Fatal Immunohaemolysis after the Consumption of the Poison Pax Mushroom: A Focus on the Diagnosis of the Paxillus Syndrome with the Aid of Two Case Reports
Abstract
:1. Introduction
2. Methods
2.1. Case Histories and Course of Events
2.1.1. Case 1
2.1.2. Case 2
2.2. Laboratory Tests during Hospitalisation and Post-Mortem Investigations
3. Results
3.1. Laboratory Tests During Hospitalisation
3.1.1. Case 1
3.1.2. Case 2
3.2. Post-Mortem Immunohaematological Tests
3.2.1. Case 1
3.2.2. Case 2
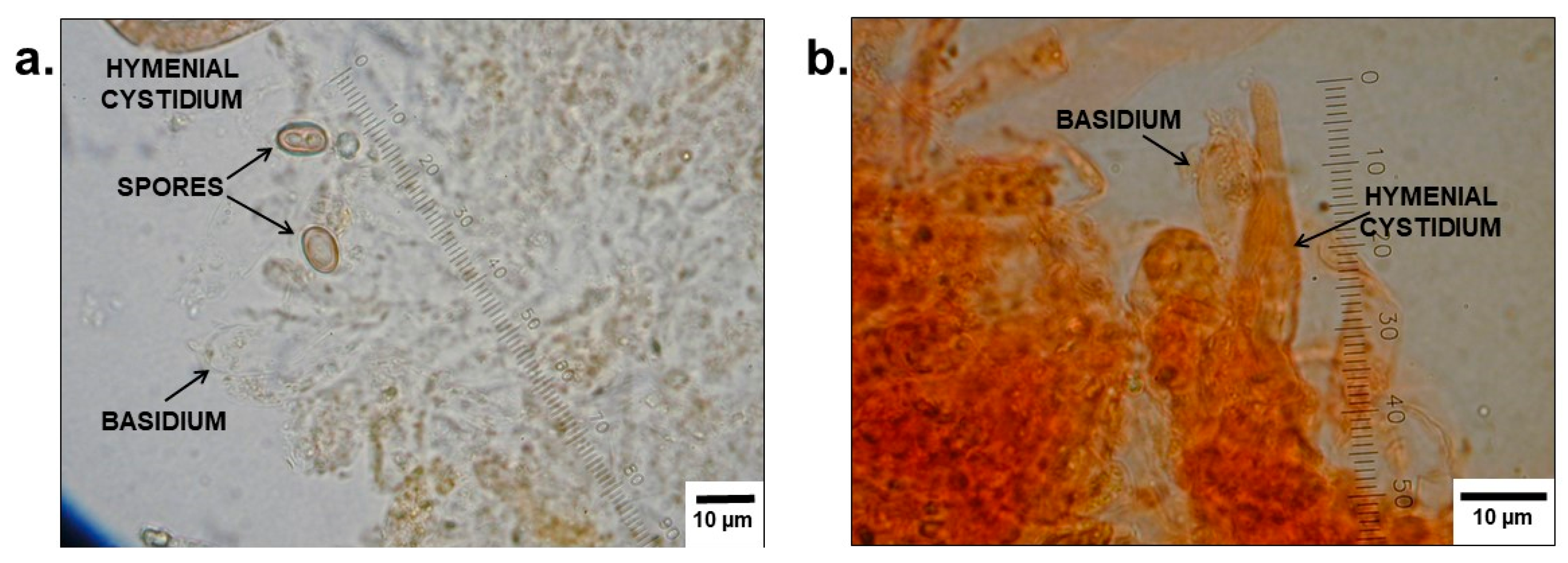
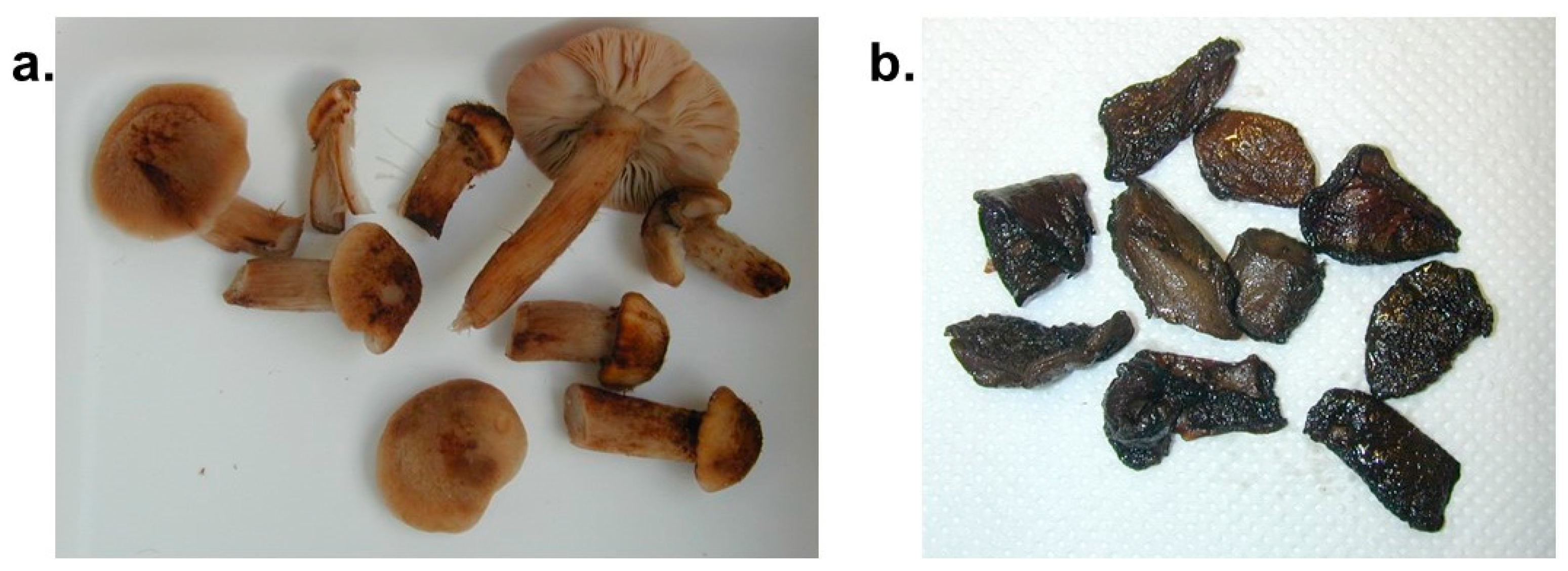
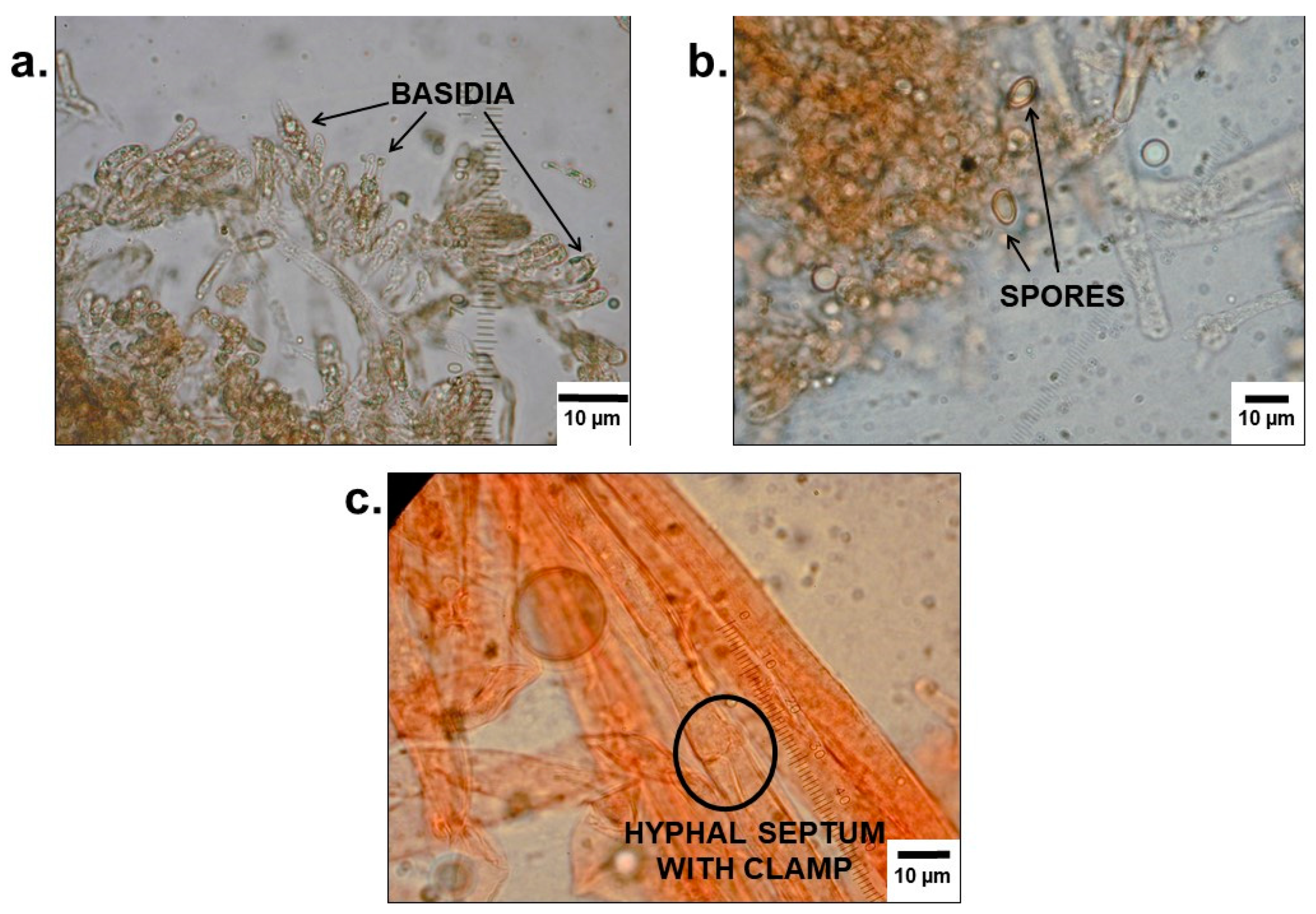
3.3. Mycological Analyses
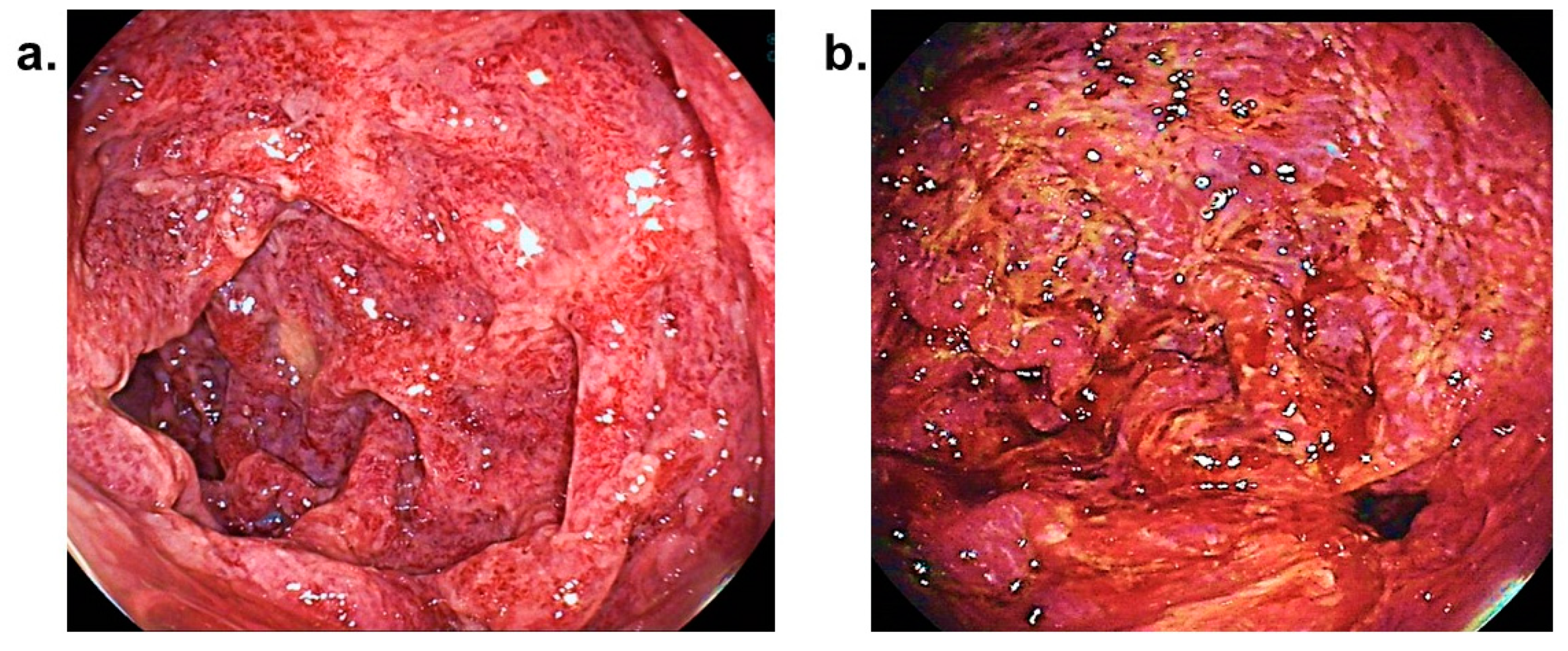
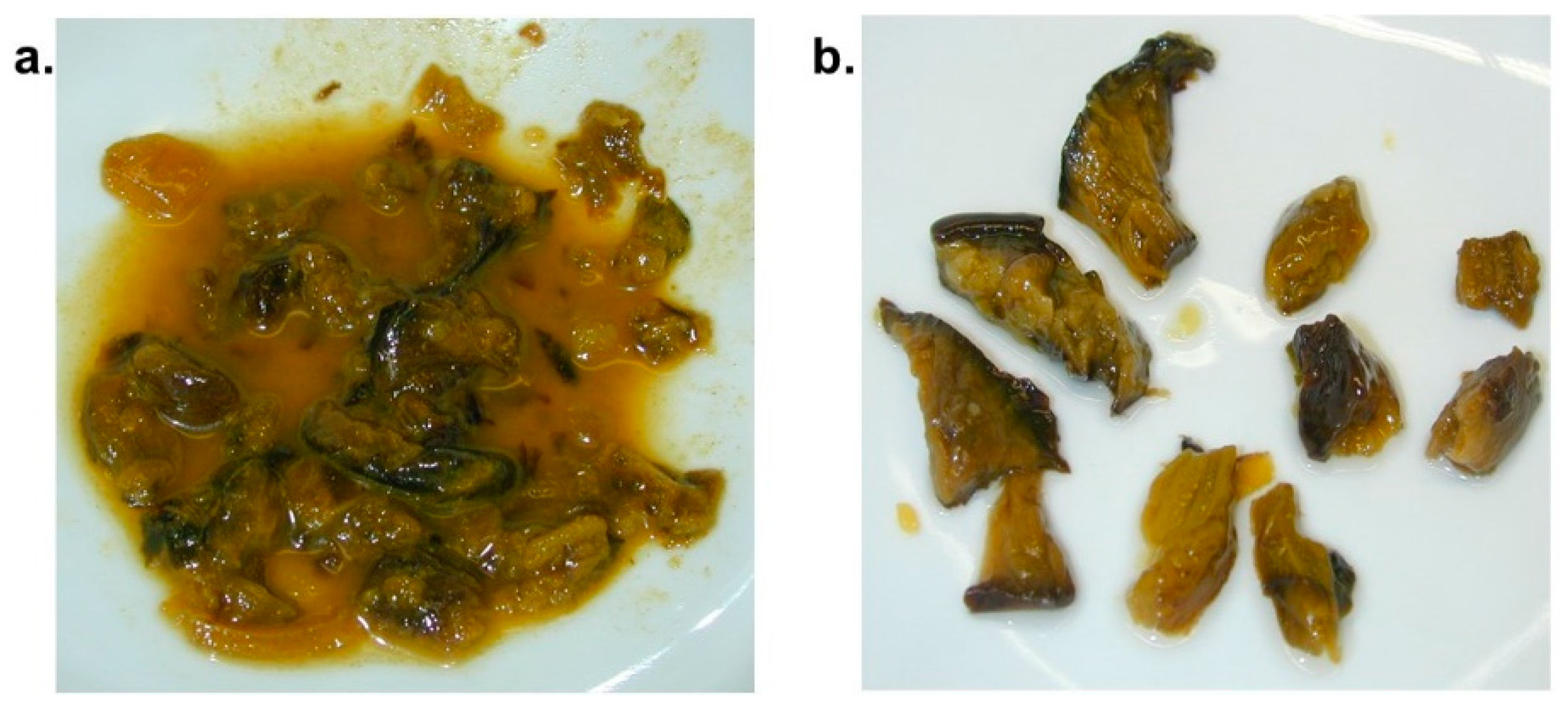
3.3.1. Analysis of Stomach Contents of Case 1
3.3.2. Analysis of Samples from the Mushroom Meal Consumed by Patient 2
3.4. Post-Mortem Examination
3.4.1. Autopsy of Case 1
3.4.2. Necropsy of Case 2
3.5. Toxicological Analyses
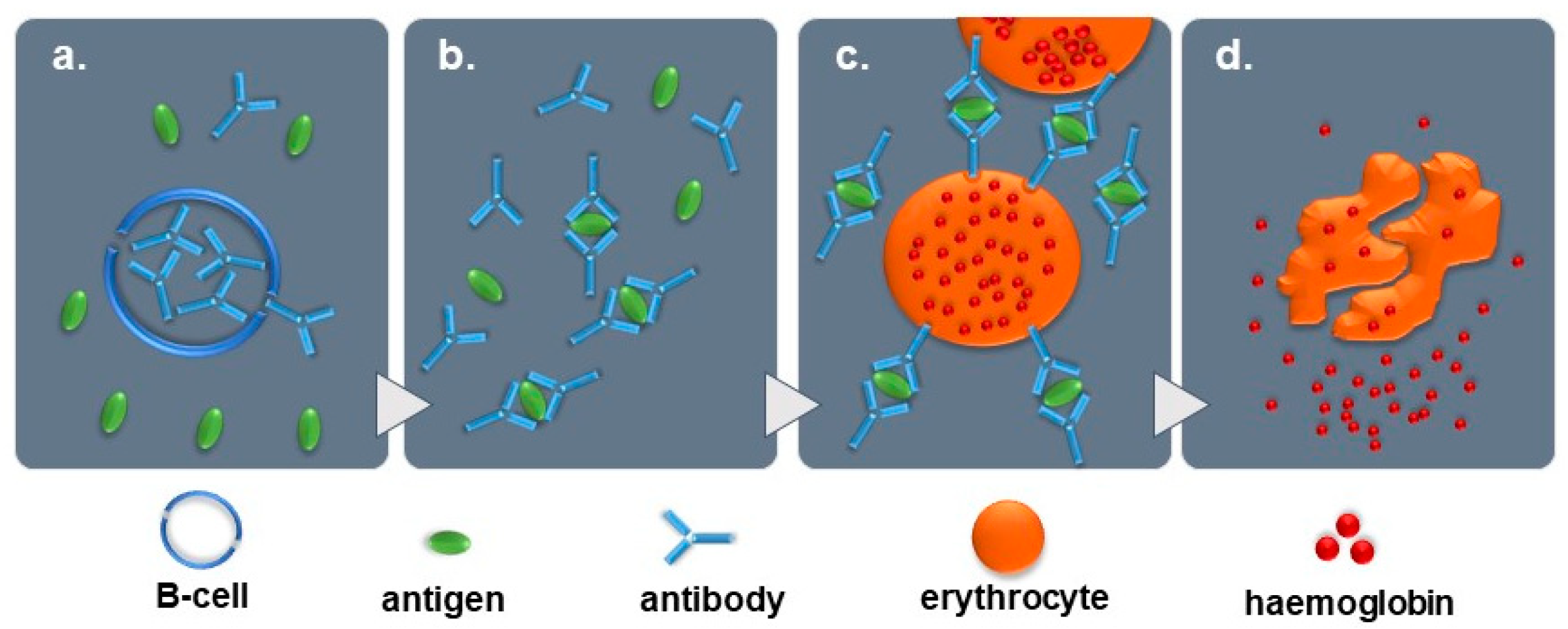
4. Discussion
5. Conclusions
Author Contributions
Acknowledgments
Conflicts of Interest
Consent for Publication
References
- White, J.; Weinstein, S.A.; De Haro, L.; Bédry, R.; Schaper, A.; Rumack, B.H.; Zilker, T. Mushroom poisoning: A proposed new clinical classification. Toxicon 2019, 157, 53–65. [Google Scholar] [CrossRef] [PubMed]
- Zilker, T.; Faulstich, H. Cyclopeptide-containing mushrooms: The deadly Amanitas. Crit. Care Toxicol. Diagn. Manag. Crit. Poisoned Patient 2017, 1–21. [Google Scholar] [CrossRef]
- Erden, A.; Esmeray, K.; Karagöz, H.; Karahan, S.; Gümüşçü, H.H.; Başak, M.; Cetinkaya, A.; Avcı, D.; Poyrazoğlu, O.K. Acute liver failure caused by mushroom poisoning: A case report and review of the literature. Int. Med. Case Rep. J. 2013, 6, 85–90. [Google Scholar] [CrossRef] [PubMed]
- Chen, Z.; Zhang, P.; Zhang, Z. Investigation and analysis of 102 mushroom poisoning cases in Southern China from 1994 to 2012. Fungal Divers. 2014, 64, 123–131. [Google Scholar] [CrossRef]
- Ye, Y.; Liu, Z. Management of Amanita phalloides poisoning: A literature review and update. J. Crit. Care 2018, 46, 17–22. [Google Scholar] [CrossRef] [PubMed]
- Bschor, F.; Mallach, H.J. Vergiftungen durch den Kahlen Krempling (Paxillus involutus), eine genießbare Pilzart. Arch. Toxikol. 1963, 20, 82–95. [Google Scholar] [CrossRef] [PubMed]
- Deicher, H.; Stangel, W. Akute immunhämolytische Anämie nach Genuß des Kahlen Kremplings. Verh. Dtsch. Ges. Inn. Med. 1977, 83, 1606–1609. [Google Scholar] [PubMed]
- Schmidt, J.; Hartmann, W.; Würstlin, A.; Deicher, H. Akutes Nierenversagen durch immunhämolytisches Anämie nach Genuß des Kahlen Kremplings (Paxillus involutus). Dtsch. Med. Wochenschr. 1971, 28, 1188–1191. [Google Scholar] [CrossRef] [PubMed]
- Winkelmann, M.; Stangel, W.; Schedel, I.; Grabensee, B. Severe hemolysis caused by the mushroom Paxillus involutus and its therapy by plasma exchange. Klin. Wochenschr. 1986, 64, 935–938. [Google Scholar] [CrossRef] [PubMed]
- Knudsen, H.; Vesterholt, J. Funga Nordica: Agaricoid, Boletoid and Cyphelloid Genera; Nordsvamp: Copenhagen, Danmark, 2008. [Google Scholar]
- Lefèvre, H. Immunhämolytische Anämie nach Genuß des Kahlen Krempling (Paxillus involutus). Dtsch. Med. Wochenschr. 1982, 107, 1374. [Google Scholar]
- Okonek, S. Hämoperfusion mit beschichteter Aktivkohle zur Behandlung akuter Intoxikationen durch Arzneimittel, Pflanzenschutzmittel oder Pilze. Med. Klin. 1976, 71, 72. [Google Scholar]
- Winkelmann, M.; Borchard, F.; Stangel, W.; Grabensee, B. Fatal immunohaemolytic anaemia after eating the mushroom Paxillus involutus. DMW 1982, 107, 1190–1194. [Google Scholar] [CrossRef] [PubMed]
- Salama, A. Drug-induced immune hemolytic anemia. Expert Opin. Drug Saf. 2009, 8, 73–79. [Google Scholar] [CrossRef] [PubMed]
- Müller, H.M.; Pfaff, E.; Goeser, T.; Kallinowski, B.; Solbach, C.; Theilmann, L. Peripheral blood leukocytes serve as a possible extrahepatic site foe hepatitis C virus. J. Gen. Virol. 1993, 74, 669–676. [Google Scholar] [CrossRef] [PubMed]


| Patient 1 | ||||||
| DAY 1 | DAY 3 | DAY 4 | DAY 5 | |||
| 12:00 | 15:00 | evening | 18:00 | |||
| Mushroom consumption | Severe backache | Respiratory & circulatory complications | Septic shock | Patient declared brain dead | ||
| Hospital admission | Transfer to maximum-care hospital | Sudden hypertension | Exitus letalis | |||
| Increasing abdominal pain | Improvement of liver function | Massive cerebral swelling | ||||
| Acute liver failure | ||||||
| Patient 2 | ||||||
| DAY 1 | DAY 2 | DAY 3 | DAY 5 | |||
| 19:00 | 21:00 | 22:05 | 22:40 | 06:00 | 02:30 | |
| Mushroom consumption | Abdominal pain, nausea & vomiting | Notification of emergency medical services | Hospital admission & treatment Patient stabilised | Transfer to maximum-care hospital Plasmapheresis, kidney replacement & haemo-adsorption filters therapy - Patient stabilised | Patient’s condition worsens Acute on chronic liver failure | Exitus letalis |
| Parameter | Levels Measured | Reference Range |
|---|---|---|
| AST, GOT | 9500 U/L | 8–43 U/L |
| ALT, GPT | 2800 U/L | 7–45 U/L |
| LDH | 7600 U/L | 122–222 U/L |
| Blood Group | B |
|---|---|
| Rhesus Formula | CcD.ee |
| Direct Coombs Test (DCT) | |
| Polyspecific Coombs serum | +++ |
| Monospecific Coombs serum with: | |
| Anti-IgG | + |
| Anti-C3d | +++ |
| Femoral Blood | Urine | Stomach Contents | |
|---|---|---|---|
| substance | concentration | substance | substance |
| Midazolam | 2400 µg/L | Midazolam | Midazolam |
| Hydroxymidazolam | 100 µg/L | Hydroxymidazolam | Hydroxymidazolam |
| Sufentanil | 2.0 µg/L | Sufentanil | Sufentanil |
| 4-Methylaminoantipyrine | not quantified | 4-Methylaminoantipyrine | 4-Methylaminoantipyrine |
| Piritramide | 1.7 µg/L | Piritramide | not detected |
| Metoclopramide | 64 µg/L | Metoclopramide | Metoclopramide |
| Lidocaine | not quantified | Lidocaine | Lidocaine |
| Propofol | not analysed | Propofol | not analysed |
| not analysed | not analysed | Caffeine | not analysed |
| Patient Serum | |
|---|---|
| Substance | Concentration |
| Midazolam | 110 µg/L |
| Hydroxymidazolam | 22 µg/L |
| Lidocaine | 44 µg/L |
| Remifentanil acid | not quantified |
| Ibuprofen | not quantified |
| Cotinine | not quantified |
| Caffeine | not quantified |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stöver, A.; Haberl, B.; Helmreich, C.; Müller, W.; Musshoff, F.; Fels, H.; Graw, M.; Groth, O. Fatal Immunohaemolysis after the Consumption of the Poison Pax Mushroom: A Focus on the Diagnosis of the Paxillus Syndrome with the Aid of Two Case Reports. Diagnostics 2019, 9, 130. https://doi.org/10.3390/diagnostics9040130
Stöver A, Haberl B, Helmreich C, Müller W, Musshoff F, Fels H, Graw M, Groth O. Fatal Immunohaemolysis after the Consumption of the Poison Pax Mushroom: A Focus on the Diagnosis of the Paxillus Syndrome with the Aid of Two Case Reports. Diagnostics. 2019; 9(4):130. https://doi.org/10.3390/diagnostics9040130
Chicago/Turabian StyleStöver, Andreas, Bettina Haberl, Claudia Helmreich, Werner Müller, Frank Musshoff, Helena Fels, Matthias Graw, and Olwen Groth. 2019. "Fatal Immunohaemolysis after the Consumption of the Poison Pax Mushroom: A Focus on the Diagnosis of the Paxillus Syndrome with the Aid of Two Case Reports" Diagnostics 9, no. 4: 130. https://doi.org/10.3390/diagnostics9040130
APA StyleStöver, A., Haberl, B., Helmreich, C., Müller, W., Musshoff, F., Fels, H., Graw, M., & Groth, O. (2019). Fatal Immunohaemolysis after the Consumption of the Poison Pax Mushroom: A Focus on the Diagnosis of the Paxillus Syndrome with the Aid of Two Case Reports. Diagnostics, 9(4), 130. https://doi.org/10.3390/diagnostics9040130




