A Discussion on Different Approaches for Prescribing Physical Interventions – Four Roads Lead to Rome, but Which One Should We Choose?
Abstract
1. Introduction
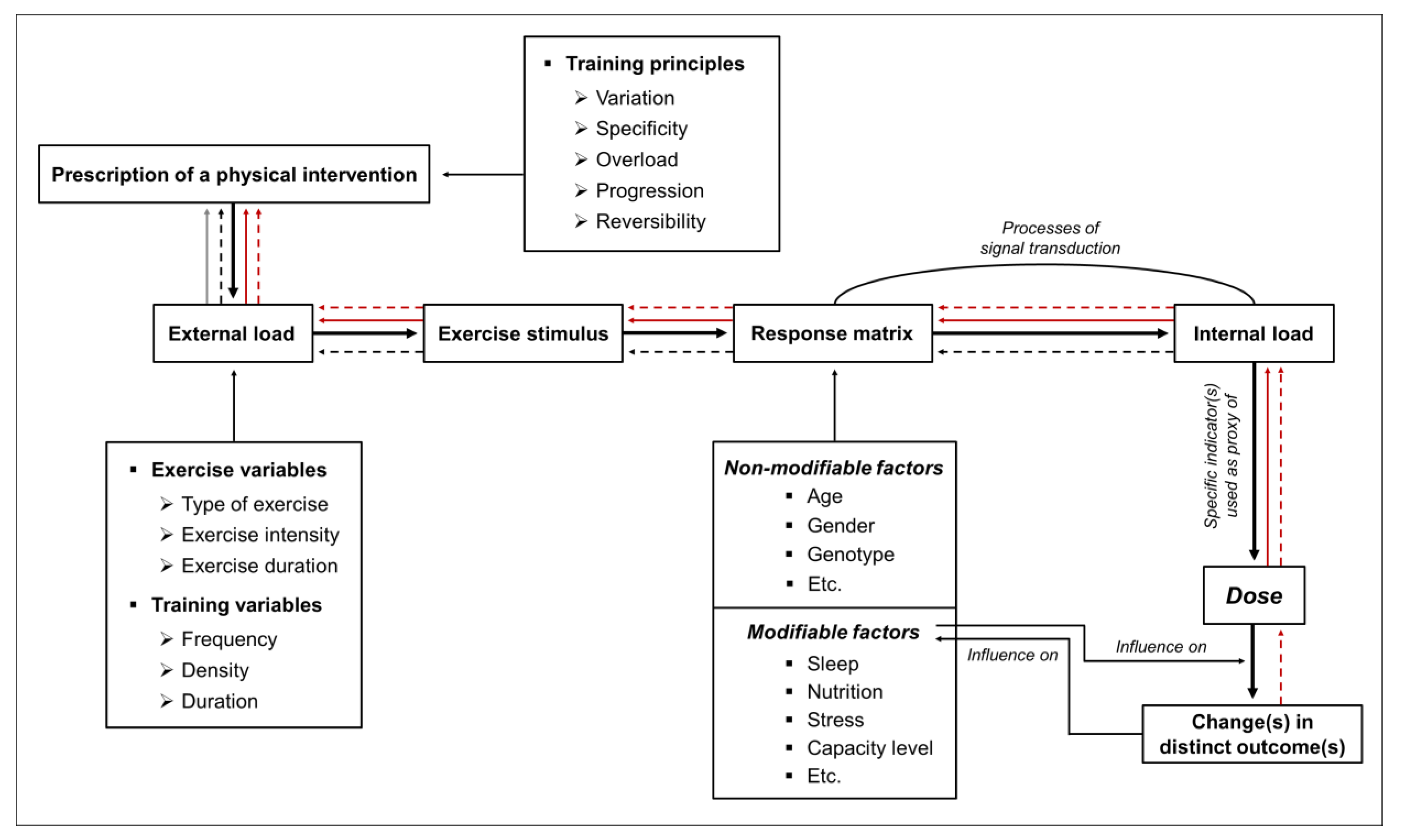
2. Different Approaches to Prescribing Physical Interventions
3. Practical Applications
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Wegner, M.; Helmich, I.; Machado, S.; Nardi, A.E.; Arias-Carrion, O.; Budde, H. Effects of exercise on anxiety and depression disorders: Review of meta-analyses and neurobiological mechanisms. CNS Neurol. Disord. Drug Targets 2014, 13, 1002–1014. [Google Scholar] [CrossRef] [PubMed]
- Budde, H.; Wegner, M.; Soya, H.; Voelcker-Rehage, C.; McMorris, T. Neuroscience of Exercise: Neuroplasticity and Its Behavioral Consequences. Neural Plast. 2016, 2016, 3643879. [Google Scholar] [CrossRef] [PubMed]
- Pedersen, B.K.; Saltin, B. Exercise as medicine—Evidence for prescribing exercise as therapy in 26 different chronic diseases. Scand. J. Med. Sci. Sports 2015, 25, 1–72. [Google Scholar] [CrossRef] [PubMed]
- Pedersen, B.K.; Saltin, B. Evidence for prescribing exercise as therapy in chronic disease. Scand. J. Med. Sci. Sports 2006, 16 (Suppl. 1), 3–63. [Google Scholar] [CrossRef]
- Hillman, C.H.; Erickson, K.I.; Kramer, A.F. Be smart, exercise your heart: Exercise effects on brain and cognition. Nat. Rev. Neurosci. 2008, 9, 58–65. [Google Scholar] [CrossRef] [PubMed]
- Luan, X.; Tian, X.; Zhang, H.; Huang, R.; Li, N.; Chen, P.; Wang, R. Exercise as a prescription for patients with various diseases. J. Sport Health Sci. 2019, 8, 422–441. [Google Scholar] [CrossRef] [PubMed]
- Chodzko-Zajko, W.J.; Proctor, D.N.; Fiatarone Singh, M.A.; Minson, C.T.; Nigg, C.R.; Salem, G.J.; Skinner, J.S. American College of Sports Medicine position stand. Exercise and physical activity for older adults. Med. Sci. Sports Exerc. 2009, 41, 1510–1530. [Google Scholar] [CrossRef]
- Garber, C.E.; Blissmer, B.; Deschenes, M.R.; Franklin, B.A.; Lamonte, M.J.; Lee, I.-M.; Nieman, D.C.; Swain, D.P. American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: Guidance for prescribing exercise. Med. Sci. Sports Exerc. 2011, 43, 1334–1359. [Google Scholar] [CrossRef]
- Liu-Ambrose, T.; Barha, C.K.; Best, J.R. Physical activity for brain health in older adults. Appl. Physiol. Nutr. Metab. 2018, 1–8. [Google Scholar] [CrossRef]
- Erickson, K.I.; Hillman, C.; Stillman, C.M.; Ballard, R.M.; Bloodgood, B.; Conroy, D.E.; Macko, R.; Marquez, D.X.; Petruzzello, S.J.; Powell, K.E. Physical Activity, Cognition, and Brain Outcomes: A Review of the 2018 Physical Activity Guidelines. Med. Sci. Sports Exerc. 2019, 51, 1242–1251. [Google Scholar] [CrossRef]
- Higuera-Hernández, M.F.; Reyes-Cuapio, E.; Gutiérrez-Mendoza, M.; Rocha, N.B.; Veras, A.B.; Budde, H.; Jesse, J.; Zaldívar-Rae, J.; Blanco-Centurión, C.; Machado, S.; et al. Fighting obesity: Non-pharmacological interventions. Clin. Nutr. ESPEN 2018, 25, 50–55. [Google Scholar] [CrossRef]
- Liu-Ambrose, T.; Best, J.R. Exercise is Medicine for the Aging Brain. Kinesiol. Rev. 2017, 6, 22–29. [Google Scholar] [CrossRef]
- Niemann, C.; Wegner, M.; Voelcker-Rehage, C.; Holzweg, M.; Arafat, A.M.; Budde, H. Influence of acute and chronic physical activity on cognitive performance and saliva testosterone in preadolescent school children. Ment. Health Phys. Act. 2013, 6, 197–204. [Google Scholar] [CrossRef]
- Sallis, R.E. Exercise is medicine and physicians need to prescribe it! Br. J. Sports Med. 2009, 43, 3–4. [Google Scholar] [CrossRef] [PubMed]
- Berryman, J.W. Exercise is medicine: A historical perspective. Curr. Sports Med. Rep. 2010, 9, 195–201. [Google Scholar] [CrossRef] [PubMed]
- Lobelo, F.; Stoutenberg, M.; Hutber, A. The Exercise is Medicine Global Health Initiative: A 2014 update. Br. J. Sports Med. 2014, 48, 1627–1633. [Google Scholar] [CrossRef] [PubMed]
- Budde, H.; Schwarz, R.; Velasques, B.; Ribeiro, P.; Holzweg, M.; Machado, S.; Brazaitis, M.; Staack, F.; Wegner, M. The need for differentiating between exercise, physical activity, and training. Autoimmun. Rev. 2016, 15, 110–111. [Google Scholar] [CrossRef] [PubMed]
- Caspersen, C.J.; Powell, K.E.; Christenson, G.M. Physical activity, exercise, and physical fitness: Definitions and distinctions for health-related research. Public Health Rep. 1985, 100, 126–131. [Google Scholar]
- Wegner, M.; Amatriain-Fernández, S.; Kaulitzky, A.; Murillo-Rodriguez, E.; Machado, S.; Budde, H. Systematic Review of Meta-Analyses: Exercise Effects on Depression in Children and Adolescents. Front. Psychiatry 2020, 11. [Google Scholar] [CrossRef]
- Ainsworth, B.E.; Haskell, W.L.; Whitt, M.C.; Irwin, M.L.; Swartz, A.M.; Strath, S.J.; O’Brien, W.L.; Bassett, D.R.; Schmitz, K.H.; Emplaincourt, P.O.; et al. Compendium of physical activities: An update of activity codes and MET intensities. Med. Sci. Sports Exerc. 2000, 32, S498–S504. [Google Scholar] [CrossRef]
- Herold, F.; Müller, P.; Gronwald, T.; Müller, N.G. Dose-response matters!—A perspective on the exercise prescription in exercise-cognition research. Front. Psychol. 2019. [Google Scholar] [CrossRef] [PubMed]
- Gronwald, T.; Budde, H. Commentary: Physical Exercise as Personalized Medicine for Dementia Prevention? Front. Physiol. 2019, 10, 726. [Google Scholar] [CrossRef] [PubMed]
- Herold, F.; Hamacher, D.; Schega, L.; Müller, N.G. Thinking While Moving or Moving While Thinking—Concepts of Motor-Cognitive Training for Cognitive Performance Enhancement. Front. Aging Neurosci. 2018, 10, 228. [Google Scholar] [CrossRef] [PubMed]
- Herold, F.; Törpel, A.; Schega, L.; Müller, N.G. Functional and/or structural brain changes in response to resistance exercises and resistance training lead to cognitive improvements—A systematic review. Eur. Rev. Aging Phys. Act. 2019, 16, 1676. [Google Scholar] [CrossRef] [PubMed]
- Scheuer, J.; Tipton, C.M. Cardiovascular adaptations to physical training. Annu. Rev. Physiol. 1977, 39, 221–251. [Google Scholar] [CrossRef]
- Howley, E.T. Type of activity: Resistance, aerobic and leisure versus occupational physical activity. Med. Sci. Sports Exerc. 2001, 33, S364–S369. [Google Scholar] [CrossRef] [PubMed]
- Fiuza-Luces, C.; Garatachea, N.; Berger, N.A.; Lucia, A. Exercise is the real polypill. Physiology 2013, 28, 330–358. [Google Scholar] [CrossRef]
- Köppel, M.; Hamacher, D. Kräftigung wider das Altern. B G Beweg. Gesundh. 2018, 34, 218–224. [Google Scholar] [CrossRef]
- Pareja-Galeano, H.; Garatachea, N.; Lucia, A. Exercise as a Polypill for Chronic Diseases. Prog. Mol. Biol. Transl. Sci. 2015, 135, 497–526. [Google Scholar] [CrossRef]
- Rebelo-Marques, A.; de Sousa Lages, A.; Andrade, R.; Ribeiro, C.F.; Mota-Pinto, A.; Carrilho, F.; Espregueira-Mendes, J. Aging Hallmarks: The Benefits of Physical Exercise. Front. Endocrinol. 2018, 9, 258. [Google Scholar] [CrossRef]
- Buford, T.W.; Roberts, M.D.; Church, T.S. Toward exercise as personalized medicine. Sports Med. 2013, 43, 157–165. [Google Scholar] [CrossRef] [PubMed]
- Zubin Maslov, P.; Schulman, A.; Lavie, C.J.; Narula, J. Personalized exercise dose prescription. Eur. Heart J. 2018, 39, 2346–2355. [Google Scholar] [CrossRef] [PubMed]
- Pickering, C.; Kiely, J. Do Non-Responders to Exercise Exist—And If So, What Should We Do About Them? Sports Med. 2018, 23, 30. [Google Scholar] [CrossRef]
- Montero, D.; Lundby, C. Refuting the myth of non-response to exercise training: ‘Non-responders’ do respond to higher dose of training. J. Physiol. 2017, 595, 3377–3387. [Google Scholar] [CrossRef] [PubMed]
- Ross, R.; de Lannoy, L.; Stotz, P.J. Separate Effects of Intensity and Amount of Exercise on Interindividual Cardiorespiratory Fitness Response. Mayo Clin. Proc. 2015, 90, 1506–1514. [Google Scholar] [CrossRef]
- Bonafiglia, J.T.; Rotundo, M.P.; Whittall, J.P.; Scribbans, T.D.; Graham, R.B.; Gurd, B.J. Inter-Individual Variability in the Adaptive Responses to Endurance and Sprint Interval Training: A Randomized Crossover Study. PLoS ONE 2016, 11, e0167790. [Google Scholar] [CrossRef]
- Voils, C.I.; Chang, Y.; Crandell, J.; Leeman, J.; Sandelowski, M.; Maciejewski, M.L. Informing the dosing of interventions in randomized trials. Contemp. Clin. Trials 2012, 33, 1225–1230. [Google Scholar] [CrossRef]
- Burgess, D.J. The Research Doesn’t Always Apply: Practical Solutions to Evidence-Based Training-Load Monitoring in Elite Team Sports. Int. J. Sports Physiol. Perform. 2017, 12, S2136–S2141. [Google Scholar] [CrossRef]
- Bourdon, P.C.; Cardinale, M.; Murray, A.; Gastin, P.; Kellmann, M.; Varley, M.C.; Gabbett, T.J.; Coutts, A.J.; Burgess, D.J.; Gregson, W.; et al. Monitoring Athlete Training Loads: Consensus Statement. Int. J. Sports Physiol. Perform. 2017, 12, S2-161–S2-170. [Google Scholar] [CrossRef]
- McLaren, S.J.; Macpherson, T.W.; Coutts, A.J.; Hurst, C.; Spears, I.R.; Weston, M. The Relationships Between Internal and External Measures of Training Load and Intensity in Team Sports: A Meta-Analysis. Sports Med. 2018, 48, 641–658. [Google Scholar] [CrossRef]
- Vanrenterghem, J.; Nedergaard, N.J.; Robinson, M.A.; Drust, B. Training Load Monitoring in Team Sports: A Novel Framework Separating Physiological and Biomechanical Load-Adaptation Pathways. Sports Med. 2017, 47, 2135–2142. [Google Scholar] [CrossRef] [PubMed]
- Wallace, L.K.; Slattery, K.M.; Coutts, A.J. The ecological validity and application of the session-RPE method for quantifying training loads in swimming. J. Strength Cond. Res. 2009, 23, 33–38. [Google Scholar] [CrossRef] [PubMed]
- Halson, S.L. Monitoring training load to understand fatigue in athletes. Sports Med. 2014, 44 (Suppl. 2), S139–S147. [Google Scholar] [CrossRef]
- Impellizzeri, F.M.; Marcora, S.M.; Coutts, A.J. Internal and External Training Load: 15 Years On. Int. J. Sports Physiol. Perform. 2019, 14, 270–273. [Google Scholar] [CrossRef] [PubMed]
- Soligard, T.; Schwellnus, M.; Alonso, J.-M.; Bahr, R.; Clarsen, B.; Dijkstra, H.P.; Gabbett, T.; Gleeson, M.; Hägglund, M.; Hutchinson, M.R.; et al. How much is too much? (Part 1) International Olympic Committee consensus statement on load in sport and risk of injury. Br. J. Sports Med. 2016, 50, 1030–1041. [Google Scholar] [CrossRef] [PubMed]
- Hofmann, P.; Tschakert, G. Special needs to prescribe exercise intensity for scientific studies. Cardiol. Res. Pract. 2010, 2011, 209302. [Google Scholar] [CrossRef]
- Mann, T.; Lamberts, R.P.; Lambert, M.I. Methods of prescribing relative exercise intensity: Physiological and practical considerations. Sports Med. 2013, 43, 613–625. [Google Scholar] [CrossRef]
- Gass, G.C.; McLellan, T.M.; Gass, E.M. Effects of prolonged exercise at a similar percentage of maximal oxygen consumption in trained and untrained subjects. Eur. J. Appl. Physiol. 1991, 63, 430–435. [Google Scholar] [CrossRef]
- Katch, V.; Weltman, A.; Sady, S.; Freedson, P. Validity of the relative percent concept for equating training intensity. Eur. J. Appl. Physiol. 1978, 39, 219–227. [Google Scholar] [CrossRef]
- Meyer, T.; Gabriel, H.H.; Kindermann, W. Is determination of exercise intensities as percentages of VO2max or HRmax adequate? Med. Sci. Sports Exerc. 1999, 31, 1342–1345. [Google Scholar] [CrossRef]
- Scharhag-Rosenberger, F.; Meyer, T.; Gässler, N.; Faude, O.; Kindermann, W. Exercise at given percentages of VO2max: Heterogeneous metabolic responses between individuals. J. Sci. Med. Sport 2010, 13, 74–79. [Google Scholar] [CrossRef] [PubMed]
- Weltman, A.; Weltman, J.; Rutt, R.; Seip, R.; Levine, S.; Snead, D.; Kaiser, D.; Rogol, A. Percentages of maximal heart rate, heart rate reserve, and VO2peak for determining endurance training intensity in sedentary women. Int. J. Sports Med. 1989, 10, 212–216. [Google Scholar] [CrossRef] [PubMed]
- Weltman, A.; Snead, D.; Seip, R.; Schurrer, R.; Weltman, J.; Rutt, R.; Rogol, A. Percentages of maximal heart rate, heart rate reserve and VO2max for determining endurance training intensity in male runners. Int. J. Sports Med. 1990, 11, 218–222. [Google Scholar] [CrossRef] [PubMed]
- Weatherwax, R.M.; Harris, N.K.; Kilding, A.E.; Dalleck, L.C. The incidence of training responsiveness to cardiorespiratory fitness and cardiometabolic measurements following individualized and standardized exercise prescription: Study protocol for a randomized controlled trial. Trials 2016, 17, 601. [Google Scholar] [CrossRef] [PubMed]
- Gronwald, T.; Velasques, B.; Ribeiro, P.; Machado, S.; Murillo-Rodríguez, E.; Ludyga, S.; Yamamoto, T.; Budde, H. Increasing exercise’s effect on mental health: Exercise intensity does matter. Proc. Natl. Acad. Sci. USA 2018, 115, E11890–E11891. [Google Scholar] [CrossRef] [PubMed]
- Suwabe, K.; Byun, K.; Hyodo, K.; Reagh, Z.M.; Roberts, J.M.; Matsushita, A.; Saotome, K.; Ochi, G.; Fukuie, T.; Suzuki, K.; et al. Reply to Gronwald et al.: Exercise intensity does indeed matter; maximal oxygen uptake is the gold-standard indicator. Proc. Natl. Acad. Sci. USA 2018. [Google Scholar] [CrossRef]
- Toigo, M.; Boutellier, U. New fundamental resistance exercise determinants of molecular and cellular muscle adaptations. Eur. J. Appl. Physiol. 2006, 97, 643–663. [Google Scholar] [CrossRef]
- Schneider, J.; Schlüter, K.; Sprave, T.; Wiskemann, J.; Rosenberger, F. Exercise intensity prescription in cancer survivors: Ventilatory and lactate thresholds are useful submaximal alternatives to VO2peak. Support. Care Cancer 2020. [Google Scholar] [CrossRef]
- Herold, F.; Gronwald, T.; Scholkmann, F.; Zohdi, H.; Wyser, D.; Müller, N.G.; Hamacher, D. New Directions in Exercise Prescription: Is There a Role for Brain-Derived Parameters Obtained by Functional Near-Infrared Spectroscopy? Brain Sci. 2020, 10, 342. [Google Scholar] [CrossRef]
- Impellizzeri, F.M.; Rampinini, E.; Marcora, S.M. Physiological assessment of aerobic training in soccer. J. Sports Sci. 2005, 23, 583–592. [Google Scholar] [CrossRef]
- Impellizzeri, F.M.; Rampinini, E.; Coutts, A.J.; Sassi, A.; Marcora, S.M. Use of RPE-based training load in soccer. Med. Sci. Sports Exerc. 2004, 36, 1042–1047. [Google Scholar] [CrossRef] [PubMed]
- Vollaard, N.B.J.; Constantin-Teodosiu, D.; Fredriksson, K.; Rooyackers, O.; Jansson, E.; Greenhaff, P.L.; Timmons, J.A.; Sundberg, C.J. Systematic analysis of adaptations in aerobic capacity and submaximal energy metabolism provides a unique insight into determinants of human aerobic performance. J. Appl. Physiol. 2009, 106, 1479–1486. [Google Scholar] [CrossRef] [PubMed]
- Tschakert, G.; Hofmann, P. High-Intensity Intermittent Exercise: Methodological and Physiological Aspects. Int. J. Sports Physiol. Perform. 2013, 8, 600–610. [Google Scholar] [CrossRef] [PubMed]
- Stöggl, T.L.; Sperlich, B. The training intensity distribution among well-trained and elite endurance athletes. Front. Physiol. 2015, 6, 295. [Google Scholar] [CrossRef]
- Beneke, R.; Leithäuser, R.M.; Ochentel, O. Blood lactate diagnostics in exercise testing and training. Int. J. Sports Physiol. Perform. 2011, 6, 8–24. [Google Scholar] [CrossRef]
- Faude, O.; Kindermann, W.; Meyer, T. Lactate threshold concepts: How valid are they? Sports Med. 2009, 39, 469–490. [Google Scholar] [CrossRef]
- Seiler, K.S.; Kjerland, G.Ø. Quantifying training intensity distribution in elite endurance athletes: Is there evidence for an “optimal” distribution? Scand. J. Med. Sci. Sports 2006, 16, 49–56. [Google Scholar] [CrossRef]
- Lüscher, T.F. What is a normal blood pressure? Eur. Heart J. 2018, 39, 2233–2240. [Google Scholar] [CrossRef]
- Guyatt, G.; Sackett, D.; Adachi, J.; Roberts, R.; Chong, J.; Rosenbloom, D.; Keller, J. A clinician’s guide for conducting randomized trials in individual patients. CMAJ 1988, 139, 497–503. [Google Scholar]
- Kwasnicka, D.; Naughton, F. N-of-1 methods: A practical guide to exploring trajectories of behaviour change and designing precision behaviour change interventions. Psychol. Sport Exerc. 2019, 101570. [Google Scholar] [CrossRef]
- Nikles, C.J.; Clavarino, A.M.; Del Mar, C.B. Using n-of-1 trials as a clinical tool to improve prescribing. Br. J. Gen. Pract. 2005, 55, 175–180. [Google Scholar] [PubMed]
- Nikles, J.; Mitchell, G. The Essential Guide to N-of-1 Trials in Health; Springer Netherlands: Dordrecht, The Netherlands, 2015; ISBN 978-94-017-7199-3. [Google Scholar]
- Xie, T.; Yu, Z. N-of-1 Design and Its Applications to Personalized Treatment Studies. Stat. Biosci. 2017, 9, 662–675. [Google Scholar] [CrossRef][Green Version]
- Schork, N.J. Personalized medicine: Time for one-person trials. Nature 2015, 520, 609–611. [Google Scholar] [CrossRef] [PubMed]
- Lillie, E.O.; Patay, B.; Diamant, J.; Issell, B.; Topol, E.J.; Schork, N.J. The n-of-1 clinical trial: The ultimate strategy for individualizing medicine? Per. Med. 2011, 8, 161–173. [Google Scholar] [CrossRef] [PubMed]
- Düking, P.; Achtzehn, S.; Holmberg, H.-C.; Sperlich, B. Integrated Framework of Load Monitoring by a Combination of Smartphone Applications, Wearables and Point-of-Care Testing Provides Feedback that Allows Individual Responsive Adjustments to Activities of Daily Living. Sensors 2018, 18. [Google Scholar] [CrossRef]
- Hasenöhrl, T.; Windschnurer, T.; Dorotka, R.; Ambrozy, C.; Crevenna, R. Prescription of individual therapeutic exercises via smartphone app for patients suffering from non-specific back pain: A qualitative feasibility and quantitative pilot study. Wien. Klin. Wochenschr. 2020, 132, 115–123. [Google Scholar] [CrossRef]
- Düking, P.; Hotho, A.; Holmberg, H.-C.; Fuss, F.K.; Sperlich, B. Comparison of Non-Invasive Individual Monitoring of the Training and Health of Athletes with Commercially Available Wearable Technologies. Front. Physiol. 2016, 7, 71. [Google Scholar] [CrossRef]
- Düking, P.; Fuss, F.K.; Holmberg, H.-C.; Sperlich, B. Recommendations for Assessment of the Reliability, Sensitivity, and Validity of Data Provided by Wearable Sensors Designed for Monitoring Physical Activity. JMIR Mhealth Uhealth 2018, 6, e102. [Google Scholar] [CrossRef]
- Peake, J.M.; Kerr, G.; Sullivan, J.P. A Critical Review of Consumer Wearables, Mobile Applications, and Equipment for Providing Biofeedback, Monitoring Stress, and Sleep in Physically Active Populations. Front. Physiol. 2018, 9, 743. [Google Scholar] [CrossRef]
- Bonato, M.; Turrini, F.; de Zan, V.; Meloni, A.; Plebani, M.; Brambilla, E.; Giordani, A.; Vitobello, C.; Caccia, R.; Piacentini, M.F.; et al. A Mobile Application for Exercise Intervention in People Living with HIV. Med. Sci. Sports Exerc. 2020, 52, 425–433. [Google Scholar] [CrossRef]
- Lambert, T.E.; Harvey, L.A.; Avdalis, C.; Chen, L.W.; Jeyalingam, S.; Pratt, C.A.; Tatum, H.J.; Bowden, J.L.; Lucas, B.R. An app with remote support achieves better adherence to home exercise programs than paper handouts in people with musculoskeletal conditions: A randomised trial. J. Physiother. 2017, 63, 161–167. [Google Scholar] [CrossRef] [PubMed]
- Voth, E.C.; Oelke, N.D.; Jung, M.E. A Theory-Based Exercise App to Enhance Exercise Adherence: A Pilot Study. JMIR Mhealth Uhealth 2016, 4, e62. [Google Scholar] [CrossRef] [PubMed]
- Cardinale, M.; Varley, M.C. Wearable Training-Monitoring Technology: Applications, Challenges, and Opportunities. Int. J. Sports Physiol. Perform. 2017, 12, S255–S262. [Google Scholar] [CrossRef] [PubMed]
- Gronwald, T.; de Bem Alves, A.C.; Murillo-Rodríguez, E.; Latini, A.; Schuette, J.; Budde, H. Standardization of exercise intensity and consideration of a dose-response is essential. Commentary on “Exercise-linked FNDC5/irisin rescues synaptic plasticity and memory defects in Alzheimer’s models”, by Lourenco et al., published 2019 in Nature Medicine. J. Sport Health Sci. 2019, 8, 353–354. [Google Scholar] [CrossRef]
- Herold, F.; Aye, N.; Lehmann, N.; Taubert, M.; Müller, N.G. The Contribution of Functional Magnetic Resonance Imaging to the Understanding of the Effects of Acute Physical Exercise on Cognition. Brain Sci. 2020, 10, 175. [Google Scholar] [CrossRef]
- Budde, H.; Akko, D.P.; Ainamani, H.E.; Murillo-Rodríguez, E.; Weierstall, R. The impact of an exercise training intervention on cortisol levels and post-traumatic stress disorder in juveniles from an Ugandan refugee settlement: Study protocol for a randomized control trial. Trials 2018, 19, 364. [Google Scholar] [CrossRef]
| External Load | Internal Load | Dose | Outcome | |||||
|---|---|---|---|---|---|---|---|---|
| CAI | IH | CAI | IH | CAI | IH | CAI | IH | |
| (i) Comparable external load | ↑ | ↓ | ↓ | ↑ | ↓ | ↑ | ↓ | ↑ |
| (ii) Comparable internal load | ↓ | ↑ | ↑ | ↓ | ↓ | ↑ | ↓ | ↑ |
| (iii) Comparable dose | ↓ | ↑ | ↓ | ↑ | ↑ | ↓ | ? | ? |
| (iv) Comparable outcome | ↓ | ↑ | ↓ | ↑ | ? | ? | ↑ | ↓ |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Herold, F.; Törpel, A.; Hamacher, D.; Budde, H.; Gronwald, T. A Discussion on Different Approaches for Prescribing Physical Interventions – Four Roads Lead to Rome, but Which One Should We Choose? J. Pers. Med. 2020, 10, 55. https://doi.org/10.3390/jpm10030055
Herold F, Törpel A, Hamacher D, Budde H, Gronwald T. A Discussion on Different Approaches for Prescribing Physical Interventions – Four Roads Lead to Rome, but Which One Should We Choose? Journal of Personalized Medicine. 2020; 10(3):55. https://doi.org/10.3390/jpm10030055
Chicago/Turabian StyleHerold, Fabian, Alexander Törpel, Dennis Hamacher, Henning Budde, and Thomas Gronwald. 2020. "A Discussion on Different Approaches for Prescribing Physical Interventions – Four Roads Lead to Rome, but Which One Should We Choose?" Journal of Personalized Medicine 10, no. 3: 55. https://doi.org/10.3390/jpm10030055
APA StyleHerold, F., Törpel, A., Hamacher, D., Budde, H., & Gronwald, T. (2020). A Discussion on Different Approaches for Prescribing Physical Interventions – Four Roads Lead to Rome, but Which One Should We Choose? Journal of Personalized Medicine, 10(3), 55. https://doi.org/10.3390/jpm10030055








