Codex (Cognitive Disorders Examination) Decision Tree Modified for the Detection of Dementia and MCI
Abstract
1. Introduction
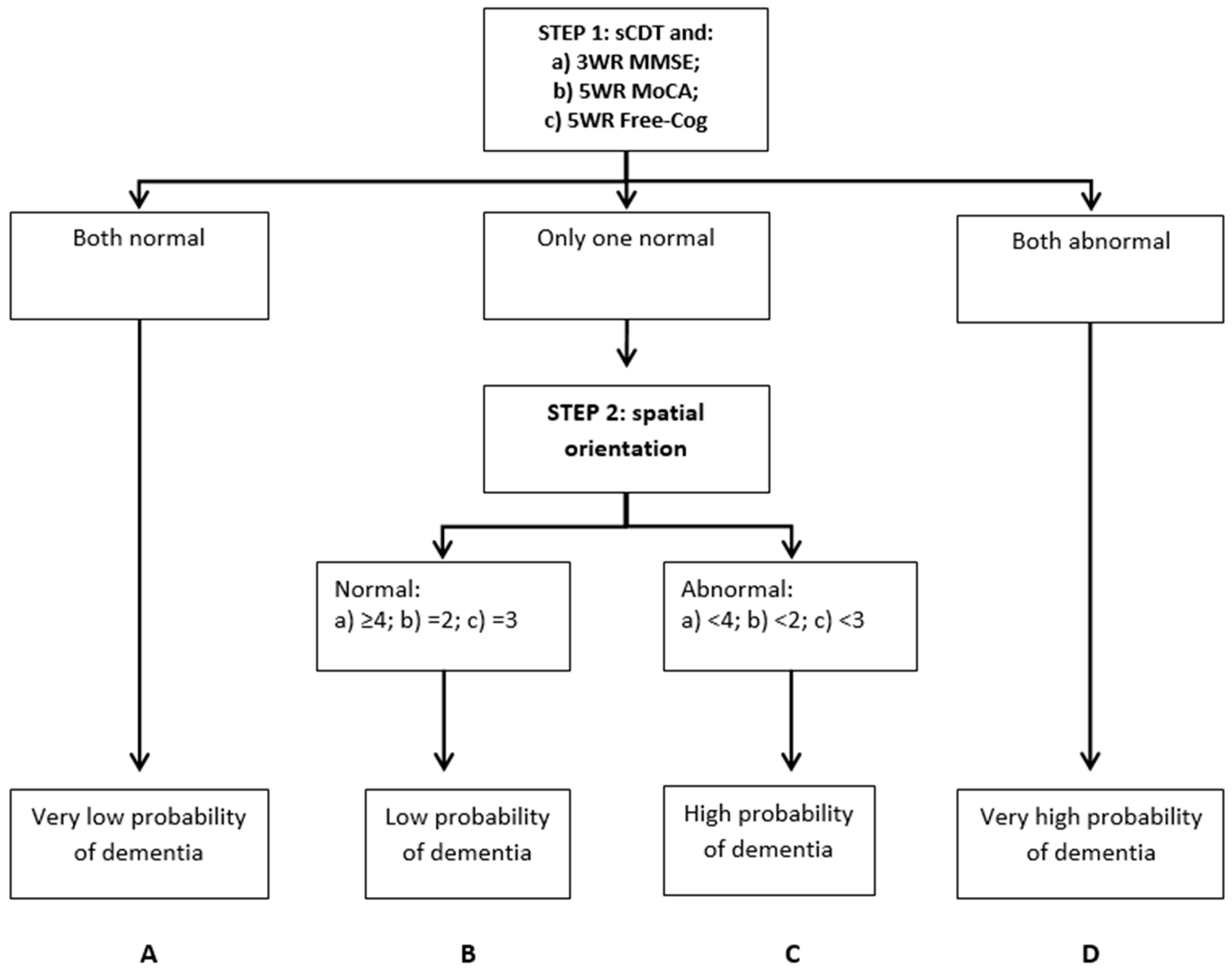
2. Materials and Methods
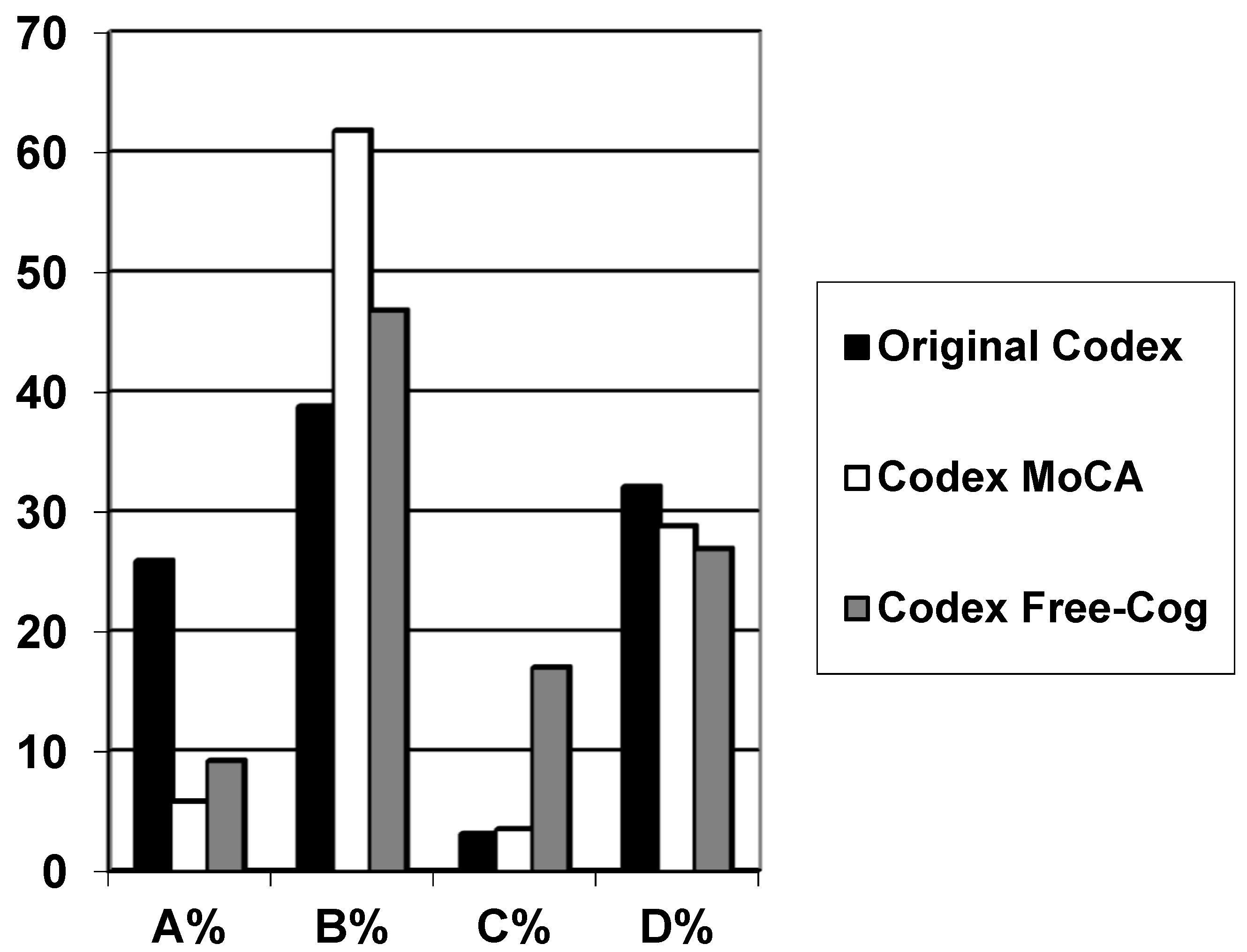
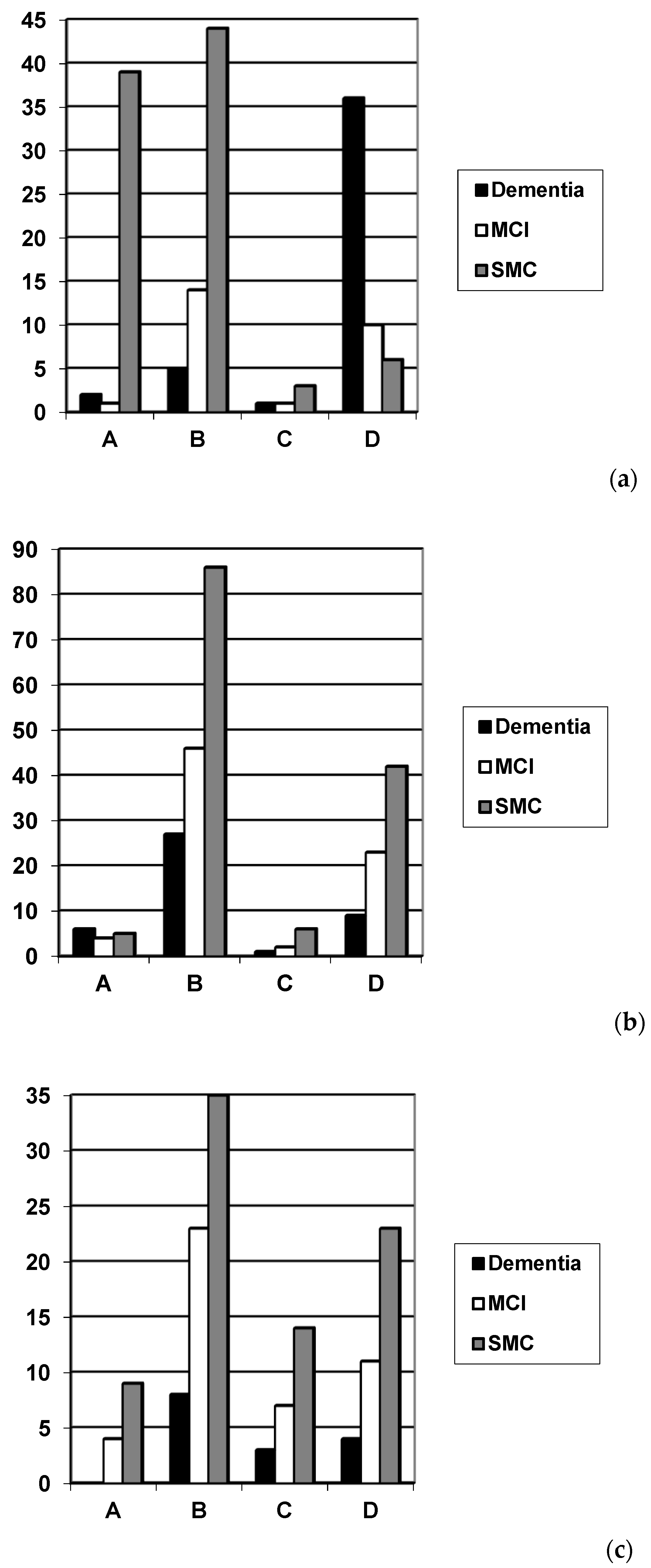
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Belmin, J.; Pariel-Madjlessi, S.; Surun, P.; Bentot, C.; Feteanu, D.; Lefebvre des Noettes, V.; Onen, F.; Drunat, O.; Trivalle, C.; Chassagne, P.; et al. The cognitive disorders examination (Codex) is a reliable 3-minute test for detection of dementia in the elderly (validation study in 323 subjects). Presse Med. 2007, 36, 1183–1190. [Google Scholar] [CrossRef] [PubMed]
- Belmin, J.; Oasi, C.; Folio, P.; Pariel-Madjlessi, S. Codex, un test ultra-rapide pour le repérage des démences chez les sujets âgés. Revue Geriatr. 2007, 32, 627–631. [Google Scholar]
- Folstein, M.F.; Folstein, S.E.; McHugh, P.R. “Mini-Mental State.” A practical method for grading the cognitive state of patients for the clinician. J. Psychiatr. Res. 1975, 12, 189–198. [Google Scholar] [CrossRef]
- Larner, A.J. Codex (cognitive disorders examination) for the detection of dementia and mild cognitive impairment. Codex pour la détection de la démence et du mild cognitive impairment. Presse Med. 2013, 42, e425–e428. [Google Scholar] [CrossRef] [PubMed]
- Ziso, B.; Larner, A.J. Codex (cognitive disorders examination) for the detection of dementia and mild cognitive impairment: Diagnostic utility. J. Neurol. Neurosurg. Psychiatry 2013, 84, e2. [Google Scholar] [CrossRef]
- Larner, A.J. Dementia in Clinical Practice: A Neurological Perspective. Pragmatic Studies in the Cognitive Function Clinic, 3rd ed.; Springer: London, UK, 2018; pp. 89–90. [Google Scholar]
- Avgerinou, C.; Koufogianni, K.; Solini-Kosti, E.; Belmin, J. Validation of the Greek translation of the Cognitive Disorders Examination (Codex) for the detection of dementia in primary care. Ann. Hellenic Med. 2017, 34, 334–342. [Google Scholar]
- Mézière, A.; Paillaud, E.; Belmin, J.; Pariel, S.; Herbaud, S.; Canouï-Poitrine, F.; Le Thuautd, A.; Martyce, J.; Plaud, B. Delirium in older people after proximal femoral fracture repair: role of a preoperative screening cognitive test. Ann. Fr. Anesth. Reanim. 2013, 32, e91–e96. [Google Scholar] [CrossRef]
- Ambert-Dahan, E.; Routier, S.; Marot, L.; Bouccara, D.; Sterkers, O.; Ferrary, E.; Mosnier, I. Cognitive evaluation of cochlear implanted adults using CODEX and MoCA screening tests. Otol. Neurotol. 2017, 38, e282–e284. [Google Scholar] [CrossRef] [PubMed]
- Vannier-Nitenberg, C.; Dauphinot, V.; Bongue, B.; Sass, C.; Rouch, I.; Beuachet, O.; Krolak-Salmon, P.; Fantino, B. Early detection of memory impairment in people over 65 years old consulting at Health Examination Centers for the French health insurance: the EVATEM protocol. BMC Geriatr. 2013, 13, 55. [Google Scholar] [CrossRef]
- Vannier-Nitenberg, C.; Dauphinot, V.; Bongue, B.; Sass, C.; Bathsavanis, A.; Rouch, I.; Deville, N.; Beauchet, O.; Krolak-Salmon, P.; Fantino, B. Performance of cognitive tests, individually and combined, for the detection of cognitive disorders amongst community-dwelling elderly people with memory complaints: The EVATEM study. Eur. J. Neurol. 2016, 23, 554–561. [Google Scholar] [CrossRef]
- Nasreddine, Z.S.; Phillips, N.A.; Bédirian, V.; Charbonneau, S.; Whitehead, V.; Collin, I.; Cummings, J.L.; Chertkow, H. The Montreal Cognitive Assessment, MoCA: A brief screening tool for mild cognitive impairment. J. Am. Geriatr. Soc. 2005, 53, 695–699. [Google Scholar] [CrossRef]
- Larner, A.J. Comparing diagnostic accuracy of cognitive screening instruments: A weighted comparison approach. Dement. Geriatr. Cogn. Disord. Extra 2013, 3, 60–65. [Google Scholar] [CrossRef] [PubMed]
- Larner, A.J. MACE versus MoCA: equivalence or superiority? Pragmatic diagnostic test accuracy study. Int. Psychogeriatr. 2017, 29, 931–937. [Google Scholar] [CrossRef] [PubMed]
- Larner, A.J. Free-Cog: Pragmatic test accuracy study. Dement. Geriatr. Cogn. Disord. 2019, 48. accepted. [Google Scholar]
- Winblad, B.; Palmer, K.; Kivipelto, M.; Jelic, V.; Fratiglioni, L.; Wahlund, L.-O.; Nordberg, A.; Bäckman, L.; Albert, M.; Almkvist, O.; et al. Mild cognitive impairment – beyond controversies, towards a consensus: report of the International Working Group on Mild Cognitive Impairment. J. Intern. Med. 2004, 256, 240–246. [Google Scholar] [CrossRef] [PubMed]
- Bossuyt, P.M.; Reitsma, J.B.; Bruns, D.E.; Gatsonis, C.A.; Glasziou, P.P.; Irwig, L.M.; Moher, D.; Rennie, D.; de Vet, H.C.W.; Lijmer, J.G. The STARD statement for reporting studies of diagnostic accuracy: explanation and elaboration. Clin. Chem. 2003, 49, 7–18. [Google Scholar] [CrossRef]
- Noel-Storr, A.H.; McCleery, J.M.; Richard, E.; Ritchie, C.W.; Flicker, L.; Cullum, S.J.; Davis, D.; Quinn, T.J.; Hyde, C.; Rutjes, A.W.; et al. Reporting standards for studies of diagnostic test accuracy in dementia: The STARDdem Initiative. Neurology 2014, 83, 364–373. [Google Scholar] [CrossRef] [PubMed]
- Larner, A.J. Evaluating cognitive screening instruments with the “likelihood to be diagnosed or misdiagnosed” measure. Int. J. Clin. Pract. 2019, 73, e13265. [Google Scholar] [CrossRef]
- Albert, M.S.; DeKosky, S.T.; Dickson, D.; Dubois, B.; Feldman, H.H.; Fox, N.C.; Gamst, A.; Holtzman, D.M.; Jagust, W.J.; Petersen, R.C.; et al. The diagnosis of mild cognitive impairment due to Alzheimer’s disease: Recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011, 7, 270–279. [Google Scholar] [CrossRef]
- Kalbe, E.; Kessler, J. DemTect. In Cognitive Screening Instruments. A Practical Approach, 2nd ed.; Larner, A.J., Ed.; Springer: London, UK, 2017; pp. 197–208. [Google Scholar]
- Pellegrini, E.; Ballerini, L.; Hernandez, M.D.C.V.; Chappell, F.M.; Gonzalez-Castro, V.; Anblagan, D.; Danso, S.; Muñoz-Maniega, S.; Job, D.; Pernet, C.; et al. Machine learning of neuroimaging for assisted diagnosis of cognitive impairment and dementia: A systematic review. Alzheimers Dement. (Amst) 2018, 10, 519–535. [Google Scholar] [CrossRef]
- Chiu, P.Y.; Tang, H.; Wei, C.Y.; Zhang, C.; Hung, G.U.; Zhou, W. NMD-12: A new machine-learning derived screening instrument to detect mild cognitive impairment and dementia. PLoS ONE 2019, 14, e0213430. [Google Scholar] [CrossRef] [PubMed]
- Larner, A.J. Performance-based cognitive screening instruments: an extended analysis of the time versus accuracy trade-off. Diagnostics (Basel) 2015, 5, 504–512. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, S.; McGrory, S.; Leslie, F.; Dawson, K.; Ahmed, S.; Butler, C.R.; Rowe, J.B.; Mioshi, E.; Hodges, J.R. The Mini-Addenbrooke’s Cognitive Examination: A new assessment tool for dementia. Dement. Geriatr. Cogn. Disord. 2015, 39, 1–11. [Google Scholar] [CrossRef] [PubMed]
- O’Caoimh, R.; Gao, Y.; McGlade, C.; Henry, L.; Gallagher, P.; Timmons, S.; Molloy, D.W. Comparison of the quick mild cognitive impairment (Qmci) screen and the SMMSE in screening for mild cognitive impairment. Age Ageing 2012, 41, 624–629. [Google Scholar] [CrossRef] [PubMed]
| Codex | N | Gender F:M (% Female) | Age Range (Median) | Diagnosis Dementia/MCI/SMC (%) | Codex Category | |||
|---|---|---|---|---|---|---|---|---|
| A (%) | B (%) | C (%) | D (%) | |||||
| Original | 162 | 79:83 (49) | 20–89 (61) | 44/26/92 (27/16/57) | 42 (25.9) | 63 (38.8) | 5 (3.1) | 52 (32.1) |
| Modified from MoCA | 257 | 116:141 (45) | 22–89 (59) | 43/75/139 (17/29/54) | 15 (5.8) | 159 (61.8) | 9 (3.5) | 74 (28.8) |
| Modified from Free-Cog | 141 | 61:80 (43) | 28–88 (62) | 15/45/81 (11/32/57) | 13 (9.2) | 66 (46.8) | 24 (17.0) | 38 (26.9) |
| Diagnosis of Dementia vs. No Dementia (MCI + SMC) | Diagnosis of Dementia vs. MCI | Diagnosis of MCI vs. No Cognitive Impairment (SMC) | |
|---|---|---|---|
| N | 162 (44 vs. 118) | 70 (44 vs. 26) | 118 (26 vs. 92) |
| Prevalence (P = pre-test probability) | Dementia 0.27 | Dementia 0.63 | MCI 0.22 |
| Pre-test odds (= P/1 − P) | Dementia 0.37 | Dementia 1.69 | MCI 0.28 |
| Sensitivity (Se) | 0.84 (0.73–0.95) | 0.84 (0.73–0.95) | 0.42 (0.23–0.61) |
| Specificity (Sp) | 0.83 (0.76–0.90) | 0.58 (0.39–0.77) | 0.90 (0.84–0.96) |
| Y | 0.67 | 0.42 | 0.32 |
| PPV (= post-test probability) | 0.65 (0.53–0.77) | 0.77 (0.65–0.89) | 0.55 (0.33–0.77) |
| NPV | 0.93 (0.89–0.98) | 0.68 (0.49–0.88) | 0.85 (0.78–0.92) |
| PSI | 0.58 | 0.45 | 0.40 |
| Accuracy (Acc) | 0.83 (0.78–0.89) | 0.74 (0.64–0.85) | 0.80 (0.72–0.87) |
| Net Reclassification Improvement (NRI = Acc − P) | 0.56 | 0.11 | 0.58 |
| LDM (= NNM/NND, NNM/NNP) | 4.02, 3.48 | 1.63, 1.75 | 1.57, 1.97 |
| LR+ | 4.96 (3.29–7.49) = moderate | 1.99 (1.25–3.17) = slight | 4.32 (2.01–9.30) = moderate |
| LR− | 0.19 (0.13–0.29) = large | 0.28 (0.17–0.44) = moderate | 0.64 (0.30–1.38) = slight |
| DOR | 25.9 (17.2–39.1) | 7.21 (4.52–11.5) | 6.76 (3.14–14.5) |
| Post-test odds (= pre-test odds × LR+) | Dementia 1.85 | Dementia 3.36 | MCI 1.21 |
| CUI+ (= Se × PPV) | 0.55 = adequate | 0.65 = good | 0.23 = very poor |
| CUI− (= Sp × NPV) | 0.78 = good | 0.39 = poor | 0.76 = good |
| Diagnosis of Dementia vs. No Dementia (MCI + SMC) | Diagnosis of Dementia vs. MCI | Diagnosis of MCI vs. No Cognitive Impairment (SMC) | |
|---|---|---|---|
| N | 257 (43 vs. 214) | 118 (43 vs. 75) | 214 (75 vs. 139) |
| Prevalence (P = pre-test probability) | Dementia 0.17 | Dementia 0.36 | MCI 0.35 |
| Pre-test odds (= P/1 − P) | Dementia 0.20 | Dementia 0.57 | MCI 0.54 |
| Sensitivity (Se) | 0.23 (0.11–0.36) | 0.23 (0.11–0.36) | 0.33 (0.23–0.44) |
| Specificity (Sp) | 0.66 (0.60–0.72) | 0.67 (0.56–0.77) | 0.65 (0.58–0.73) |
| Y | −0.11 | −0.10 | −0.02 |
| PPV (= post-test probability) | 0.12 (0.05–0.19) | 0.29 (0.14–0.44) | 0.34 (0.23–0.45) |
| NPV | 0.81 (0.75–0.87) | 0.60 (0.50–0.71) | 0.65 (0.57–0.72) |
| PSI | −0.07 | −0.11 | −0.01 |
| Accuracy (Acc) | 0.59 (0.53–0.65) | 0.51 (0.42–0.60) | 0.54 (0.48–0.61) |
| Net Reclassification Improvement (NRI = Acc − P) | 0.42 | 0.15 | 0.19 |
| LDM (= NNM/NND, NNM/NNP) | −0.27, −0.17 | −0.20, −0.22 | −0.04, −0.02 |
| LR+ | 0.68 (0.38–1.21) = slight | 0.70 (0.37–1.31) = slight | 0.97 (0.65–1.43) = slight |
| LR− | 1.16 (0.66–2.07) = slight | 1.15 (0.61–2.16) = slight | 1.02 (0.69–1.51) = slight |
| DOR | 0.59 (0.33–1.04) | 0.61 (0.32–1.14) | 0.95 (0.64–1.40) |
| Post-test odds (= pre-test odds × LR+) | Dementia 0.14 | Dementia 0.40 | MCI 0.52 |
| CUI+ (= Se × PPV) | 0.03 = very poor | 0.07 = very poor | 0.11 = very poor |
| CUI− (= Sp × NPV) | 0.53 = adequate | 0.40 = poor | 0.42 = poor |
| Diagnosis of Dementia vs. No Dementia (MCI + SMC) | Diagnosis of Dementia vs. MCI | Diagnosis of MCI vs. No Cognitive Impairment (SMC) | |
|---|---|---|---|
| N | 141 (15 vs. 126) | 60 (15 vs. 45) | 126 (45 vs. 81) |
| Prevalence (P = pre-test probability) | Dementia 0.11 | Dementia 0.25 | MCI 0.36 |
| Pre-test odds (= P/1 − P) | Dementia 0.12 | Dementia 0.33 | MCI 0.56 |
| Sensitivity (Se) | 0.47 (0.21–0.72) | 0.47 (0.21–0.72) | 0.40 (0.26–0.54) |
| Specificity (Sp) | 0.56 (0.48–0.65) | 0.60 (0.47–0.74) | 0.54 (0.43–0.65) |
| Y | 0.03 | 0.07 | −0.06 |
| PPV (= post-test probability) | 0.11 (0.03–0.19) | 0.28 (0.10–0.46) | 0.33 (0.20–0.45) |
| NPV | 0.90 (0.83–0.97) | 0.77 (0.63–0.91) | 0.62 (0.51–0.73) |
| PSI | 0.01 | 0.05 | −0.05 |
| Accuracy (Acc) | 0.55 (0.47–0.64) | 0.57 (0.44–0.69) | 0.49 (0.40–0.58) |
| Net Reclassification Improvement (NRI = Acc − P) | 0.44 | 0.32 | 0.13 |
| LDM (= NNM/NND, NNM/NNP) | 0.07, 0.02 | 0.63, 0.12 | −0.12, −0.10 |
| LR+ | 1.07 (0.60–1.91) = slight | 1.17 (0.61–2.23) = slight | 0.88 (0.57–1.35) = slight |
| LR− | 0.95 (0.53–1.68) = slight | 0.89 (0.46–1.70) = slight | 1.10 (0.72–1.70) = slight |
| DOR | 1.13 (0.63–2.01) | 1.31 (0.69–2.51) | 0.79 (0.52–1.22) |
| Post-test odds (= pre-test odds × LR+) | Dementia 0.13 | Dementia 0.38 | MCI 0.49 |
| CUI+ (= Se × PPV) | 0.05 = very poor | 0.13 = very poor | 0.13 = very poor |
| CUI− (= Sp × NPV) | 0.51 = adequate | 0.46 = poor | 0.34 = very poor |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ziso, B.; Larner, A.J. Codex (Cognitive Disorders Examination) Decision Tree Modified for the Detection of Dementia and MCI. Diagnostics 2019, 9, 58. https://doi.org/10.3390/diagnostics9020058
Ziso B, Larner AJ. Codex (Cognitive Disorders Examination) Decision Tree Modified for the Detection of Dementia and MCI. Diagnostics. 2019; 9(2):58. https://doi.org/10.3390/diagnostics9020058
Chicago/Turabian StyleZiso, Besa, and Andrew J. Larner. 2019. "Codex (Cognitive Disorders Examination) Decision Tree Modified for the Detection of Dementia and MCI" Diagnostics 9, no. 2: 58. https://doi.org/10.3390/diagnostics9020058
APA StyleZiso, B., & Larner, A. J. (2019). Codex (Cognitive Disorders Examination) Decision Tree Modified for the Detection of Dementia and MCI. Diagnostics, 9(2), 58. https://doi.org/10.3390/diagnostics9020058




