Nasolacrimal Canal Topography in Relation to the Maxillary Position: CBCT Insights into Le Fort Osteotomy and Fixation Safety
Abstract
1. Introduction
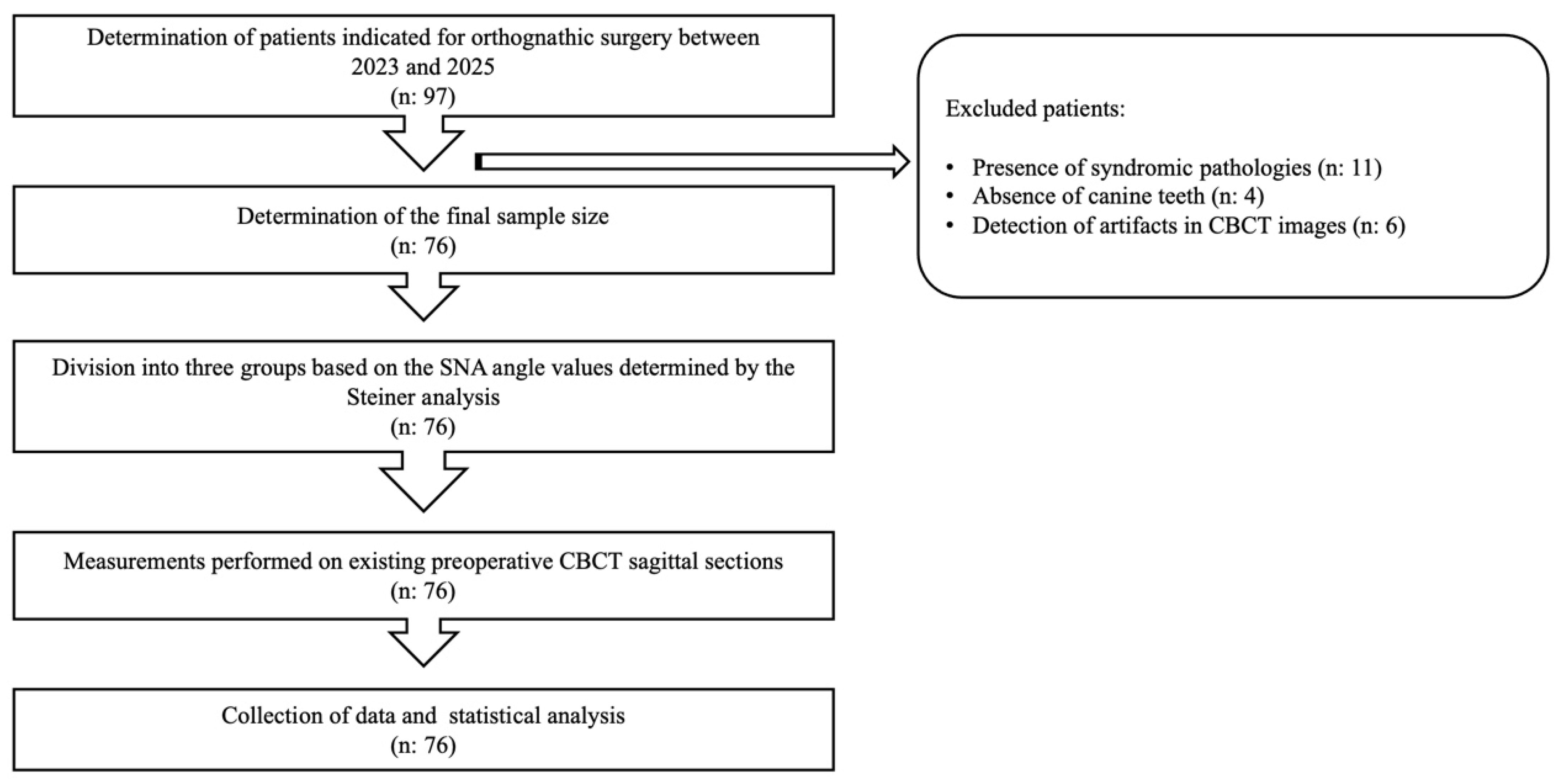
2. Materials and Methods
2.1. Study Design and Ethics Approval
2.2. The Study Sample
- Group 1 (retrognathic maxilla): 30 individuals—60 lacrimal canals
- Group 2 (orthognathic maxilla): 22 individuals—44 lacrimal canals
- Group 3 (prognathic maxilla): 24 individuals—48 lacrimal canals
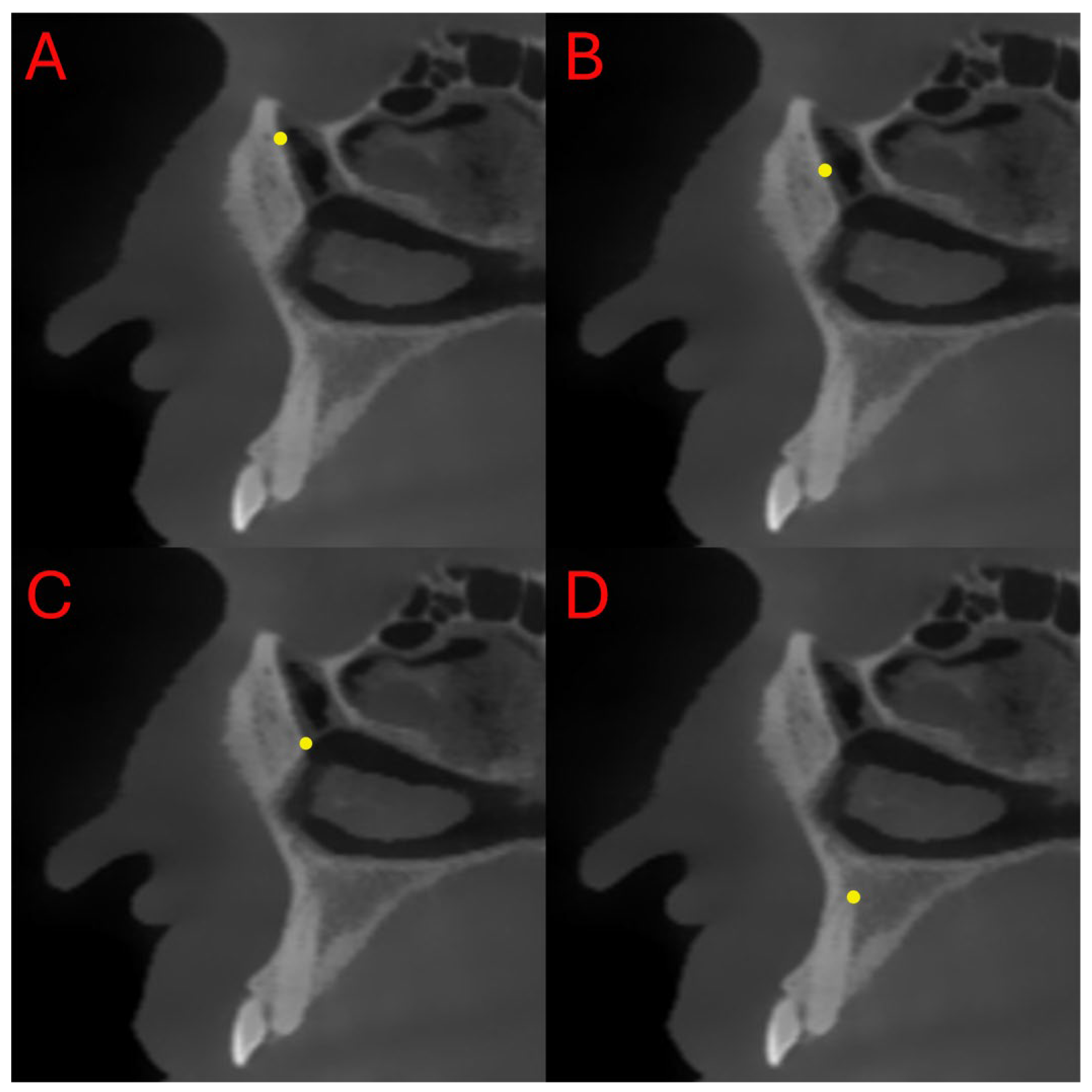
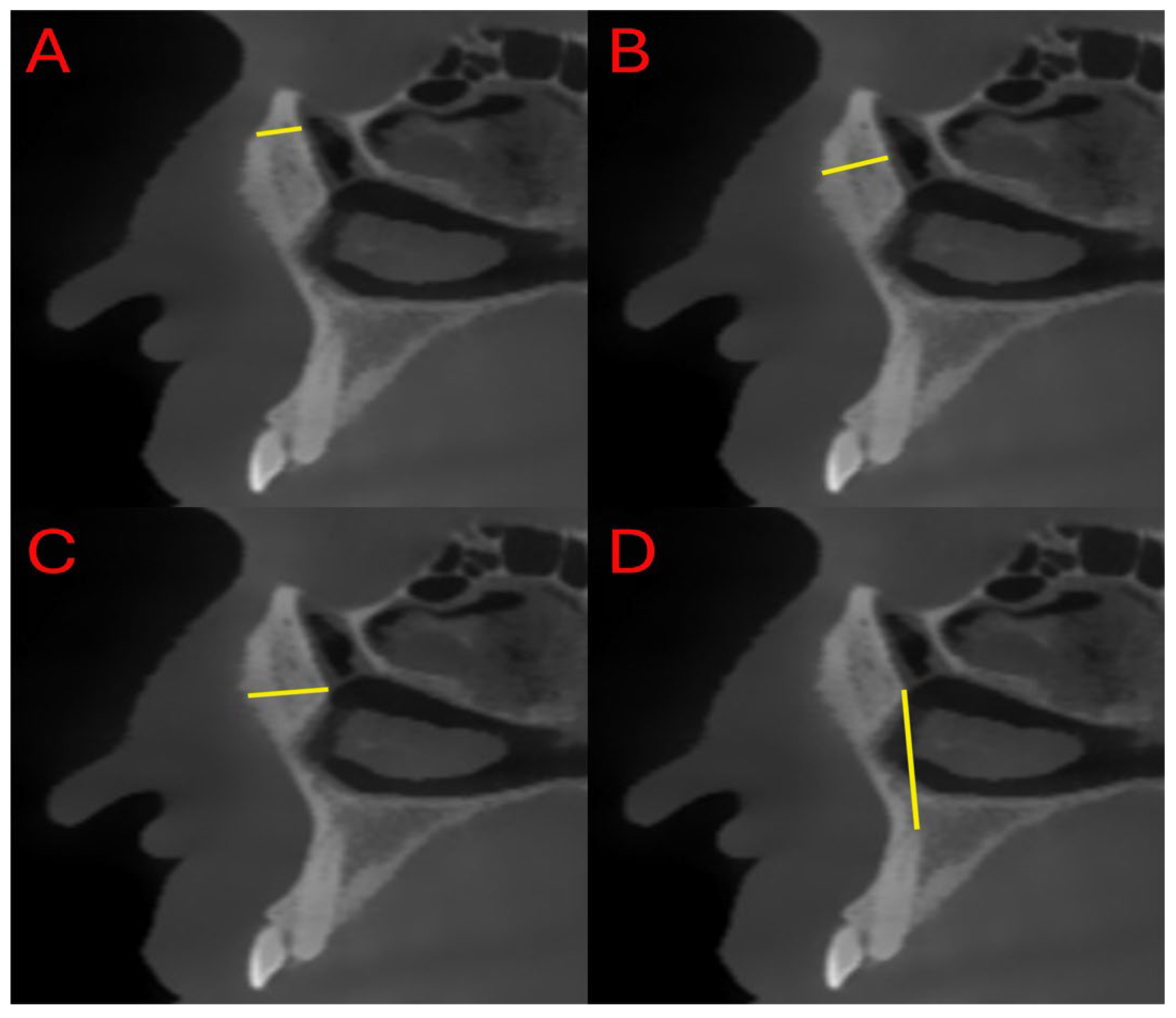
2.3. Measurements
- Distance between the superior ostium (S) of the nasolacrimal canal and the anterior maxillary border (SL)
- Distance between the middle point (M) of the nasolacrimal canal and the anterior maxillary border (ML)
- Distance between the inferior ostium (I) of the nasolacrimal canal and the anterior maxillary border (IL)
- Distance between the canine apex (C) and the inferior ostium (I) of the nasolacrimal canal (IC)
2.4. Measurement Repeatability and Reliability
2.5. Imaging Protocol
2.6. Statistical Analysis
3. Results
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ALARA | As low as possible achievable |
| ANOVA | Analysis of variance |
| CBCT | Cone-Beam Computed Tomography |
| FOV | Field of view |
| ICC | Intraclass correlation coefficient |
| IC | Distance between the canine apex and the inferior ostium of the NLD |
| IL | Distance between the inferior ostium of the NLD and the anterior maxillary border |
| ML | Distance between the middle point of the NLD and the anterior maxillary border |
| NLD | Nasolacrimal duct |
| SD | Standard deviation |
| SL | Distance between the superior ostium of the NLD and the anterior maxillary border |
| SNA | Sella-Nasion-A point angle |
References
- Weiss, R.O.; Ong, A.A.; Reddy, L.V.; Bahmanyar, S.; Vincent, A.G.; Ducic, Y. Orthognathic Surgery-LeFort I Osteotomy. Facial Plast. Surg. 2021, 37, 703–708. [Google Scholar] [CrossRef] [PubMed]
- Pearl, C.; Chubb, D.W.R.; Marchena, J.M.; Waite, P.; Buendia, A.M.; Kau, C.H. Surgery First: Current State of the Art Orthognathic Surgery and Its Potential as a Primary Treatment Modality in Obstructive Sleep Apnea with Concurrent Dentofacial Deformities. Front. Oral Maxillofac. Med. 2022, 4, 29. [Google Scholar] [CrossRef]
- Ozcan, E.M.; Dergin, G.; Basa, S. Prevalence of Nasolacrimal Canal Obstruction and Epiphora Following Maxillary Orthognathic Surgery. Int. J. Oral Maxillofac. Surg. 2018, 47, 715–720. [Google Scholar] [CrossRef] [PubMed]
- Alali, Y.S.; Aldokhi, H.D.; Alayoub, R.A.; Mohammed, W.A.; Alshehri, S.; Alshayban, M. Assessment of Post-Operative Neurosensory Deficiency Following Le Fort I Maxillary Osteotomy and Its Impact on Patient Satisfaction: A Retrospective Clinical Cross-Sectional Study. J. Clin. Med. 2025, 14, 1115. [Google Scholar] [CrossRef]
- Peltoperä, J.; Kotaniemi, K.V.M.; Suojanen, J.; Stoor, P. Bad Splits in Orthognathic Surgery, Prevention and Management. Curr. Probl. Surg. 2024, 61, 101587. [Google Scholar] [CrossRef]
- Ülker, Ö.; Demirbaş, A.E.; Kütük, N.; Kılıç, E.; Alkan, A. Causes of Ortognatic Surgery Complications and Comparison of the Literature: Retrospective Cohort Research. Turk. Klin. J. Dent. Sci. 2023, 29, 15–21. [Google Scholar] [CrossRef]
- Kaba, Y.N.; Demirbas, A.E.; Topan, C.; Yılmaz-Asan, C.; Ersu, N. The Evaluation of Nasolacrimal Duct Injury in Le Fort I Osteotomy Patients. Med. Oral Patol. Oral Cir. Bucal 2023, 29, e187. [Google Scholar] [CrossRef]
- Chow, L.K.; Singh, B.; Chiu, W.K.; Samman, N. Prevalence of Postoperative Complications After Orthognathic Surgery: A 15-Year Review. J. Oral Maxillofac. Surg. 2007, 65, 984–992. [Google Scholar] [CrossRef]
- Steel, B.J.; Cope, M.R. Unusual and Rare Complications of Orthognathic Surgery: A Literature Review. J. Oral Maxillofac. Surg. 2012, 70, 1678–1691. [Google Scholar] [CrossRef]
- Humber, C.C.; Lanigan, D.T.; Hohn, F.I. Retrograde Hemorrhage (Hemolacria) from the Lacrimal Puncta after a Le Fort i Osteotomy: A Report of 2 Cases and a Review of the Literature. J. Oral Maxillofac. Surg. 2011, 69, 520–527. [Google Scholar] [CrossRef]
- Chrcanovic, B.R.; Nunes, F.C.F.; Freire-Maia, B. Bloody Tears after Miniplate Osteosynthesis for Le Fort I Osteotomy. J. Oral Maxillofac. Surg. Med. Pathol. 2013, 25, 32–34. [Google Scholar] [CrossRef]
- Ali, M.J. Etiopathogenesis of Primary Acquired Nasolacrimal Duct Obstruction (PANDO). Prog. Retin. Eye Res. 2023, 96, 101193. [Google Scholar] [CrossRef] [PubMed]
- Findik, H.; Uzun, F.; Kaim, M.; Birinci, M.; Çeliker, M.; Okutucu, M.; Aslan, M.G. The Impact of Systemic Inflammation on Recurrence in Patients with Congenital Nasolacrimal Duct Obstruction. J. Clin. Med. 2024, 13, 6834. [Google Scholar] [CrossRef] [PubMed]
- Avrămuț, R.-P.; Stăncioiu, A.-A.; Talpos, S.; Motofelea, A.C.; Popa, M.; Szuhanek, C. Quantitative Evaluation of Skeletal, Dental, and Soft Tissue Changes After Orthognathic Surgery: A Cephalometric and Statistical Analysis. J. Clin. Med. 2025, 14, 7336. [Google Scholar] [CrossRef]
- Ghodasra, R.; Brizuela, M. Orthodontics, Cephalometric Analysis; StatPearls: Treasure Island, FL, USA, 2023. [Google Scholar]
- Nguyen, T.K. A Systematic Review of Cephalometric Normative Data in Children. Master’s Thesis, McGill University, Montreal, QC, Canada, 2022. [Google Scholar]
- Kundi, I.; Kumar, H.; Alam, M.K. Determination of Craniofacial Morphometry of Saudi Adults by Steiner’s Analysis. J. Clin. Diagn. Res. 2019, 13, ZC45–ZC48. [Google Scholar] [CrossRef]
- Jang, S.Y.; Kim, M.K.; Choi, S.M.; Jang, J.W. Nasolacrimal Duct Obstruction after Maxillary Orthognathic Surgery. J. Oral. Maxillofac. Surg. 2013, 71, 1085–1098. [Google Scholar] [CrossRef]
- Helal, M.S.; Gaber, R.M.; El-Kassaby, M. A Rare Complication of Hemolacria after Le Fort I Osteotomy: A Case Presentation. Maxillofac. Plast. Reconstr. Surg. 2022, 44, 29. [Google Scholar] [CrossRef]
- Agarwal, A.; Naik, M.; Ali, M.J.; Bothra, N. The Role of CT-DCG in Hardware—Associated Secondary Acquired Lacrimal Duct Obstruction: SALDO Update Study—(SUP)—Paper III. Am. J. Ophthalmol. Case Rep. 2024, 34, 102026. [Google Scholar] [CrossRef]
- Canlı, A.; Vatansever, A.; Akay, E. Morphometric Relationship of Nasolacrimal Duct with Maxillary Sinus and Nasal Septum. Anatomy 2022, 16, 69–75. [Google Scholar] [CrossRef]
- Almashity, S.; Karwad, M.; Araibi1, O.; Alfitorey, A.; Algadi, A.; Karwad, M.A. Morphometric Evaluation of Bony Nasolacrimal Canal in Libyan Adults in Benghazi Using CT Scan. Libyan J. Med. Res. 2025, 19, 69–76. [Google Scholar] [CrossRef]
- Razavi, M.; Shams, N.; Afshari, F.; Nanai, S. Investigating the Morphology of the Nasolacrimal Canal in Cone Beam Computed Tomography Images and Its Relationship with Age and Gender. Maedica 2024, 19, 303–311. [Google Scholar] [CrossRef]
- Shoshani, Y.; Samet, N.; Ardekian, L.; Taicher, S. Nasolacrimal Duct Injury after Le Fort I Osteotomy. J. Oral Maxillofac. Surg. 1994, 52, 406–407. [Google Scholar] [CrossRef]
- Keller, E.E.; Sather, A.H. Quadrangular Le Fort I Osteotomy: Surgical Technique and Review of 54 Patients. J. Oral Maxillofac. Surg. 1990, 48, 2–11. [Google Scholar] [CrossRef]
- Freihofer, H.P.M.; Brouns, J.J.A. Midfacial Movements A Reappraisal. Oral Maxillofac. Surg. Clin. N. Am. 1990, 2, 761–773. [Google Scholar] [CrossRef]
- Dabir, A.; Vahanwala, J. Orthognathic Surgery for the Maxilla-LeFort I and Anterior Maxillary Osteotomy. In Oral and Maxillofacial Surgery for the Clinician; Springer: Berlin/Heidelberg, Germany, 2021; pp. 1513–1548. [Google Scholar] [CrossRef]
- Buchanan, E.P.; Hyman, C.H. LeFort I Osteotomy. Semin. Plast. Surg. 2013, 27, 149–154. [Google Scholar] [CrossRef]
- You, Z.H.; Bell, W.H.; Finn, R.A. Location of the Nasolacrimal Canal in Relation to the High Le Fort I Osteotomy. J. Oral Maxillofac. Surg. 1992, 50, 1075–1080. [Google Scholar] [CrossRef] [PubMed]
- Shimoa, T.; Nishiyamaa, A.; Jinno, T.; Sasakr, A. Severe Gummy Smile with Class II Malocclusion Treated with LeFort I Osteotomy Combined with Horseshoe Osteotomy and Intraoral Vertical Ramus Osteotomy. Acta Med. Okayama 2013, 67, 55–60. [Google Scholar] [CrossRef]
- Anehosur, V.; Joshi, A.; Nathani, J.; Suresh, A. Modification of LeFort I Osteotomy for Severe Maxillary Vertical Excess Asymmetry. Br. J. Oral Maxillofac. Surg. 2019, 57, 374–377. [Google Scholar] [CrossRef] [PubMed]
| Group | Chi-Square Test | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Retrognathic | Orthognathic | Prognathic | Total | χ2 | p | ||||||
| n | % | n | % | n | % | n | % | ||||
| Sex | Female | 38 | 63.3 | 30 | 68.2 | 18 | 37.5 | 86 | 56.6 | 10.6 | 0.005 |
| Male | 22 | 36.7 | 14 | 31.8 | 30 | 62.5 | 66 | 43.4 | |||
| Total | 60 | 100.0 | 44 | 100.0 | 48 | 100.0 | 152 | 100.0 | |||
| Group | Kruskal–Wallis H Test | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Mean | Median | Minimum | Maximum | SD | Mean Rank | H | p | Post Hoc | ||
| Age | Retrognathic | 60 | 27.77 | 26 | 15 | 55 | 8.30 | 83.23 | 6.7 | 0.054 | - |
| Orthognathic | 44 | 24.00 | 25 | 18 | 34 | 3.92 | 62.05 | ||||
| Prognathic | 48 | 26.63 | 26 | 18 | 37 | 5.52 | 81.33 | ||||
| Group | Kruskal–Wallis H Test | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Mean | Median | Minimum | Maximum | SD | Mean Rank | H | p | Post Hoc | ||
| SL | Retrognathic | 60 | 3.91 | 3.83 | 2.36 | 5.79 | 0.75 | 84.95 | 5.5 | 0.063 | - |
| Orthognathic | 44 | 3.63 | 3.51 | 2.75 | 5.33 | 0.56 | 64.40 | ||||
| Prognathic | 48 | 3.76 | 3.69 | 2.75 | 4.84 | 0.52 | 77.03 | ||||
| Group | One-Way ANOVA | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| n | Mean | Minimum | Maximum | SD | F | p | Post Hoc | ||
| ML | Retrognathic | 60 | 5.42 | 3.23 | 8.61 | 1.34 | 9.09 | 0.0001 | 3-1 3-2 |
| Orthognathic | 44 | 5.83 | 3.84 | 7.34 | 0.81 | ||||
| Prognathic | 48 | 6.26 | 4.87 | 8.17 | 0.62 | ||||
| IL | Retrognathic | 60 | 5.92 | 3.37 | 8.73 | 1.12 | 14.3 | 0.0001 | 1-2 1-3 |
| Orthognathic | 44 | 6.58 | 4.66 | 8.18 | 0.94 | ||||
| Prognathic | 48 | 6.91 | 5.17 | 8.69 | 0.80 | ||||
| IC | Retrognathic | 60 | 19.68 | 13.86 | 24.27 | 2.31 | 1.98 | 0.141 | - |
| Orthognathic | 44 | 19.99 | 15.48 | 26.02 | 2.74 | ||||
| Prognathic | 48 | 20.64 | 15.16 | 25.91 | 2.50 | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yurttutan, M.E.; Kadıoğlu, M.B.; Yıldız, M.; Kocamaz, Ö.F.; Durmaz, M.; Eriş, M.A.; Kamal, A. Nasolacrimal Canal Topography in Relation to the Maxillary Position: CBCT Insights into Le Fort Osteotomy and Fixation Safety. Diagnostics 2025, 15, 3008. https://doi.org/10.3390/diagnostics15233008
Yurttutan ME, Kadıoğlu MB, Yıldız M, Kocamaz ÖF, Durmaz M, Eriş MA, Kamal A. Nasolacrimal Canal Topography in Relation to the Maxillary Position: CBCT Insights into Le Fort Osteotomy and Fixation Safety. Diagnostics. 2025; 15(23):3008. https://doi.org/10.3390/diagnostics15233008
Chicago/Turabian StyleYurttutan, Mehmet Emre, Merve Berika Kadıoğlu, Mahzun Yıldız, Ömer Faruk Kocamaz, Meyra Durmaz, Mehmet Alp Eriş, and Anıl Kamal. 2025. "Nasolacrimal Canal Topography in Relation to the Maxillary Position: CBCT Insights into Le Fort Osteotomy and Fixation Safety" Diagnostics 15, no. 23: 3008. https://doi.org/10.3390/diagnostics15233008
APA StyleYurttutan, M. E., Kadıoğlu, M. B., Yıldız, M., Kocamaz, Ö. F., Durmaz, M., Eriş, M. A., & Kamal, A. (2025). Nasolacrimal Canal Topography in Relation to the Maxillary Position: CBCT Insights into Le Fort Osteotomy and Fixation Safety. Diagnostics, 15(23), 3008. https://doi.org/10.3390/diagnostics15233008







