Abstract
Social cognition is strongly linked to social functioning outcomes, making it a promising treatment target. Because social cognition measures tend to be sensitive to linguistic and cultural differences, existing measures should be evaluated based on their relevance for Japanese populations. We aimed to establish an expert consensus on the use of social cognition measures in Japanese populations to provide grounds for clinical use and future treatment development. We assembled a panel of experts in the fields of schizophrenia, social psychology, social neuroscience, and developmental disorders. The panel engaged in a modified Delphi process to (1) affirm expert consensus on the definition of social cognition and its constituent domains, (2) determine criteria to evaluate measures, and (3) identify measures appropriate for Japanese patients with a view toward future quantitative research. Through two online voting rounds and two online video conferences, the panel agreed upon a definition and four-domain framework for social cognition consistent with recent literature. Evaluation criteria for measures included feasibility and tolerability, reliability, clinical effectiveness, validity, and international comparability. The panel finally identified nine promising measures, including one task originally developed in Japan. In conclusion, we established an expert consensus on key discussion points in social cognition and arrived at an expert-selected set of measures. We hope that this work facilitates the use of these measures in Japanese clinical scenarios. We plan to further examine these measures in a psychometric evaluation study.
1. Introduction
Schizophrenia is a severe mental disorder, and many patients with schizophrenia experience some degree of long-lasting functional impairment. One area that is impaired throughout the course of the disease is social cognition, which is defined as “the mental operations that underlie social interactions, including perceiving, interpreting, and generating responses to the intentions, dispositions, and behaviors of others” [1]. Social cognitive impairments directly affect patients’ social participation and capacity to build and maintain social relationships, thereby profoundly decreasing quality of life. This area has garnered considerable interest in recent years because the social cognition construct is believed to be more strongly linked to social functioning outcomes than traditional neurocognition [2], making it a promising treatment target.
With the emergence of social cognition as a major focus of schizophrenia research, numerous measures have been developed to assess its various aspects. However, the complexity and breadth of the social cognition construct, together with a lack of consensus regarding its constituent subdomains, has resulted in an overwhelming variety of measures based on differing theories and interpretations. Paradoxically, there is a dearth of widely accepted and standardized measures available for practical use. The Social Cognition Psychometric Evaluation (SCOPE) study aimed to establish a consensus on the theoretical structure of social cognition in schizophrenia and to systematically evaluate the psychometric properties of existing measures [3,4,5]. Four core theoretical domains of social cognition were established through expert surveys and RAND expert panel discussions: emotion processing, attributional style/bias, social perception, and theory of mind (ToM) [3]. Experts further identified the existing measures best suited to assess these domains. Two large-scale studies of schizophrenia patients and healthy control groups were subsequently conducted to examine the psychometric properties of 11 measures. Three measures showing particularly strong psychometric properties and associations with functional outcomes were recommended for use in clinical trials: the Hinting task [6], the Bell Lysaker Emotion Recognition Task (BLERT) [7], and the Penn Emotion Recognition Task (ER-40) [8].
The SCOPE study represents a significant step forward by providing a provisional battery of measures and a springboard for future endeavors. However, these results were based on data collected exclusively in the United States and may not be generalizable to different cultural contexts. Social cognition tasks are more sensitive to cultural and linguistic differences than neurocognitive tasks [9]. Stimuli for social cognition tasks often require the participant to understand social interactions. The “correct” interpretation of a social situation may be less obvious or even entirely different for people from a different culture. Stimuli may also include words or ambiguous dialogue with meanings that are not fully replicable across languages. Furthermore, there are believed to be baseline cultural differences in social cognitive ability and tendencies [10]. In short, the same measures established in the United States may not be suitable for assessing social cognition in other, particularly non-English-speaking, cultures. Thus, the cultural relevance and translatability of tasks must be individually considered for each culture [11].
Until recently, social cognition research in Asian populations has been limited to specific domains or been inconsistent in its choice of measures [12,13,14]. Following the SCOPE study, Lim et al. conducted a psychometric evaluation study examining a similar array of social cognition tasks with Singaporean schizophrenia patients and healthy controls [15]. All participants were fluent in English, and tasks were registered verbatim, without any modifications to the original English versions. The results were consistent with those of the SCOPE study in that the BLERT and ER-40 showed the strongest psychometric properties. However, contrary to the SCOPE study, the Hinting task showed less favorable characteristics. A possible explanation offered by the authors was that some of the vignettes used in the task could be culturally sensitive. These results suggest that, even with a shared language, social cognition tasks may show differing psychometric properties among populations with different cultural backgrounds. However, this study did not examine associations with neurocognitive and social functioning measures.
To our knowledge, no comprehensive psychometric evaluation studies in non-English-speaking populations have been conducted using either translated or originally non-English tasks. Such an attempt would face several new challenges. First, many social cognition tasks include ambiguous phrases or dialogue, which may be difficult to translate fully. Another factor is the anticipated correlation between familiarity with a culture and fluency in its language and its effect on task performance. In other words, in a typically non-English speaking country or cultural group, individuals fluent in English would be expected to have more insight into Western culture and thus may perform better on certain Western-developed tasks. The presence of such factors dictates the need to consider alternative social cognition measures than those originally developed in the Anglosphere.
The present study aimed to identify social cognition measures suitable for use in Japanese schizophrenia patients. It represents a pioneering attempt to systematically investigate the utility of social cognition measures for a non-English-speaking population. An expert panel was assembled and tasked with selecting a comprehensive group of measures that are relevant for the target population while also consistent with the abovementioned related studies.
2. Materials and Methods
2.1. Expert Panel Members
Expert panel members were recruited using a reputation-based snowball sampling procedure. Panel members were chosen from Japanese researchers performing psychological, neurobiological, psychophysiological, or neuroimaging research in the area of social cognition, broadly defined. Experts from fields other than schizophrenia were included to incorporate important concepts from closely related areas. Ultimately, nine experts in the areas of social psychology, social neuroscience, schizophrenia, and developmental disorders agreed to serve as panelists (Table S1). No panelists reported financial conflicts of interest.
2.2. Key Discussion Points and Candidate Social Cognition Measures
We prepared a draft of items comprising key discussion points for establishing an expert consensus. This list included the definition and core domains of social cognition, the target population for the social cognition measures selected in this study, objectives for their use, and evaluation criteria for final recommendations following a psychometric evaluation study.
The definition of social cognition was quoted from the NIMH Workshop on Social Cognition in Schizophrenia [1], as this definition that had already garnered consensus from several experts in the SCOPE study [3]. We prepared a preliminary list of candidate social cognition measures to be considered by the expert panel. Measures were selected based on similar studies examining the psychometric properties of social cognition measures. The SCOPE study recommendations were given particular importance, although measures cited as promising but ultimately excluded were also reconsidered. In addition, the authors inspected the literature for relevant or promising social cognition measures that were originally developed in Japan or with pre-existing Japanese versions. The resulting list comprised 15 preliminary candidate measures, including all six measures recommended by the SCOPE study and two measures developed in Japan. The remaining measures were selected based on history of use in Japanese populations (Table 1). The principal investigators and secretariat then prepared a database listing the results of previous studies that examined the psychometric properties for each measure (Table S3).

Table 1.
Candidate social cognition measures.
2.3. The Modified Delphi Process
This study used a modified Delphi process (RAND/UCLA appropriateness method) to (1) reaffirm consensus on the definition of the social cognition construct and its key domains, (2) establish criteria for evaluating the appropriateness of social cognition measures for use in Japanese populations, and (3) rate and select measures based on the established criteria with a view toward future psychometric evaluation studies (see Figure 1) [28,29]. This method was also chosen for the SCOPE study as a proven method to develop consensus-based test batteries, having been successfully used in the development of the MATRICS battery [30] and VALERO initiative [31] in the field of schizophrenia research [3]. We defined consensus as when the compilation of item statements reached approval of 80% or higher [32] in online voting sessions conducted via the Google Forms website. Panelists had approximately 2 weeks to complete each of the online surveys. Voting was repeated until consensus was reached on all items. After each round, iterative refinements were made to the item compilation based on participant feedback.
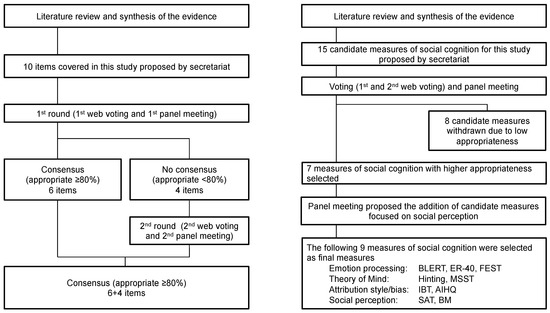
Figure 1.
Overview of voting process.
Panelists rated the appropriateness of each measure for use in Japanese schizophrenia patients based on the following criteria: (1) practicality of administration and tolerability for participants, (2) reliability, (3) utility, (4) convergent and criterion validity, and (5) international comparability. Panel members were provided with detailed descriptions of each measure, including psychometric data from the SCOPE study if available, along with a supplementary database of psychometric indicators for each measure that we compiled from the literature (Table S3). Ratings were given on a 9-point scale, where 1 was “extremely inappropriate” and 9 was “extremely appropriate.” Panel members were also encouraged to provide feedback on individual items through a free form comment section. After each round, the results were compiled to prepare a summary document that presented the raw rating, mean, and median scores in histograms, together with individual comments gathered from each panel member. These documents were shared and used as a basis for the discussion rounds, where individual rating discrepancies were addressed. Certain points were agreed upon beforehand; 7 measures were to be selected from the 15 candidates for inclusion in a subsequent psychometric evaluation study, and the selected measures were to, as a whole, address as wide a range of social cognition domains as possible. Discussions were held in the form of online video conferences because of the COVID-19 pandemic and precautions regarding face-to-face group meetings and traveling.
3. Results
The final list of items agreed upon by the expert panel is shown in Table S2.
3.1. Definition and Core Domains of Social Cognition
The panel agreed to maintain the well-known NIMH Workshop definition [1] and the four-domain structure of emotion processing, attribution style/bias, social perception, and ToM for social cognition in schizophrenia.
3.2. Target Population, Purpose of Use, and Evaluation Criteria of Social Cognition Measures
The target population for the social cognition measures selected in this study was Japanese schizophrenia patients. It was further specified in the panel discussions that the subsequent psychometric study would target “patients with schizophrenia whose symptoms have stabilized following the medication adjustment period in the acute phase and who are undergoing rehabilitation to improve social function.”
The initial focus of this study was to select measures that could be widely used in clinical practice. However, following discussion, the objectives were expanded to also consider the suitability of the measures for clinical trials.
A set of criteria to assess social cognition measures following the psychometric study was discussed and agreed upon among the panel. Feasibility and tolerability criteria were established in terms of administration time and participant ratings, respectively. Test–retest reliability would be considered acceptable with correlation coefficients greater than or equal to 0.6. Utility as a measure would be assessed in terms of floor and ceiling effects, with emphasis being placed particularly on the absence of floor effects because a task showing ceiling effects may still be useful for clinical purposes such as screening and aiding diagnosis. However, if a task is to be used as an outcome for interventional studies, the absence of both floor and ceiling effects across administration times was agreed to be favorable. Measures showing clear group differences between patients and healthy controls would be favored. Correlation with social function outcomes would also be emphasized. Incremental validity, or, in this case, increased predictive ability of social function outcomes beyond neurocognition, would also be given consideration. Finally, tasks recommended in the SCOPE study were agreed to be favorable in terms of international comparability. Grading criteria were modified so that grades would be considered for each purpose of use. Specific advantages and precautions for the use of each test would be described in the final article.
3.3. Panel Ratings and Selection of Social Cognition Measures
Descriptive statistics for the two rounds of panel ratings are provided in Table 2. A set of consensus measures was selected based on the final ratings. Seven tasks with the highest mean appropriateness ratings were selected: three tasks representing the emotion processing domain (the BLERT, ER-40, and Facial Emotion Selection Test (FEST)) and two tasks each for the domains of attributional style/bias (the Ambiguous Intentions and Hostility Questionnaire (AIHQ) and the Intentionality Bias Task (IBT)) and ToM (the Hinting Task and the Metaphor and Sarcasm Scenario Test (MSST)) (Table 3). No social perception tasks were included in the initially planned selection of seven tasks, prompting an additional discussion regarding whether the omission of a previously established core domain was acceptable. Ultimately, it was unanimously agreed to include two tasks representing social perception: The Social Attribution Task-Multiple Choice (SAT-MC) and the Biological Motion (BM) task. Thus, a total of nine measures representing each of the four established core domains comprised the final selection.

Table 2.
Results of the expert panel ratings.

Table 3.
List and descriptions of the final measures.
4. Discussion
Our primary aim was to identify social cognition measures appropriate for Japanese schizophrenia patients based on the opinions of experts in related fields, with a view toward future quantitative research. After establishing grounds for measure selection, the panel rated and discussed the suitability of 15 candidate measures (Table 2), ultimately arriving at nine measures representing all four domains (Table 3).
We first sought to obtain an expert consensus on the definition and theoretical framework of the social cognition construct. Our proposal of using the same four core domains established in the SCOPE study was met with some debate in the initial round of surveys. Several experts questioned the inclusion of the social perception domain, with concerns about the lack of clarity surrounding its definition and scope and an absence of well-established tasks. However, it was agreed that such shortcomings underscore the need for inclusion and further investigation of the construct. Other experts were concerned about the omission of metacognitive aspects. Nonetheless, the panel ultimately agreed to adopt the proposed four-domain structure, citing the importance of consistency and international comparability.
Initially, the target population was not specified to any stage of schizophrenia. However, it was pointed out that performance on social cognition tasks would vary significantly depending on what stage the patient was in and that such variance would make it difficult to adequately evaluate tasks’ psychometric properties. The panel agreed to narrow the target population to more stable patients, as they would also be the main targets for treatments to improve social functioning. The initial target population also included outpatients only. However, the panel discussed the need to address social cognitive dysfunctions in chronic patients hospitalized for reasons other than pure severity of symptoms, such as those in forensic psychiatric wards or patients with problematic behaviors not directly related to psychosis. Thus, the phrasing was modified to include such patients.
Two of the selected measures, the MSST and BM, are novel tasks that have yet to be systematically examined in the context of social cognition in schizophrenia. Furthermore, the MSST is a task that was developed in Japan. The panel unanimously agreed that the nature of this study as one of the first attempts to examine social cognition tasks in a non-English context dictates the need to consider tasks already established as suitable for Japanese populations. Although originally intended to evaluate autism spectrum disorder tendencies in children, it was agreed that the MSST could be applied to assess ToM in schizophrenia populations. The BM task has been mentioned in the literature in the context of incorporating social neuroscience paradigms into the field of social cognition [33,34] and specifically as a promising measure to explore the social perception domain [5]. The panel deemed the BM suitable for the particular objectives of this study due to its low dependence on cultural and linguistic factors, which suggests a high level of international comparability.
The AIHQ and SAT-MC were included despite being classified as “not recommended” in the SCOPE study [4,5]. The AIHQ comprises both open-ended, scorer-rated items and self-report Likert scales assessing participants’ responses to negative social situations. Answers for the open-ended questions are coded by two independent raters, which has been speculated to negatively affect psychometrics such as test–retest reliability. Buck et al. suggested that the psychometric properties of the AIHQ could be improved by expanding self-report items and removing the open-ended questions [35]. The Singaporean psychometric evaluation study conducted by Lim et al. showed more favorable results for the AIHQ, further suggesting its utility [15]. The SAT-MC was not included in the initially planned selection of seven tasks but was chosen as the highest rated among candidate social perception tasks. In the SCOPE study, the SAT-MC showed sub-par results in basic psychometrics such as test–retest reliability, owing largely to the use of two independent forms across the two administration times. The use of consistent test forms across administration times may produce more favorable results. In addition, given that the SCOPE study evaluated tasks based on suitability for clinical trials, the SAT-MC may potentially receive more favorable gradings when viewed through the lens of utility in clinical practice. Furthermore, the SAT-MC has long been considered less affected by linguistic and cultural differences than other social cognition tasks because it is non-verbal and less culturally loaded [26,36,37]. A recent cross-cultural study with South Korean and North American schizophrenia patients and healthy controls showed the SAT-MC to be consistent across groups and supported its utility across language and cultures [13], making it a strong candidate for our current study.
Notable omissions included the Eyes test and The Awareness of Social Inference Test (TASIT), which were both included in the SCOPE recommendations. The Eyes test was seen as possibly not suitable for Japanese populations due to cultural differences; in Japan, it is considered rude to stare at someone’s face and it is therefore not customary to read others’ emotions through their eyes. There was also further concern that the Eyes test significantly overlaps with emotion processing, despite being classified as a measure of ToM. The TASIT, which uses short but relatively complex video vignettes of actors enacting various social interactions, received lower ratings mainly due to concerns over translatability. Many experts also shared the opinion that certain task structures, such as the TASIT, are inherently more dependent on working memory, with performance on these tasks at risk of reflecting neurocognitive ability more strongly than social cognitive function.
This study is not without its limitations. First, it was largely influenced by the SCOPE study, and measures indicated in the SCOPE study therefore received more attention than others. We attempted to reduce these limitations by reconsidering measures not recommended by the SCOPE study and conducting a search of literature for Japanese-developed social cognition measures. Furthermore, our reliance on the SCOPE study for guidance meant inheriting its limitations regarding the social perception domain and lack of strong candidate measures to represent it. The expert rating results and ensuing discussions also suggested that the objectives of the present study may have inadvertently led to emotion processing tasks being favored because their simpler structures seemingly make them less vulnerable to changes in psychometrics caused by translation to Japanese. These observations were addressed in the panel discussions and ultimately influenced the decision to include a roughly equal number of measures from each of the four core domains. Another limitation is the relatively small number of experts recruited. Diversity regarding fields of expertise may have been somewhat limited, with relatively high weight on the field of schizophrenia and only one expert representing another clinical population (developmental disorders). Furthermore, this study may have benefited from including experts from other academic fields, such as cultural anthropology, to provide a more rigid examination of which tasks may or may not be appropriate for Japanese people.
The present study established an expert consensus on key discussion points and promising measures for assessing social cognition in Japanese schizophrenia patients. There is currently a lack of available information regarding the use of social cognition measures in a non-English-speaking cultural context. We hope that our research will inform and facilitate future endeavors in other countries. Subsequent phases of this study will involve a multi-center psychometric evaluation study in Japanese schizophrenia and healthy control populations using the expert-selected measures. However, a considerable portion of the selected tasks has yet to be validated in Japanese schizophrenia populations (BLERT, BM, and MSST) or even translated to Japanese (SAT-MC and IBT). A pilot study may be warranted to preliminarily confirm the utility and structural validity of the tasks and to identify any need for modifications. Cross-cultural studies comparing results among groups of different cultural and linguistic backgrounds may shed further light on which measures are more suitable for international comparison and collaborative research.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/jpm11040275/s1, Table S1: Expert panel members, Table S2: List of items agreed upon by the expert panel, Table S3: Supplementary data for candidate social cognition measures.
Author Contributions
Conceptualization, R.O., S.I., H.O., R.K., N.H., A.T., A.M., Y.S., and Y.Y.; writing—original draft preparation, H.O.; writing—review and editing, R.O. and S.I.; supervision, T.N. and M.M. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by AMED, grant number JP20dk0307092.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Institutional Review Board of National Center of Neurology and Psychiatry Hospital (B2020-107; 7 December 2020).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
None.
Acknowledgments
We would like to thank the expert panel members for their participation: Akiko Kikuchi, Toshiya Murai, Shinichi Niwa, Tomiki Sumiyoshi, Tatsuya Koeda, Motomu Suga, Daisuke Haga, and Jun Tayama. We would also like to thank Kazuyuki Nakagome for his role in selecting the panel members and reviewing this article.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Green, M.F.; Penn, D.L.; Bentall, R.; Carpenter, W.T.; Gaebel, W.; Gur, R.C.; Kring, A.M.; Park, S.; Silverstein, S.M.; Heinssen, R. Social cognition in schizophrenia: An NIMH workshop on definitions, assessment, and research opportunities. Schizophr. Bull. 2008, 34, 1211–1220. [Google Scholar] [CrossRef] [PubMed]
- Pinkham, A.E.; Penn, D.L. Neurocognitive and social cognitive predictors of interpersonal skill in schizophrenia. Psychiatry Res. 2006, 143, 167–178. [Google Scholar] [CrossRef] [PubMed]
- Pinkham, A.E.; Penn, D.L.; Green, M.F.; Buck, B.; Healey, K.; Harvey, P.D. The social cognition psychometric evaluation study: Results of the expert survey and RAND panel. Schizophr. Bull. 2014, 40, 813–823. [Google Scholar] [CrossRef] [PubMed]
- Pinkham, A.E.; Penn, D.L.; Green, M.F.; Harvey, P.D. Social Cognition Psychometric Evaluation: Results of the Initial Psychometric Study. Schizophr. Bull. 2016, 42, 494–504. [Google Scholar] [CrossRef] [PubMed]
- Pinkham, A.E.; Harvey, P.D.; Penn, D.L. Social Cognition Psychometric Evaluation: Results of the Final Validation Study. Schizophr. Bull. 2018, 44, 737–748. [Google Scholar] [CrossRef]
- Corcoran, R.; Mercer, G.; Frith, C.D. Schizophrenia, symptomatology and social inference: Investigating “theory of mind” in people with schizophrenia. Schizophr. Res. 1995, 17, 5–13. [Google Scholar] [CrossRef]
- Bryson, G.; Bell, M.; Lysaker, P. Affect recognition in schizophrenia: A function of global impairment or a specific cognitive deficit. Psychiatry Res. 1997, 71, 105–113. [Google Scholar] [CrossRef]
- Kohler, C.G.; Turner, T.H.; Bilker, W.B.; Brensinger, C.M.; Siegel, S.J.; Kanes, S.J.; Gur, R.E.; Gur, R.C. Facial emotion recognition in schizophrenia: Intensity effects and error pattern. Am. J. Psychiatry 2003, 160, 1768–1774. [Google Scholar] [CrossRef]
- Hajdúk, M.; Achim, A.M.; Brunet-Gouet, E.; Mehta, U.M.; Pinkham, A.E. How to move forward in social cognition research? Put it into an international perspective. Schizophr. Res. 2020, 215, 463–464. [Google Scholar] [CrossRef]
- Wu, S.; Keysar, B. The effect of culture on perspective taking. Psychol. Sci. 2007, 18, 600–606. [Google Scholar] [CrossRef]
- Mehta, U.M.; Thirthalli, J.; Gangadhar, B.N.; Keshavan, M.S. Need for culture specific tools to assess social cognition in schizophrenia. Schizophr. Res. 2011, 133, 255–256. [Google Scholar] [CrossRef]
- Chen, K.W.; Lee, S.C.; Chiang, H.Y.; Syu, Y.C.; Yu, X.X.; Hsieh, C.L. Psychometric properties of three measures assessing advanced theory of mind: Evidence from people with schizophrenia. Psychiatry Res. 2017, 257, 490–496. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.S.; Corbera, S.; Poltorak, A.; Park, K.; Assaf, M.; Bell, M.D.; Wexler, B.E.; Cho, Y.I.; Jung, S.; Brocke, S.; et al. Measuring theory of mind in schizophrenia research: Cross-cultural validation. Schizophr. Res. 2018, 201, 187–195. [Google Scholar] [CrossRef]
- Mehta, U.M.; Thirthalli, J.; Naveen Kumar, C.; Mahadevaiah, M.; Rao, K.; Subbakrishna, D.K.; Gangadhar, B.N.; Keshavan, M.S. Validation of Social Cognition Rating Tools in Indian Setting (SOCRATIS): A new test-battery to assess social cognition. Asian J. Psychiatry 2011, 4, 203–209. [Google Scholar] [CrossRef] [PubMed]
- Lim, K.; Lee, S.A.; Pinkham, A.E.; Lam, M.; Lee, J. Evaluation of social cognitive measures in an Asian schizophrenia sample. Schizophr. Res. Cogn. 2020, 20, 100169. [Google Scholar] [CrossRef] [PubMed]
- Kerr, S.L.; Neale, J.M. Emotion perception in schizophrenia: Specific deficit or further evidence of generalized poor performance? J. Abnorm. Psychol. 1993, 102, 312–318. [Google Scholar] [CrossRef] [PubMed]
- Minoshita, S.; Morita, N.; Yamashita, T.; Yoshikawa, M.; Kikuchi, T.; Satoh, S. Recognition of affect in facial expression using the Noh Mask Test: Comparison of individuals with schizophrenia and normal controls. Psychiatry Clin. Neurosci. 2005, 59, 4–10. [Google Scholar] [CrossRef]
- Stone, V.E.; Baron-Cohen, S.; Knight, R.T. Frontal lobe contributions to theory of mind. J. Cogn. Neurosci. 1998, 10, 640–656. [Google Scholar] [CrossRef] [PubMed]
- Adachi, T.; Koeda, T.; Hirabayashi, S.; Maeoka, Y.; Shiota, M.; Wright, E.C.; Wada, A. The metaphor and sarcasm scenario test: A new instrument to help differentiate high functioning pervasive developmental disorder from attention deficit/hyperactivity disorder. Brain Dev. 2004, 26, 301–306. [Google Scholar] [CrossRef]
- Baron-Cohen, S.; Wheelwright, S.; Hill, J.; Raste, Y.; Plumb, I. The “Reading the Mind in the Eyes” Test revised version: A study with normal adults, and adults with Asperger syndrome or high-functioning autism. J. Child Psychol. Psychiatry 2001, 42, 241–251. [Google Scholar] [CrossRef]
- McDonald, S.; Flanagan, S.; Rollins, J.; Kinch, J. TASIT: A new clinical tool for assessing social perception after traumatic brain injury. J. Head Trauma Rehabil. 2003, 18, 219–238. [Google Scholar] [CrossRef] [PubMed]
- Combs, D.R.; Penn, D.L.; Wicher, M.; Waldheter, E. The Ambiguous Intentions Hostility Questionnaire (AIHQ): A new measure for evaluating hostile social-cognitive biases in paranoia. Cogn. Neuropsychiatry 2007, 12, 128–143. [Google Scholar] [CrossRef] [PubMed]
- Rosset, E. It′s no accident: Our bias for intentional explanations. Cognition 2008, 108, 771–780. [Google Scholar] [CrossRef]
- Roberts, D.L.; Fiszdon, J.; Tek, C. Initial validity of the Social Cognition Screening Questionnaire (SCSQ). Schizophr. Bull. 2011, 37 (Suppl. 1), 280. [Google Scholar]
- Hashimoto, N.; Toyomaki, A.; Hirai, M.; Miyamoto, T.; Narita, H.; Okubo, R.; Kusumi, I. Absent activation in medial prefrontal cortex and temporoparietal junction but not superior temporal sulcus during the perception of biological motion in schizophrenia: A functional MRI study. Neuropsychiatry Dis. Treat. 2014, 10, 2221–2230. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Bell, M.D.; Fiszdon, J.M.; Greig, T.C.; Wexler, B.E. Social attribution test--multiple choice (SAT-MC) in schizophrenia: Comparison with community sample and relationship to neurocognitive, social cognitive and symptom measures. Schizophr. Res. 2010, 122, 164–171. [Google Scholar] [CrossRef]
- Corrigan, P.W.; Green, M.F. The Situational Feature Recognition Test: A Measure of Schema Comprehension for Schizophrenia; John Wiley & Sons: Hoboken, NJ, USA, 1993; pp. 29–35. [Google Scholar]
- Fitch, K.; Bernstein, S.J.; Aguilar, M.D.; Burnand, B.; LaCalle, J.R.; Lazaro, P.; van het Loo, M.; McDonnell, J.; Vader, J.; Kahan, J.P. The RAND/UCLA Appropriateness Method User′s Manual; RAND Corporation: Santa Monica, CA, USA, 2001. [Google Scholar]
- Hasson, F.; Keeney, S.; McKenna, H. Research guidelines for the Delphi survey technique. J. Adv. Nurs. 2000, 32, 1008–1015. [Google Scholar]
- Marder, S.R.; Fenton, W. Measurement and Treatment Research to Improve Cognition in Schizophrenia: NIMH MATRICS initiative to support the development of agents for improving cognition in schizophrenia. Schizophr. Res. 2004, 72, 5–9. [Google Scholar] [CrossRef]
- Leifker, F.R.; Patterson, T.L.; Heaton, R.K.; Harvey, P.D. Validating measures of real-world outcome: The results of the VALERO expert survey and RAND panel. Schizophr. Bull. 2011, 37, 334–343. [Google Scholar] [CrossRef]
- Green, B.; Jones, M.; Hughes, D.; Williams, A. Applying the Delphi technique in a study of GPs′ information requirements. Health Soc. Care Community 1999, 7, 198–205. [Google Scholar] [CrossRef]
- Kern, R.S.; Penn, D.L.; Lee, J.; Horan, W.P.; Reise, S.P.; Ochsner, K.N.; Marder, S.R.; Green, M.F. Adapting social neuroscience measures for schizophrenia clinical trials, Part 2: Trolling the depths of psychometric properties. Schizophr. Bull. 2013, 39, 1201–1210. [Google Scholar] [CrossRef] [PubMed]
- Olbert, C.M.; Penn, D.L.; Kern, R.S.; Lee, J.; Horan, W.P.; Reise, S.P.; Ochsner, K.N.; Marder, S.R.; Green, M.F. Adapting social neuroscience measures for schizophrenia clinical trials, part 3: Fathoming external validity. Schizophr. Bull. 2013, 39, 1211–1218. [Google Scholar] [CrossRef] [PubMed]
- Buck, B.; Iwanski, C.; Healey, K.M.; Green, M.F.; Horan, W.P.; Kern, R.S.; Lee, J.; Marder, S.R.; Reise, S.P.; Penn, D.L. Improving measurement of attributional style in schizophrenia; A psychometric evaluation of the Ambiguous Intentions Hostility Questionnaire (AIHQ). J. Psychiatry Res. 2017, 89, 48–54. [Google Scholar] [CrossRef] [PubMed]
- Horan, W.P.; Nuechterlein, K.H.; Wynn, J.K.; Lee, J.; Castelli, F.; Green, M.F. Disturbances in the spontaneous attribution of social meaning in schizophrenia. Psychol. Med. 2009, 39, 635–643. [Google Scholar] [CrossRef] [PubMed]
- Johannesen, J.K.; Lurie, J.B.; Fiszdon, J.M.; Bell, M.D. The Social Attribution Task-Multiple Choice (SAT-MC): A Psychometric and Equivalence Study of an Alternate Form. ISRN Psychiatry 2013, 2013, 830825. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).