Application of Artificial Intelligence in COVID-19 Diagnosis and Therapeutics
Abstract
:1. Introduction
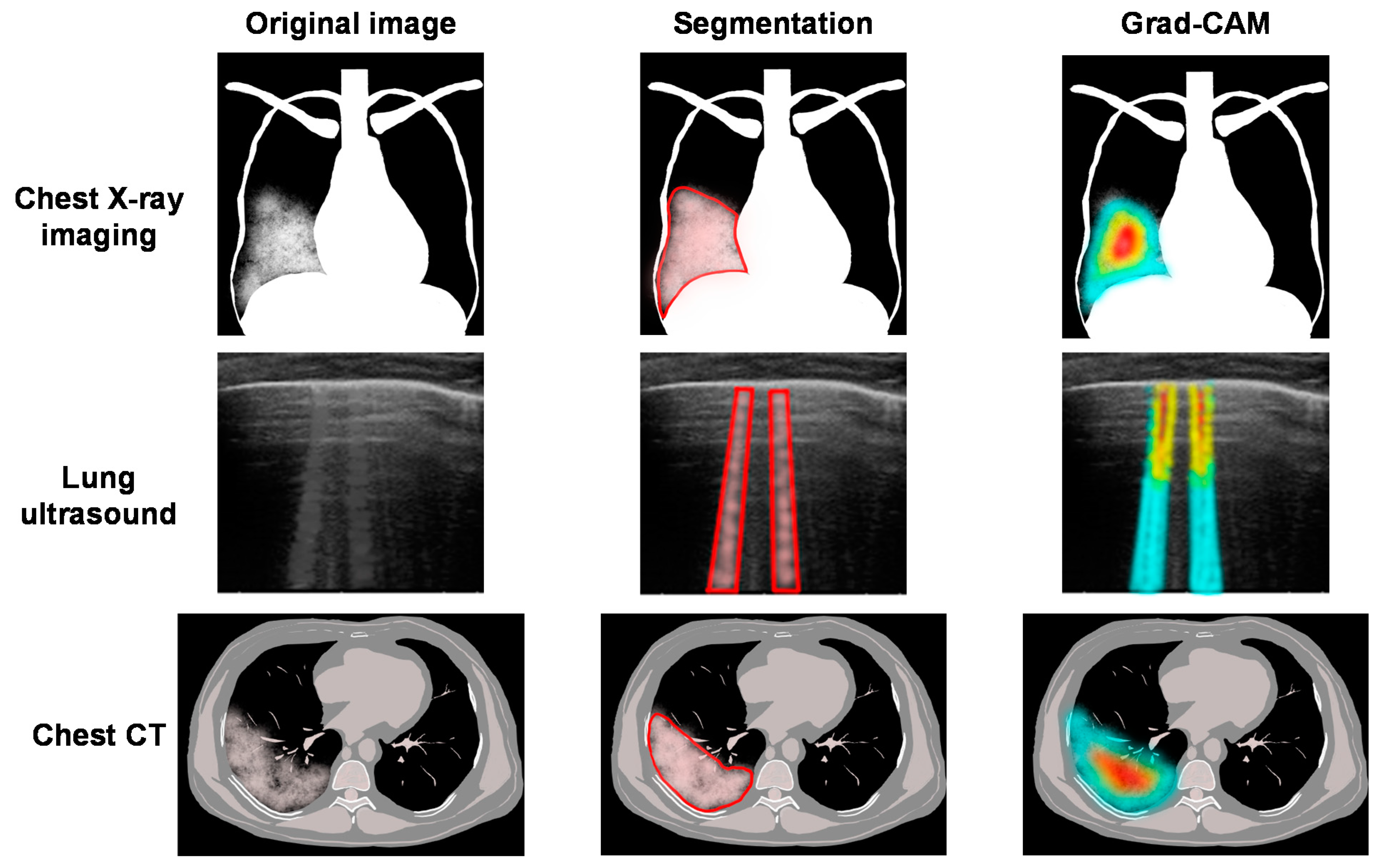
2. Medical Imaging Analysis
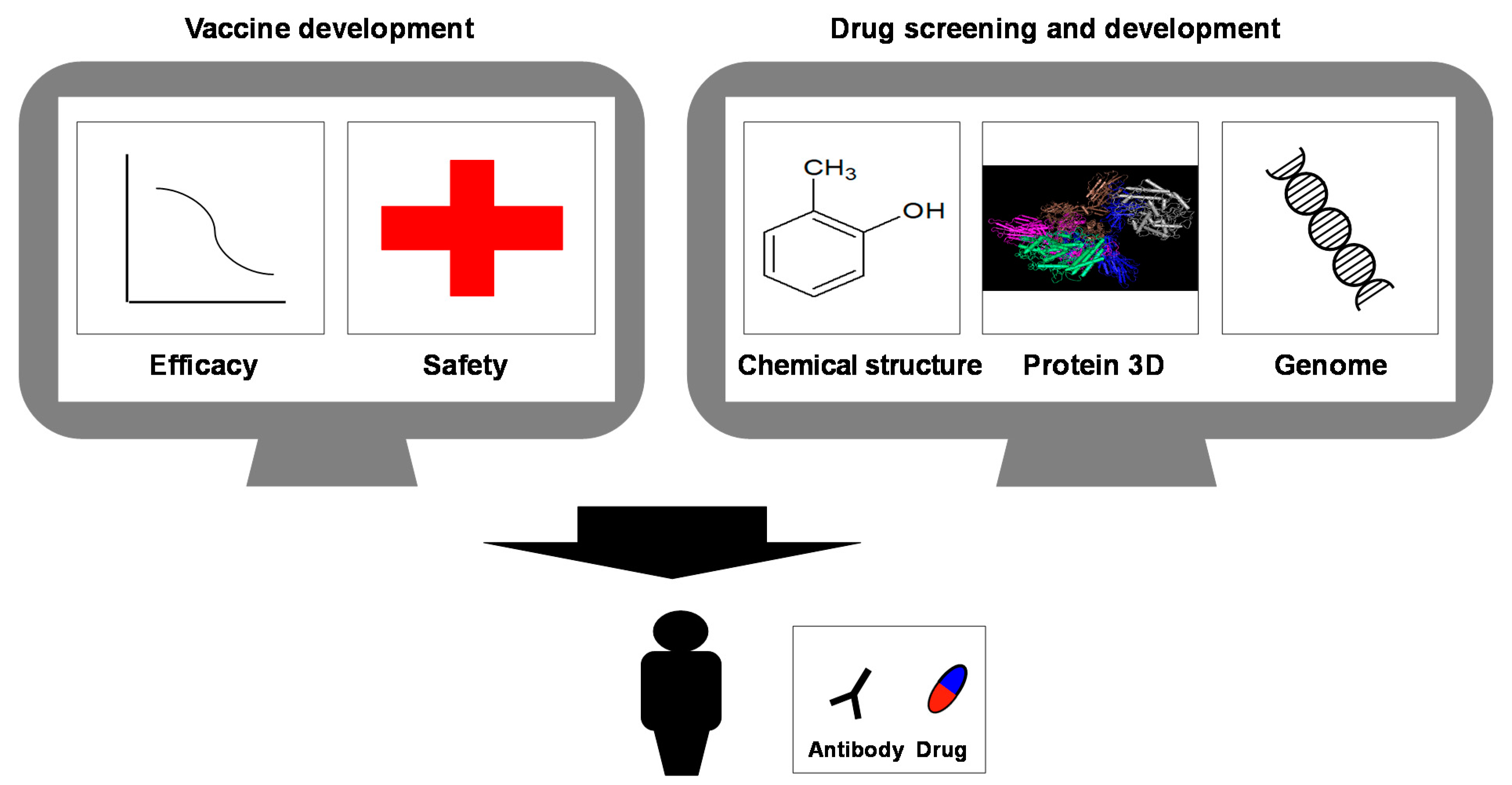
3. Drug Discovery and Vaccine Development
3.1. General Background for the Vaccine
3.2. AI-Driven Drug Discovery
4. Public Health
4.1. AI Used in Public Health Decision-Making
| Tasks of ML Models | Models Used in the Study | References |
|---|---|---|
| Determine a new daily cases peak with a forecasted curve | Modified autoencoder and SEIR compartment model | Distante et al. [103] |
| Forecast the spread of infection | First-principles epidemiological equations and neural network model | Dandekar et al. [104] |
| Detect early warning indicators (EWIs) | Neural network model | Uhlig et al. [105] |
| Long-term prediction and estimation of the number of asymptomatic infections | ML-based fine-grained simulator (ML-Sim) | Yu et al. [106] |
| (1) Predict new confirmed cases, (2) predict how many cases end in death, and (3) provide joint predictions of cases, deaths, and recoveries | Bayesian time series model and a random forest algorithm within an epidemiological compartmental model | Watson et al. [107] |
| Predict the strength and timing of the peak of the COVID-19 epidemic in Iran and the total number of cases expected during the epidemic | (1) Random forest, (2) multi-layer perceptron, and (3) LSTM | Kafieh et al. [108] |
| Generate forecasts of disease outbreak | PNN + cf | Fong et al. [109] |
| Predict the COVID-19 infection status in various regions and countries of the world | Variational LSTM autoencoder model | Ibrahim et al. [110] |
| Predict the number of confirmed cases in the short term | Adaptive neuro-fuzzy inference system using an enhanced flower pollination algorithm and salp swarm algorithm | Al-Qaness et al. [111] |
| Regression of the daily infection cases over the coming 24 days | XGBoost and MultiOutputRegressor | Suzuki et al. [112] |
| Combine health, demographic, and geographic characteristics to predict the near-future infection risk at county level | Three-stage XGBoost modeling process | Mehta et al. [113] |
| Early identification of the spread of COVID-19 | DNN classifier using pre-trained bidirectional encoder representations from transformers (BERT) | Klein et al. and Golder et al. [114,115] |
| Identify abnormalities in the incidence of the disease | Determine the parameters that minimize mean absolute error | Chamberlain et al. [116] |
| Predict of influenza-like illnesses | Importance contribution index for various feature selection and pattern classification approaches | Pei et al. [117] |
| Ultra-fast COVID-19 virus genome signature analysis with the alignment-free approach | Supervised ML with digital signal processing | Randhawa et al. [118] |
| Detect fever and cyanosis; estimate heart rate and respiratory effort | Person detection using algorithms based on DL | Hegde et al. [119] |
| Distinguish COVID-19 coughs from non-COVID-19 coughs | Domain recognition AI engine | Imran et al. [120] |
| Estimate the probability that an individual will test positive for COVID-19 based on the responses to nine simple questions related to SARS-CoV-2 infection | Logistic regression models and gradient boosting decision trees models | Shoer et al. [121] |
4.2. Models for Predicting the Dynamics of Infectious Diseases and the Effects of Interventions

4.3. Surveillance and Outbreak Detection
4.4. Scalable Real-Time Screening Tools
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Chan, J.F.-W.; Yuan, S.; Kok, K.-H.; To, K.K.-W.; Chu, H.; Yang, J.; Xing, F.; Liu, J.; Yip, C.C.-Y.; Poon, R.W.-S.; et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: A study of a family cluster. Lancet 2020, 395, 514–523. [Google Scholar] [CrossRef] [Green Version]
- Gkiouras, K.; Nigdelis, M.P.; Grammatikopoulou, M.G.; Goulis, D.G. Tracing open data in emergencies: The case of the COVID-19 pandemic. Eur. J. Clin. Investig. 2020, 50, e13323. [Google Scholar] [CrossRef]
- Mughees, M.; Chugh, H.; Naqvi, S.H.; Wajid, S. COVID-19 threat to the world: Current and possible diagnostic/treatment strategies. Crit. Rev. Biomed. Eng. 2021, 49, 21–33. [Google Scholar] [CrossRef]
- Wouters, O.J.; Shadlen, K.C.; Salcher-Konrad, M.; Pollard, A.J.; Larson, H.J.; Teerawattananon, Y.; Jit, M. Challenges in ensuring global access to COVID-19 vaccines: Production, affordability, allocation, and deployment. Lancet 2021, 397, 1023–1034. [Google Scholar] [CrossRef]
- Kashte, S.; Gulbake, A.; El-Amin, S.F., III; Gupta, A. COVID-19 vaccines: Rapid development, implications, challenges and future prospects. Hum. Cell 2021, 34, 711–733. [Google Scholar] [CrossRef] [PubMed]
- Lazarevic, I.; Pravica, V.; Miljanovic, D.; Cupic, M. Immune evasion of SARS-CoV-2 emerging variants: What have we learnt so far? Viruses 2021, 13, 1192. [Google Scholar] [CrossRef]
- Rashed, E.A.; Hirata, A. Infectivity Upsurge by COVID-19 viral variants in Japan: Evidence from deep learning modeling. Int. J. Environ. Res. Public Health 2021, 18, 7799. [Google Scholar] [CrossRef] [PubMed]
- Layne, S.P.; Taubenberger, J.K. Increasing threats from SARS-CoV-2 variants: Time to establish global surveillance. Sci. Transl. Med. 2021, 13, eabj6984. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, H.; Hirayama, A.; Nagai, H.; Shirai, C.; Takahashi, Y.; Shinomiya, H.; Taniguchi, C.; Ogata, T. Increased transmissibility of the SARS-CoV-2 alpha variant in a japanese population. Int. J. Environ. Res. Public Health 2021, 18, 7752. [Google Scholar] [CrossRef] [PubMed]
- Salleh, M.Z.; Derrick, J.P.; Deris, Z.Z. Structural evaluation of the spike glycoprotein variants on SARS-CoV-2 transmission and immune evasion. Int. J. Mol. Sci. 2021, 22, 7425. [Google Scholar] [CrossRef]
- Chatterjee, S.; Mishra, S.; Chowdhury, K.D.; Ghosh, C.K.; Saha, K.D. Various theranostics and immunization strategies based on nanotechnology against Covid-19 pandemic: An interdisciplinary view. Life Sci. 2021, 278, 119580. [Google Scholar] [CrossRef]
- Quek, E.; Tahir, H.; Kumar, P.; Hastings, R.; Jha, R. Treatment of COVID-19: A review of current and prospective pharmacotherapies. Br. J. Hosp. Med. 2021, 82, 1–9. [Google Scholar] [CrossRef]
- Siemieniuk, R.A.; Bartoszko, J.J.; Ge, L.; Zeraatkar, D.; Izcovich, A.; Kum, E.; Pardo-Hernandez, H.; Qasim, A.; Martinez, J.P.D.; Rochwerg, B.; et al. Drug treatments for covid-19: Living systematic review and network meta-analysis. BMJ 2020, 370, m2980. [Google Scholar] [CrossRef]
- Kim, P.S.; Read, S.W.; Fauci, A.S. Therapy for early COVID-19: A critical need. JAMA 2020, 324, 2149–2150. [Google Scholar] [CrossRef]
- Hamamoto, R.; Suvarna, K.; Yamada, M.; Kobayashi, K.; Shinkai, N.; Miyake, M.; Takahashi, M.; Jinnai, S.; Shimoyama, R.; Sakai, A.; et al. Application of artificial intelligence technology in oncology: Towards the establishment of precision medicine. Cancers 2020, 12, 3532. [Google Scholar] [CrossRef]
- Asada, K.; Kaneko, S.; Takasawa, K.; Machino, H.; Takahashi, S.; Shinkai, N.; Shimoyama, R.; Komatsu, M.; Hamamoto, R. Integrated analysis of whole genome and epigenome data using machine learning technology: Toward the establishment of precision oncology. Front. Oncol. 2021, 11, 666937. [Google Scholar] [CrossRef]
- Asada, K.; Kobayashi, K.; Joutard, S.; Tubaki, M.; Takahashi, S.; Takasawa, K.; Komatsu, M.; Kaneko, S.; Sese, J.; Hamamoto, R. Uncovering prognosis-related genes and pathways by multi-omics analysis in lung cancer. Biomolecules 2020, 10, 524. [Google Scholar] [CrossRef] [Green Version]
- Hamamoto, R.; Komatsu, M.; Takasawa, K.; Asada, K.; Kaneko, S. Epigenetics analysis and integrated analysis of multiomics data, including epigenetic data, using artificial intelligence in the era of precision medicine. Biomolecules 2020, 10, 62. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jinnai, S.; Yamazaki, N.; Hirano, Y.; Sugawara, Y.; Ohe, Y.; Hamamoto, R. The development of a skin cancer classification system for pigmented skin lesions using deep learning. Biomolecules 2020, 10, 1123. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, K.; Bolatkan, A.; Shiina, S.; Hamamoto, R. Fully-connected neural networks with reduced parameterization for predicting histological types of lung cancer from somatic mutations. Biomolecules 2020, 10, 1249. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, S.; Asada, K.; Takasawa, K.; Shimoyama, R.; Sakai, A.; Bolatkan, A.; Shinkai, N.; Kobayashi, K.; Komatsu, M.; Kaneko, S.; et al. Predicting deep learning based multi-omics parallel integration survival subtypes in lung cancer using reverse phase protein array data. Biomolecules 2020, 10, 1460. [Google Scholar] [CrossRef]
- Takahashi, S.; Takahashi, M.; Kinoshita, M.; Miyake, M.; Kawaguchi, R.; Shinojima, N.; Mukasa, A.; Saito, K.; Nagane, M.; Otani, R.; et al. Fine-tuning approach for segmentation of gliomas in brain magnetic resonance images with a machine learning method to normalize image differences among facilities. Cancers 2021, 13, 1415. [Google Scholar] [CrossRef]
- Takahashi, S.; Takahashi, M.; Tanaka, S.; Takayanagi, S.; Takami, H.; Yamazawa, E.; Nambu, S.; Miyake, M.; Satomi, K.; Ichimura, K.; et al. A new era of neuro-oncology research pioneered by multi-omics analysis and machine learning. Biomolecules 2021, 11, 565. [Google Scholar] [CrossRef]
- Yamada, M.; Saito, Y.; Imaoka, H.; Saiko, M.; Yamada, S.; Kondo, H.; Takamaru, H.; Sakamoto, T.; Sese, J.; Kuchiba, A.; et al. Development of a real-time endoscopic image diagnosis support system using deep learning technology in colonoscopy. Sci. Rep. 2019, 9, 14465. [Google Scholar] [CrossRef] [Green Version]
- Yamada, M.; Saito, Y.; Yamada, S.; Kondo, H.; Hamamoto, R. Detection of flat colorectal neoplasia by artificial intelligence: A systematic review. Best Pract. Res. Clin. Gastroenterol. 2021, 101745. [Google Scholar] [CrossRef] [PubMed]
- Dozen, A.; Komatsu, M.; Sakai, A.; Komatsu, R.; Shozu, K.; Machino, H.; Yasutomi, S.; Arakaki, T.; Asada, K.; Kaneko, S.; et al. Image segmentation of the ventricular septum in fetal cardiac ultrasound videos based on deep learning using time-series information. Biomolecules 2020, 10, 1526. [Google Scholar] [CrossRef] [PubMed]
- Hamamoto, R. Application of artificial intelligence for medical research. Biomolecules 2021, 11, 90. [Google Scholar] [CrossRef]
- Kawaguchi, R.K.; Takahashi, M.; Miyake, M.; Kinoshita, M.; Takahashi, S.; Ichimura, K.; Hamamoto, R.; Narita, Y.; Sese, J. Assessing versatile machine learning models for glioma radiogenomic studies across hospitals. Cancers 2021, 13, 611. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, K.; Miyake, M.; Takahashi, M.; Hamamoto, R. Observing deep radiomics for the classification of glioma grades. Sci. Rep. 2021, 11, 10942. [Google Scholar] [CrossRef]
- Komatsu, M.; Sakai, A.; Dozen, A.; Shozu, K.; Yasutomi, S.; Machino, H.; Asada, K.; Kaneko, S.; Hamamoto, R. Towards clinical application of artificial intelligence in ultrasound imaging. Biomedicines 2021, 9, 720. [Google Scholar] [CrossRef]
- Komatsu, M.; Sakai, A.; Komatsu, R.; Matsuoka, R.; Yasutomi, S.; Shozu, K.; Dozen, A.; Machino, H.; Hidaka, H.; Arakaki, T.; et al. Detection of cardiac structural abnormalities in fetal ultrasound videos using deep learning. Appl. Sci. 2021, 11, 371. [Google Scholar] [CrossRef]
- Shozu, K.; Komatsu, M.; Sakai, A.; Komatsu, R.; Dozen, A.; Machino, H.; Yasutomi, S.; Arakaki, T.; Asada, K.; Kaneko, S.; et al. Model-agnostic method for thoracic wall segmentation in fetal ultrasound videos. Biomolecules 2020, 10, 1691. [Google Scholar] [CrossRef]
- Yasutomi, S.; Arakaki, T.; Matsuoka, R.; Sakai, A.; Komatsu, R.; Shozu, K.; Dozen, A.; Machino, H.; Asada, K.; Kaneko, S.; et al. Shadow estimation for ultrasound images using auto-encoding structures and synthetic shadows. Appl. Sci. 2021, 11, 1127. [Google Scholar] [CrossRef]
- Akl, E.A.; Blažić, I.; Yaacoub, S.; Frija, G.; Chou, R.; Appiah, J.A.; Fatehi, M.; Flor, N.; Hitti, E.; Jafri, H.; et al. Use of chest imaging in the diagnosis and management of COVID-19: A WHO rapid advice guide. Radiology 2021, 298, E63–E69. [Google Scholar] [CrossRef]
- Minaee, S.; Kafieh, R.; Sonka, M.; Yazdani, S.; Jamalipour Soufi, G. Deep-COVID: Predicting COVID-19 from chest X-ray images using deep transfer learning. Med. Image Anal. 2020, 65, 101794. [Google Scholar] [CrossRef]
- Oh, Y.; Park, S.; Ye, J.C. Deep learning COVID-19 features on CXR using limited training data sets. IEEE Trans. Med. Imaging 2020, 39, 2688–2700. [Google Scholar] [CrossRef] [PubMed]
- Signoroni, A.; Savardi, M.; Benini, S.; Adami, N.; Leonardi, R.; Gibellini, P.; Vaccher, F.; Ravanelli, M.; Borghesi, A.; Maroldi, R.; et al. BS-Net: Learning COVID-19 pneumonia severity on a large chest X-ray dataset. Med. Image Anal. 2021, 71, 102046. [Google Scholar] [CrossRef] [PubMed]
- Kulkarni, A.R.; Athavale, A.M.; Sahni, A.; Sukhal, S.; Saini, A.; Itteera, M.; Zhukovsky, S.; Vernik, J.; Abraham, M.; Joshi, A.; et al. Deep learning model to predict the need for mechanical ventilation using chest X-ray images in hospitalised patients with COVID-19. BMJ Innov. 2021, 7, 261–270. [Google Scholar] [CrossRef]
- Zandehshahvar, M.; van Assen, M.; Maleki, H.; Kiarashi, Y.; De Cecco, C.N.; Adibi, A. Toward understanding COVID-19 pneumonia: A deep-learning-based approach for severity analysis and monitoring the disease. Sci. Rep. 2021, 11, 11112. [Google Scholar] [CrossRef] [PubMed]
- Cheung, J.C.-H.; Lam, K.N. POCUS in COVID-19: Pearls and pitfalls. Lancet Respir. Med. 2020, 8, e34. [Google Scholar] [CrossRef]
- Lichtenstein, D.A.; Mezière, G.A.; Lagoueyte, J.-F.; Biderman, P.; Goldstein, I.; Gepner, A. A-lines and B-lines: Lung ultrasound as a bedside tool for predicting pulmonary artery occlusion pressure in the critically ill. Chest 2009, 136, 1014–1020. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Roy, S.; Menapace, W.; Oei, S.; Luijten, B.; Fini, E.; Saltori, C.; Huijben, I.; Chennakeshava, N.; Mento, F.; Sentelli, A.; et al. Deep learning for classification and localization of COVID-19 markers in point-of-care lung ultrasound. IEEE Trans. Med. Imaging 2020, 39, 2676–2687. [Google Scholar] [CrossRef]
- Dastider, A.G.; Sadik, F.; Fattah, S.A. An integrated autoencoder-based hybrid CNN-LSTM model for COVID-19 severity prediction from lung ultrasound. Comput. Biol. Med. 2021, 132, 104296. [Google Scholar] [CrossRef]
- Xue, W.; Cao, C.; Liu, J.; Duan, Y.; Cao, H.; Wang, J.; Tao, X.; Chen, Z.; Wu, M.; Zhang, J.; et al. Modality alignment contrastive learning for severity assessment of COVID-19 from lung ultrasound and clinical information. Med. Image Anal. 2021, 69, 101975. [Google Scholar] [CrossRef] [PubMed]
- Bonow, R.O.; O’Gara, P.T.; Yancy, C.W. Cardiology and COVID-19. JAMA 2020, 324, 1131–1132. [Google Scholar] [CrossRef]
- Zhang, K.; Liu, X.; Shen, J.; Li, Z.; Sang, Y.; Wu, X.; Zha, Y.; Liang, W.; Wang, C.; Wang, K. Clinically applicable AI system for accurate diagnosis, quantitative measurements, and prognosis of COVID-19 pneumonia using computed tomography. Cell 2020, 181, 1423–1433.e11. [Google Scholar] [CrossRef]
- Harmon, S.A.; Sanford, T.H.; Xu, S.; Turkbey, E.B.; Roth, H.; Xu, Z.; Yang, D.; Myronenko, A.; Anderson, V.; Amalou, A.; et al. Artificial intelligence for the detection of COVID-19 pneumonia on chest CT using multinational datasets. Nat. Commun. 2020, 11, 4080. [Google Scholar] [CrossRef] [PubMed]
- Jin, C.; Chen, W.; Cao, Y.; Xu, Z.; Tan, Z.; Zhang, X.; Deng, L.; Zheng, C.; Zhou, J.; Shi, H.; et al. Development and evaluation of an artificial intelligence system for COVID-19 diagnosis. Nat. Commun. 2020, 11, 5088. [Google Scholar] [CrossRef]
- Chao, H.; Fang, X.; Zhang, J.; Homayounieh, F.; Arru, C.D.; Digumarthy, S.R.; Babaei, R.; Mobin, H.K.; Mohseni, I.; Saba, L.; et al. Integrative analysis for COVID-19 patient outcome prediction. Med. Image Anal. 2021, 67, 101844. [Google Scholar] [CrossRef]
- Wu, X.; Chen, C.; Zhong, M.; Wang, J.; Shi, J. COVID-AL: The diagnosis of COVID-19 with deep active learning. Med. Image Anal. 2021, 68, 101913. [Google Scholar] [CrossRef]
- Li, Z.; Zhao, W.; Shi, F.; Qi, L.; Xie, X.; Wei, Y.; Ding, Z.; Gao, Y.; Wu, S.; Liu, J.; et al. A novel multiple instance learning framework for COVID-19 severity assessment via data augmentation and self-supervised learning. Med. Image Anal. 2021, 69, 101978. [Google Scholar] [CrossRef]
- Lassau, N.; Ammari, S.; Chouzenoux, E.; Gortais, H.; Herent, P.; Devilder, M.; Soliman, S.; Meyrignac, O.; Talabard, M.P.; Lamarque, J.P.; et al. Integrating deep learning CT-scan model, biological and clinical variables to predict severity of COVID-19 patients. Nat. Commun. 2021, 12, 634. [Google Scholar] [CrossRef] [PubMed]
- Goncharov, M.; Pisov, M.; Shevtsov, A.; Shirokikh, B.; Kurmukov, A.; Blokhin, I.; Chernina, V.; Solovev, A.; Gombolevskiy, V.; Morozov, S.; et al. CT-Based COVID-19 triage: Deep multitask learning improves joint identification and severity quantification. Med. Image Anal. 2021, 71, 102054. [Google Scholar] [CrossRef] [PubMed]
- Wang, R.; Jiao, Z.; Yang, L.; Choi, J.W.; Xiong, Z.; Halsey, K.; Tran, T.M.L.; Pan, I.; Collins, S.A.; Feng, X.; et al. Artificial intelligence for prediction of COVID-19 progression using CT imaging and clinical data. Eur. Radiol. 2021, 659, 1–8. [Google Scholar] [CrossRef]
- Hu, K.; Huang, Y.; Huang, W.; Tan, H.; Chen, Z.; Zhong, Z.; Li, X.; Zhang, Y.; Gao, X. Deep supervised learning using self-adaptive auxiliary loss for COVID-19 diagnosis from imbalanced CT images. Neurocomputing 2021, 458, 232–245. [Google Scholar] [CrossRef] [PubMed]
- Arru, C.; Ebrahimian, S.; Falaschi, Z.; Hansen, J.V.; Pasche, A.; Lyhne, M.D.; Zimmermann, M.; Durlak, F.; Mitschke, M.; Carriero, A.; et al. Comparison of deep learning, radiomics and subjective assessment of chest CT findings in SARS-CoV-2 pneumonia. Clin. Imaging 2021, 80, 58–66. [Google Scholar] [CrossRef]
- World Health Organization. COVID-19 Vaccine Tracker and Landscape. Available online: https://www.who.int/publications/m/item/draft-landscape-of-covid-19-candidate-vaccines (accessed on 3 August 2021).
- Our World in Data. Coronavirus (COVID-19) Vaccinations. Available online: https://ourworldindata.org/covid-vaccinations (accessed on 3 August 2021).
- Walsh, E.E.; Frenck, R.W., Jr.; Falsey, A.R.; Kitchin, N.; Absalon, J.; Gurtman, A.; Lockhart, S.; Neuzil, K.; Mulligan, M.J.; Bailey, R.; et al. Safety and immunogenicity of two RNA-based Covid-19 vaccine candidates. N. Engl. J. Med. 2020, 383, 2439–2450. [Google Scholar] [CrossRef]
- Liu, J.; Liu, Y.; Xia, H.; Zou, J.; Weaver, S.C.; Swanson, K.A.; Cai, H.; Cutler, M.; Cooper, D.; Muik, A.; et al. BNT162b2-elicited neutralization of B.1.617 and other SARS-CoV-2 variants. Nature 2021, 596, 273–275. [Google Scholar] [CrossRef]
- Wang, Z.; Muecksch, F.; Schaefer-Babajew, D.; Finkin, S.; Viant, C.; Gaebler, C.; Hoffmann, H.H.; Barnes, C.O.; Cipolla, M.; Ramos, V.; et al. Naturally enhanced neutralizing breadth against SARS-CoV-2 one year after infection. Nature 2021, 595, 426–431. [Google Scholar] [CrossRef]
- Khoury, D.S.; Cromer, D.; Reynaldi, A.; Schlub, T.E.; Wheatley, A.K.; Juno, J.A.; Subbarao, K.; Kent, S.J.; Triccas, J.A.; Davenport, M.P. Neutralizing antibody levels are highly predictive of immune protection from symptomatic SARS-CoV-2 infection. Nat. Med. 2021, 27, 1205–1211. [Google Scholar] [CrossRef]
- Baden, L.R.; El Sahly, H.M.; Essink, B.; Kotloff, K.; Frey, S.; Novak, R.; Diemert, D.; Spector, S.A.; Rouphael, N.; Creech, C.B.; et al. Efficacy and safety of the mRNA-1273 SARS-CoV-2 vaccine. N. Engl. J. Med. 2021, 384, 403–416. [Google Scholar] [CrossRef]
- Collier, A.Y.; McMahan, K.; Yu, J.; Tostanoski, L.H.; Aguayo, R.; Ansel, J.; Chandrashekar, A.; Patel, S.; Bondzie, E.A.; Sellers, D.; et al. Immunogenicity of COVID-19 mRNA Vaccines in Pregnant and Lactating Women. JAMA 2021, 325, 2370–2380. [Google Scholar] [CrossRef]
- Doria-Rose, N.; Suthar, M.S.; Makowski, M.; O’Connell, S.; McDermott, A.B.; Flach, B.; Ledgerwood, J.E.; Mascola, J.R.; Graham, B.S.; Lin, B.C.; et al. Antibody persistence through 6 months after the second dose of mRNA-1273 vaccine for Covid-19. N. Engl. J. Med. 2021, 384, 2259–2261. [Google Scholar] [CrossRef] [PubMed]
- Greaney, A.J.; Loes, A.N.; Gentles, L.E.; Crawford, K.H.D.; Starr, T.N.; Malone, K.D.; Chu, H.Y.; Bloom, J.D. Antibodies elicited by mRNA-1273 vaccination bind more broadly to the receptor binding domain than do those from SARS-CoV-2 infection. Sci. Transl. Med. 2021, 13. [Google Scholar] [CrossRef] [PubMed]
- Larson, K.F.; Ammirati, E.; Adler, E.D.; Cooper, L.T.; Hong, K.N.; Saponara, G.; Couri, D.; Cereda, A.; Procopio, A.; Cavalotti, C.; et al. Myocarditis after BNT162b2 and mRNA-1273 vaccination. Circulation 2021, 144, 506–508. [Google Scholar] [CrossRef]
- World Health Organization. Tracking SARS-CoV-2 Variants. Available online: https://www.who.int/en/activities/tracking-SARS-CoV-2-variants/ (accessed on 11 August 2021).
- Xie, X.; Liu, Y.; Liu, J.; Zhang, X.; Zou, J.; Fontes-Garfias, C.R.; Xia, H.; Swanson, K.A.; Cutler, M.; Cooper, D.; et al. Neutralization of SARS-CoV-2 spike 69/70 deletion, E484K and N501Y variants by BNT162b2 vaccine-elicited sera. Nat. Med. 2021, 27, 620–621. [Google Scholar] [CrossRef]
- Karim, S.A.; de Oliveira, T. New SARS-CoV-2 variants—Clinical, public health, and vaccine implications. N. Engl. J. Med. 2021, 384, 1866–1868. [Google Scholar] [CrossRef]
- Alter, G.; Yu, J.; Liu, J.; Chandrashekar, A.; Borducchi, E.N.; Tostanoski, L.H.; McMahan, K.; Jacob-Dolan, C.; Martinez, D.R.; Chang, A.; et al. Immunogenicity of Ad26.COV2.S vaccine against SARS-CoV-2 variants in humans. Nature 2021, 596, 268–272. [Google Scholar] [CrossRef] [PubMed]
- Hacisuleyman, E.; Hale, C.; Saito, Y.; Blachere, N.E.; Bergh, M.; Conlon, E.G.; Schaefer-Babajew, D.J.; DaSilva, J.; Muecksch, F.; Gaebler, C.; et al. Vaccine breakthrough infections with SARS-CoV-2 variants. N. Engl. J. Med. 2021, 384, 2212–2218. [Google Scholar] [CrossRef] [PubMed]
- Zhou, D.; Dejnirattisai, W.; Supasa, P.; Liu, C.; Mentzer, A.J.; Ginn, H.M.; Zhao, Y.; Duyvesteyn, H.M.E.; Tuekprakhon, A.; Nutalai, R.; et al. Evidence of escape of SARS-CoV-2 variant B.1.351 from natural and vaccine-induced sera. Cell 2021, 184, 2348–2361.e6. [Google Scholar] [CrossRef] [PubMed]
- Mason, D.M.; Friedensohn, S.; Weber, C.R.; Jordi, C.; Wagner, B.; Meng, S.M.; Ehling, R.A.; Bonati, L.; Dahinden, J.; Gainza, P.; et al. Optimization of therapeutic antibodies by predicting antigen specificity from antibody sequence via deep learning. Nat. Biomed. Eng. 2021, 5, 600–612. [Google Scholar] [CrossRef]
- Chen, B.; Khodadoust, M.S.; Olsson, N.; Wagar, L.E.; Fast, E.; Liu, C.L.; Muftuoglu, Y.; Sworder, B.J.; Diehn, M.; Levy, R.; et al. Predicting HLA class II antigen presentation through integrated deep learning. Nat. Biotechnol. 2019, 37, 1332–1343. [Google Scholar] [CrossRef] [PubMed]
- Fast, E.; Altman, R.B.; Chen, B. Potential T-cell and B-cell epitopes of 1019-nCoV. bioRxiv 2020, 9, 1–9. [Google Scholar] [CrossRef] [Green Version]
- Ripoll, D.R.; Chaudhury, S.; Wallqvist, A. Using the antibody-antigen binding interface to train image-based deep neural networks for antibody-epitope classification. PLoS Comput. Biol. 2021, 17, e1008864. [Google Scholar] [CrossRef] [PubMed]
- Kc, G.B.; Bocci, G.; Verma, S.; Hassan, M.M.; Holmes, J.; Yang, J.J.; Sirimulla, S.; Oprea, T.I. A machine learning platform to estimate anti-SARS-CoV-2 activities. Nat. Mach. Intell. 2021, 3, 527–535. [Google Scholar] [CrossRef]
- Kowalewski, J.; Ray, A. Predicting novel drugs for SARS-CoV-2 using machine learning from a >10 million chemical space. Heliyon 2020, 6, e04639. [Google Scholar] [CrossRef]
- The nCov-Group Data Repository. Available online: https://2019-ncovgroup.github.io/data/ (accessed on 3 August 2021).
- Taguchi, Y.H.; Turki, T. A new advanced in silico drug discovery method for novel coronavirus (SARS-CoV-2) with tensor decomposition-based unsupervised feature extraction. PLoS ONE 2020, 15, e0238907. [Google Scholar] [CrossRef]
- Douangamath, A.; Fearon, D.; Gehrtz, P.; Krojer, T.; Lukacik, P.; Owen, C.D.; Resnick, E.; Strain-Damerell, C.; Aimon, A.; Abranyi-Balogh, P.; et al. Crystallographic and electrophilic fragment screening of the SARS-CoV-2 main protease. Nat. Commun. 2020, 11, 5047. [Google Scholar] [CrossRef]
- Gordon, D.E.; Jang, G.M.; Bouhaddou, M.; Xu, J.; Obernier, K.; White, K.M.; O’Meara, M.J.; Rezelj, V.V.; Guo, J.Z.; Swaney, D.L.; et al. A SARS-CoV-2 protein interaction map reveals targets for drug repurposing. Nature 2020, 583, 459–468. [Google Scholar] [CrossRef]
- Bakowski, M.A.; Beutler, N.; Wolff, K.C.; Kirkpatrick, M.G.; Chen, E.; Nguyen, T.H.; Riva, L.; Shaabani, N.; Parren, M.; Ricketts, J.; et al. Drug repurposing screens identify chemical entities for the development of COVID-19 interventions. Nat. Commun. 2021, 12, 3309. [Google Scholar] [CrossRef]
- Mongia, A.; Saha, S.K.; Chouzenoux, E.; Majumdar, A. A computational approach to aid clinicians in selecting anti-viral drugs for COVID-19 trials. Sci. Rep. 2021, 11, 9047. [Google Scholar] [CrossRef] [PubMed]
- Ke, Y.Y.; Peng, T.T.; Yeh, T.K.; Huang, W.Z.; Chang, S.E.; Wu, S.H.; Hung, H.C.; Hsu, T.A.; Lee, S.J.; Song, J.S.; et al. Artificial intelligence approach fighting COVID-19 with repurposing drugs. Biomed. J. 2020, 43, 355–362. [Google Scholar] [CrossRef] [PubMed]
- An, C.; Lim, H.; Kim, D.W.; Chang, J.H.; Choi, Y.J.; Kim, S.W. Machine learning prediction for mortality of patients diagnosed with COVID-19: A nationwide Korean cohort study. Sci. Rep. 2020, 10, 18716. [Google Scholar] [CrossRef] [PubMed]
- Gao, Y.; Cai, G.Y.; Fang, W.; Li, H.Y.; Wang, S.Y.; Chen, L.; Yu, Y.; Liu, D.; Xu, S.; Cui, P.F.; et al. Machine learning based early warning system enables accurate mortality risk prediction for COVID-19. Nat. Commun. 2020, 11, 5033. [Google Scholar] [CrossRef]
- Li, X.; Ge, P.; Zhu, J.; Li, H.; Graham, J.; Singer, A.; Richman, P.S.; Duong, T.Q. Deep learning prediction of likelihood of ICU admission and mortality in COVID-19 patients using clinical variables. PeerJ 2020, 8, e10337. [Google Scholar] [CrossRef]
- Yan, L.; Zhang, H.-T.; Goncalves, J.; Xiao, Y.; Wang, M.; Guo, Y.; Sun, C.; Tang, X.; Jing, L.; Zhang, M.; et al. An interpretable mortality prediction model for COVID-19 patients. Nat. Mach. Intell. 2020, 2, 283–288. [Google Scholar] [CrossRef]
- Rechtman, E.; Curtin, P.; Navarro, E.; Nirenberg, S.; Horton, M.K. Vital signs assessed in initial clinical encounters predict COVID-19 mortality in an NYC hospital system. Sci. Rep. 2020, 10, 21545. [Google Scholar] [CrossRef]
- Achdout, H.; Aimon, A.; Bar-David, E.; Barr, H.; Ben-Shmuel, A.; Bennett, J.; Bobby, M.L.; Brun, J.; Sarma, B.; Calmiano, M.; et al. COVID moonshot: Open science discovery of SARS-CoV-2 main protease inhibitors by combining crowdsourcing, high-throughput experiments, computational simulations, and machine learning. bioRxiv 2020, 10, 1–10. [Google Scholar] [CrossRef]
- Islam, A.; Beg, O.U.; Persson, B.; Zaidi, Z.H.; Jornvall, H. Primary structure of the hemoglobin alpha-chain of rose-ringed parakeet (Psittacula krameri). J. Protein. Chem. 1988, 7, 561–569. [Google Scholar] [CrossRef]
- Morris, A.; McCorkindale, W.; Consortium, T.C.M.; Drayman, N.; Chodera, J.D.; Tay, S.; London, N.; Lee, A.A. Discovery of SARS-CoV-2 main protease inhibitors using a synthesis-directed de novo design model. Chem. Commun. 2021, 57, 5909–5912. [Google Scholar] [CrossRef]
- Winslow, C.E. The untilled fields of public health. Science 1920, 51, 23–33. [Google Scholar] [CrossRef] [Green Version]
- Syrowatka, A.; Kuznetsova, M.; Alsubai, A.; Beckman, A.L.; Bain, P.A.; Craig, K.J.T.; Hu, J.; Jackson, G.P.; Rhee, K.; Bates, D.W. Leveraging artificial intelligence for pandemic preparedness and response: A scoping review to identify key use cases. NPJ Digit. Med. 2021, 4, 96. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. WHO Coronavirus (COVID-19) Dashboard. Available online: https://covid19.who.int/ (accessed on 5 July 2021).
- Qiu, J. Covert coronavirus infections could be seeding new outbreaks. Nature 2020. [Google Scholar] [CrossRef] [PubMed]
- Dong, Y.; Mo, X.; Hu, Y.; Qi, X.; Jiang, F.; Jiang, Z.; Tong, S. Epidemiology of COVID-19 among children in China. Pediatrics 2020, 145, e20200702. [Google Scholar] [CrossRef] [Green Version]
- Bilinski, A.; Emanuel, E.J. COVID-19 and excess all-cause mortality in the US and 18 comparison countries. JAMA 2020, 324, 2100–2102. [Google Scholar] [CrossRef]
- Morgan, O. How decision makers can use quantitative approaches to guide outbreak responses. Philos. Trans. R. Soc. Lond. B Biol. Sci. 2019, 374, 20180365. [Google Scholar] [CrossRef] [Green Version]
- Bickley, S.J.; Chan, H.F.; Skali, A.; Stadelmann, D.; Torgler, B. How does globalization affect COVID-19 responses? Glob. Health 2021, 17, 57. [Google Scholar] [CrossRef]
- Distante, C.; Pereira, I.G.; Gonçalves, L.M.G.; Piscitelli, P.; Miani, A. Forecasting Covid-19 outbreak progression in italian regions: A model based on neural network training from Chinese data. medRxiv 2020, 1–33. [Google Scholar] [CrossRef] [Green Version]
- Dandekar, R.; Barbastathis, G. Quantifying the effect of quarantine control in Covid-19 infectious spread using machine learning. medRxiv 2020, 1–13. [Google Scholar] [CrossRef] [Green Version]
- Uhlig, S.; Nichani, K.; Uhlig, C.; Simon, K. Modeling projections for COVID-19 pandemic by combining epidemiological, statistical, and neural network approaches. medRxiv 2020, 1–6. [Google Scholar] [CrossRef] [Green Version]
- Yu, Y.; Liu, Y.-R.; Luo, F.-M.; Tu, W.-W.; Zhan, D.-C.; Yu, G.; Zhou, Z.-H. COVID-19 Asymptomatic infection estimation. medRxiv 2020, 1–23. [Google Scholar] [CrossRef] [Green Version]
- Watson, G.L.; Xiong, D.; Zhang, L.; Zoller, J.A.; Shamshoian, J.; Sundin, P.; Bufford, T.; Rimoin, A.W.; Suchard, M.A.; Ramirez, C.M. Pandemic velocity: Forecasting COVID-19 in the US with a machine learning & Bayesian time series compartmental model. PLoS Comput. Biol. 2021, 17, e1008837. [Google Scholar] [CrossRef]
- Kafieh, R.; Arian, R.; Saeedizadeh, N.; Minaee, S.; Amini, Z.; Yadav, S.K.; Vaezi, A.; Rezaei, N.; Javanmard, S.H. COVID-19 in Iran: A deeper look into the future. medRxiv 2020, 1–8. [Google Scholar] [CrossRef]
- Fong, S.J.; Li, G.; Dey, N.; Crespo, R.G.; Herrera-Viedma, E. Finding an accurate early forecasting model from small dataset: A case of 2019-ncov novel coronavirus outbreak. arXiv 2020, arXiv:2003.10776. [Google Scholar] [CrossRef]
- Ibrahim, M.R.; Haworth, J.; Lipani, A.; Aslam, N.; Cheng, T.; Christie, N. Variational-LSTM autoencoder to forecast the spread of coronavirus across the globe. PLoS ONE 2021, 16, e0246120. [Google Scholar] [CrossRef]
- Al-Qaness, M.A.A.; Ewees, A.A.; Fan, H.; Abd El Aziz, M. Optimization method for forecasting confirmed cases of COVID-19 in China. J. Clin. Med. 2020, 9, 674. [Google Scholar] [CrossRef] [Green Version]
- Suzuki, Y.; Suzuki, A.; Nakamura, S.; Ishikawa, T.; Kinoshita, A. Machine learning model estimating number of COVID-19 infection cases over coming 24 days in every province of South Korea (XGBoost and MultiOutputRegressor). medRxiv 2020, 1–11. [Google Scholar] [CrossRef]
- Mehta, M.; Julaiti, J.; Griffin, P.; Kumara, S. Early stage machine learning-based prediction of US county vulnerability to the COVID-19 pandemic: Machine learning approach. JMIR Public Health Surveill. 2020, 6, e19446. [Google Scholar] [CrossRef] [PubMed]
- Golder, S.; Klein, A.Z.; Magge, A.; O’Connor, K.; Cai, H.; Weissenbacher, D.; Gonzalez-Hernandez, G. Extending A chronological and geographical analysis of personal reports of COVID-19 on Twitter to England, UK. medRxiv 2020, 1–8. [Google Scholar] [CrossRef]
- Klein, A.Z.; Magge, A.; O’Connor, K.; Cai, H.; Weissenbacher, D.; Gonzalez-Hernandez, G. A Chronological and geographical analysis of personal reports of COVID-19 on Twitter. medRxiv 2020, 1–9. [Google Scholar] [CrossRef]
- Chamberlain, S.D.; Singh, I.; Ariza, C.; Daitch, A.; Philips, P.; Dalziel, B.D. Real-time detection of COVID-19 epicenters within the United States using a network of smart thermometers. medRxiv 2020, 1–5. [Google Scholar] [CrossRef]
- Pei, J.; Ling, B.; Liao, S.; Liu, B.; Huang, J.X.; Strome, T.; de Faria, R.L.; Zhang, M.G. Improving prediction accuracy of influenza-like illnesses in hospital emergency departments. In Proceedings of the 2013 IEEE International Conference on Bioinformatics and Biomedicine, Shanghai, China, 18–21 December 2013; pp. 602–607. [Google Scholar]
- Randhawa, G.S.; Soltysiak, M.P.M.; El Roz, H.; de Souza, C.P.E.; Hill, K.A.; Kari, L. Machine learning using intrinsic genomic signatures for rapid classification of novel pathogens: COVID-19 case study. PLoS ONE 2020, 15, e0232391. [Google Scholar] [CrossRef] [Green Version]
- Hegde, C.; Jiang, Z.; Suresha, P.B.; Zelko, J.; Seyedi, S.; Smith, M.A.; Wright, D.W.; Kamaleswaran, R.; Reyna, M.A.; Clifford, G.D. AutoTriage—An open source edge computing raspberry pi-based clinical screening system. medRxiv 2020, 1–13. [Google Scholar] [CrossRef]
- Imran, A.; Posokhova, I.; Qureshi, H.N.; Masood, U.; Riaz, M.S.; Ali, K.; John, C.N.; Hussain, M.I.; Nabeel, M. AI4COVID-19: AI enabled preliminary diagnosis for COVID-19 from cough samples via an app. Inform Med. Unlocked 2020, 20, 100378. [Google Scholar] [CrossRef] [PubMed]
- Shoer, S.; Karady, T.; Keshet, A.; Shilo, S.; Rossman, H.; Gavrieli, A.; Meir, T.; Lavon, A.; Kolobkov, D.; Kalka, I.; et al. A prediction model to prioritize individuals for a SARS-CoV-2 test built from national symptom surveys. Medicine 2021, 2, 196–208.e194. [Google Scholar] [CrossRef] [PubMed]
- Lin, Q.; Zhao, S.; Gao, D.; Lou, Y.; Yang, S.; Musa, S.S.; Wang, M.H.; Cai, Y.; Wang, W.; Yang, L.; et al. A conceptual model for the coronavirus disease 2019 (COVID-19) outbreak in Wuhan, China with individual reaction and governmental action. Int. J. Infect. Dis. 2020, 93, 211–216. [Google Scholar] [CrossRef]
- Python Script for SEIR Model. Available online: (GitHub): Script https://github.com/moonmile/seir-model/blob/master/py/seir2.py;licence https://github.com/moonmile/seir-model/blob/master/LICENSE (accessed on 8 August 2021).
- Endo, H.; Ohbe, H.; Kumasawa, J.; Uchino, S.; Hashimoto, S.; Aoki, Y.; Asaga, T.; Hashiba, E.; Hatakeyama, J.; Hayakawa, K.; et al. Conventional risk prediction models fail to accurately predict mortality risk among patients with coronavirus disease 2019 in intensive care units: A difficult time to assess clinical severity and quality of care. J. Intensive Care 2021, 9, 42. [Google Scholar] [CrossRef]
- Chinazzi, M.; Davis, J.T.; Ajelli, M.; Gioannini, C.; Litvinova, M.; Merler, S.; Pastore, Y.P.A.; Mu, K.; Rossi, L.; Sun, K.; et al. The effect of travel restrictions on the spread of the 2019 novel coronavirus (COVID-19) outbreak. Science 2020, 368, 395–400. [Google Scholar] [CrossRef] [Green Version]
- Koo, J.R.; Cook, A.R.; Park, M.; Sun, Y.; Sun, H.; Lim, J.T.; Tam, C.; Dickens, B.L. Interventions to mitigate early spread of SARS-CoV-2 in Singapore: A modelling study. Lancet Infect. Dis. 2020, 20, 678–688. [Google Scholar] [CrossRef] [Green Version]
- Wu, J.T.; Leung, K.; Leung, G.M. Nowcasting and forecasting the potential domestic and international spread of the 2019-nCoV outbreak originating in Wuhan, China: A modelling study. Lancet 2020, 395, 689–697. [Google Scholar] [CrossRef] [Green Version]
- Gudbjartsson, D.F.; Helgason, A.; Jonsson, H.; Magnusson, O.T.; Melsted, P.; Norddahl, G.L.; Saemundsdottir, J.; Sigurdsson, A.; Sulem, P.; Agustsdottir, A.B.; et al. Spread of SARS-CoV-2 in the Icelandic population. N. Engl. J. Med. 2020, 382, 2302–2315. [Google Scholar] [CrossRef]
- Thorpe, W.; Kurver, M.; King, G.; Salome, C. Acoustic analysis of cough. In Proceedings of the The Seventh Australian and New Zealand Intelligent Information Systems Conference, Perth, Australia, 18–21 November 2001; pp. 391–394. [Google Scholar]
- Chatrzarrin, H.; Arcelus, A.; Goubran, R.; Knoefel, F. Feature extraction for the differentiation of dry and wet cough sounds. In Proceedings of the 2011 IEEE International Symposium on Medical Measurements and Applications, Bari, Italy, 30–31 May 2011; pp. 162–166. [Google Scholar]
- Song, I. Diagnosis of pneumonia from sounds collected using low cost cell phones. In Proceedings of the 2015 International Joint Conference on Neural Networks (IJCNN), Killarney, Ireland, 12–17 July 2015; pp. 1–8. [Google Scholar]
- Infante, C.; Chamberlain, D.; Fletcher, R.; Thorat, Y.; Kodgule, R. Use of cough sounds for diagnosis and screening of pulmonary disease. In Proceedings of the 2017 IEEE Global Humanitarian Technology Conference (GHTC), San Jose, CA, USA, 19–22 October 2017; pp. 1–10. [Google Scholar]
- You, M.; Wang, H.; Liu, Z.; Chen, C.; Liu, J.; Xu, X.-H.; Qiu, Z.-M. Novel feature extraction method for cough detection using NMF. IET Signal Process. 2017, 11, 515–520. [Google Scholar] [CrossRef]
- Pramono, R.X.A.; Imtiaz, S.A.; Rodriguez-Villegas, E. Automatic cough detection in acoustic signal using spectral features. In Proceedings of the 2019 41st Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Berlin, Germany, 23–27 July 2019; pp. 7153–7156. [Google Scholar]
- Miranda, I.D.; Diacon, A.H.; Niesler, T.R. A comparative study of features for acoustic cough detection using deep architectures. In Proceedings of the 2019 41st Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Berlin, Germany, 23–27 July 2019; pp. 2601–2605. [Google Scholar]
- Soliński, M.; Łepek, M.; Kołtowski, Ł. Automatic cough detection based on airflow signals for portable spirometry system. Inform. Med. Unlocked 2020, 18, 100313. [Google Scholar] [CrossRef]
- Martin, A.; Nateqi, J.; Gruarin, S.; Munsch, N.; Abdarahmane, I.; Zobel, M.; Knapp, B. An artificial intelligence-based first-line defence against COVID-19: Digitally screening citizens for risks via a chatbot. Sci. Rep. 2020, 10, 19012. [Google Scholar] [CrossRef]
- Hassan, M.R.; Hassan, M.M.; Altaf, M.; Yeasar, M.S.; Hossain, M.I.; Fatema, K.; Shaharin, R.; Ahmed, A.F. B5G-enabled distributed artificial intelligence on edges for COVID-19 pandemic outbreak prediction. IEEE Netw. 2021, 35, 48–55. [Google Scholar] [CrossRef]
- Valtchev, S.Z.; Asgary, A.; Chen, M.; Cronemberger, F.A.; Najafabadi, M.M.; Cojocaru, M.G.; Wu, J. Managing SARS-CoV-2 Testing in schools with an artificial intelligence model and application developed by simulation data. Electronics 2021, 10, 1626. [Google Scholar] [CrossRef]
- Capobianco, R.; Kompella, V.; Ault, J.; Sharon, G.; Jong, S.; Fox, S.; Meyers, L.; Wurman, P.R.; Stone, P. Agent-based markov modeling for improved COVID-19 mitigation policies. J. Artif. Intell. Res. 2021, 71, 953–992. [Google Scholar] [CrossRef]
- Bae, Y.S.; Kim, K.H.; Choi, S.W.; Ko, T.; Lim, J.S.; Piao, M. Satisfaction and usability of an ICT-based system by clinically healthy COVID-19 patients and medical professionals. JMIR Form. Res. 2021, 5, e26227. [Google Scholar] [CrossRef] [PubMed]
- Yu, H.; Liu, P.; Huang, X.; Cao, Y. Teacher online informal learning as a means to innovative teaching during home quarantine in the COVID-19 pandemic. Front. Psychol. 2021, 12, 596582. [Google Scholar] [CrossRef]
- Ajcevic, M.; Furlanis, G.; Naccarato, M.; Caruso, P.; Polverino, P.; Marsich, A.; Accardo, A.; Manganotti, P. e-Health solution for home patient telemonitoring in early post-acute TIA/Minor stroke during COVID-19 pandemic. Int. J. Med. Inform. 2021, 152, 104442. [Google Scholar] [CrossRef]
- Pooch, E.H.P.; Ballester, P.L.; Barros, R.C. Can we trust deep learning models diagnosis? The impact of domain shift in chest radiograph classification. arXiv 2020, arXiv:1909.01940. [Google Scholar]
- Stacke, K.; Eilertsen, G.; Unger, J.; Lundstrom, C. Measuring domain shift for deep learning in histopathology. IEEE J. Biomed. Health Inform. 2020, 25, 325–336. [Google Scholar] [CrossRef] [PubMed]
- Gu, Y.; Ge, Z.; Bonnington, C.P.; Zhou, J. Progressive transfer learning and adversarial domain adaptation for cross-domain skin disease classification. IEEE J. Biomed. Health Inform. 2020, 24, 1379–1393. [Google Scholar] [CrossRef] [PubMed]
- Jiang, J.; Hu, Y.C.; Tyagi, N.; Wang, C.; Lee, N.; Deasy, J.O.; Sean, B.; Veeraraghavan, H. Self-derived organ attention for unpaired CT-MRI deep domain adaptation based MRI segmentation. Phys. Med. Biol. 2020, 65, 205001. [Google Scholar] [CrossRef] [PubMed]
- Choudhary, A.; Tong, L.; Zhu, Y.; Wang, M.D. Advancing medical imaging informatics by deep learning-based domain adaptation. Yearb. Med. Inform. 2020, 29, 129–138. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Asada, K.; Komatsu, M.; Shimoyama, R.; Takasawa, K.; Shinkai, N.; Sakai, A.; Bolatkan, A.; Yamada, M.; Takahashi, S.; Machino, H.; et al. Application of Artificial Intelligence in COVID-19 Diagnosis and Therapeutics. J. Pers. Med. 2021, 11, 886. https://doi.org/10.3390/jpm11090886
Asada K, Komatsu M, Shimoyama R, Takasawa K, Shinkai N, Sakai A, Bolatkan A, Yamada M, Takahashi S, Machino H, et al. Application of Artificial Intelligence in COVID-19 Diagnosis and Therapeutics. Journal of Personalized Medicine. 2021; 11(9):886. https://doi.org/10.3390/jpm11090886
Chicago/Turabian StyleAsada, Ken, Masaaki Komatsu, Ryo Shimoyama, Ken Takasawa, Norio Shinkai, Akira Sakai, Amina Bolatkan, Masayoshi Yamada, Satoshi Takahashi, Hidenori Machino, and et al. 2021. "Application of Artificial Intelligence in COVID-19 Diagnosis and Therapeutics" Journal of Personalized Medicine 11, no. 9: 886. https://doi.org/10.3390/jpm11090886
APA StyleAsada, K., Komatsu, M., Shimoyama, R., Takasawa, K., Shinkai, N., Sakai, A., Bolatkan, A., Yamada, M., Takahashi, S., Machino, H., Kobayashi, K., Kaneko, S., & Hamamoto, R. (2021). Application of Artificial Intelligence in COVID-19 Diagnosis and Therapeutics. Journal of Personalized Medicine, 11(9), 886. https://doi.org/10.3390/jpm11090886







