Simple and Reliable Method for Gastric Subepithelial Tumor Localization Using Endoscopic Tattooing before Totally Laparoscopic Resection
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
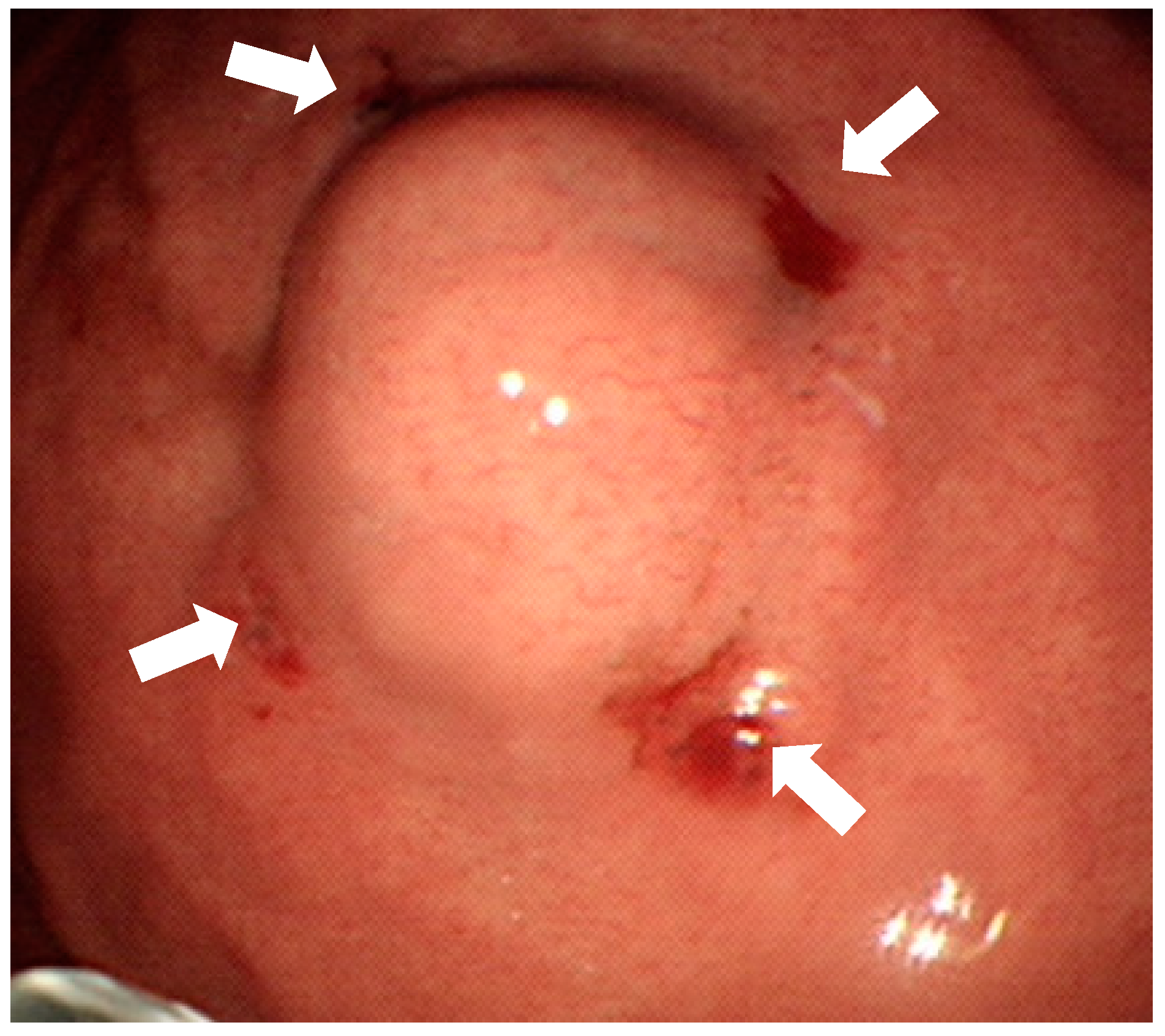
2.2. Localization Method
2.3. Surgery
2.4. Statistical Analysis
3. Result
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kang, K.J.; Kim, K.M.; Min, B.H.; Lee, J.H.; Kim, J.J. Endoscopic submucosal dissection of early gastric cancer. Gut Liver 2011, 5, 418–426. [Google Scholar] [CrossRef]
- Espinel, J.; Pinedo, E.; Ojeda, V.; Del Rio, M.G. Treatment modalities for early gastric cancer. World J. Gastrointest. Endosc. 2015, 7, 1062–1069. [Google Scholar] [CrossRef] [PubMed]
- Sano, T.; Aiko, T. New Japanese classifications and treatment guidelines for gastric cancer: Revision concepts and major revised points. Gastric Cancer 2011, 14, 97–100. [Google Scholar] [CrossRef]
- Kida, M.; Kawaguchi, Y.; Miyata, E.; Hasegawa, R.; Kaneko, T.; Yamauchi, H.; Koizumi, S.; Okuwaki, K.; Miyazawa, S.; Iwai, T.; et al. Endoscopic ultrasonography diagnosis of subepithelial lesions. Dig. Endosc. 2017, 29, 431–443. [Google Scholar] [CrossRef] [PubMed]
- He, Z.; Sun, C.; Zheng, Z.; Yu, Q.; Wang, T.; Chen, X.; Cao, H.; Liu, W.; Wang, B. hepatology. Endoscopic submucosal dissection of large gastrointestinal stromal tumors in the esophagus and stomach. J. Gastroenterol. Hepatol. 2013, 28, 262–267. [Google Scholar] [CrossRef] [PubMed]
- Blay, J.; Bonvalot, S.; Casali, P.; Choi, H.; Debiec-Richter, M.; Dei Tos, A.; Emile, J.; Gronchi, A.; Hogendoorn, P.; Joensuu, H. Consensus meeting for the management of gastrointestinal stromal tumors Report of the GIST Consensus Conference of 20–21 March 2004, under the auspices of ESMO. Ann. Oncol. 2005, 16, 566–578. [Google Scholar] [CrossRef] [PubMed]
- Otani, Y.; Furukawa, T.; Yoshida, M.; Saikawa, Y.; Wada, N.; Ueda, M.; Kubota, T.; Mukai, M.; Kameyama, K.; Sugino, Y.J.S. Operative indications for relatively small (2–5 cm) gastrointestinal stromal tumor of the stomach based on analysis of 60 operated cases. Surgery 2006, 139, 484–492. [Google Scholar] [CrossRef]
- Ryu, K.-J.; Jung, S.-R.; Choi, J.-S.; Jang, Y.-J.; Kim, J.-H.; Park, S.-S.; Park, B.J.; Park, S.-H.; Kim, S.-J.; Mok, Y.-J. Laparoscopic resection of small gastric submucosal tumors. Surg Endosc. 2011, 25, 271–277. [Google Scholar] [CrossRef]
- Kim, H.G.; Ryu, S.Y.; Yun, S.K.; Kim, D.Y. Surgical Outcomes of Laparoscopic Resection for Subepithelial Lesions on the Gastric Fundus Performed in the Supine or Lateral Decubitus Position. J. Laparoendosc. Adv. Surg. Tech. A 2018, 28, 962–966. [Google Scholar] [CrossRef]
- Lee, C.M.; Kim, H.H. Minimally invasive surgery for submucosal (subepithelial) tumors of the stomach. World J. Gastroenterol. 2014, 20, 13035–13043. [Google Scholar] [CrossRef]
- Jeong, S.H.; Seo, K.W.; Min, J.S. Intraoperative Tumor Localization of Early Gastric Cancers. J. Gastric Cancer 2021, 21, 4–15. [Google Scholar] [CrossRef]
- Tokuhara, T.; Nakata, E.; Tenjo, T.; Kawai, I.; Satoi, S.; Inoue, K.; Araki, M.; Ueda, H.; Higashi, C. A novel option for preoperative endoscopic marking with India ink in totally laparoscopic distal gastrectomy for gastric cancer: A useful technique considering the morphological characteristics of the stomach. Mol. Clin. Oncol. 2017, 6, 483–486. [Google Scholar] [CrossRef]
- Hachisu, T.; Miyazaki, S.-I.; Hamaguchi, K.-I. Endoscopic clip-marking of lesions using the newly developed HX-3L clip. Surg. Endosc. 1989, 3, 142–147. [Google Scholar] [CrossRef]
- Kojima, F.; Sato, T.; Tsunoda, S.; Takahata, H.; Hamaji, M.; Komatsu, T.; Okada, M.; Sugiura, T.; Oshiro, O.; Sakai, Y. Development of a novel marking system for laparoscopic gastrectomy using endoclips with radio frequency identification tags: Feasibility study in a canine model. Surg. Endosc. 2014, 28, 2752–2759. [Google Scholar] [CrossRef]
- Matsui, H.; Okamoto, Y.; Nabeshima, K.; Kondoh, Y.; Ogoshi, K.; Makuuchi, H. Endoscopy-assisted gastric resection: A safe and reliable procedure for tumor clearance during laparoscopic high distal or proximal gastrectomy. Surg. Endosc. 2009, 23, 1146–1149. [Google Scholar] [CrossRef]
- Qi, X.D. Gastroscopic mucosal biopsy and carbon ink injection marking for determination of resection line on the gastric wall in stomach cancer. Chin. J. Oncol. 1989, 11, 136–138. [Google Scholar]
- Sekimoto, M.; Tamura, S.; Hasuike, Y.; Yano, M.; Murata, A.; Inoue, M.; Shiozaki, H.; Monden, M. A new technique for laparoscopic resection of a submucosal tumor on the posterior wall of the gastric fundus. Surg. Endosc. 1999, 13, 71–74. [Google Scholar] [CrossRef] [PubMed]
- Standards of Practice, C.; Faulx, A.L.; Kothari, S.; Acosta, R.D.; Agrawal, D.; Bruining, D.H.; Chandrasekhara, V.; Eloubeidi, M.A.; Fanelli, R.D.; Gurudu, S.R.; et al. The role of endoscopy in subepithelial lesions of the GI tract. Gastrointest. Endosc. 2017, 85, 1117–1132. [Google Scholar] [CrossRef]
- de Moura, D.T.H.; McCarty, T.R.; Jirapinyo, P.; Ribeiro, I.B.; Flumignan, V.K.; Najdawai, F.; Ryou, M.; Lee, L.S.; Thompson, C.C. EUS-guided fine-needle biopsy sampling versus FNA in the diagnosis of subepithelial lesions: A large multicenter study. Gastrointest. Endosc. 2020, 92, 108–119.e3. [Google Scholar] [CrossRef]
- Crinò, S.F.; Di Mitri, R.; Nguyen, N.Q.; Tarantino, I.; de Nucci, G.; Deprez, P.H.; Carrara, S.; Kitano, M.; Shami, V.M.; Fernández-Esparrach, G.J.G. Endoscopic Ultrasound-guided Fine-needle Biopsy With or Without Rapid On-site Evaluation for Diagnosis of Solid Pancreatic Lesions: A Randomized Controlled Non-Inferiority Trial. Gastroenterology 2021. [Google Scholar] [CrossRef]
- Crinò, S.F.; Ammendola, S.; Meneghetti, A.; Bernardoni, L.; Bellocchi, M.C.C.; Gabbrielli, A.; Landoni, L.; Paiella, S.; Pin, F.; Parisi, A.J.P. Comparison between EUS-guided fine-needle aspiration cytology and EUS-guided fine-needle biopsy histology for the evaluation of pancreatic neuroendocrine tumors. Pancreatology 2021, 21, 443–450. [Google Scholar] [CrossRef]
- Larghi, A.; Fuccio, L.; Chiarello, G.; Attili, F.; Vanella, G.; Paliani, G.B.; Napoleone, M.; Rindi, G.; Larocca, L.M.; Costamagna, G.J.E. Fine-needle tissue acquisition from subepithelial lesions using a forward-viewing linear echoendoscope. Endoscopy 2014, 46, 39–45. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.H.; Cho, C.J.; Park, Y.S.; Ahn, J.Y.; Kim, D.H.; Na, H.K.; Choi, K.D.; Song, H.J.; Lee, G.H.; Jung, H.-Y. EUS-guided 22-gauge fine needle biopsy for the diagnosis of gastric subepithelial tumors larger than 2 cm. Scand. J. Gastroenterol. 2016, 51, 486–493. [Google Scholar] [CrossRef]
- Hedenström, P.; Marschall, H.-U.; Nilsson, B.; Demir, A.; Lindkvist, B.; Nilsson, O.; Sadik, R. High clinical impact and diagnostic accuracy of EUS-guided biopsy sampling of subepithelial lesions: A prospective, comparative study. Surg. Endosc. 2018, 32, 1304–1313. [Google Scholar] [CrossRef] [PubMed]
- Fujita, A.; Ryozawa, S.; Mizuide, M.; Araki, R.; Nagata, K.; Tanisaka, Y.; Harada, M.; Ogawa, T.; Tashima, T.; Nonaka, K.J. Does endoscopic ultrasound-guided fine needle biopsy using a Franseen needle really offer high diagnostic accuracy? A propensity-matched analysis. Endosc. Int. Open 2019, 7, E1327–E1332. [Google Scholar] [CrossRef] [PubMed]
- Jeong, S.-H.; Bae, K.; Ha, C.-Y.; Lee, Y.-J.; Lee, O.-J.; Jung, W.-T.; Choi, S.-K.; Hong, S.-C.; Jung, E.-J.; Ju, Y.-T.J. Effectiveness of endoscopic clipping and computed tomography gastroscopy for the preoperative localization of gastric cancer. J. Korean Surg. Soc. 2013, 84, 80–87. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Chung, J.W.; Seo, K.W.; Jung, K.; Park, M.I.; Kim, S.E.; Park, S.J.; Lee, S.H.; Shin, Y.M. A promising method for tumor localization during total laparoscopic distal gastrectomy: Preoperative endoscopic clipping based on negative biopsy and selective intraoperative radiography findings. J. Gastric Cancer 2017, 17, 220–227. [Google Scholar] [CrossRef]
- Ohdaira, T.; Nagai, H.J. Intraoperative localization of early-stage upper gastrointestinal tumors using a magnetic marking clip–detecting system. Surg. Endosc. 2007, 21, 810–815. [Google Scholar] [CrossRef] [PubMed]
- Choi, Y.; Kim, K.G.; Kim, J.K.; Nam, K.W.; Kim, H.H.; Sohn, D.K. A novel endoscopic fluorescent clip for the localization of gastrointestinal tumors. Surg. Endosc. 2011, 25, 2372–2377. [Google Scholar] [CrossRef]
- Luigiano, C.; Ferrara, F.; Morace, C.; Mangiavillano, B.; Fabbri, C.; Cennamo, V.; Bassi, M.; Virgilio, C.; Consolo, P.J. Endoscopic tattooing of gastrointestinal and pancreatic lesions. Adv. Ther. 2012, 29, 864–873. [Google Scholar] [CrossRef]
- Committee, A.T.; Kethu, S.R.; Banerjee, S.; Desilets, D.; Diehl, D.L.; Farraye, F.A.; Kaul, V.; Kwon, R.S.; Mamula, P.; Pedrosa, M.C.; et al. Endoscopic tattooing. Gastrointest. Endosc. 2010, 72, 681–685. [Google Scholar] [CrossRef]
- Trakarnsanga, A.; Akaraviputh, T. Endoscopic tattooing of colorectal lesions: Is it a risk-free procedure? World J. Gastrointest. Endosc. 2011, 3, 256. [Google Scholar] [CrossRef] [PubMed]
- Miyoshi, N.; Ohue, M.; Noura, S.; Yano, M.; Sasaki, Y.; Kishi, K.; Yamada, T.; Miyashiro, I.; Ohigashi, H.; Iishi, H. Surgical usefulness of indocyanine green as an alternative to India ink for endoscopic marking. Surg. Endosc. 2009, 23, 347–351. [Google Scholar] [CrossRef] [PubMed]
- Park, J.W.; Sohn, D.K.; Hong, C.W.; Han, K.S.; Choi, D.H.; Chang, H.J.; Lim, S.B.; Choi, H.S.; Jeong, S.Y. The usefulness of preoperative colonoscopic tattooing using a saline test injection method with prepackaged sterile India ink for localization in laparoscopic colorectal surgery. Surg. Endosc. 2008, 22, 501–505. [Google Scholar] [CrossRef]
- McArthur, C.; Roayaie, S.; Waye, J. Safety of preoperation endoscopic tattoo with india ink for identification of colonic lesions. Surg. Endosc. 1999, 13, 397–400. [Google Scholar] [CrossRef]
- Hyman, N.; Waye, J.D. Endoscopic four quadrant tattoo for the identification of colonic lesions at surgery. Gastrointest. Endosc. 1991, 37, 56–58. [Google Scholar] [CrossRef]
- Siow, S.L.; Mahendran, H.A.; Wong, C.M. Laparoscopic transgastric resection for intraluminal gastric gastrointestinal stromal tumors located at the posterior wall and near the gastroesophageal junction. Asian J. Surg. 2017, 40, 407–414. [Google Scholar] [CrossRef]
- Askin, M.P.; Waye, J.D.; Fiedler, L.; Harpaz, N. Tattoo of colonic neoplasms in 113 patients with a new sterile carbon compound. Gastrointest. Endosc. 2002, 56, 339–342. [Google Scholar] [CrossRef]

| Pt No | M/F | Age | Initial Symptom | Tumor Location | Time to Op (Hour) | EUS Layer | Endoscopy Size (cm) | Pathological Diagnosis | Stomach Diameter (cm) | Tumor Diameter (cm) | Diameter Ratio | Surgery Time (min) | Complication | Hospital Days | Time to Intake (Day) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | F | 70 | No symptom | Fundus | 20.5 | 4 | 1.2 | Leiomyoma | 4.0 | 2.2 | 0.550 | 90 | No | 5 | 2 |
| 2 | F | 51 | Fullness | Fundus | 3.5 | not done | 3 | GIST | 6.0 | 3.5 | 0.583 | 111 | Fever | 5 | 2 |
| 3 | F | 43 | No symptom | Fundus | 3.5 | 4 | 1.2 | GIST | 2.9 | 1.6 | 0.552 | 120 | No | 3 | 1 |
| 4 | F | 44 | Epigastric pain | Posterior wall | 5 | 4 | 1.5 | Leiomyoma | 6.6 | 1.8 | 0.273 | 105 | No | 8 | 4 |
| 5 | M | 70 | No symptom | Posterior wall | 8 | not done | 2 | GIST | 6.5 | 5.7 | 0.877 | 120 | No | 11 | 3 |
| 6 | F | 57 | Epigastric pain | Anterior wall | 3.5 | 4 | 2 | GIST | 5.1 | 2.5 | 0.490 | 90 | No | 6 | 4 |
| 7 | F | 63 | No symptom | Lesser curvature | 7 | 4 | 2 | GIST | 4.5 | 3.7 | 0.822 | 110 | No | 6 | 5 |
| 8 | F | 44 | No symptom | Posterior wall | 4.5 | 4 | 1.2 | GIST | 3.1 | 1.4 | 0.452 | 120 | No | 4 | 2 |
| 9 | F | 66 | No symptom | Greater curvature | 2.5 | 4 | 2 | Glomus tumor | 3.0 | 2.0 | 0.667 | 120 | No | 8 | 3 |
| 10 | M | 70 | UGI bleeding | Posterior wall | 4 | not done | 3 | GIST | 5.3 | 2.5 | 0.472 | 150 | Fever | 10 | 4 |
| 11 | F | 64 | UGI bleeding | Fundus | 23 | 4 | 3 | GIST | 7.8 | 3.2 | 0.410 | 140 | No | 6 | 2 |
| 12 | F | 50 | No symptom | Posterior wall | 3 | 4 | 1 | Leiomyoma | 6.4 | 0.9 | 0.141 | 70 | No | 3 | 2 |
| 13 | M | 50 | No symptom | Posterior wall | 3 | 4 | 2 | Ectopic pancreas | 2.8 | 1.4 | 0.500 | 100 | No | 5 | 4 |
| 14 | F | 70 | No symptom | Greater curvature | 3 | 4 | 1.5 | GIST | 2.8 | 1.6 | 0.571 | 110 | No | 6 | 3 |
| 15 | M | 52 | Epigastric pain | Anterior wall | 6.5 | 4 | 1 | Leiomyoma | 4.1 | 0.9 | 0.220 | 60 | No | 9 | 5 |
| 16 | M | 50 | No symptom | Fundus | 3 | 4 | 1.4 | GIST | 5.3 | 1.2 | 0.226 | 130 | No | 6 | 3 |
| 17 | F | 62 | No symptom | Cardia | 2.5 | 4 | 3 | Leiomyoma | 4.5 | 2.4 | 0.533 | 150 | No | 7 | 3 |
| 18 | F | 57 | No symptom | Lesser curvature | 22 | not done | 2 | GIST | 3.6 | 2.1 | 0.583 | 105 | No | 5 | 3 |
| 19 | F | 73 | No symptom | Fundus | 2 | 4 | 2 | GIST | 3.6 | 2.5 | 0.694 | 100 | No | 5 | 3 |
| Total | AW + GC + Fundus (n = 10) | PW + LC + Cardia (n = 9) | p Value | |
|---|---|---|---|---|
| Age(year) | 58.2 ± 10.1 | 59.6 ± 10.3 | 56.7 ± 10.2 | 0.456 |
| Gender | 0.434 | |||
| Male | 5 (26.3%) | 2 (20.0%) | 3 (33.3%) | |
| Female | 14 (73.7%) | 8 (80.0%) | 6 (66.7%) | |
| Tumor size(cm) | ||||
| Endoscopy | 1.9 ± 0.7 | 1.8 ± 0.7 | 2.0 ± 0.7 | 0.634 |
| EUS | 1.8 ± 0.5 | 1.8 ± 0.6 | 1.6 ± 0.4 | 0.976 |
| CT | 2.2 ± 1.3 | 2.2 ± 1.2 | 2.2 ± 1.5 | 0.749 |
| Specimen | 2.3 ± 1.2 | 2.1 ± 0.8 | 2.4 ± 1.5 | 0.921 |
| Pathology diagnosis | 0.478 | |||
| leiomyoma | 5 (26.3%) | 2 (20.0%) | 3 (33.3%) | |
| GIST | 12 (63.2%) | 7 (70.0%) | 5 (55.6%) | |
| Glomus tumor | 1 (5.3%) | 1 (10.0%) | 0 (0.0%) | |
| Ectopic pancreas | 1 (5.3%) | 0 (0.0%) | 1 (11.1%) | |
| Mitosis of GIST (/50HPF) | 1.5 ± 1.8 | 1.8 ± 2.1 | 1.2 ± 1.4 | 0.509 |
| Time to surgery (hour) | 6.8 ± 6.8 | 7.1 ± 7.8 | 6.6 ± 6.1 | 0.508 |
| Procedure of surgery | 0.950 | |||
| Partial gastrectomy | 1 | 1 (10.0%) | 0 (0%) | |
| Wedge resection | 18 | 9 (90.0%) | 9 (90%) |
| AW + GC + Fundus (n = 10) | PW + LC + Cardia (n = 9) | p Value | |
|---|---|---|---|
| Margin free (%) | 10 (100%) | 9 (100%) | 1.000 |
| Distance from margin (cm) | 0.5 ± 0.3 | 0.5 ± 0.4 | 0.795 |
| Specimen size | |||
| Maximal diameter of stomach (cm) | 4.5 ± 1.6 | 4.8 ± 1.5 | 0.509 |
| Maximal diameter of tumor (cm) | 2.1 ± 0.8 | 2.4 ± 1.5 | 0.921 |
| Ratio of diameter (tumor/stomach) | 0.5 ± 0.1 | 0.5 ± 0.2 | 0.922 |
| Duration of operation (min) | 107.0 ± 23.0 | 114.0 ± 25.0 | 0.644 |
| Blood loss (mL) | 5.2 ± 1.9 | 10.6 ± 14.9 | 0.296 |
| Complication | 0.950 | ||
| No | 8 (80.0%) | 8 (88.8%) | |
| Yes | |||
| Leakage | 0 (0.0%) | 0 (0.0%) | |
| Fever | 1 (10.0%) | 1 (11.1%) | |
| Hospital days (day) | 5.9 ± 1.7 | 6.6 ± 2.7 | 0.763 |
| Time to intake (day) | 2.8 ± 1.1 | 3.3 ± 1 | 0.324 |
| Follow up (month) | 10.1 ± 6.8 | 11.2 ± 6.2 | 0.589 |
| Time to last image (month) | 12.6 ± 8 | 9.8 ± 6.2 | 0.648 |
| Recurrence | 1.000 | ||
| Yes | 0 (0.0%) | 0 (0.0%) | |
| No | 10 (100.0%) | 9 (100.0%) |
| Tattoo on Day of Surgery (n = 16) | Tattoo on Day Before Surgery (n = 3) | p Value | |
|---|---|---|---|
| Distance from margin (cm) | 0.4 ± 0.3 | 0.8 ± 0.1 | 0.078 |
| Specimen size | |||
| Maximal diameter of stomach (cm) | 4.5 ± 1.4 | 5.1 ± 2.3 | 0.542 |
| Maximal diameter of tumor (cm) | 2.2 ± 1.2 | 2.5 ± 0.6 | 0.716 |
| Ratio of diameter (tumor/stomach) | 0.5 ± 0.2 | 0.5 ± 0.1 | 0.938 |
| Duration of operation (min) | 110.3 ± 24.1 | 111.6 ± 25.6 | 0.943 |
| Blood loss (mL) | 8.4 ± 11.2 | 4.0 ± 1.7 | 0.513 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, S.-F.; Cheng, H.-T.; Hsu, J.-T.; Wu, C.-H.; Chen, C.-W.; Lin, C.-J.; Sung, K.-F. Simple and Reliable Method for Gastric Subepithelial Tumor Localization Using Endoscopic Tattooing before Totally Laparoscopic Resection. J. Pers. Med. 2021, 11, 855. https://doi.org/10.3390/jpm11090855
Wang S-F, Cheng H-T, Hsu J-T, Wu C-H, Chen C-W, Lin C-J, Sung K-F. Simple and Reliable Method for Gastric Subepithelial Tumor Localization Using Endoscopic Tattooing before Totally Laparoscopic Resection. Journal of Personalized Medicine. 2021; 11(9):855. https://doi.org/10.3390/jpm11090855
Chicago/Turabian StyleWang, Sheng-Fu, Hao-Tsai Cheng, Jun-Te Hsu, Chi-Huan Wu, Chun-Wei Chen, Chun-Jung Lin, and Kai-Feng Sung. 2021. "Simple and Reliable Method for Gastric Subepithelial Tumor Localization Using Endoscopic Tattooing before Totally Laparoscopic Resection" Journal of Personalized Medicine 11, no. 9: 855. https://doi.org/10.3390/jpm11090855
APA StyleWang, S.-F., Cheng, H.-T., Hsu, J.-T., Wu, C.-H., Chen, C.-W., Lin, C.-J., & Sung, K.-F. (2021). Simple and Reliable Method for Gastric Subepithelial Tumor Localization Using Endoscopic Tattooing before Totally Laparoscopic Resection. Journal of Personalized Medicine, 11(9), 855. https://doi.org/10.3390/jpm11090855






