Associations between Multimorbidity Patterns and Subsequent Labor Market Marginalization among Refugees and Swedish-Born Young Adults—A Nationwide Registered-Based Cohort Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Study Population
2.2. Data Sources
2.3. Exposure Assessment
2.4. Outcome Ascertainment
2.5. Covariates
2.6. Statistical Analysis
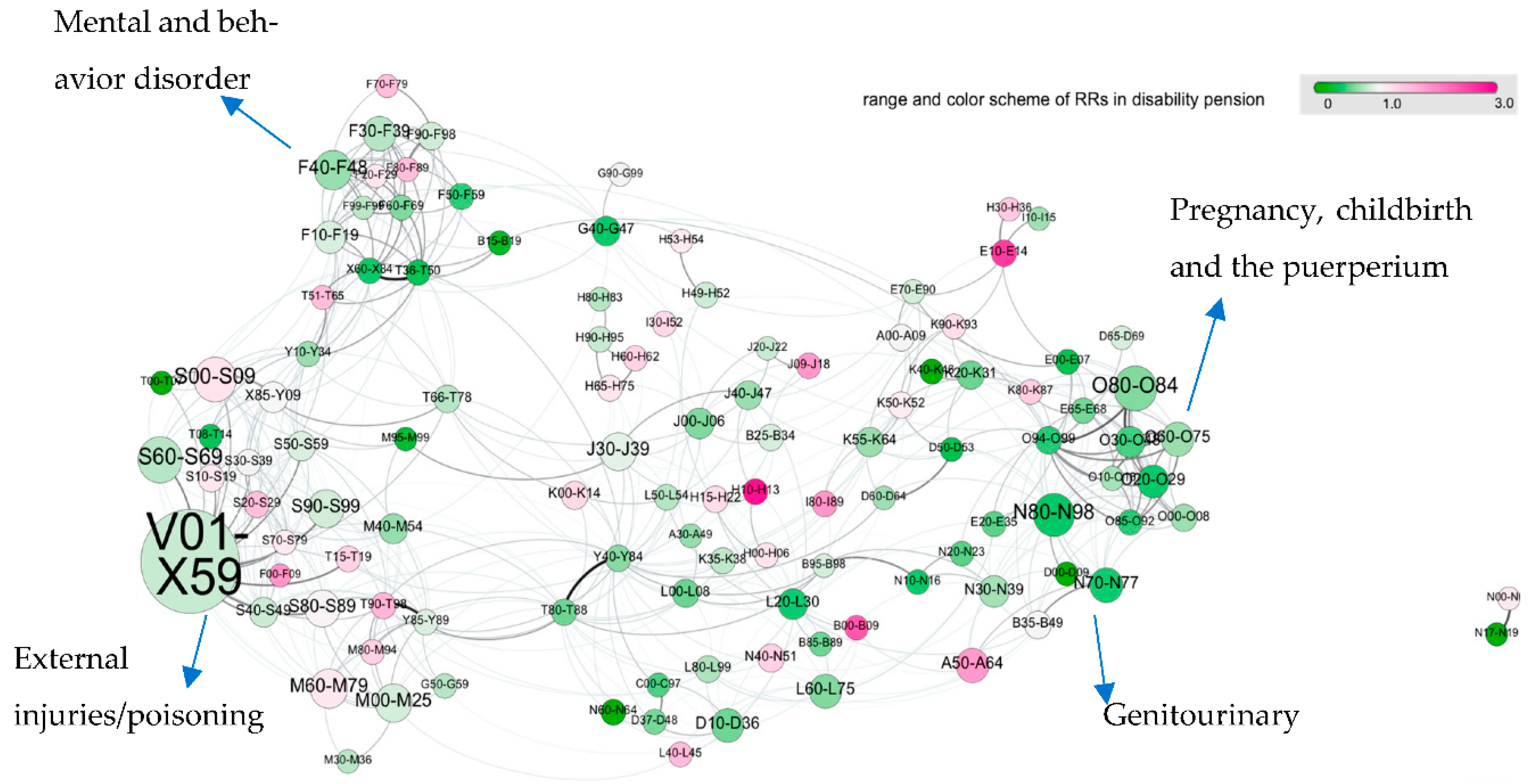
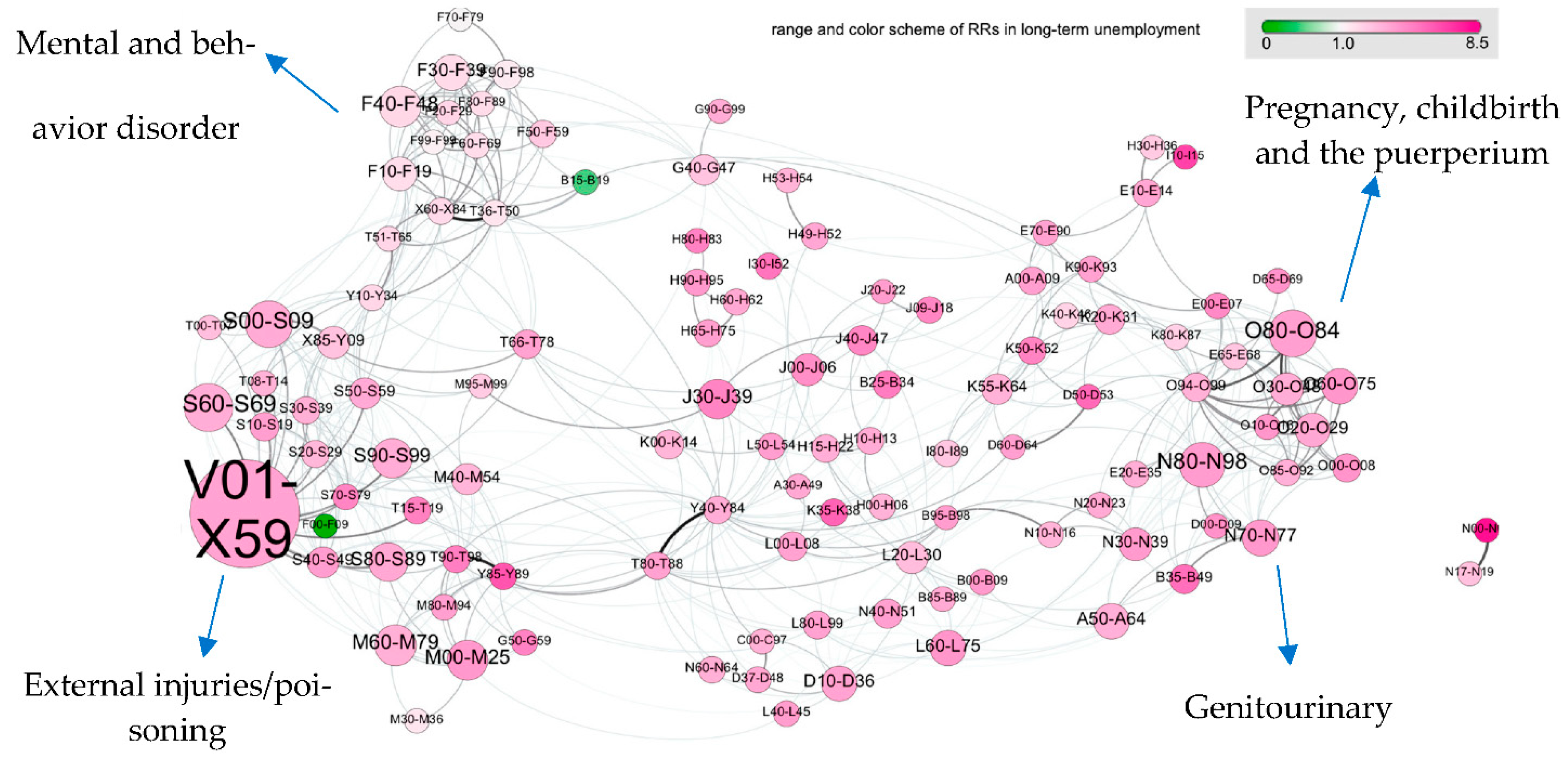
2.6.1. Multimorbidity Network
2.6.2. Logistic Regression
2.6.3. Relative Risks of Diagnostic Groups
3. Results
3.1. Baseline Characteristics
3.2. Multimorbidity Network
4. Discussion
Methodological Considerations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- United Nations High Commissioner for Refugees. Global Trends Forced Displacement in 2018; UNHCR: Geneva, Switzerland, 2018. [Google Scholar]
- Helgesson, M.; Wang, M.; Niederkrotenthaler, T.; Saboonchi, F.; Mittendorfer-Rutz, E. Labour market marginalisation among refugees from different countries of birth: A prospective cohort study on refugees to Sweden. J. Epidemiol. Community Health 2019, 73, 407–415. [Google Scholar] [CrossRef] [PubMed]
- Organisation for Economic Co-Operation and Development. OECD Employment Outlook 2019; OECD: Paris, France, 2019. [Google Scholar]
- Di Thiene, D.; Mittendorfer-Rutz, E.; Rahman, S.; Wang, M.; Alexanderson, K.; Tiihonen, J.; La Torre, G.; Helgesson, M. Trajectories of sickness absence, disability pension and unemployment in young immigrants with common mental disorders. Eur. J. Public Health 2019, 29, 1055–1062. [Google Scholar] [CrossRef] [Green Version]
- Di Thiene, D.; Helgesson, M.; Alexanderson, K.; La Torre, G.; Tiihonen, J.; Mittendorfer-Rutz, E. Risk of disability pension in first and second generation immigrants: The role of age and region of birth in a prospective population-based study from Sweden. BMC Public Health 2017, 17, 931. [Google Scholar] [CrossRef] [Green Version]
- Bernitz, B.K.; Grees, N.; Randers, M.J.; Gerner, U.; Bergendorff, S. Young adults on disability benefits in 7 countries. Scand. J. Public Health 2013, 41, 3–26. [Google Scholar] [CrossRef]
- Organisation for Economic Co-Operation and Development. Finding the Way: A Discussion of the Swedish Migrant Integration System; OECD Publishing: Paris, France, 2014. [Google Scholar]
- Schwandt, H.; Wachter, T.V. Unlucky Cohorts: Estimating the Long-Term Effects of Entering the Labor Market in a Recession in Large Cross-Sectional Data Sets. J. Labor Econ. 2019, 37, S161–S198. [Google Scholar] [CrossRef] [Green Version]
- Helgesson, M.; Tinghög, P.; Niederkrotenthaler, T.; Saboonchi, F.; Mittendorfer-Rutz, E. Labour-market marginalisation after mental disorders among young natives and immigrants living in Sweden. BMC Public Health 2017, 17, 593. [Google Scholar] [CrossRef] [PubMed]
- Çelikaksoy, A.; Wadensjö, E. Refugee Youth Who Arrived in Sweden as Unaccompanied Minors and Separated Children: Education and Labour Market Well-being. Nord. J. Migr. Res. 2019, 9, 179–200. [Google Scholar] [CrossRef] [Green Version]
- Fazel, M.; Reed, R.V.; Panter-Brick, C.; Stein, A. Mental health of displaced and refugee children resettled in high-income countries: Risk and protective factors. Lancet 2012, 379, 266–282. [Google Scholar] [CrossRef]
- Slopen, N.; Koenen, K.C.; Kubzansky, L.D. Childhood adversity and immune and inflammatory biomarkers associated with cardiovascular risk in youth: A systematic review. Brain Behav. Immun. 2012, 26, 239–250. [Google Scholar] [CrossRef]
- Ervasti, J.; Virtanen, M.; Pentti, J.; Lallukka, T.; Tinghög, P.; Kjeldgard, L.; Mittendorfer-Rutz, E.; Alexanderson, K. Work Disability Before and After Diabetes Diagnosis: A Nationwide Population-Based Register Study in Sweden. Am. J. Public Health 2015, 105, e22–e29. [Google Scholar] [CrossRef] [PubMed]
- Graff, H.J.; Siersma, V.; Møller, A.; Kragstrup, J.; Andersen, L.L.; Egerod, I.; Malá Rytter, H. Labour market attachment after mild traumatic brain injury: Nationwide cohort study with 5-year register follow-up in Denmark. BMJ Open 2019, 9, e026104. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dorner, T.E.; Alexanderson, K.; Svedberg, P.; Ropponen, A.; Stein, K.V.; Mittendorfer-Rutz, E. Sickness absence due to back pain or depressive episode and the risk of all-cause and diagnosis-specific disability pension: A Swedish cohort study of 4,823,069 individuals. Eur. J. Pain 2015, 19, 1308–1320. [Google Scholar] [CrossRef]
- Virtanen, M.; Lallukka, T.; Kivimäki, M.; Alexanderson, K.; Ervasti, J.; Mittendorfer-Rutz, E. Neurodevelopmental disorders among young adults and the risk of sickness absence and disability pension: A nationwide register linkage study. Scandinavian J. Work. Environ. Health 2020, 46, 410–416. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mittendorfer-Rutz, E.; Ivert, T.; Vaez, M.; Dorner, T.E. Synergistic effect between ischaemic heart disease and common mental disorders and the risk of premature exit from the labour market: A nationwide register based study from Sweden. Eur. Heart J. 2018, 39, 578–585. [Google Scholar] [CrossRef] [PubMed]
- Hidalgo, C.A.; Blumm, N.; Barabási, A.-L.; Christakis, N.A. A Dynamic Network Approach for the Study of Human Phenotypes. PLoS Comput. Biol. 2009, 5, e1000353. [Google Scholar] [CrossRef]
- Rzhetsky, A.; Wajngurt, D.; Park, N.; Zheng, T. Probing genetic overlap among complex human phenotypes. Proc. Natl. Acad. Sci. USA 2007, 104, 11694–11699. [Google Scholar] [CrossRef] [Green Version]
- Chmiel, A.; Klimek, P.; Thurner, S. Spreading of diseases through comorbidity networks across life and gender. New J. Phys. 2014, 16. [Google Scholar] [CrossRef]
- Barnett, K.; Mercer, S.W.; Norbury, M.; Watt, G.; Wyke, S.; Guthrie, B. Epidemiology of multimorbidity and implications for health care, research, and medical education: A cross-sectional study. Lancet 2012, 380, 37–43. [Google Scholar] [CrossRef] [Green Version]
- Barabási, A.-L.; Gulbahce, N.; Loscalzo, J. Network medicine: A network-based approach to human disease. Nat. Rev. Genet. 2011, 12, 56–68. [Google Scholar] [CrossRef] [Green Version]
- Loscalzo, J.; Barabási, A.-L.; Silverman, E.K. Network Medicine; Harvard Univeristy Press: Harvard, MA, USA, 2017. [Google Scholar]
- Fortunato, S. Community detection in graphs. Phys. Rep. 2010, 486, 75–174. [Google Scholar] [CrossRef] [Green Version]
- Fotouhi, B.; Momeni, N.; Riolo, M.A.; Buckeridge, D.L. Statistical methods for constructing disease comorbidity networks from longitudinal inpatient data. Appl. Netw. Sci. 2018, 3, 1–34. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Serrano, M.A.; Boguna, M.; Vespignani, A. Extracting the multiscale backbone of complex weighted networks. Proc. Natl. Acad. Sci. USA 2009, 106, 6483–6488. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dikeos, D.; Georgantopoulos, G. Medical comorbidity of sleep disorders. Curr. Opin. Psychiatry 2011, 24, 346–354. [Google Scholar] [CrossRef] [PubMed]
- Ranasinghe, I.; Wang, Y.; Dharmarajan, K.; Hsieh, A.F.; Bernheim, S.M.; Krumholz, H.M. Readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia among young and middle-aged adults: A retrospective observational cohort study. PLoS Med. 2014, 11, e1001737. [Google Scholar] [CrossRef] [Green Version]
- McGregor, M.J.; Reid, R.J.; Schulzer, M.; Fitzgerald, J.M.; Levy, A.R.; Cox, M.B. Socioeconomic status and hospital utilization among younger adult pneumonia admissions at a Canadian hospital. BMC Health Serv. Res. 2006, 6, 152. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Metersky, M.L.; Masterton, R.G.; Lode, H.; File, T.M., Jr.; Babinchak, T. Epidemiology, microbiology, and treatment considerations for bacterial pneumonia complicating influenza. Int. J. Infect. Dis. 2012, 16, e321. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Collaborators, G.B.D.I. Mortality, morbidity, and hospitalisations due to influenza lower respiratory tract infections, 2017: An analysis for the Global Burden of Disease Study 2017. Lancet Respir. Med. 2019, 7, 69–89. [Google Scholar] [CrossRef] [Green Version]
- Girard, T.D.; Self, W.H.; Edwards, K.M.; Grijalva, C.G.; Zhu, Y.; Williams, D.J.; Jain, S.; Jackson, J.C. Long-Term Cognitive Impairment after Hospitalization for Community-Acquired Pneumonia: A Prospective Cohort Study. J. Gen. Intern. Med. 2018, 33, 929–935. [Google Scholar] [CrossRef] [Green Version]
- Castelli, F.; Sulis, G. Migration and infectious diseases. Clin. Microbiol. Infect. 2017, 23, 283–289. [Google Scholar] [CrossRef]
- Pavli, A.; Maltezou, H. Health problems of newly arrived migrants and refugees in Europe. J. Travel Med. 2017, 24. [Google Scholar] [CrossRef]
- Frølich, A.; Ghith, N.; Schiøtz, M.; Jacobsen, R.; Stockmarr, A. Multimorbidity, healthcare utilization and socioeconomic status: A register-based study in Denmark. PLoS ONE 2019, 14, e0214183. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Volandes, A.E.; Paasche-Orlow, M.K. Health Literacy, Health Inequality and a Just Healthcare System. Am. J. Bioeth. 2007, 7, 5–10. [Google Scholar] [CrossRef] [PubMed]
- Byrow, Y.; Pajak, R.; Specker, P.; Nickerson, A. Perceptions of mental health and perceived barriers to mental health help-seeking amongst refugees: A systematic review. Clin. Psychol. Rev. 2020, 75, 101812. [Google Scholar] [CrossRef]
- Maldari, T.; Elsley, N.; Abdul Rahim, R. The health status of newly arrived Syrian refugees at the Refugee Health Service, South Australia, 2016. Aust. J. Gen. Pract. 2019, 48, 480–486. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Österberg, T.; Gustafsson, B. Disability pension among immigrants in Sweden. Soc. Sci. Med. 2006, 863, 805–816. [Google Scholar] [CrossRef]
- Johnston, M.C.; Black, C.; Mercer, S.W.; Prescott, G.J.; Crilly, M.A. Impact of educational attainment on the association between social class at birth and multimorbidity in middle age in the Aberdeen Children of the 1950s cohort study. BMJ Open 2019, 9, e024048. [Google Scholar] [CrossRef]
- Manhica, H.; Berg, L.; Almquist, Y.B.; Rostila, M.; Hjern, A. Labour market participation among young refugees in Sweden and the potential of education: A national cohort study. J. Youth Stud. 2018, 22, 533–550. [Google Scholar] [CrossRef] [Green Version]
- Claussen, B.; Smeby, L.; Bruusgaard, D. Disability Pension Rates Among Immigrants in Norway. J. Immigr. Minority Health 2010, 14, 259–263. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cao, Q.; Huang, Y.-H.; Jiang, M.; Dai, C. The prevalence and risk factors of psychological disorders, malnutrition and quality of life in IBD patients. Scand. J. Gastroenterol. 2019, 54, 1458–1466. [Google Scholar] [CrossRef]
- Bernklev, T.; Jahnsen, J.; Henriksen, M.; Lygren, I.; Aadland, E.; Sauar, J.; Schulz, T.; Stray, N.; Vatn, M.; Moum, B. Relationship between sick leave, unemployment, disability, and health-related quality of life in patients with inflammatory bowel disease. Inflamm. Bowel Dis. 2006, 12, 402–412. [Google Scholar] [CrossRef]
- Pizzi, L.T.; Weston, C.M.; Goldfarb, N.I.; Moretti, D.; Cobb, N.; Howell, J.B.; Infantolino, A.; DiMarino, A.J.; Cohen, S. Impact of chronic conditions on quality of life in patients with inflammatory bowel disease. Inflamm. Bowel Dis. 2006, 12, 47–52. [Google Scholar] [CrossRef] [PubMed]
- Jones, J.L.; Nguyen, G.C.; Benchimol, E.I.; Bernstein, C.N.; Bitton, A.; Kaplan, G.G.; Murthy, S.K.; Lee, K.; Cooke-Lauder, J.; Otley, A.R. The Impact of Inflammatory Bowel Disease in Canada 2018: Quality of Life. J. Can. Assoc. Gastroenterol. 2019, 2, S42–S48. [Google Scholar] [CrossRef] [PubMed]
- Niederkrotenthaler, T.; Mittendorfer-Rutz, E.; Saboonchi, F.; Helgesson, M. The role of refugee status and mental disorders regarding subsequent labour market marginalisation: A register study from Sweden. Soc. Psychiatry Psychiatr. Epidemiol. 2020, 55, 697–704. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Refugees | Swedish-Born 1 | p-Value | |
|---|---|---|---|
| (n = 41,516) | (n = 207,729) | ||
| Age (mean, sd) | 22.6 (1.71) | 22.6 (1.71) | |
| Gender (male, n(%)) | 22,189 (53.5) | 110,982 (53.4) | |
| Family situation, n(%) | |||
| Married or cohabitant without children | 2127 (5.12) | 2067 (1.00) | <0.0001 |
| Married or cohabitant with children | 4053 (9.76) | 10,421 (5.02) | <0.0001 |
| Single without children 2 | 30,130 (72.6) | 170,272 (82.0) | <0.0001 |
| Single with children | 1267 (3.05) | 2466 (1.19) | <0.0001 |
| Youth (≤20 years) living at home | 3939 (9.49) | 22,503 (10.8) | <0.0001 |
| Type of living area, n(%) | |||
| Big cities | 18,463 (44.5) | 92,652 (44.6) | |
| Medium-sized cities | 17,002 (41.0) | 85,035 (40.9) | |
| Rural areas | 6051 (14.6) | 30,042 (14.5) | |
| Education levels, n(%) | |||
| 0–9 years | 10,207 (24.6) | 17,633 (8.49) | <0.0001 |
| 10–12 years | 19,637 (47.3) | 123,849 (59.6) | <0.0001 |
| >12 years | 9884 (23.8) | 65,713 (31.6) | <0.0001 |
| Missing | 1788 (4.31) | 534 (0.26) | |
| Previous Sickness absences, n(%) 3 | 467 (1.12) | 3526 (1.70) | <0.0001 |
| Previous Unemployment, n(%) 4 | 3583 (8.63) | 4857 (2.34) | <0.0001 |
| Refugees (n = 41,516) | Swedish-Born (n = 207,729) | |||||
|---|---|---|---|---|---|---|
| n | Crude | Multivariate Model 1 | n | Crude | Multivariate Model 1 | |
| Disability Pension as outcome | ||||||
| Multimorbidity score in disability pension | 379 | 1.67 (1.60, 1.75) | 1.59 (1.52, 1.67) | 2462 | 1.68 (1.66, 1.71) | 1.51 (1.48, 1.54) |
| Unemployment as outcome | ||||||
| Multimorbidity score in unemployment | 7141 | 1.22 (1.19, 1.25) | 1.15 (1.12, 1.17) | 9182 | 1.26 (1.24, 1.28) | 1.12 (1.10, 1.14) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, J.; Mittendorfer-Rutz, E.; Berg, L.; Norredam, M.; Sijbrandij, M.; Klimek, P. Associations between Multimorbidity Patterns and Subsequent Labor Market Marginalization among Refugees and Swedish-Born Young Adults—A Nationwide Registered-Based Cohort Study. J. Pers. Med. 2021, 11, 1305. https://doi.org/10.3390/jpm11121305
Chen J, Mittendorfer-Rutz E, Berg L, Norredam M, Sijbrandij M, Klimek P. Associations between Multimorbidity Patterns and Subsequent Labor Market Marginalization among Refugees and Swedish-Born Young Adults—A Nationwide Registered-Based Cohort Study. Journal of Personalized Medicine. 2021; 11(12):1305. https://doi.org/10.3390/jpm11121305
Chicago/Turabian StyleChen, Jiaying, Ellenor Mittendorfer-Rutz, Lisa Berg, Marie Norredam, Marit Sijbrandij, and Peter Klimek. 2021. "Associations between Multimorbidity Patterns and Subsequent Labor Market Marginalization among Refugees and Swedish-Born Young Adults—A Nationwide Registered-Based Cohort Study" Journal of Personalized Medicine 11, no. 12: 1305. https://doi.org/10.3390/jpm11121305
APA StyleChen, J., Mittendorfer-Rutz, E., Berg, L., Norredam, M., Sijbrandij, M., & Klimek, P. (2021). Associations between Multimorbidity Patterns and Subsequent Labor Market Marginalization among Refugees and Swedish-Born Young Adults—A Nationwide Registered-Based Cohort Study. Journal of Personalized Medicine, 11(12), 1305. https://doi.org/10.3390/jpm11121305






