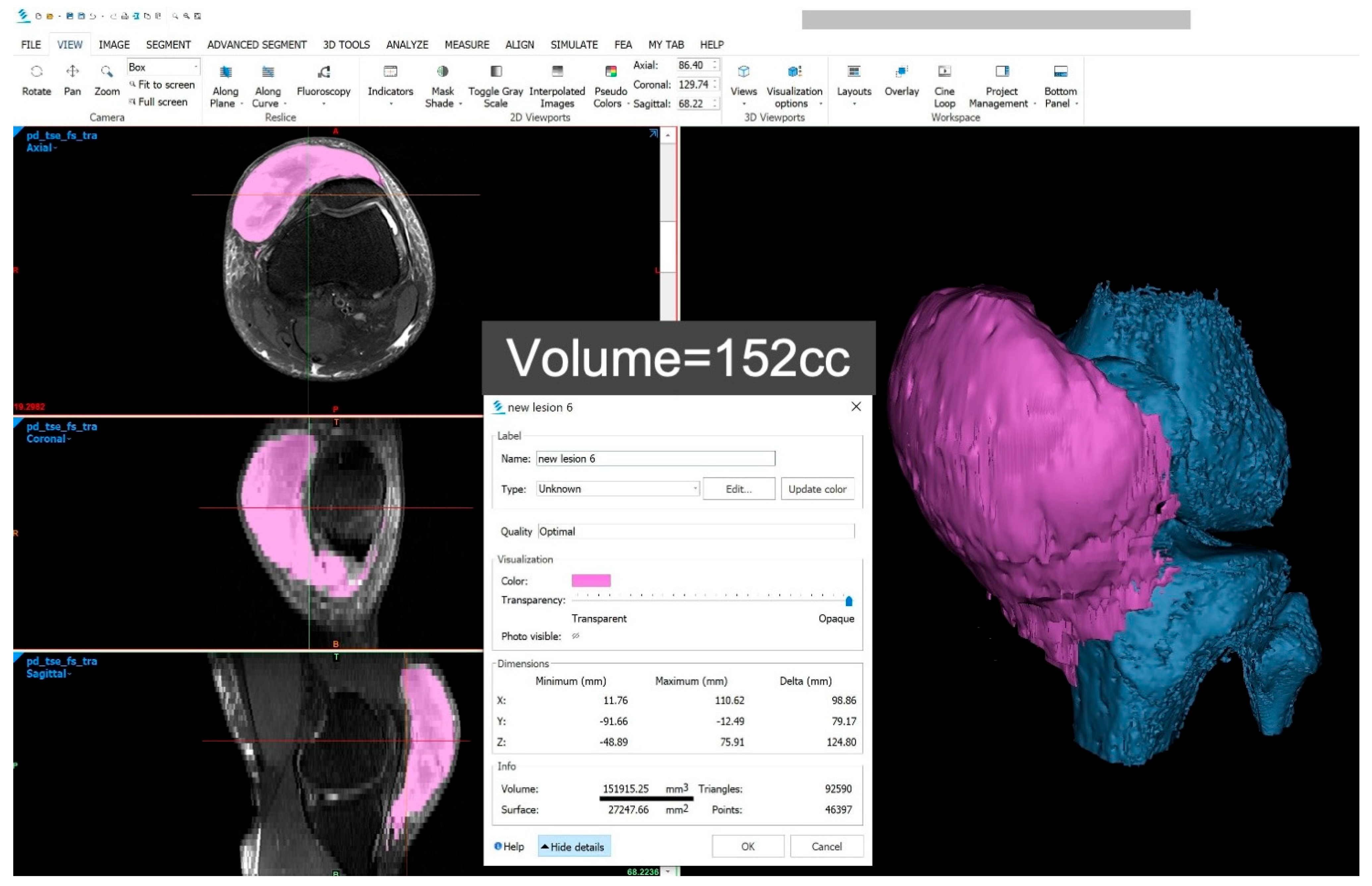
Sonographic Diagnosis and Follow-Up of a Rare Large Pre-Patellar Morel-Lavallée Lesion
Abstract





Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Letournel, E.; Judet, R. (Eds.) Fractures of the Acetabulum, 2nd ed.; Springer: Berlin/Heidelberg, Germany, 1993. [Google Scholar]
- Shen, C.; Peng, J.P.; Chen, X.D. Efficacy of treatment in peri-pelvic Morel-Lavallee lesion: A systematic review of the literature. Arch. Orthop. Trauma. Surg. 2013, 133, 635–640. [Google Scholar] [CrossRef] [PubMed]
- Scolaro, J.A.; Chao, T.; Zamorano, D.P. The Morel-Lavallee Lesion: Diagnosis and Management. J. Am. Acad. Orthop. Surg. 2016, 24, 667–672. [Google Scholar] [CrossRef] [PubMed]
- Borrero, C.G.; Maxwell, N.; Kavanagh, E. MRI findings of prepatellar Morel-Lavallee effusions. Skeletal Radiol. 2008, 37, 451–455. [Google Scholar] [CrossRef] [PubMed]
- Bonilla-Yoon, I.; Masih, S.; Patel, D.B.; White, E.A.; Levine, B.D.; Chow, K.; Gottsegen, C.J.; Matcuk, G.R., Jr. The Morel-Lavallee lesion: Pathophysiology, clinical presentation, imaging features, and treatment options. Emerg. Radiol. 2014, 21, 35–43. [Google Scholar] [CrossRef]
- Vanhegan, I.S.; Dala-Ali, B.; Verhelst, L.; Mallucci, P.; Haddad, F.S. The morel-lavallee lesion as a rare differential diagnosis for recalcitrant bursitis of the knee: Case report and literature review. Case Rep. Orthop. 2012, 2012, 593193. [Google Scholar] [CrossRef] [PubMed]
- Caglayan, G.; Ozcakar, L.; Kaymak, S.U.; Kaymak, B.; Tan, A.A. Effects of Sono-feedback during aspiration of Baker’s cysts: A controlled clinical trial. J. Rehabil. Med. 2016, 48, 386–389. [Google Scholar] [CrossRef]
- Wu, W.T.; Onishi, K.; Mezian, K.; Nanka, O.; Wang, B.; Su, D.C.; Ricci, V.; Chang, K.V.; Ozcakar, L. Ultrasound imaging of the posterior lateral corner of the knee: A pictorial review of anatomy and pathologies. Insights Imaging 2024, 15, 39. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Siu, P.K.-T.; Wu, W.-T.; Özçakar, L.; Chang, K.-V. Sonographic Diagnosis and Follow-Up of a Rare Large Pre-Patellar Morel-Lavallée Lesion. Diagnostics 2025, 15, 883. https://doi.org/10.3390/diagnostics15070883
Siu PK-T, Wu W-T, Özçakar L, Chang K-V. Sonographic Diagnosis and Follow-Up of a Rare Large Pre-Patellar Morel-Lavallée Lesion. Diagnostics. 2025; 15(7):883. https://doi.org/10.3390/diagnostics15070883
Chicago/Turabian StyleSiu, Peter Kam-To, Wei-Ting Wu, Levent Özçakar, and Ke-Vin Chang. 2025. "Sonographic Diagnosis and Follow-Up of a Rare Large Pre-Patellar Morel-Lavallée Lesion" Diagnostics 15, no. 7: 883. https://doi.org/10.3390/diagnostics15070883
APA StyleSiu, P. K.-T., Wu, W.-T., Özçakar, L., & Chang, K.-V. (2025). Sonographic Diagnosis and Follow-Up of a Rare Large Pre-Patellar Morel-Lavallée Lesion. Diagnostics, 15(7), 883. https://doi.org/10.3390/diagnostics15070883









