1. Introduction
In breast imaging, there are many diagnostic techniques that, with various modalities and different performance levels, detect breast cancer early and estimate residual disease. The best known are mammography (MG), ultrasound (US), and breast magnetic resonance imaging (MRI). New imaging techniques such as digital breast tomosynthesis (DBT), contrast-enhancement spectral mammography (CESM), and automated breast ultrasound (ABUS) have recently been introduced.
Establishing a correct response to oncological therapies is particularly complicated in exclusively morphological techniques such as mammography, especially in findings such as distortions, microcalcifications, or spiculated masses in which the quotas attributable to fibrosis, desmoplastic reaction, and neoplastic vital residue often appear indistinguishable [
1]. This problem is overcome with contrast techniques, MRI and CESM, that emphasize the tumor areas with active neoangiogenesis by separating them from the areas with fibrosis and necrosis, which better highlights the complete pathological response (pCR) [
1,
2]. MRI is an older, more widespread and studied technique than CESM. It is multiparametric, three-dimensional, and has no exposure to X-rays, which is why it is of preferential use compared to the latter, even if the performances between the latter two techniques are comparable [
2]. Some authors suggest that MRI is more accurate than other imaging modalities for assessing residual disease after neoadjuvant chemotherapy (NAC) [
1].
Studying tumor microenvironments represents the next frontier in oncological therapies, as it will help quantify the evolution of diseases in the coming years and possibly predict tumor recurrence or progression [
3].
In this context, an emerging parameter in breast imaging, which could represent the microenvironment characteristics, is the background of parenchymal enhancement (BPE). BPE is defined as the normal background impregnation of the gland after gadolinium injection [
4,
5,
6] related to the physiological vascularization and perfusion of breast tissue [
7,
8,
9,
10,
11].
Several studies detected a high value of BPE as a decisive predictive factor of breast cancer risk, regardless of other typical factors such as breast density. Moreover, BPE is frequently associated with a higher incidence of ductal carcinoma in situ [
12,
13,
14,
15]. A more evident BPE around the tumor, associated with a high T stage, represents a potential independent factor related to shorter disease-free survival [
16].
A moderate to high BPE may also impact the diagnostic sensitivity and accuracy of an MRI test [
17,
18,
19] Therefore, BPE has been recently included in the MRI’s Lexicon ACR-BIRADS [
20,
21], which suggests reporting distribution and intensity through a subdivision into four classes: minimal (BPE <25% of glandular tissue demonstrating enhancement), mid (25–50% enhancement), moderate (50–75% enhancement)), and marked (>75% enhancement).
According to some previous studies, BPE is considered to be a potential predictor of response to neoadjuvant therapy [
22,
23,
24,
25,
26]. In particular, the reduction in BPE intensity over time, measured by MRI in the disease-free breast, depends on the menopausal status and appears to be more associated with pCR than NAC. However, it could also be related to ovarian suppression caused by chemotherapy and to the better vascularization and vasal permeability of certain types of breasts. This type of assessment is still being studied; particularly, the information concerning pre-treatment BPE intensity [
4,
6,
22,
26,
27,
28,
29,
30] appears to be controversial. For the reasons mentioned above, BPE is considered an interesting diagnostic and prognostic indicator in breast oncology, yet some aspects are still not fully defined and are deserving of further studies.
This evaluation can be carried out by qualitative method, i.e., by the visual evaluation of one or more radiologists, or by automatic or semi-automatic quantitative methods [
25,
30,
31]. It is important to note that assessing BPE using an objective and automated evaluation method may achieve opposite results [
30,
31]. Therefore, more in-depth studies are necessary along with more standardized methods to validate them.
Another aspect of great interest is the effectiveness of specific neoadjuvant treatments that depend on the cancer molecular subtype and treatment [
31]. Since quantitative methods are being developed and are not yet standardized, in this preliminary study, we examine the qualitative assessment of BPE, which is more standardized and suitable in current clinical practice.
This work aims to analyze BPE as a potential prognostic, predictive factor when evaluating the effect of oncological neoadjuvant therapies on the basis of qualitative criteria.
2. Materials and Methods
2.1. Experimental Data
From 1 September 2015 to 31 July 2020, we collected data and MRI images of 80 consecutive patients suffering from breast cancer. These patients were subjected to at least two diagnostic steps in the course of neoadjuvant oncological therapy and treated at the Istituto Tumori “Giovanni Paolo II” of Bari.
Patients were recruited according to the following inclusion criteria:
Patients over the age of 18 with a histological diagnosis of infiltrative breast cancer of various histology (ductal, lobular, other) and various molecular subtypes, with clinical-stage II-III sec. The Classification of Malignant Tumours TNM [
1] 8^ edition received a clinical indication for neoadjuvant chemotherapy.
Carrying out at least two MRI evaluations, i.e., before the onset of oncology treatment and after three months of therapy.
Written informed consent to procedures and use of data.
The exclusion criteria were as follows:
This study was approved by the Scientific Board of the Istituto Tumori “Giovanni Paolo II” and carried out in the manner prescribed by the Helsinki Statement. On the basis of our regulation on retrospective studies, all patients who gave consent to use the data for scientific purposes were recruited.
2.2. Molecular Subtype Characterization and Neoadjuvant Cancer Therapy
In this study, we retrospectively analyzed data from a sample of 80 patients diagnosed with breast cancer from stage I to stage III, according to the TNM 8^ edition. Candidates received neoadjuvant chemotherapy. The different molecular histotypes were also defined by an immunohistochemical assessment of the expression of estrogen and progesterone receptors, as well as ki67 and Her-2 status, according to the molecular classification of the St. Gallen Consensus Conference of 2013 [
32]. They were, therefore, divided into five main groups: luminal A-like; luminal B-like HER2-negative; luminal B-like HER2-positive; HER2-positive non-luminal; triple-negative. The status of HER2 was defined according to the international ASCO-CAP [
3] the American Society of Clinical Oncology and the College of American Pathologists guidelines [
33,
34].
NAC administration followed a specific scheme. For patients with breast cancer, it went as follows: luminal A-like, luminal B-like, HER2-negative, and triple-negative. Next, sequential chemotherapy with four cycles of anthracycline (adriamycin or epirubicin) was combined with cyclophosphamide at three-week intervals for three months, followed by a further three months of therapy with taxanes (i.e., docetaxel for four cycles at three-week intervals or weekly paclitaxel for 12 consecutive weeks). For HER2 positive patients, a combination of taxanes and trastuzumab was used.
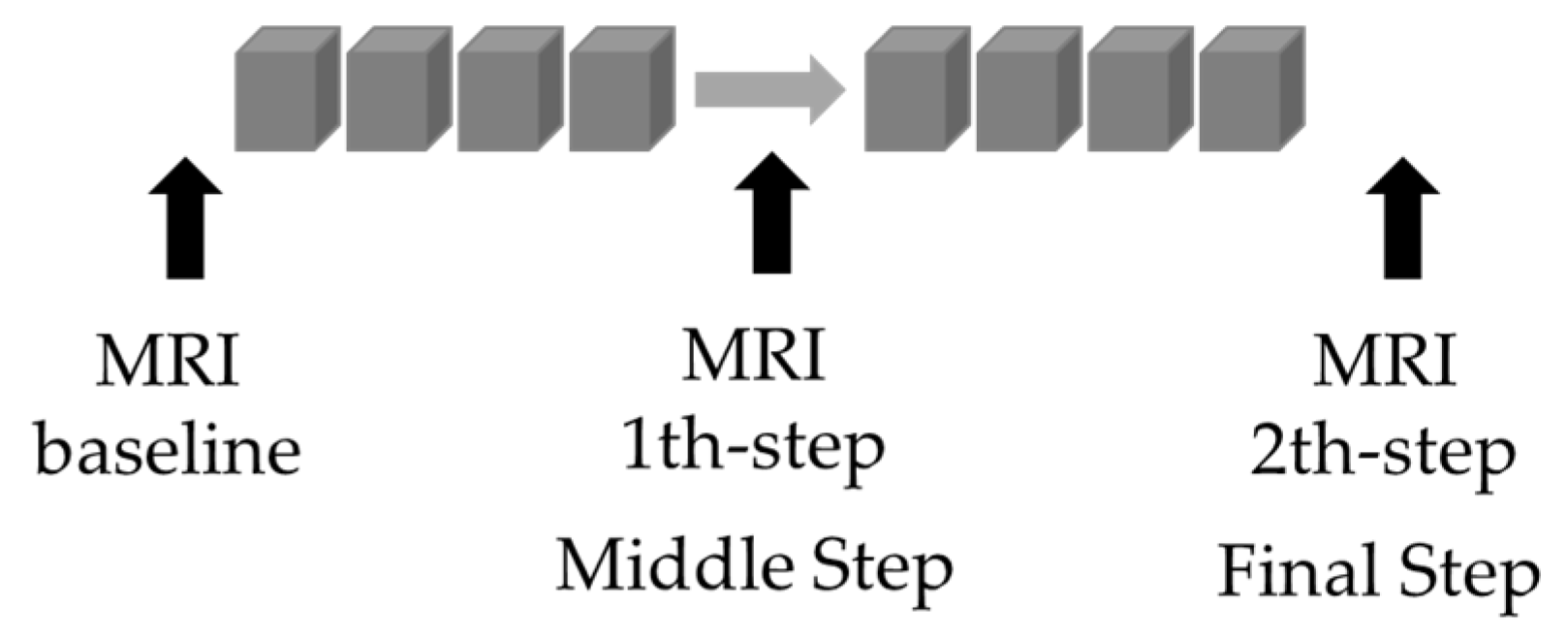
The patients were subjected to MRI timed controls. The first one, defined as the “basaline”, occurred before the beginning of the NAC. The second, defined as “step I or the middle step”, was performed after at least three months of treatment, i.e., after the first four rounds of therapy. The third MRI control, defined as “step II or the final step”, was performed after the end of sequential chemotherapy with taxanes (whether or not combined with anti-HER2 therapy according to the molecular subgroup).
In accordance whit RECIST Criteria [
35], pathological responses to therapy were assessed by considering four possible outcomes:
Complete Response (CR): Disappearance of all target lesions. Any pathological lymph nodes (whether target or non-target) must have reduction in short axis to <10 mm;
Partial Response (PR): At least a 30% decrease in the sum of diameters of target lesions, taking as reference the baseline sum diameters;
Progressive Disease (PD): At least a 20% increase in the sum of diameters of target lesions, taking as reference the smallest sum on study (this includes the baseline sum if that is the smallest on study). In addition to the relative increase of 20%, the sum must also demonstrate an absolute increase of at least 5 mm. (note: the appearance of one or more new lesions is also considered progression);
Stable Disease (SD): Neither sufficient shrinkage to qualify for PR nor sufficient increase to qualify for PD, taking as reference the smallest sum diameters while on study.
The pathological response category was attributed after surgery and evaluated respect to the initial size of the tumor before treatment observed in MRI by considering the RECIST criteria.
2.3. Protocol for Patient Data Collection in Neoadjuvant Therapy
Three radiologists dedicated to breast imaging with 10 or more years of experience with breast MRI examined, in triple-blind modality, the available MRI. They identified the portion of fibroglandular tissue (FGT) and BPE of the contralateral breast to the tumor in the basal control pre-treatment (baseline). In the following steps, they performed these after three months of therapy (intermediate step) and at the end of treatment before surgery (final step). All 80 patients presented at least the basal and intermediate steps to the final observation. Each radiologist independently acquired the BPE and the prevailing class was considered valid. The divergent cases in the evaluations came among operators from a class discussed during a dedicated multidisciplinary meeting to gain consensus.
Investigations were carried out using MRI 1.5 Tesla equipment (Achieva, Philips Medical Systems, Best, The Netherlands). Patients lay prone on dedicated coils while radiologists examined their breasts. For premenopausal patients or women who had still not undergone ovarian suppression, the study was performed in the second week of the cycle. The sequences used were as follows: T1 inversion recovery (STIR), diffusion (DWI), turbo-spin-echo (TSE) without contrast administration, and T1 3D-DCE (6 dynamic acquisitions of 1.5 mm
3 a voxel isotropic of 60 s each, one before and five after intravenous administration, with automatic paramagnetic contrast agent injector at a dose of 0.1 mmol/kg body weight and a flow of 2–2.5 mL/s, followed by 20 mL of saline solution). At the end of the acquisition of dynamic T1 sequences, an automatic subtraction process between post-contrast and pre-contractual images (of the same sequence) allowed for the detection of images subtracted with an emphasis on areas of pathological enhancement in the breast. The investigation was then completed with the creation of I/T [
5] enhancement curves and a maximum intensity projection vascular map (MIP).
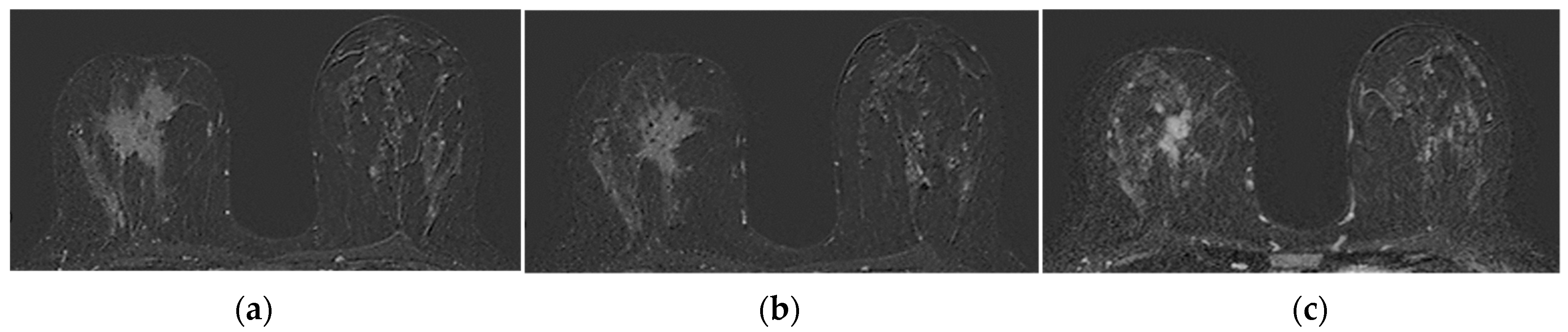
The operators’ assessments of FGT were carried out on the T2 morphological sequences and the first post-contrast acquisition of the dynamic sequence; otherwise, BPE evaluations were carried out on the first post-gadolinium dynamic sequence, as based on the literature [
23,
34]. FGT and BPE were classified according to ACR BIRADS [
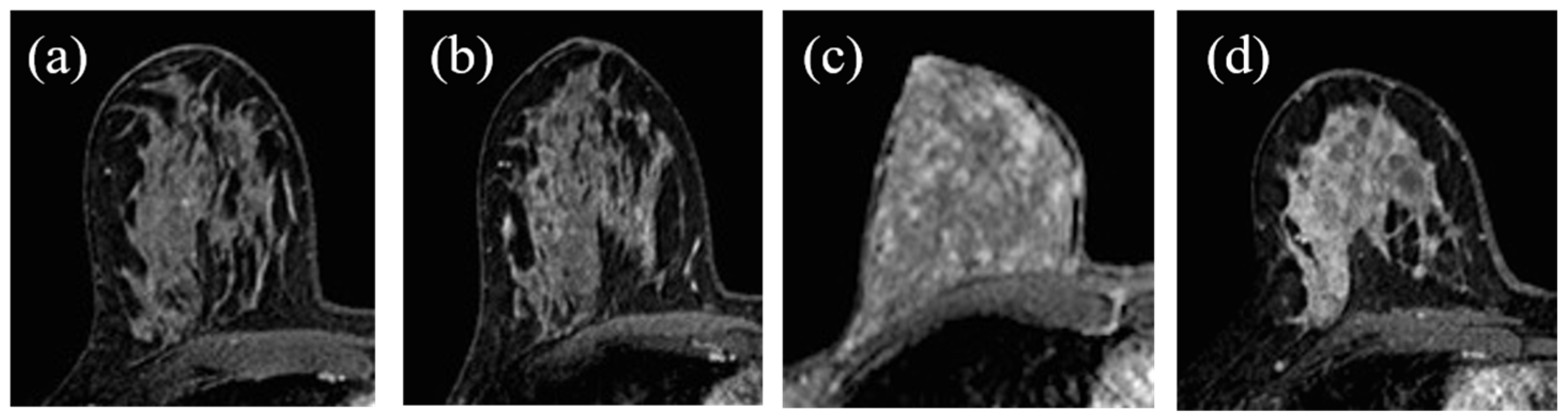
7] criteria in four groups: FGT in almost entirely fat (a), scattered fibro glandular tissue (b), heterogeneous fibro glandular tissue (c), extreme fibro glandular tissue (d), and BPE in minimal (I), mild (II), moderate (III), marked (IV), symmetric, or asymmetric. Examples of this classification are shown in
Figure 1 and
Figure 2.
For the study, we selected and differentiated patients who underwent therapy with anthracyclines and cyclophosphamide in the first three months of treatment and only taxanes (with and without anti-HER2+therapy) in the following three months until the end (
Figure 3).
2.4. Statistical Analysis
The Chi-square test was used to evaluate the significant association between two categorical variables, such as BPE, FGT, the type of therapy, molecular subtype, the menopausal state, response to therapy, and BPE reduction.
Patients were classified into five groups of cancer subtypes according to the St. Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2013 [
32]: luminal A, luminal B HER2 negative, luminal B HER2 positive, HER2 positive non-luminal, and triple-negative.
BPE reduction was assessed considering, for each patient, the transition to a lower class after three months of therapy (BPE middle step) or the end (BPE final step) compared to the basal assessment (BPE baseline).
Cohen’s kappa statistics were used to assess the inter-observer agreement for classifying BPE and FGT.
A result was considered significant when the p-value was less than 0.05. All calculations were performed using SPSS statistical software.
3. Results
Table 1 summarizes the characteristics of the analyzed samples. In total, 80 patients with histologically proven breast cancer aged between 31 and 80 years (with average, first, and fourth quartiles of 49.0, 43.3, and 62.8 years, respectively). All patients had at least two MRI evaluations during neoadjuvant therapy, but only 37.5% (30/80) of patients performed all three steps.
The operators’ evaluation of the FGT and BPE in the three resonance steps had a good level of agreement with a Cohen’s kappa value of about 0.55 for each comparison that was significantly different from 0 (p-values Cohen’s kappa test of each comparison <0.05). However, as described above, the discordant cases over a class (n = 9) were then reassessed and a general consensus was achieved. In the remaining cases, the most represented class was acquired.
Menopausal status was significantly associated with FGT (
Table 2) and baseline BPE (
Table 3). Indeed, patients with low FGT (I, II) and low baseline BPE (minimal, mild) tended to be post-menopausal patients, while patients with high FGT (IV) and baseline BPE (moderate, marked) were pre-menopausal. This was probably related also to the age factor with which the FGT and baseline BPE were significantly associated (
p-value Kruskal–Wallis test < 0.05).
As shown in
Table 4, after the middle-step MRI step, 79.4% of patients with a moderate baseline BPE showed minimal BPE, while 54.4% of patients with a mild baseline BPE showed moderate BPE. Although only 37.5% of the patients in the sample performed the final step MRI, 93.3% of patients with a moderate baseline BPE exhibited a significant class reduction towards the minimal BPE.
Specifically, after the first three months of NAC, 49 patients (61.3%) showed a reduction in the BPE class, while 31 (38.7%) patients maintained the starting class. Among the 30 patients who also performed the final MRI step, 26 (86.7%) showed a class reduction compared to the baseline BPE. BPE reduction was associated with the baseline BPE class; in particular, a reduction was observed when BPE was moderate/mild (
Table 5).
BPE reduction was significantly associated with the chemotherapy administrated in the first round of neoadjuvant therapy (
Table 6). A significant BPE reduction was observed in patients treated with anthracyclines, taxanes, or both. On the other hand, there was no significant association concerning other characteristics examined.
The response to therapy was associated with the size of the lesions. The initial size of the lesion for patients who had a complete response was on average 17.5 mm, while for those who had a partial response was 38.0 mm (
Table 7). The response to therapy was not associated with the menopausal status, age, and molecular subtype of the tumor.
The response to NAC was not associated with FGT, BPE baseline, as well as BPE in the middle and final step (
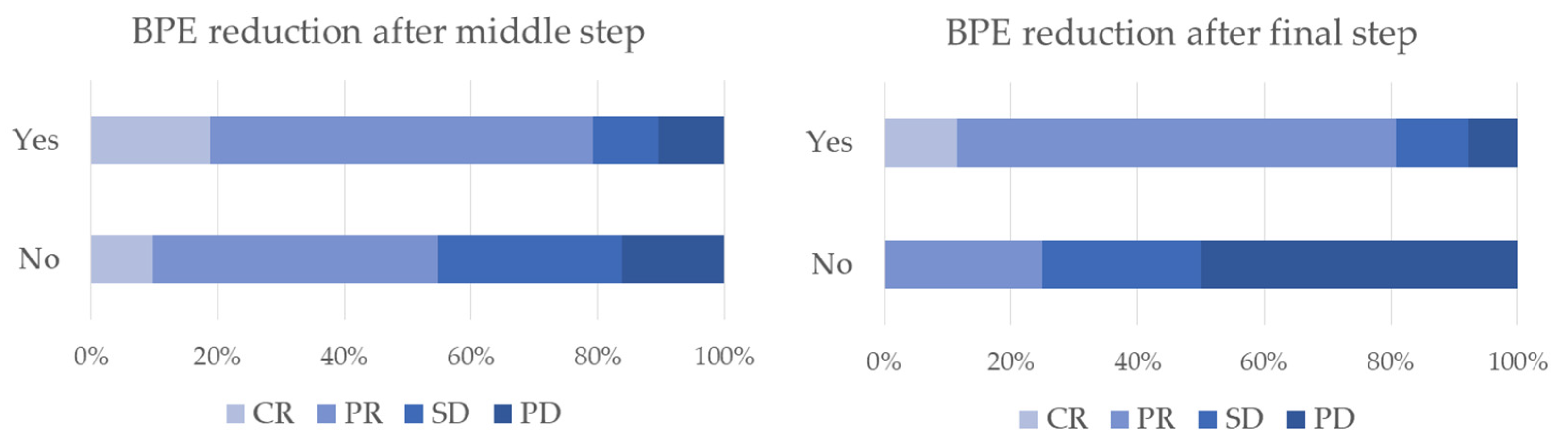
Table 8). We counted the cases that found BPE reduction to be at least one BIRADS class at the middle and/or final step MRI compared to the baseline. The response to therapy was found to be significantly associated with BPE reduction (
Figure 4). Indeed, 61.2% and 18.4% of patients who showed a reduction in BPE after the first three months of NAC had a partial and a complete response; only 45.2% of patients who did not show a reduction in BPE after the first three months of NAC had a partial response, while 29.0% with the disease remained stable (
Table 8). Therefore, sensitivity and specificity for BPE reduction predicted a partial or complete response was 77.6% and 45.2%, respectively, with positive and negative predictive values of 55 and 24, respectively. In addition, there was no significant association between a response to therapy or dosing regimen (
Table 9).
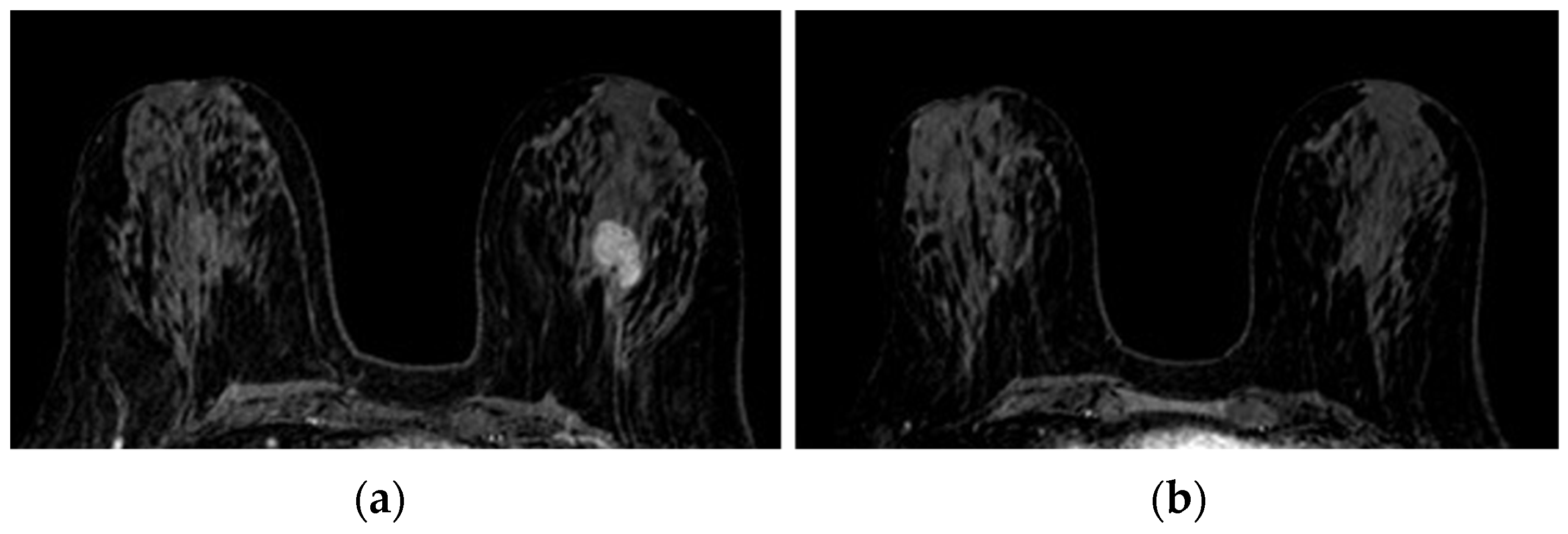
Figure 5,
Figure 6 and
Figure 7 show three different examples of responses to cancer therapies according to the RECIST criteria.
4. Discussion
This study evaluated the possible correlations between changes in BPE (pre-treatment, after the first three months, and at the end of the treatment), FGT, menopausal state, therapies administered, molecular type, and the size of the tumor in breast cancer patients in neoadjuvant oncological treatment.
Menopausal status was associated significantly with FGT and baseline BPE, meaning that patients with both FGT and baseline BPE tended to be post-menopausal, whereas patients with high FGT and a higher baseline BPE were more likely pre-menopausal. These findings are naturally related to the age factor with which FGT and baseline BPE are significantly associated.
FGT is the proportion of fibroglandular tissue present in MRI and resembles mammography density, a known independent risk factor of BP [
13]. FGT is like density on mammography, it can regress with the passing of age and especially after menopause.
Furthermore, BPE, linked to the glandular tissue physiological permeation, depends on several factors including age, hormonal status, ongoing hormonal therapies, previous radiotherapy, and ovariectomy [
4,
6,
7,
8,
9,
10,
11].
In a qualitative analysis, it is also essential to precisely establish the research criteria. Indeed, according to the ACR guidelines, analyses should be performed on the first dynamic sequence after gadolinium, even if some authors verified the reliability of the measurements, subtractions, or the first three post-gadolinium sequences in an automated form after consensus between two or more radiologists [
8,
17,
23,
24]. On the basis of these indications, the observational evaluation in this study was conducted in the first post-contrast dynamic.
The qualitative measurement of these class parameters was also subject to inter-intra-observer variability [
25,
30,
31,
36,
37,
38] and would require the consensus of three radiologists through BIRADS criteria [
20,
39]. Therefore, an independent qualitative analysis with three different operators was carried out in order to minimize variability. This allowed us to reduce the number of discordant cases beyond one class (9/80 patients), which was then collectively revaluated in order to acquire a consensus.
The results of this study show a statistically significant reduction of the BPE class during serial evaluation performed in the course of neoadjuvant therapy. The reduction in BPE was significantly correlated to the share of responding patients with a complete or partial response (CR and PR). This presents a reduction of at least one class of BPE after the middle step MRI was 79.6% and became substantially unchanged even in the post final step MRI (79.2%). Among non-responding patients or patients with stable/progressing disease (SD, PD), only 20.2% after the middle step and 17.7% after the final step showed a reduction of at least one class of BPE. BPE decreased during neoadjuvant therapy in 4/5 responding patients and in 1/5 non-responders. This is an important aspect in our study because, if confirmed in larger cohorts of patients with quantitative evaluations, BPE could be confirmed as a marker of predictive response to NAC, thus allowing for an early detection of responders in a therapy continuation and sending non-responders straight to surgery. This may result in the optimization of the therapeutic path, as well as significant economic savings for the healthcare system. The standardization of automatic detection methods and quantification of BPE through specific features could improve the results shortly, starting from the correlation with molecular subtypes, as it happens in CESM [
40]; however, this correlation is also possible with qualitative observational methods [
41]
BPE reduction is significantly related to the administration of taxanes or anthracyclines in the first round of NAC compared to anti-HER2+combined therapies, which is consistent with reports from other authors [
31]. This aspect could be related to the combination of the anti-angiogenetic drug with common chemotherapeutic agents that, in addition to improving the tumor’s response during chemotherapy, could operate through the normalization of the tumor vascular function while it converts non-functional vessels into functional ones. This would allow for more chemotherapeutic agents to reach the tumor [
30]. This would also explain the lower BPE reduction related to the preserved tissue perfusion and the consequent higher percentage of pCR (18.8%) in HER2+ tumors compared to tumors observed in the study.
The relatively low sample size in the various categories represents our study limitation, even though it is in line with other published works [
26,
42]
A second limit may be the retrospective nature of the study. From having analyzed only two MRI steps in a significant proportion of the sample, this limit could eventually be considered apparent since the most significant changes in BPE occurred in the first treatment phase, as reported in the literature [
22,
23,
24,
30]. Our study supported this consideration by highlighting the BPE class’s confirmation between the intermediate and final step, showing a significant concordance in the results.
Throughout the study, the concordance among the operators was high (p-values k kappa of Cohen test <0.05), which could result from common training and years of experience in breast imaging, specifically. This correlation could probably be reduced if operators carried out assessments with different training and years of seniority. This may be the subject of evaluation in future work.