The Neutrophil-to-Lymphocyte and Platelet-to-Lymphocyte Ratios Predict Reperfusion and Prognosis after Endovascular Treatment of Acute Ischemic Stroke
Abstract
:1. Introduction
2. Methods
2.1. Study Population
2.2. Data Collection and Definition of Parameters
2.3. Statistical Analyses
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| NLR | neutrophil-to-lymphocyte ratio |
| PLR | platelet-to-lymphocyte ratio |
| EVT | endovascular treatment |
| IVT | intravenous thrombolysis |
References
- Powers, W.J.; Derdeyn, C.P.; Biller, J.; Coffey, C.S.; Hoh, B.L.; Jauch, E.C.; Johnston, K.C.; Johnston, S.C.; Khalessi, A.A.; Kidwell, C.S.; et al. 2015 American Heart Association/American Stroke Association Focused Update of the 2013 Guidelines for the Early Management of Patients With Acute Ischemic Stroke Regarding Endovascular Treatment: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke 2015, 46, 3020–3035. [Google Scholar] [PubMed] [Green Version]
- Powers, W.J.; Rabinstein, A.A.; Ackerson, T.; Adeoye, O.M.; Bambakidis, N.C.; Becker, K.; Biller, J.; Brown, M.; Demaerschalk, B.M.; Hoh, B.; et al. 2018 Guidelines for the Early Management of Patients With Acute Ischemic Stroke: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke 2018, 49, e46–e110. [Google Scholar] [CrossRef] [PubMed]
- Campbell, B.C.V.; Donnan, G.A.; Lees, K.R.; Hacke, W.; Khatri, P.; Hill, M.D.; Goyal, M.; Mitchell, P.J.; Saver, J.L.; Diener, H.C.; et al. Endovascular stent thrombectomy: The new standard of care for large vessel ischaemic stroke. Lancet Neurol. 2015, 14, 846–854. [Google Scholar] [CrossRef]
- Lemmens, R.; Hamilton, S.A.; Liebeskind, D.S.; Tomsick, T.A.; Demchuk, A.M.; Nogueira, R.G.; Marks, M.P.; Jahan, R.; Gralla, J.; Yoo, A.J.; et al. Effect of endovascular reperfusion in relation to site of arterial occlusion. Neurology 2016, 86, 762–770. [Google Scholar] [CrossRef] [Green Version]
- Libby, P.; Ridker, P.M.; Maseri, A. Inflammation and atherosclerosis. Circulation 2002, 105, 1135–1143. [Google Scholar] [CrossRef]
- Lind, L. Circulating markers of inflammation and atherosclerosis. Atherosclerosis 2003, 169, 203–214. [Google Scholar] [CrossRef]
- Parikh, N.S.; Merkler, A.E.; Iadecola, C. Inflammation, Autoimmunity, Infection, and Stroke: Epidemiology and Lessons From Therapeutic Intervention. Stroke 2020, 51, 711–718. [Google Scholar] [CrossRef]
- Schuhmann, M.K.; Stoll, G.; Bieber, M.; Vogtle, T.; Hofmann, S.; Klaus, V.; Kraft, P.; Seyhan, M.; Kollikowski, A.M.; Papp, L.; et al. CD84 Links T Cell and Platelet Activity in Cerebral Thrombo-Inflammation in Acute Stroke. Circ. Res. 2020, 127, 1023–1035. [Google Scholar] [CrossRef]
- Stoll, G.; Nieswandt, B. Thrombo-inflammation in acute ischaemic stroke—Implications for treatment. Nat. Rev. Neurol. 2019, 15, 473–481. [Google Scholar] [CrossRef]
- Tokgoz, S.; Keskin, S.; Kayrak, M.; Seyithanoglu, A.; Ogmegul, A. Is neutrophil/lymphocyte ratio predict to short-term mortality in acute cerebral infarct independently from infarct volume? J. Stroke Cerebrovasc. Dis. 2014, 23, 2163–2168. [Google Scholar] [CrossRef] [PubMed]
- Guo, Z.; Yu, S.; Xiao, L.; Chen, X.; Ye, R.; Zheng, P.; Dai, Q.; Sun, W.; Zhou, C.; Wang, S.; et al. Dynamic change of neutrophil to lymphocyte ratio and hemorrhagic transformation after thrombolysis in stroke. J. Neuroinflamm. 2016, 13, 199. [Google Scholar] [CrossRef] [Green Version]
- Duan, Z.; Wang, H.; Wang, Z.; Hao, Y.; Zi, W.; Yang, D.; Zhou, Z.; Liu, W.; Lin, M.; Shi, Z.; et al. Neutrophil-Lymphocyte Ratio Predicts Functional and Safety Outcomes after Endovascular Treatment for Acute Ischemic Stroke. Cerebrovasc. Dis. 2018, 45, 221–227. [Google Scholar] [CrossRef]
- Xue, J.; Huang, W.; Chen, X.; Li, Q.; Cai, Z.; Yu, T.; Shao, B. Neutrophil-to-Lymphocyte Ratio Is a Prognostic Marker in Acute Ischemic Stroke. J. Stroke Cerebrovasc. Dis. 2017, 26, 650–657. [Google Scholar] [CrossRef]
- Zhu, B.; Pan, Y.; Jing, J.; Meng, X.; Zhao, X.; Liu, L.; Wang, D.; Johnston, S.C.; Li, H.; Wang, Y.; et al. Neutrophil counts, neutrophil ratio, and new stroke in minor ischemic stroke or TIA. Neurology 2018, 90, e1870–e1878. [Google Scholar] [CrossRef] [PubMed]
- Lux, D.; Alakbarzade, V.; Bridge, L.; Clark, C.N.; Clarke, B.; Zhang, L.; Khan, U.; Pereira, A.C. The association of neutrophil-lymphocyte ratio and lymphocyte-monocyte ratio with 3-month clinical outcome after mechanical thrombectomy following stroke. J. Neuroinflamm. 2020, 17, 60. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gong, P.; Liu, Y.; Gong, Y.; Chen, G.; Zhang, X.; Wang, S.; Zhou, F.; Duan, R.; Chen, W.; Huang, T.; et al. The association of neutrophil to lymphocyte ratio, platelet to lymphocyte ratio, and lymphocyte to monocyte ratio with post-thrombolysis early neurological outcomes in patients with acute ischemic stroke. J. Neuroinflamm. 2021, 18, 51. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.L.; Wu, Z.Q.; Qu, J.F.; Qiu, D.H.; Luo, G.P.; Yin, H.P.; Fang, X.W.; Wang, F.; Chen, Y.K. High neutrophil-to-lymphocyte ratio is a predictor of poor short-term outcome in patients with mild acute ischemic stroke receiving intravenous thrombolysis. Brain Behav. 2020, 10, e01857. [Google Scholar] [CrossRef] [PubMed]
- Xu, J.H.; He, X.W.; Li, Q.; Liu, J.R.; Zhuang, M.T.; Huang, F.F.; Bao, G.S. Higher Platelet-to-Lymphocyte Ratio Is Associated With Worse Outcomes After Intravenous Thrombolysis in Acute Ischaemic Stroke. Front. Neurol. 2019, 10, 1192. [Google Scholar] [CrossRef] [Green Version]
- Pektezel, M.Y.; Yilmaz, E.; Arsava, E.M.; Topcuoglu, M.A. Neutrophil-to-Lymphocyte Ratio and Response to Intravenous Thrombolysis in Patients with Acute Ischemic Stroke. J. Stroke Cerebrovasc. Dis. 2019, 28, 1853–1859. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Cheng, Q.; Peng, M.; Lv, D.; Zi, W.; Xu, G.; Liu, X. The relationship between the platelet to leukocyte ratio and mechanical thrombectomy outcomes in acute ischemic stroke patients. Neurol. Res. 2020, 42, 890–896. [Google Scholar] [CrossRef] [PubMed]
- Switonska, M.; Piekus-Slomka, N.; Slomka, A.; Sokal, P.; Zekanowska, E.; Lattanzi, S. Neutrophil-to-Lymphocyte Ratio and Symptomatic Hemorrhagic Transformation in Ischemic Stroke Patients Undergoing Revascularization. Brain Sci. 2020, 10, 771. [Google Scholar] [CrossRef]
- Altintas, O.; Altintas, M.O.; Tasal, A.; Kucukdagli, O.T.; Asil, T. The relationship of platelet-to-lymphocyte ratio with clinical outcome and final infarct core in acute ischemic stroke patients who have undergone endovascular therapy. Neurol. Res. 2016, 38, 759–765. [Google Scholar] [CrossRef]
- Ko, Y.; Lee, S.; Chung, J.W.; Han, M.K.; Park, J.M.; Kang, K.; Park, T.H.; Park, S.S.; Cho, Y.J.; Hong, K.S.; et al. MRI-based Algorithm for Acute Ischemic Stroke Subtype Classification. J. Stroke 2014, 16, 161–172. [Google Scholar] [CrossRef] [Green Version]
- Menon, B.K.; d’Esterre, C.D.; Qazi, E.M.; Almekhlafi, M.; Hahn, L.; Demchuk, A.M.; Goyal, M. Multiphase CT Angiography: A New Tool for the Imaging Triage of Patients with Acute Ischemic Stroke. Radiology 2015, 275, 510–520. [Google Scholar] [CrossRef] [Green Version]
- Dargazanli, C.; Fahed, R.; Blanc, R.; Gory, B.; Labreuche, J.; Duhamel, A.; Marnat, G.; Saleme, S.; Costalat, V.; Bracard, S.; et al. Modified Thrombolysis in Cerebral Infarction 2C/Thrombolysis in Cerebral Infarction 3 Reperfusion Should Be the Aim of Mechanical Thrombectomy: Insights From the ASTER Trial(Contact Aspiration Versus Stent Retriever for Successful Revascularization). Stroke 2018, 49, 1189–1196. [Google Scholar] [CrossRef]
- De Meyer, S.F.; Denorme, F.; Langhauser, F.; Geuss, E.; Fluri, F.; Kleinschnitz, C. Thromboinflammation in Stroke Brain Damage. Stroke 2016, 47, 1165–1172. [Google Scholar] [CrossRef] [Green Version]
- Iadecola, C.; Anrather, J. The immunology of stroke: From mechanisms to translation. Nat. Med. 2011, 17, 796–808. [Google Scholar] [CrossRef] [PubMed]
- Lievens, D.; von Hundelshausen, P. Platelets in atherosclerosis. Thromb. Haemost. 2011, 106, 827–838. [Google Scholar] [PubMed]
- Yan, J.; Greer, J.M.; Etherington, K.; Cadigan, G.P.; Cavanagh, H.; Henderson, R.D.; O’Sullivan, J.D.; Pandian, J.D.; Read, S.J.; McCombe, P.A. Immune activation in the peripheral blood of patients with acute ischemic stroke. J. Neuroimmunol. 2009, 206, 112–117. [Google Scholar] [CrossRef] [PubMed]
- Yilmaz, G.; Granger, D.N. Leukocyte recruitment and ischemic brain injury. Neuromolecular. Med. 2010, 12, 193–204. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Anrather, J.; Iadecola, C. Inflammation and Stroke: An Overview. Neurotherapeutics 2016, 13, 661–670. [Google Scholar] [CrossRef] [PubMed]
- Rosell, A.; Cuadrado, E.; Ortega-Aznar, A.; Hernandez-Guillamon, M.; Lo, E.H.; Montaner, J. MMP-9-positive neutrophil infiltration is associated to blood-brain barrier breakdown and basal lamina type IV collagen degradation during hemorrhagic transformation after human ischemic stroke. Stroke 2008, 39, 1121–1126. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Garcia-Bonilla, L.; Moore, J.M.; Racchumi, G.; Zhou, P.; Butler, J.M.; Iadecola, C.; Anrather, J. Inducible nitric oxide synthase in neutrophils and endothelium contributes to ischemic brain injury in mice. J. Immunol. 2014, 193, 2531–2537. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Goyal, N.; Tsivgoulis, G.; Chang, J.J.; Malhotra, K.; Pandhi, A.; Ishfaq, M.F.; Alsbrook, D.; Arthur, A.S.; Elijovich, L.; Alexandrov, A.V. Admission Neutrophil-to-Lymphocyte Ratio as a Prognostic Biomarker of Outcomes in Large Vessel Occlusion Strokes. Stroke 2018, 49, 1985–1987. [Google Scholar] [CrossRef] [PubMed]
- Al-Dasuqi, K.; Payabvash, S.; Torres-Flores, G.A.; Strander, S.M.; Nguyen, C.K.; Peshwe, K.U.; Kodali, S.; Silverman, A.; Malhotra, A.; Johnson, M.H.; et al. Effects of Collateral Status on Infarct Distribution Following Endovascular Therapy in Large Vessel Occlusion Stroke. Stroke 2020, 51, e193–e202. [Google Scholar] [CrossRef]
- Akkaya, E.; Gul, M.; Ugur, M. Platelet to lymphocyte ratio: A simple and valuable prognostic marker for acute coronary syndrome. Int. J. Cardiol. 2014, 177, 597–598. [Google Scholar] [CrossRef]
- Corriere, T.; Di Marca, S.; Cataudella, E.; Pulvirenti, A.; Alaimo, S.; Stancanelli, B.; Malatino, L. Neutrophil-to-Lymphocyte Ratio is a strong predictor of atherosclerotic carotid plaques in older adults. Nutr. Metab. Cardiovasc. Dis. 2018, 28, 23–27. [Google Scholar] [CrossRef]
- Aukrust, P.; Halvorsen, B.; Ueland, T.; Michelsen, A.E.; Skjelland, M.; Gullestad, L.; Yndestad, A.; Otterdal, K. Activated platelets and atherosclerosis. Expert Rev. Cardiovasc. Ther. 2010, 8, 1297–1307. [Google Scholar] [CrossRef]
- Balta, S.; Celik, T.; Mikhailidis, D.P.; Ozturk, C.; Demirkol, S.; Aparci, M.; Iyisoy, A. The Relation Between Atherosclerosis and the Neutrophil-Lymphocyte Ratio. Clin. Appl. Thromb. Hemost. 2016, 22, 405–411. [Google Scholar] [CrossRef]
| Successful Reperfusion (n = 224) | Unsuccessful Reperfusion (n = 58) | p-Value | |
|---|---|---|---|
| Age (SD) | 68.7 (13.7) | 72.8 (11.7) | 0.17 |
| Male, % (SD) | 135 (60.3) | 27 (46.6) | 0.07 * |
| BMI (SD) | 25.5 (23.2) | 23.4 (3.8) | 0.59 † |
| NIHSS (IQR) | 14 (9–18) | 15 (11-18) | 0.13 ‡ |
| Interval from arrival to puncture, min (IQR) | 96.5 (75.0–134.0) | 101.5 (73.0–156.0) | 0.18 ‡ |
| Stroke mechanism, % (SD) | 0.12 * | ||
| LAA | 55 (24.6) | 21 (36.2) | |
| CE | 130 (58.0) | 25 (43.1) | |
| Others | 39 (17.4) | 12 (20.7) | |
| Previous stroke, % (SD) | 49 (21.9) | 10 (17.2) | 0.44 * |
| HTN, % (SD) | 121 (54.0) | 38 (65.5) | 0.12 * |
| DM, % (SD) | 62 (27.7) | 15 (25.9) | 0.78 * |
| HL, % (SD) | 33 (14.7) | 7 (12.1) | 0.60 * |
| Current smoking, % (SD) | 31 (13.8) | 7 (12.1) | 0.73 * |
| Atrial fibrillation, % (SD) | 120 (53.6) | 25 (43.1) | 0.16 * |
| Previous use of antithrombotics, % (SD) | 87 (38.8) | 18 (31.0) | 0.27 * |
| Previous use of statin, % (SD) | 49 (21.9) | 5 (8.6) | 0.02 * |
| WBC, x1000/µL (SD) | 8.70 (3.26) | 9.46 (4.42) | 0.03 † |
| Creatinine, mg/dL (SD) | 0.98 (0.60) | 0.87 (0.30) | 0.36 † |
| Hemoglobin, g/dL (SD) | 13.7 (2.1) | 13.4 (2.2) | 0.76 † |
| Platelet, x1000/µL (SD) | 221.9 (70.9) | 250.9 (125.9) | 0.02 † |
| LDLc, mg/dL (SD) | 46.1 (30.8) | 48.2 (34.8) | 0.03 † |
| HbA1c, % (SD) | 6.2 (1.4) | 5.9 (0.7) | <0.001 † |
| Prothrombin time, INR (SD) | 1.08 (0.25) | 1.05 (0.11) | 0.22 † |
| CRP, mg/dL (SD) | 12.2 (25.0) | 14.0 (26.2) | 0.28 † |
| Initial random glucose, mg/dL (SD) | 141.2 (51.6) | 148.9 (63.7) | 0.95 † |
| SBP, mmHg (SD) | 149.2 (26.4) | 149.3 (25.9) | 0.70 † |
| Successful Reperfusion (n = 224) | Unsuccessful Reperfusion (n = 58) | p-Value | |
|---|---|---|---|
| Reperfusion therapy, % (SD) | 0.67 * | ||
| EVT only | 105 (46.9) | 29 (50.0) | |
| Combined IVT and EVT | 119 (53.1) | 29 (50.0) | |
| LVO location, % (SD) | 0.76 * | ||
| ICA | 17 (7.6) | 3 (5.2) | |
| M1/M2 MCA | 183 (81.7) | 46 (79.3) | |
| BA/VA | 24 (10.7) | 9 (15.5) | |
| Collateral status, % (SD) | 0.06 * | ||
| Poor | 100 (44.6) | 22 (37.9) | |
| Intermediate | 35 (15.6) | 17 (29.3) | |
| Good | 89 (39.7) | 19 (32.8) | |
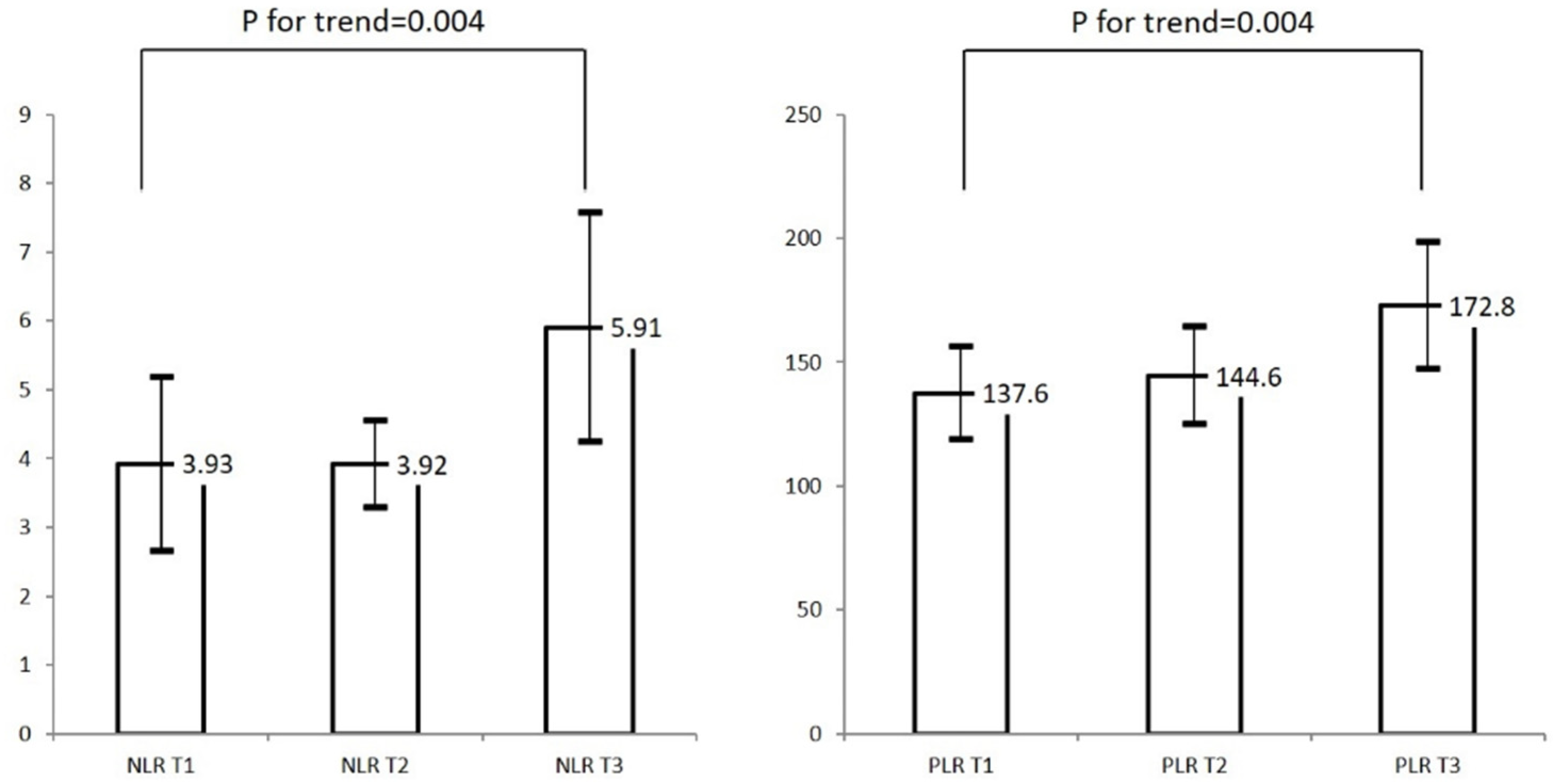
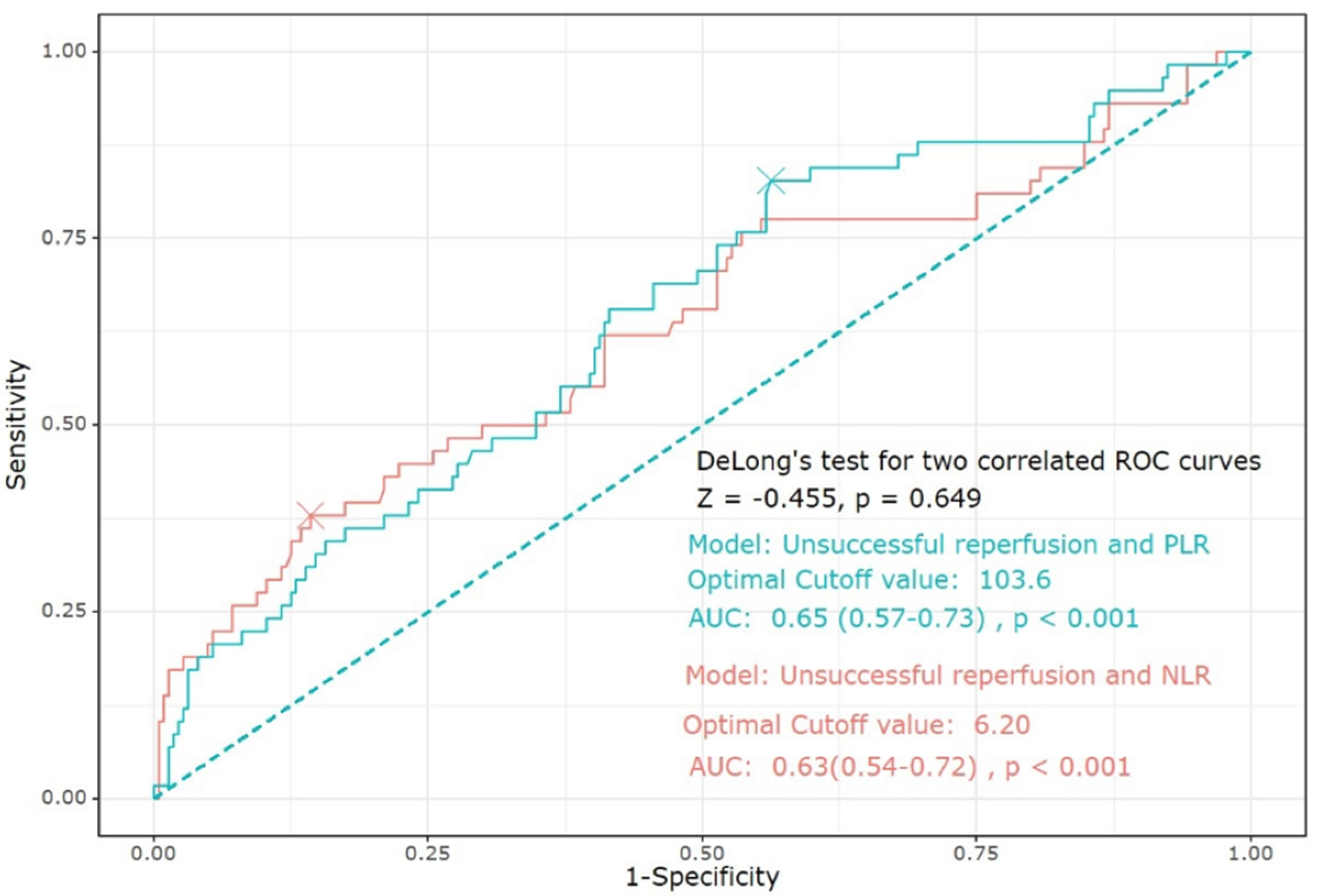
| NLR (IQR) | 2.48 (1.52–4.87) | 3.92 (2.29–8.14) | 0.002 † |
| PLR (IQR) | 113.2 (80.9–168.8) | 147.2 (109.0–227.9) | 0.001 † |
| Infarct volume, cm3 (IQR) | 12.25 (2.64–50.78) | 28.88 (9.20–102.63) | <0.001 † |
| aOR | 95% CI | p-Value | aOR | 95% CI | p-Value | ||
|---|---|---|---|---|---|---|---|
| raw NLR | 1.11 | 1.04–1.19 | 0.001 | raw PLR | 1.004 | 1.001–1.01 | 0.01 |
| NLR T1 | reference | PLR T1 | reference | ||||
| NLR T2 | 1.33 | 0.56–3.12 | 0.52 | PLR T2 | 2.56 | 1.06–6.22 | 0.04 |
| NLR T3 | 2.51 | 1.11–5.70 | 0.03 | PLR T3 | 2.84 | 1.15–6.99 | 0.02 |
| aOR | 95% CI | p-Value | aOR | 95% CI | p-Value | ||
|---|---|---|---|---|---|---|---|
| raw NLR | 1.20 | 1.06–1.35 | 0.004 | raw PLR | 1.01 | 1.004–1.02 | <0.001 |
| NLR T1 | reference | PLR T1 | reference | ||||
| NLR T2 | 2.32 | 1.15–4.70 | 0.02 | PLR T2 | 1.52 | 0.75–3.09 | 0.24 |
| NLR T3 | 3.67 | 1.67–8.06 | 0.001 | PLR T3 | 2.59 | 1.10–5.55 | 0.02 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, S.-H.; Jang, M.U.; Kim, Y.; Park, S.Y.; Kim, C.; Kim, Y.J.; Sohn, J.-H. The Neutrophil-to-Lymphocyte and Platelet-to-Lymphocyte Ratios Predict Reperfusion and Prognosis after Endovascular Treatment of Acute Ischemic Stroke. J. Pers. Med. 2021, 11, 696. https://doi.org/10.3390/jpm11080696
Lee S-H, Jang MU, Kim Y, Park SY, Kim C, Kim YJ, Sohn J-H. The Neutrophil-to-Lymphocyte and Platelet-to-Lymphocyte Ratios Predict Reperfusion and Prognosis after Endovascular Treatment of Acute Ischemic Stroke. Journal of Personalized Medicine. 2021; 11(8):696. https://doi.org/10.3390/jpm11080696
Chicago/Turabian StyleLee, Sang-Hwa, Min Uk Jang, Yerim Kim, So Young Park, Chulho Kim, Yeo Jin Kim, and Jong-Hee Sohn. 2021. "The Neutrophil-to-Lymphocyte and Platelet-to-Lymphocyte Ratios Predict Reperfusion and Prognosis after Endovascular Treatment of Acute Ischemic Stroke" Journal of Personalized Medicine 11, no. 8: 696. https://doi.org/10.3390/jpm11080696
APA StyleLee, S.-H., Jang, M. U., Kim, Y., Park, S. Y., Kim, C., Kim, Y. J., & Sohn, J.-H. (2021). The Neutrophil-to-Lymphocyte and Platelet-to-Lymphocyte Ratios Predict Reperfusion and Prognosis after Endovascular Treatment of Acute Ischemic Stroke. Journal of Personalized Medicine, 11(8), 696. https://doi.org/10.3390/jpm11080696






