Precision Medicine in Aortic Anastomosis: A Numerical and Experimental Study of a Novel Double-Sided Needle
Abstract
1. Introduction
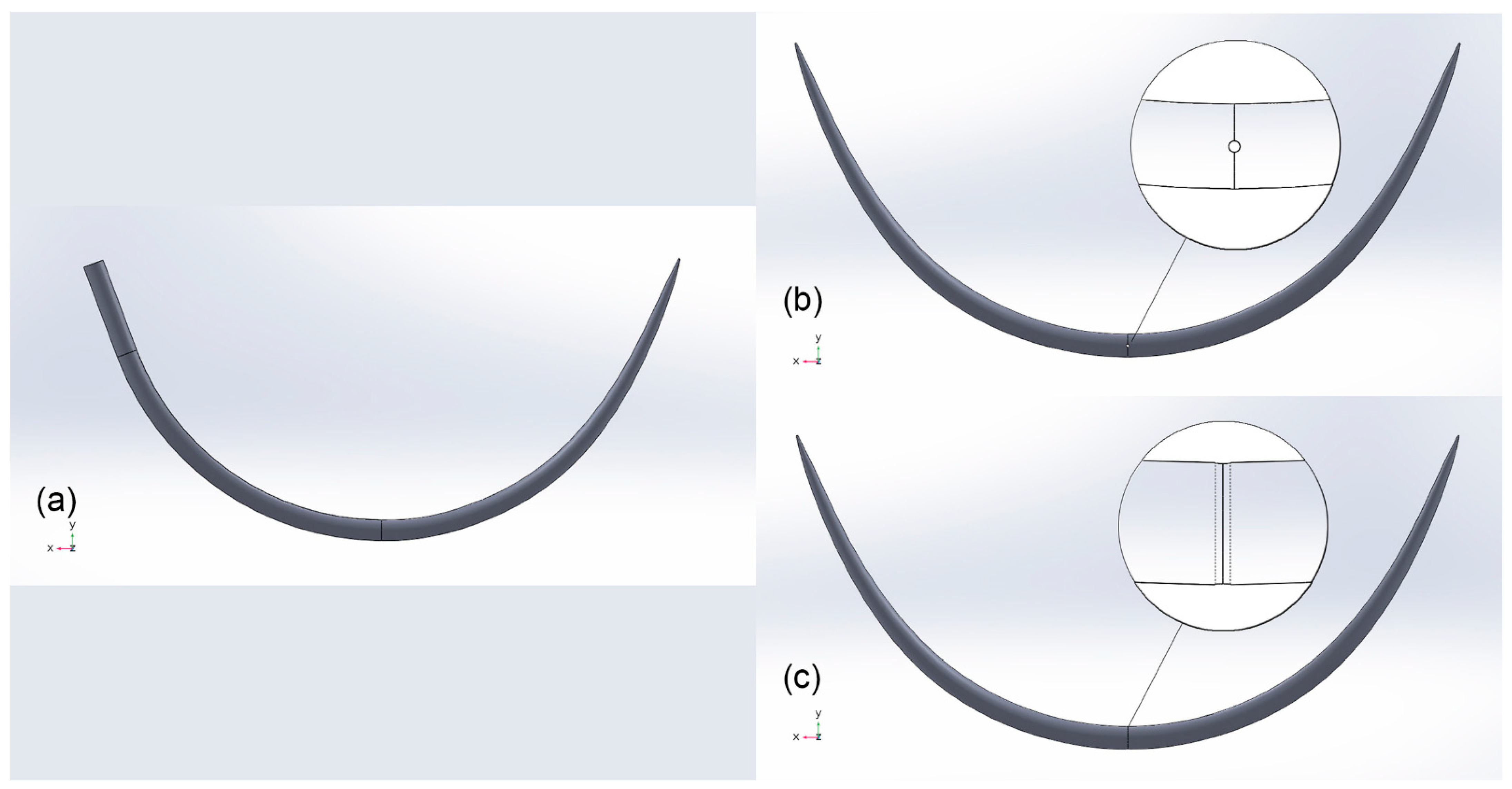
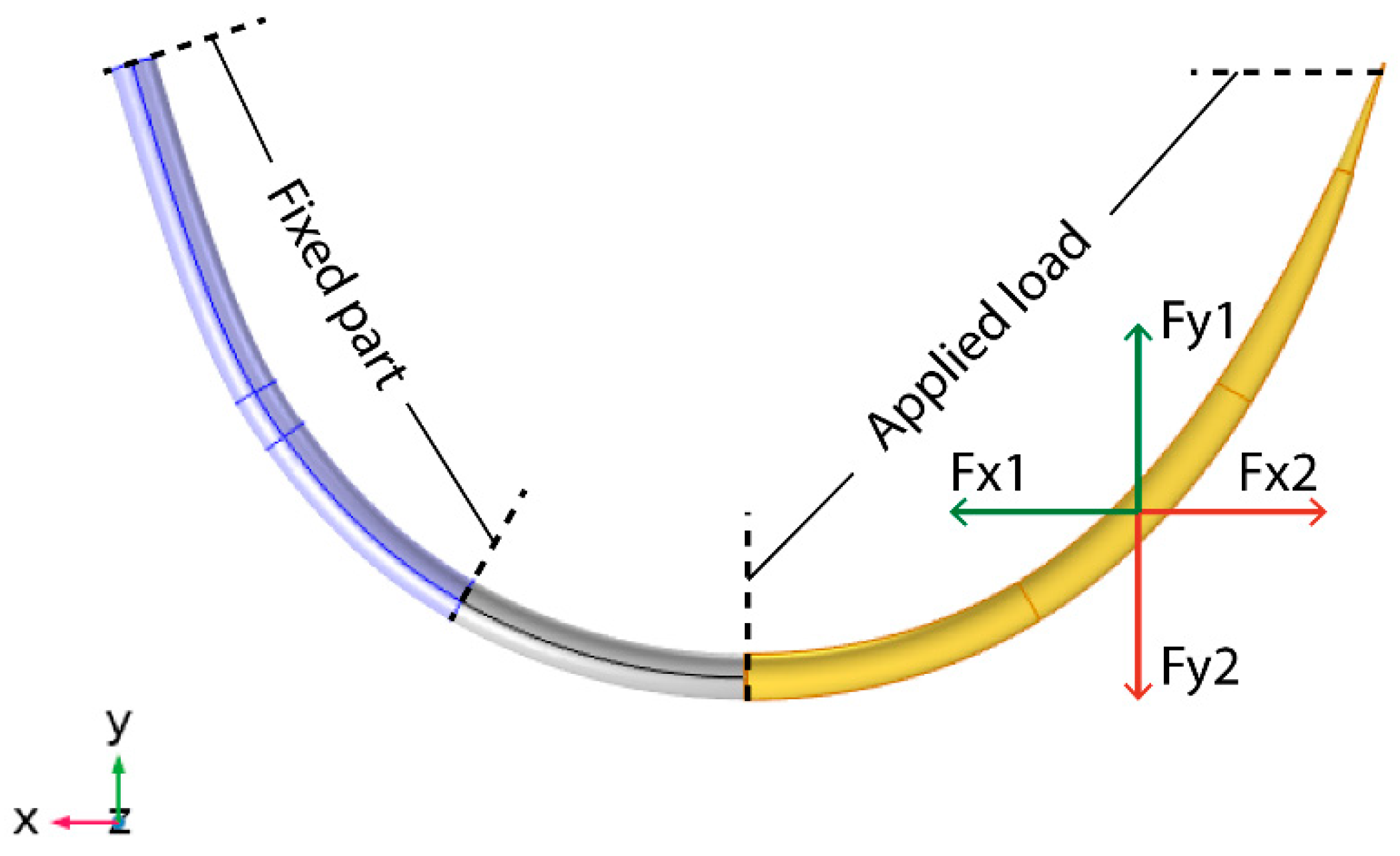
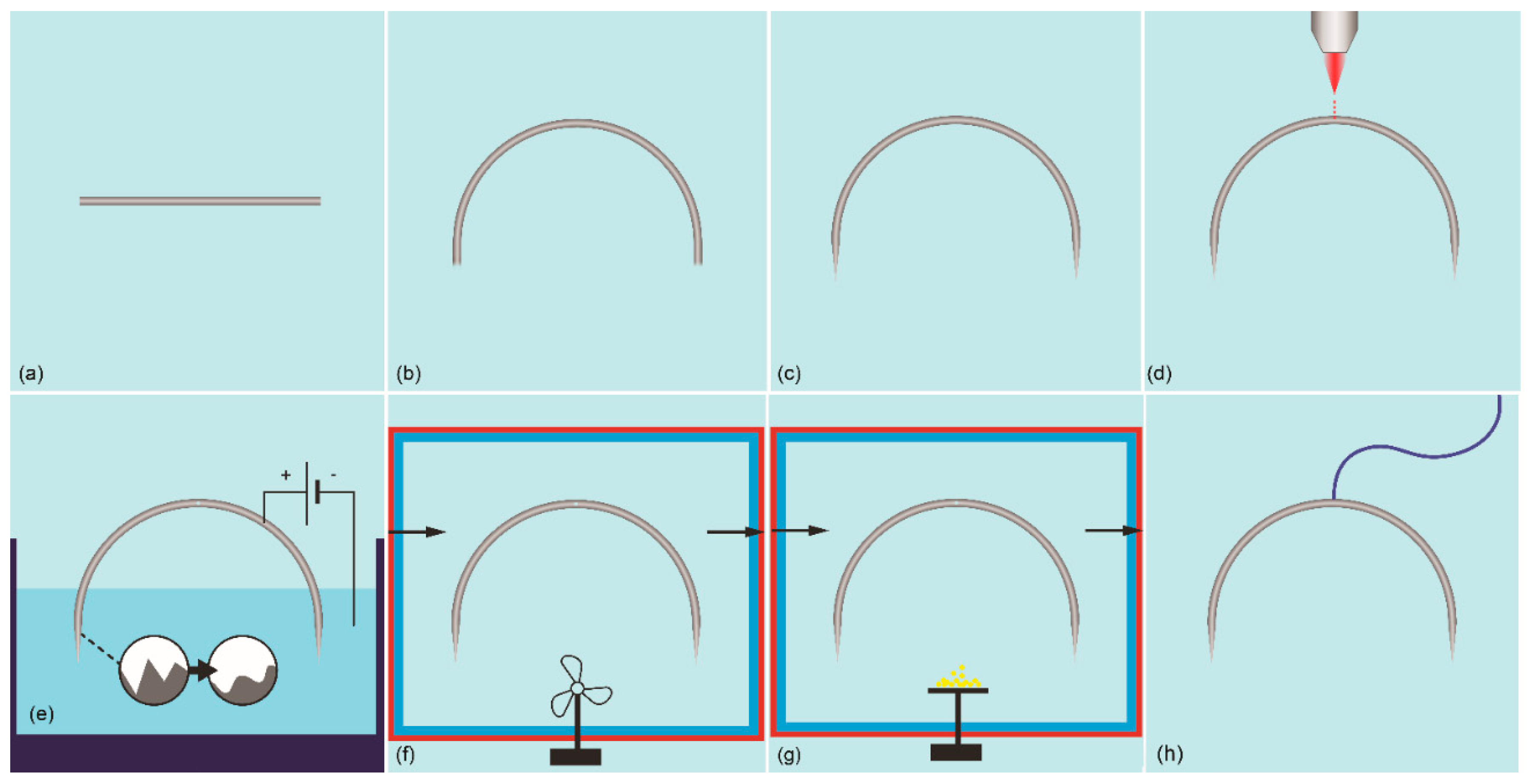
2. Materials and Methods
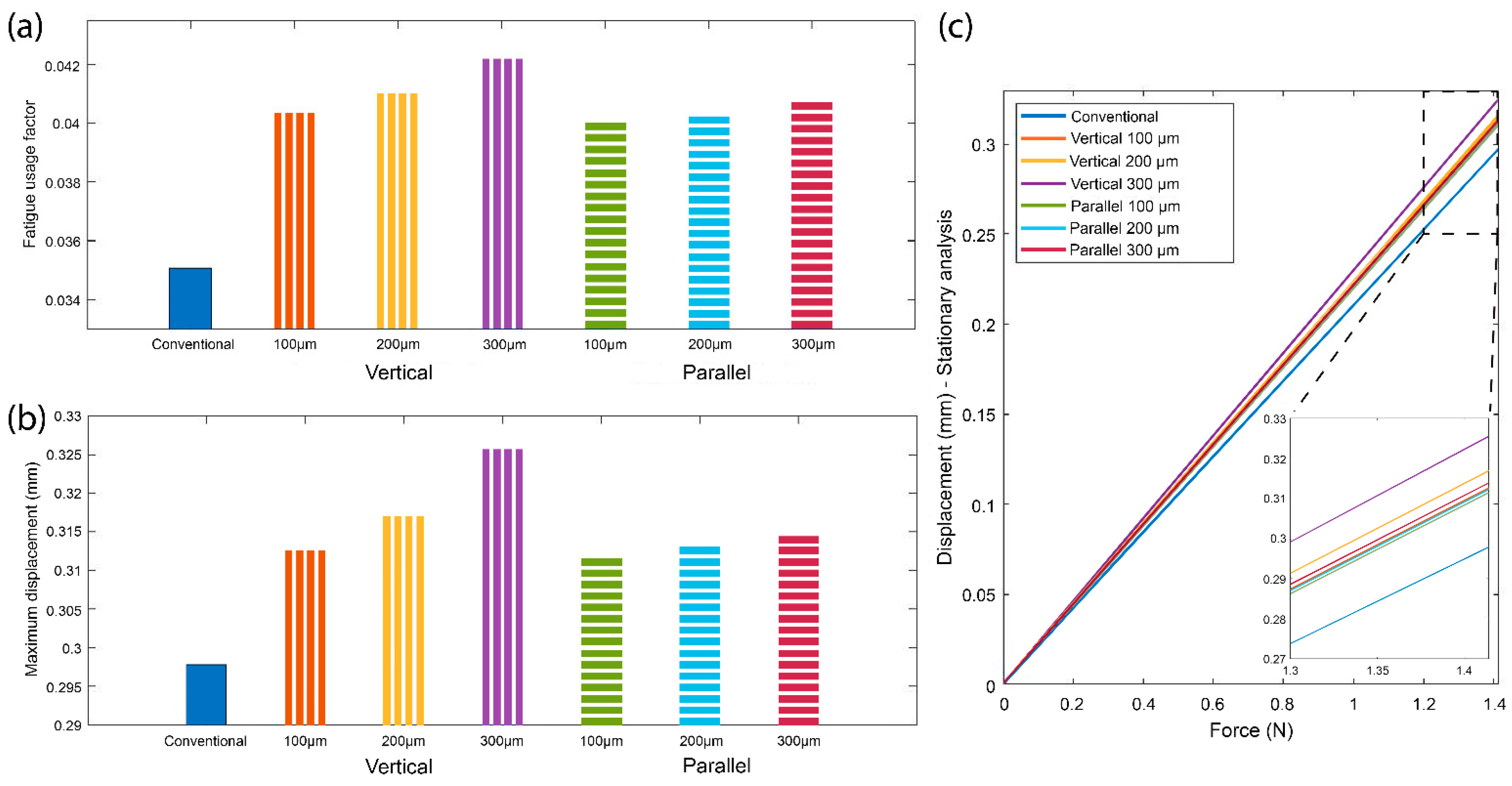
3. Results
3.1. Needle Fatigue Factor Estimation
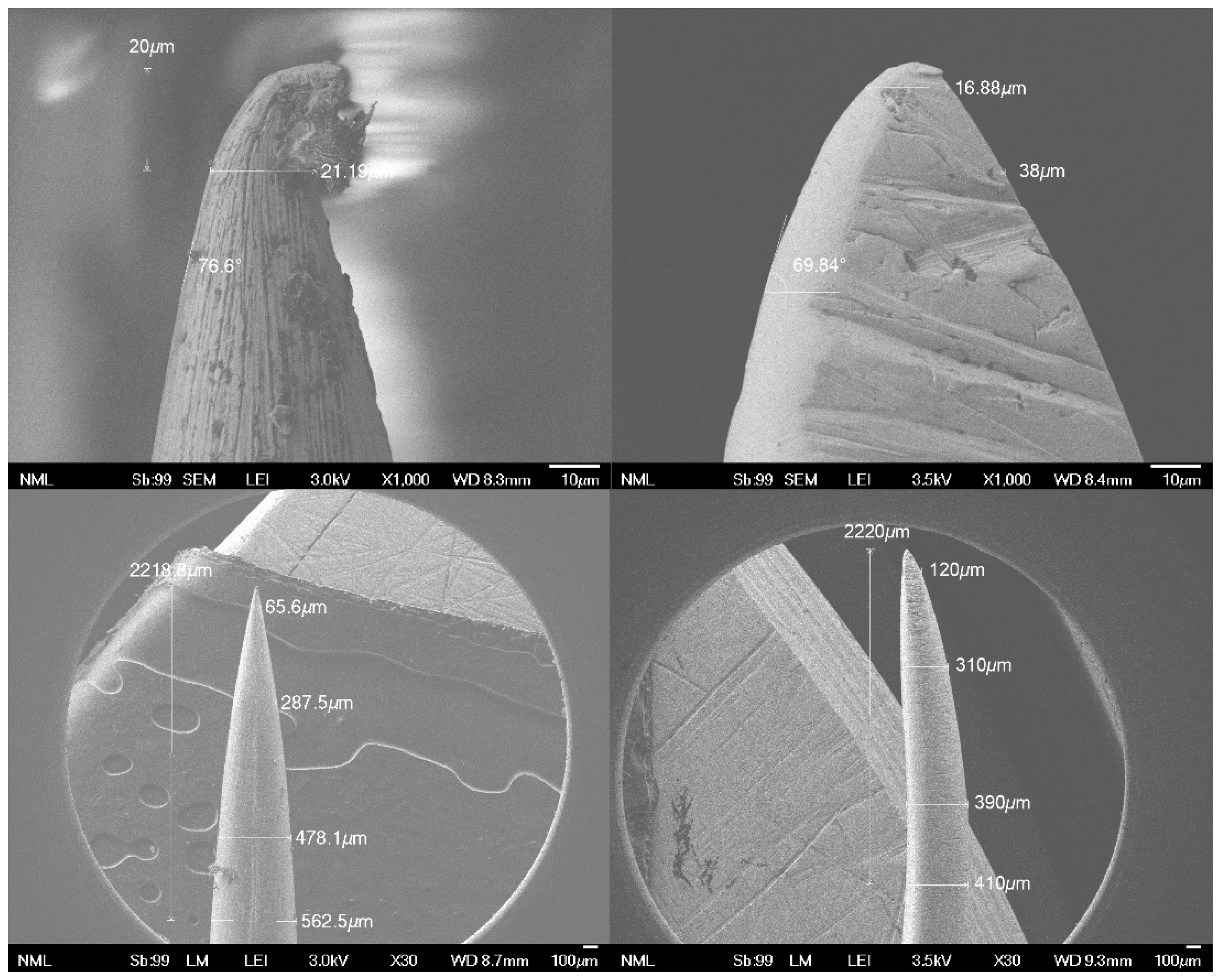
3.2. Ease of Penetration into the Tissue and Tip Sharpness
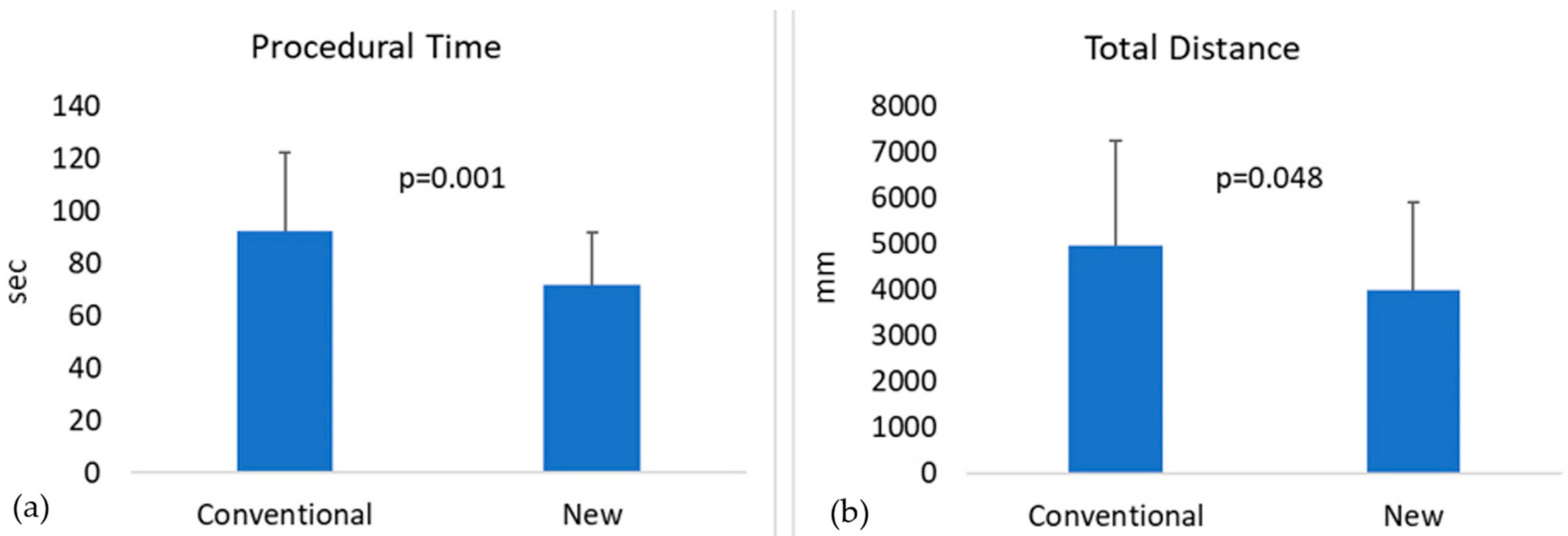
3.3. Prototype Testing
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Bossone, E.; Eagle, K.A. Epidemiology and management of aortic disease: Aortic aneurysms and acute aortic syndromes. Nat. Rev. Cardiol. 2021, 18, 331–348. [Google Scholar] [CrossRef]
- Wanhainen, A.; Verzini, F.; Herzeele, I.; van Allaire, E.; Bown, M.; Cohnert, T.; Dick, F.; Herwaarden, J.; van Karkos, C.; Koelemay, M.; et al. Editor’s Choice—European Society for Vascular Surgery (ESVS) 2019 Clinical Practice Guidelines on the Management of Abdominal Aorto-iliac Artery Aneurysms. Eur. J. Vasc. Endovasc. Surg. 2019, 57, 8–93. [Google Scholar] [CrossRef] [PubMed]
- Chaikof, E.L.; Dalman, R.L.; Eskandari, M.K.; Jackson, B.M.; Lee, W.A.; Mansour, M.A.; Mastracci, T.M.; Mell, M.; Murad, M.H.; Nguyen, L.L.; et al. The Society for Vascular Surgery practice guidelines on the care of patients with an abdominal aortic aneurysm. J. Vasc. Surg. 2018, 67, 2–77.e2. [Google Scholar] [CrossRef]
- Swerdlow, N.J.; Wu, W.W.; Schermerhorn, M.L. Open and endovascular management of aortic aneurysms. Circ. Res. 2019, 124, 647–661. [Google Scholar] [CrossRef] [PubMed]
- Suckow, B.; Goodney, P.; Columbo, J.; Kang, R.; Stone, D.; Sedrakyan, A.; Cronenwett, J.; Fillinger, M. National Trends in Open Surgical, Endovascular and Branched/ Fenestrated Endovascular Aortic Aneurysm Repair in Medicare Patients. Physiol. Behav. 2016, 176, 100–106. [Google Scholar] [CrossRef] [PubMed]
- Savlania Alexis Carrel: Father of Vascular Anastomosis and Organ Transplantation. Indian J. Vasc. Endovasc. Surg. 2017, 4, 115. [CrossRef]
- Sergeant, P.; Kocharian, R.; Patel, B.; Pfefferkorn, M.; Matonick, J. Needle-to-suture ratio, as well as suture material, impacts needle-hole bleeding in vascular anastomoses. Interact. Cardiovasc. Thorac. Surg. 2016, 22, 813–816. [Google Scholar] [CrossRef]
- Mitchell, J.H.; Dougherty, K.G.; Strickman, N.E.; Mortazavi, A.; Krajcer, Z. Endovascular repair of paraanastomotic aneurysms after aortic reconstruction. Tex. Heart Inst. J. 2007, 34, 148–153. [Google Scholar]
- Safi, H.J.; Winnerkvist, A.; Miller, C.C.; Iliopoulos, D.C.; Reardon, M.J.; Espada, R.; Baldwin, J.C. Effect of extended cross-clamp time during thoracoabdominal aortic aneurysm repair. Ann. Thorac. Surg. 1998, 66, 1204–1208. [Google Scholar] [CrossRef]
- Georgakis, P.; Paraskevas, K.I.; Bessias, N.; Mikhailidis, D.P.; Andrikopoulos, V. Duration of aortic cross-clamping during elective open abdominal aortic aneurysm repair operations and postoperative cardiac/renal function. Int. Angiol. 2010, 29, 244–248. [Google Scholar]
- Khir, A.W.; Henein, M.Y.; Koh, T.; Das, S.K.; Parker, K.H.; Gibson, D.G. Arterial waves in humans during peripheral vascular surgery. Clin. Sci. 2001, 101, 749–757. [Google Scholar] [CrossRef]
- Al-Sarraf, N.; Thalib, L.; Hughes, A.; Houlihan, M.; Tolan, M.; Young, V.; McGovern, E. Cross-clamp time is an independent predictor of mortality and morbidity in low- and high-risk cardiac patients. Int. J. Surg. 2011, 9, 104–109. [Google Scholar] [CrossRef] [PubMed]
- El-Sabrout, R.A.; Reul, G.J. Suprarenal or supraceliac aortic clamping during repair of infrarenal abdominal aortic aneurysms. Tex. Heart Inst. J. 2001, 28, 254–264. [Google Scholar] [PubMed]
- Manolesou, D.; Papaioannou, T.G.; Georgiopoulos, G.; Schizas, D.; Lazaris, A.; Stamatelopoulos, K.; Dimakakos, E.; Stergiopulos, N.; Stefanadis, C.; Liakakos, T.; et al. A systematic review and meta-analysis of the efficacy of aortic anastomotic devices. J. Vasc. Surg. 2019, 69, 598–613.e7. [Google Scholar] [CrossRef] [PubMed]
- Manolesou, D.G.; Georgiopoulos, G.; Lazaris, A.M.; Schizas, D.; Stamatelopoulos, K.S.; Khir, A.W.; Liakakos, T.; Papaioannou, T.G. Experimental Devices Versus Hand-Sewn Anastomosis of the Aorta: A Systematic Review and Meta-Analysis. J. Surg. Res. 2021, 258, 200–212. [Google Scholar] [CrossRef]
- Ho, C.; Juyoung, C.; Myung, B.; Cha, K.; Ik, S. Internal Fixation Method Using EZ-Tcon for Transconjunctival Fat Repositioning: Clinical Outcomes and Efficacy. Aesthet. Plast. Surg. 2020, 44, 1–12. [Google Scholar] [CrossRef]
- Cheol Ho, C.; Myung Kyu, C. New Internal Fixation Technique for Transconjunctival Fat Repositioning. Plast. Reconstractive Surg. Glob. Open 2017, 5, e1502. [Google Scholar] [CrossRef]
- Tiryaki, K.T.; Aksungur, E. Micro-Shuttle Lifting of the Neck: A Percutaneous Loop Suspension Method Using a Novel Double-Ended Needle. Aesthet. Surg. J. 2016, 36, 629–638. [Google Scholar] [CrossRef]
- Tiryaki, K.T. Shuttle Lifting of the Nose: A Minimally Invasive Approach for Nose Reshaping. Aesthet. Surg. J. 2010, 30, 176–185. [Google Scholar] [CrossRef]
- Fuente-del-Campo, A.; Lucchesi, R.; del Pilar Cedillo Ley, M. Bidirectional Armed Needle: A Useful Surgical Tool in Plastic Surgery. Plast. Reconstr. Surg. 1997, 100, 695–698. [Google Scholar] [CrossRef]
- Ng, E.; Ng, Y.; Gupta, R.; Lim, F.; Mah, E. Repair of acute Achilles tendon rupture using a double-ended needle. J. Orthop. Surg. 2006, 14, 142–146. [Google Scholar] [CrossRef]
- Lasheen, A.; Safwat, K.; Fiad, A.; Elmoregy, A.; Hamed, A.W. Port-Site Closure Using a Modified Aptos Needle. J. Soc. Laparosc. Surg. 2013, 312–315. [Google Scholar] [CrossRef][Green Version]
- Yanai, A.; Fukuda, O.; Hirabayashi, S. Double-tipped Center-Threading Suture Needle for Subcuticular Suturing. Plast. Reconstr. Surg. 1986, 78, 411–413. [Google Scholar] [CrossRef] [PubMed]
- Findley, W.N. A Theory for the Effect of Mean Stress on Fatigue of Metals Under Combined Torsion and Axial Load or Bending. J. Eng. Ind. 1959, 81, 301–305. [Google Scholar] [CrossRef]
- McJames, W.; Willis, B.; Smith, D.; Reynolds, E.; Gucker, C.; Nordmeyer, M. Process for Manufacturing Surgical Needles. U.S. Patent 5776268, 7 July 1998. [Google Scholar]
- Daniel, S.; Willis, B.; Marschke, K.; Littlewood, B.; Schoen, V.; Gucker, C.; Nordmeyer, M.; Miklewicz, T. Process for Manufacturing Taper Point Surgical Needles. U.S. Patent 5539973, 7 June 1996. [Google Scholar]
- Lochyński, P.; Charazińska, S.; Łyczkowska-Widłak, E.; Sikora, A. Electropolishing of stainless steel in laboratory and industrial scale. Metals 2019, 9, 854. [Google Scholar] [CrossRef]
- Raaz, U.; Zöllner, A.M.; Schellinger, I.N.; Toh, R.; Nakagami, F.; Brandt, M.; Emrich, F.C.; Kayama, Y.; Eken, S.; Adam, M.; et al. Segmental aortic stiffening contributes to experimental abdominal aortic aneurysm development. Circulation 2015, 131, 1783–1795. [Google Scholar] [CrossRef] [PubMed]
- Chowienczyk, P.J. Aortic stiffness and disease location is key. Circulation 2015, 131, 1745–1757. [Google Scholar] [CrossRef]
- Zinn, A.A. Chemical Vapor Deposition of Tungsten. In The Chemistry of Metal CVD; Kodas, T., Hampden-Smith, M., Eds.; VCH Verlagsgesellschaft: Weinheim, Germany, 1994. [Google Scholar]
- Lai, K.K.; Lamb, H.H. Tungsten chemical vapor deposition using tungsten hexacarbonyl: Microstructure of as-deposited and annealed films. Thin Solid Films 2000, 370, 114–121. [Google Scholar] [CrossRef]
- Davazoglou, D.; Pallis, G.; Psycharis, V.; Gioti, M.; Logothetidis, S. Structure and optical properties of tungsten thin films deposited by pyrolysis of W(CO)6 at various temperatures. J. Appl. Phys. 1998, 77, 6070. [Google Scholar] [CrossRef]
- Yi, N.; Bao, S.; Zhou, H.; Xin, Y.; Huang, A.; Ma, Y.; Li, R.; Jin, P. Preparation of microstructure-controllable superhydrophobic polytetrafluoroethylene porous thin film by vacuum thermal-evaporation. Front. Mater. Sci. 2016, 10, 320–327. [Google Scholar] [CrossRef]
- Feng, Y.; Uchidiuno, U.A.; Zahiri, H.R.; George, I.; Park, A.E.; Mentis, H. Comparison of Kinect and Leap Motion for Intraoperative Image Interaction. Surg. Innov. 2021, 28, 33–40. [Google Scholar] [CrossRef]
- Louie, O.; Larson, L.W. Surgical Techniques and Tools. In Surgical Implantation of Cardiac Rhythm Devices; Poole, J., Larson, L.W., Eds.; Elsevier Inc.: Amsterdam, The Netherlands, 2018; pp. 59–80. ISBN 9780323429252. [Google Scholar]
- Pande, R.L.; Beckman, J.A. Pathophysiology, Epidemiology, and Prognosis of Aortic Aneurysms, 2nd ed.; Elsevier Inc.: Amsterdam, The Netherlands, 2013; ISBN 9781437729306. [Google Scholar]
- Moll, F.L.; Powell, J.T.; Fraedrich, G.; Verzini, F.; Haulon, S.; Waltham, M.; Van Herwaarden, J.A.; Holt, P.J.E.; Van Keulen, J.W.; Rantner, B.; et al. Management of abdominal aortic aneurysms clinical practice guidelines of the European society for vascular surgery. Eur. J. Vasc. Endovasc. Surg. 2011, 41, S1–S58. [Google Scholar] [CrossRef]
- Garitey, V.; Rieu, R.; Alimi, Y. Anastomoses prothéto-prothétiques et aorto-prothétiques par stents, fils de suture, clips et agrafes—EM consulte. J. Mal. Vasc. 2003, 28, 173–177. [Google Scholar] [PubMed]
- Tamura, N.; Komiya, T.; Sakaguchi, G.; Kobayashi, T. “Turn-up” anastomotic technique for acute aortic dissection. Eur. J. Cardio-thorac. Surg. 2007, 31, 548–549. [Google Scholar] [CrossRef]
- Saxena, P.; Greason, K.L. Graft intussusception technique of vascular anastomosis. Ann. Thorac. Surg. 2014, 98, 1127–1128. [Google Scholar] [CrossRef] [PubMed]
- Rylski, B.; Siepe, M.; Blanke, P.; Euringer, W.; Schoellhorn, J.; Beyersdorf, F. Adventitial inversion with graft telescopic insertion for distal anastomosis in acute type a aortic dissection. Ann. Thorac. Cardiovasc. Surg. 2012, 18, 278–280. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Rylski, B.; Siepe, M.; Schoellhorn, J.; Beyersdorf, F. An improved technique for aortic anastomosis: Graft telescopic inversion. J. Thorac. Cardiovasc. Surg. 2010, 140, 934–935. [Google Scholar] [CrossRef] [PubMed][Green Version]



| Load Case | Force Fx (N) | Force Fy (N) |
|---|---|---|
| Load Case 1 | 0:0.1:1 | 0:0.1:1 |
| Load Case 2 | 0:−0.1:−1 | 0:−0.1:−1 |
| Material Parameter | Stainless Steel 308L Value |
|---|---|
| Poisson’s Ratio | 0.30 |
| Density | 8 g/cm3 |
| Young’s Modulus | 200 GPa |
| Normal Stress Sensitivity Coefficient k | 0.23 |
| Limit Factor f | 579 MPa |
| Time | Distance | ||
|---|---|---|---|
| New | Conventional | New | Conventional |
| 126.0 | 79.8 | 6501.7 | 1532.6 |
| 122.4 | 91.2 | 6108.9 | 5302.4 |
| 84.6 | 81.0 | 7277.7 | 6734.8 |
| 75.0 | 70.8 | 3181.4 | 4874.2 |
| 120.0 | 84.0 | 7374.2 | 4847.5 |
| 91.8 | 86.4 | 3790.8 | 2820.9 |
| 74.4 | 64.2 | 3563.4 | 3315.7 |
| 135.0 | 80.4 | 5165.1 | 1389.8 |
| 82.8 | 69.6 | 3613.1 | 3484.3 |
| 63.0 | 28.8 | 2624.1 | 2339.2 |
| 127.8 | 88.2 | 8583.7 | 6115.7 |
| 88.2 | 84.0 | 7833.3 | 7486.4 |
| 64.8 | 64.8 | 1858.3 | 3295.0 |
| 32.4 | 28.8 | 2206.0 | 2353.6 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Manolesou, D.G.; Korompili, G.; Davazoglou, D.; Lazaris, A.M.; Schizas, D.; Sanoudou, D.; Liakakos, T.; Tsioufis, C.; Papaioannou, T.G. Precision Medicine in Aortic Anastomosis: A Numerical and Experimental Study of a Novel Double-Sided Needle. J. Pers. Med. 2021, 11, 1385. https://doi.org/10.3390/jpm11121385
Manolesou DG, Korompili G, Davazoglou D, Lazaris AM, Schizas D, Sanoudou D, Liakakos T, Tsioufis C, Papaioannou TG. Precision Medicine in Aortic Anastomosis: A Numerical and Experimental Study of a Novel Double-Sided Needle. Journal of Personalized Medicine. 2021; 11(12):1385. https://doi.org/10.3390/jpm11121385
Chicago/Turabian StyleManolesou, Danae G., Georgia Korompili, Dimitris Davazoglou, Andreas M. Lazaris, Dimitrios Schizas, Despina Sanoudou, Theodore Liakakos, Constantinos Tsioufis, and Theodore G. Papaioannou. 2021. "Precision Medicine in Aortic Anastomosis: A Numerical and Experimental Study of a Novel Double-Sided Needle" Journal of Personalized Medicine 11, no. 12: 1385. https://doi.org/10.3390/jpm11121385
APA StyleManolesou, D. G., Korompili, G., Davazoglou, D., Lazaris, A. M., Schizas, D., Sanoudou, D., Liakakos, T., Tsioufis, C., & Papaioannou, T. G. (2021). Precision Medicine in Aortic Anastomosis: A Numerical and Experimental Study of a Novel Double-Sided Needle. Journal of Personalized Medicine, 11(12), 1385. https://doi.org/10.3390/jpm11121385








