on 22 November 2021).
- Pécout, C.; Pain, E.; Chekroun, M.; Champeix, C.; Kulak, C.; Prieto, R.; van Vugt, J.; Gilchrist, K.; Lainé-Pellet, A.-F. Impact of the COVID-19 Pandemic on Patients Affected by Non-Communicable Diseases in Europe and in the USA. Int. J. Environ. Res. Public Heal. 2021, 18, 6697. [Google Scholar] [CrossRef] [PubMed]
- Czeisler, M.; Marynak, K.; Clarke, K.E.; Salah, Z.; Shakya, I.; Thierry, J.M.; Ali, N.; McMillan, H.; Wiley, J.F.; Weaver, M.D.; et al. Delay or Avoidance of Medical Care Because of COVID-19–Related Concerns—United States, June 2020. MMWR. Morb. Mortal. Wkly. Rep. 2020, 69, 1250–1257. [Google Scholar] [CrossRef] [PubMed]
- Cho, S.Y.; Kang, J.-M.; Ha, Y.E.; Park, G.E.; Lee, J.Y.; Ko, J.-H.; Kim, J.M.; Kang, C.-I.; Jo, I.J.; Ryu, J.G.; et al. MERS-CoV outbreak following a single patient exposure in an emergency room in South Korea: An epidemiological outbreak study. Lancet 2016, 388, 994–1001. [Google Scholar] [CrossRef] [Green Version]
- Chen, Y.-C.; Huang, L.-M.; Chan, C.-C.; Hsueh, P.-R.; Chang, S.-C.; Chang, Y.-Y.; Chen, M.-L.; Hung, C.-C.; Chen, W.-J.; Lin, F.-Y.; et al. SARS in Hospital Emergency Room. Emerg. Infect. Dis. 2004, 10, 782–788. [Google Scholar] [CrossRef] [PubMed]
- Phua, J.; Weng, L.; Ling, L.; Egi, M.; Lim, C.-M.; Divatia, J.V.; Shrestha, B.R.; Arabi, Y.M.; Ng, J.; Gomersall, C.D.; et al. Intensive care management of coronavirus disease 2019 (COVID-19): Challenges and recommendations. Lancet Respir. Med. 2020, 8, 506–517. [Google Scholar] [CrossRef]
- Razu, S.R.; Yasmin, T.; Arif, T.B.; Islam, S.; Islam, S.M.S.; Gesesew, H.A.; Ward, P. Challenges Faced by Healthcare Professionals During the COVID-19 Pandemic: A Qualitative Inquiry From Bangladesh. Front. Public Heal. 2021, 9, 647315. [Google Scholar] [CrossRef] [PubMed]
- International Labour Organization (ILOSTAT). As the COVID-19 Crisis Puts Pressure on Health Services across the Globe, ILOSTAT Data Highlights the Already Existing Shortages of Halth Workers. Available online: https://ilostat.ilo.org/covid-19-are-there-enough-health-workers/ (accessed on 27 December 2021).
- Bae, S.-J.; Chung, H.-S.; Namgung, M.; Choi, Y.-H.; Min, J.-H.; Lee, D.-H. Comparison of the Clinical Process and Outcomes in Patients after Coronavirus Infection 2019 Outbreak. Medicina 2021, 57, 1086. [Google Scholar] [CrossRef] [PubMed]
- Bauer, M.; Gerlach, H.; Vogelmann, T.; Preissing, F.; Stiefel, J.; Adam, D. Mortality in sepsis and septic shock in Europe, North America and Australia between 2009 and 2019—results from a systematic review and meta-analysis. Crit. Care 2020, 24, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Abe, T.; Ogura, H.; Kushimoto, S.; Shiraishi, A.; Sugiyama, T.; Deshpande, G.A.; Uchida, M.; Nagata, I.; Saitoh, D.; Fujishima, S.; et al. Variations in infection sites and mortality rates among patients in intensive care units with severe sepsis and septic shock in Japan. J. Intensiv. Care 2019, 7, 1–9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Characteristics | Pre-COVID-19 (N = 121) | Post-COVID-19-Onset (N = 95) | Total (N = 216) | p-Value |
|---|---|---|---|---|
| Sex, Male | 62 (51.2%) | 46 (48.4%) | 108 (50.0%) | 0.681 |
| Age (years) | 75. 4± 12.7 | 75.4 ± 13.1 | 75.4 ± 12.9 | 0.979 |
| Form of ED arrival | ||||
| Direct visit Transfer-in | 48 (39.7%) 73 (60.3%) | 46 (48.4%) 49 (51.6%) | 94 (43.5%) 122 (56.5%) | 0.198 |
| Time from onset to ED arrival (h) | 8.7 (2.9–18.2) | 10.6 (2.3–68.8) | 9.4 (2.7–35.7) | 0.090 |
| qSOFA score | 1.4 ± 0.8 | 1.4 ± 0.9 | 1.4 ± 0.8 | 0.849 |
| SAPS III | 63.8 ± 15.5 | 67.1 ± 15.0 | 65.2 ± 15.3 | 0.114 |
| Comorbidities | ||||
| Hypertension | 66 (54.5%) | 39 (41.1%) | 105 (48.6%) | 0.049 |
| Diabetes | 38 (31.4%) | 36 (37.9%) | 74 (34.3%) | 0.318 |
| Cerebrovascular disease | 25 (20.7%) | 17 (17.9%) | 42 (19.4%) | 0.610 |
| Malignancy | 22 (18.2%) | 21 (22.1%) | 43 (19.9%) | 0.474 |
| Cardiovascular disease | 14 (11.6%) | 12 (12.6%) | 26 (12.0%) | 0.812 |
| Chronic liver disease | 7 (5.8%) | 7 (7.4%) | 14 (6.5%) | 0.639 |
| Chronic renal disease | 6 (5.0%) | 13 (13.7%) | 19 (8.8%) | 0.025 |
| Chronic lung disease | 4 (3.3%) | 6 (6.3%) | 10 (4.6%) | 0.296 |
| Time from ED arrival to blood culture (h) | 1.1 ± 0.9 | 1.1 ± 0.9 | 0.592 | |
| Time from ED arrival to administration of antibiotics (h) | 2.4 ± 1.6 | 2.2 ± 1.3 | 0.288 | |
| Time from ED arrival to CT (h) (n = 158) | 2.9 ± 1.0 (n = 90) | 3.2 ± 1.6 (n = 68) | 0.136 | |
| Time from ED arrival to emergency intervention (h) (n = 18) | 5.6 ± 3.9 (n = 10) | 3.9 ± 1.1 (n = 8) | 0.267 | |
| Infection site | ||||
| Respiratory | 47 (38.8%) | 25 (26.3%) | 72 (33.3%) | 0.053 |
| Urinary | 45 (37.2%) | 47 (49.5%) | 92 (42.6%) | 0.070 |
| Hepatobiliary | 16 (13.2%) | 15 (15.8%) | 31 (14.4%) | 0.593 |
| Gastrointestinal | 9 (7.4%) | 10 (10.5%) | 19 (8.8%) | 0.426 |
| Bone or soft tissue | 6 (5.0%) | 3 (3.2%) | 9 (4.2%) | 0.511 |
| Other or unknown | 8 (6.6%) | 6 (6.3%) | 14 (6.5%) | 0.930 |
| Duration of ED stay (h) | 5.0 ± 2.3 | 5.9 ± 3.0 | 0.015 | |
| Admission type (n = 215) 1 | ||||
| ICU Ward | 96 (79.3%) 24 (20.7%) | 63 (66.3%) 32 (33.7%) | 159 (73.6%) 56 (36.4%) | 0.023 |
| Characteristics | Pre–COVID-19 (N = 121) | Post-COVID-19-Onset (N = 95) | p-Value |
|---|---|---|---|
| Mortality | 30 (24.8%) | 34 (35.8%) | 0.079 |
| Duration of vasopressor use (days) | 3.3 ± 3.3 | 4.3 ± 4.8 | 0.057 |
| Application of mechanical ventilation | 38 (31.4%) | 22 (23.2%) | 0.179 |
| Duration of mechanical ventilation (days) | 7.8 ± 9.8 | 7.2 ± 7.1 | 0.798 |
| Application of CRRT | 21 (17.4%) | 17 (17.9%) | 0.918 |
| Duration of CRRT (days) | 3.7 ± 3.7 | 7.7 ± 9.8 | 0.129 |
| Duration of ICU stay (days) (n = 159) | 4.0 (3.0–9.0) (n = 96) | 5.0 (3.0–8.0) (n = 63) | 0.667 |
| Duration of total hospitalization (days) | 15.0 (8.0–26.0) | 15.0 (7.0–28.0) | 0.831 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, J.H.; Ahn, C.; Namgung, M. Comparative Evaluation of the Prognosis of Septic Shock Patients from Before to After the Onset of the COVID-19 Pandemic: A Retrospective Single-Center Clinical Analysis. J. Pers. Med. 2022, 12, 103. https://doi.org/10.3390/jpm12010103
Kim JH, Ahn C, Namgung M. Comparative Evaluation of the Prognosis of Septic Shock Patients from Before to After the Onset of the COVID-19 Pandemic: A Retrospective Single-Center Clinical Analysis. Journal of Personalized Medicine. 2022; 12(1):103. https://doi.org/10.3390/jpm12010103
Chicago/Turabian StyleKim, Jae Hwan, Chiwon Ahn, and Myeong Namgung. 2022. "Comparative Evaluation of the Prognosis of Septic Shock Patients from Before to After the Onset of the COVID-19 Pandemic: A Retrospective Single-Center Clinical Analysis" Journal of Personalized Medicine 12, no. 1: 103. https://doi.org/10.3390/jpm12010103
APA StyleKim, J. H., Ahn, C., & Namgung, M. (2022). Comparative Evaluation of the Prognosis of Septic Shock Patients from Before to After the Onset of the COVID-19 Pandemic: A Retrospective Single-Center Clinical Analysis. Journal of Personalized Medicine, 12(1), 103. https://doi.org/10.3390/jpm12010103







