1. Introduction
Lynch syndrome (LS) is one of the most common hereditary syndromes associated with colorectal cancer (CRC), accounting for 3–4% of all hereditary cancer syndromes [
1]. Individuals with Lynch syndrome not only have an increased risk of developing hereditary nonpolyposis colorectal cancer (HNPCC) but also have a significantly higher risk for a wide spectrum of cancers beyond the colon such as endometrial, ovarian, breast, and urothelial cancers.
Individuals with Lynch syndrome carry a heterozygous hereditary pathogenic or likely pathogenic variant (PV or LPV) in one of the tumor suppressor genes involved in mismatch repair (MMR genes),
MLH1, MSH2, MSH6, PMS2, or
EPCAM, which leads to the loss of one functional copy of these genes [
2]. This condition is inherited in an autosomal dominant manner, meaning that inheriting just one mutated allele is sufficient to increase cancer risk.
Around 90% of LS cases are caused by
MLH1 and
MSH2 gene mutations, while about 10% of LS patients carry
MSH6 and
PMS2 mutations [
3]. Mutations in the
EPCAM gene are extremely rare, occurring in only about 3% of cases [
2].
The mismatch repair (MMR) system is essential for maintaining genomic stability and integrity in the cell [
4]. Patients with LS have a heterozygous hereditary mutation in one of the MMR genes. However, to initiate tumorigenesis, both copies of the gene must be dysfunctional in the tumor cells, meaning a second genetic alteration must occur in the remaining healthy allele, leading to loss of heterozygosity (typically through somatic, acquired changes), resulting in complete loss of MMR protein expression in the tumor.
When MMR is nonfunctional in a cell, accumulation of mutations, particularly in microsatellite regions of DNA, occurs. The accumulation of mismatched bases in microsatellite regions phenotypically results in microsatellite instability (MSI) [
1,
2]. In MMR-deficient tumor cells, the length of microsatellite nucleotide repeats differs from that of the repeats in surrounding healthy tissue [
5]. Therefore, MSI is one of the main molecular characteristics of nonpolyposis CRC within Lynch syndrome. Since over 90% of CRC associated with LS is described as microsatellite-unstable, MSI can be considered a reliable marker of MMR deficiency [
5]. This characteristic is indicated in histopathological findings as MSI-H (high microsatellite instability).
The diagnostics of LS begin with genetic counseling, where individuals at increased risk for cancer are identified based on personal or family history and other characteristic features of hereditary cancer syndromes. Accordingly, they are referred to genetic testing, regular preventive screenings, or preventive pharmacological and/or surgical interventions. Early diagnosis increases the survival rate of affected individuals, as well as probands relatives who undergo testing and surveillance [
2]. Therefore, before and after genetic testing, genetic counseling must occur.
The majority of changes in MMR genes are point mutations, but there are also splice-site mutations and frameshift mutations followed by large genomic rearrangments. Large genomic rearrangements, usually defined as alterations encompassing at least 50 base pairs in length, are called structural variants. Structural variants mostly include large deletions and duplications/insertions, which can produce genomic imbalances called copy number variants (CNVs) [
6]. Due to the presence of different genomic changes in MMR genes, the diagnosis of LS requires a combination of molecular methods that can detect all possible alterations in these genes. This comprehensive approach is critical for accurate diagnosis and effective management of individuals at risk for Lynch syndrome-related cancers.
Compared to traditional molecular methods, NGS is faster, broader, and more cost-effective. It can be used for singlegenes, targeted multi-gene panels, whole exomes, or even whole genomes, giving complete genetic information but keeping costs controllable. In oncology, NGS multi-gene panel testing (MGPT) is favored due to its higher analytical sensitivity and specificity. By focusing on cancer-associated genes, it simplifies interpretation and improves diagnostic accuracy. NGS uses massive parallel sequencing of DNA fragments to detect genetic changes by analyzing read depth, while MLPA is a semi-quantitative technique based on the amplification of probes, each detecting a specific DNA sequence. It can detect deletions or duplications as small as 60 nucleotides, which allows for the detection of single exon deletions or insertions/duplications. NGS provides high throughput and the ability to analyze large gene panels in a single experiment, while MLPA is a more targeted, cost-effective, and labor-intensive method used for specific genes or regions, often as a confirmatory test for NGS results.
In this study, we hypothesized that combination of two complementary molecular methods could increase diagnostic sensitivity in molecular diagnostics of LS: next-generation sequencing multigene panel testing for detection of point mutations, frameshift mutations, splice-site mutations, small deletions, and small duplications/insertions and multiplex ligation-dependent probe amplification (MLPA) for detection of deletions and duplications/insertions (CNVs) larger than 50 base pairs in length.
2. Materials and Methods
In University Hospital Center Zagreb, after genetic counseling, 60 patients suspected of Lynch syndrome were referred to the Department of Molecular Laboratory Diagnostics for genetic testing from 2022 to 2024. Our cohort included 60 participants; 52 participants had a personal history of cancer and 8 participants were included due to positive family history suggestive of Lynch syndrome. Average age was 51.2 years (±12.8 SD, 29–78). There were 16 males and 46 females. The youngest patient confirmed to have Lynch syndrome was a 30-year-old female patient affected by colorectal cancer. A total of 24 participants had colorectal cancer; 12 of them had endometrial carcinoma and 5 of them had urothelial carcinoma.
As inclusion criteria, we used Amsterdam II clinical criteria as follows:
There should be at least three relatives with HNPCC-associated cancer (cancer of the colorectum, endometrium, small bowel, ureter, or renal pelvis) and the following:
One should be a first-degree relative to the other two;
At least two successive generations should be affected;
At least one should be diagnosed before age 50;
Familial adenomatous polyposis should be excluded;
Tumors should be verified by pathological examination.
To identify patients eligible for molecular testing for MSI, revised Bethesda criteria were used as follows:
Individual with CRC diagnosed by age 50;
Individual with synchronous or metachronous CRC, or other HNPCC-associated tumors regardless of age;
Individual with CRC and MSI-H histology diagnosed by age 60;
Individual with CRC and more than 1 first-degree relative (FDR) with an HNPCC-associated tumor, with one cancer diagnosed by age 50;
Individual with CRC and more than 2 FDRs or second-degree relatives (SDRs) with an HNPCC-associated tumor, regardless of age.
This study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of University Hospital Centre Zagreb for studies involving humans (Class 8.1-24/257-2, No 02/013AG, 4 December 2024). An informed consent statement was obtained from the participants included in the study. After peripheral blood sampling (K3EDTA, 3 mL tubes), genomic DNA extraction was performed (QIAamp DNA Blood Mini Kit, Qiagen, Germany). In all DNA samples obtained by extraction, DNA concentration and purity were checked by spectrophotometric and fluorometric measurement (NanoDrop and Qubit). For all patients, DNA samples were sequenced using next-generation sequencing (NGS) with a multigene panel covering 113 cancer susceptibility genes, including MMR genes (TruSight hereditary cancer panel, MiSeq, Illumina). The analysis was performed using the software package provided by the manufacturer (Variant Studio software package, Illumina). The NGS multigene panel testing covering 113 cancer susceptibility genes including MMR genes used predesigned, ready-to-use oligo probes that covered exonic regions for all genes and 20 bp of flanking intronic regions for each targeted gene including MMR genes (MLH1, MSH2, MSH6, PMS2, and EPCAM). For secondary and tertiary NGS data analysis, we used DRAGEN v4.3 and EMEDGENE v38 software with set criteria for germline variants: read depth threshold of 50x and variant frequency (VAF) ≥ 20%. For our NGS multi-gene panel, the mean read depth for targeted sequences ranged from about 300 to 600x between runs for different regions, including MMR genes. After the validation process, using Sanger sequencing for PV, LPV, and VUS confirmation, we determined that the NGS software package we used had a limitation in genomic variant detection at an upper limit of 50 base pairs in length. Therefore, DNA samples with no pathogenic variant in MMR genes detected by the NGS were further analyzed by the MLPA method for the presence of copy number variants. The reagents used for the MLPA analysis were provided by MRC Holland (Amsterdam, The Netherlands)—Probemix P003 (IVD) MLH1/MSH2, Probemix P008 (IVD) PMS2, Probemix P072 (IVD) MSH6-MUTYH, and Probemix P248 (IVD) MLH1-MSH2 Confirmation. In order to perform EPCAM gene testing, we used SALSA MLPA Probemix P072 MSH6-MUTYH (IVD), which detected CNVs in the MSH6 gene, the EPCAM/MSH2 region, and the MUTYH gene. For the EPCAM gene, the MLPA probes were arranged to cover exons 3, 8, and 9 and a downstream region (3′-end of EPCAM). The NGS method provided good coverage for all exons in the PMS2 gene (300–600x) by using NGS multi-gene panel testing where PMS2-PMS2CL homology (pseudogene) was solved by a novel computational method called multi-region joint detection (MRJD). Instead of considering each region in isolation and genotyping them individually, MRJD considers all locations from which a group of reads may have originated and attempts to detect the underlying sequences jointly. This approach retains reads with ambiguous alignment and is useful for instances of read misalignment due to gene conversion or crossover events. The SALSA MLPA Probemix P008 PMS2 is an in vitro diagnostic (IVD) semi-quantitative assay for the detection of deletions or duplications in exons 1–11 of the PMS2 gene and in exons 12–15 of the PMS2 gene or PMS2CL pseudogenes. Since we did not find a VUS/LP/P variant in the PMS2 gene, it was not necessary to confirm it using confirmation methods. For fragment analysis, a capillary electrophoresis device was used (ABI 3500xL Genetic Analyser, Applied Biosystems, Waltham, MA, USA). The results were analyzed using the Coffalyser.Net software tool provided by MRC Holland.
For variant interpretation, various databases were used (ExAC, gnomAD, 1000 Genomes, ClinVar, OMIM, COSMIC, PubMed, etc.). In silico programs (SIFT, PolyPhen, and Mutation Tester) were used to assess the pathogenicity of the variants. Sequence changes were defined based on the reference genome (GRCh37) and interpreted in the context of the clinically relevant transcript (NM_). All detected pathogenic or likely pathogenic variants were classified and reported according to ACMG standards and guidelines for the interpretation of sequence variants [
7].
Tumor-based analysis of Mismatch Repair (MMR) status was performed by accredited pathology services, including the Clinical Hospital Centre Zagreb (KBC Zagreb), following established national and international guidelines for Lynch syndrome screening. For immunohistochemistry (IHC), a four-antibody panel (MLH1, PMS2, MSH2, and MSH6) was used. The universal standard of loss of nuclear staining in tumor cells (with retained positivity in internal control cells) was utilized as the cut-off to define protein deficiency. For microsatellite instability status (MSI), testing was conducted using either the five-marker NCI panel (BAT25, BAT26, D5S346, D2S123, and D17S250) or an equivalent, validated commercial multiplex system. In line with consensus guidelines, MSI-High (MSI-H) was defined as instability in ≥2 of the 5 markers.
3. Results
Our study included 60 patients, 14 male (median age 49 (IQR: 40–54)) and 46 female (median age 51 (IQR: 41–63)). Almost every selected patient had previously developed some type of cancer associated with LS (colorectal, endometrial, ovarian). Only 8 out of 60 patients had not previously developed cancer but were suspected of LS regarding positive family history. Out of 60 patients, a total of 10 genetic changes in MMR genes were detected by NGS method, which corresponds to 16.7% of patients (10/60). For the patients with pathogenic variants in MMR genes detected by NGS, there was no need to perform MLPA analysis. Therefore, MLPA analysis was performed on 50 patients, where seven additional copy number variants were detected with the MLPA method, representing 14% of NGS negative patients (7/50). By using two complementary methods, a total of 17 pathogenic variants in MMR genes were detected, corresponding to 28.4% of total patients (17/60). No LPs or VUSs were detected. Of all detected variants, point mutations, frameshift mutations, and splice-site mutations account for 59% (10/17) and CNVs account for 41% (7/17). All PVs detected by NGS were confirmed with Sanger sequencing, while CNVs detected in MLH1 and MSH2 genes by MLPA were confirmed using Probemix P248 (IVD) MLH1-MSH2 Confirmation, as recommended by the manufacturer.
Data relevant to LS diagnosis for the patients with MMR pathogenic variants are presented in
Table 1.
The majority of changes were detected in the
MSH2 gene (8/17; 47.1%), followed by the
MLH1 gene (6/17; 35.3%), and 3 out of 17 were detected in
MSH6 (3/17; 17.7%).
Figure 1 graphically shows genetic changes found in our patient group. No variants in the
PMS2 and
EPCAM genes were detected. Interestingly, all PVs detected by NGS were different. There were three nonsense, three frameshift, two missense, and two splice donor pathogenic variants, whereas the CNVs detected by MLPA were repeated: all three changes detected by MLPA in the
MLH1 gene were the same deletions of exons 9–15 and two of the four changes detected by MLPA in the
MSH2 gene were the same deletions of exon 1 and the upstream region. In the
MSH6 gene CNVs were not detected.
Microsatellite instability (MSI) and/or immunohistochemical staining (IHC) were available for 13 patients where, in 11 tumor tissue samples, MSI and/or positive IHC results (lack of MMR protein expression) were confirmed, but in two tumor tissue samples, MSI was negative (sustained MMR protein expression). In five patients with positive hereditary PVs in MMR genes, the MSI and/or IHC testing results in tumor tissue for the same gene were also positive (lack of certain protein expression in tumor tissue corresponds to the mutation in the gene). However, six patients had tumors with MSI and/or positive IHC results but no detected hereditary PV in their MMR genes.
Table 2 shows the concordance of MSI/IHC-positive results with the germline findings per case.
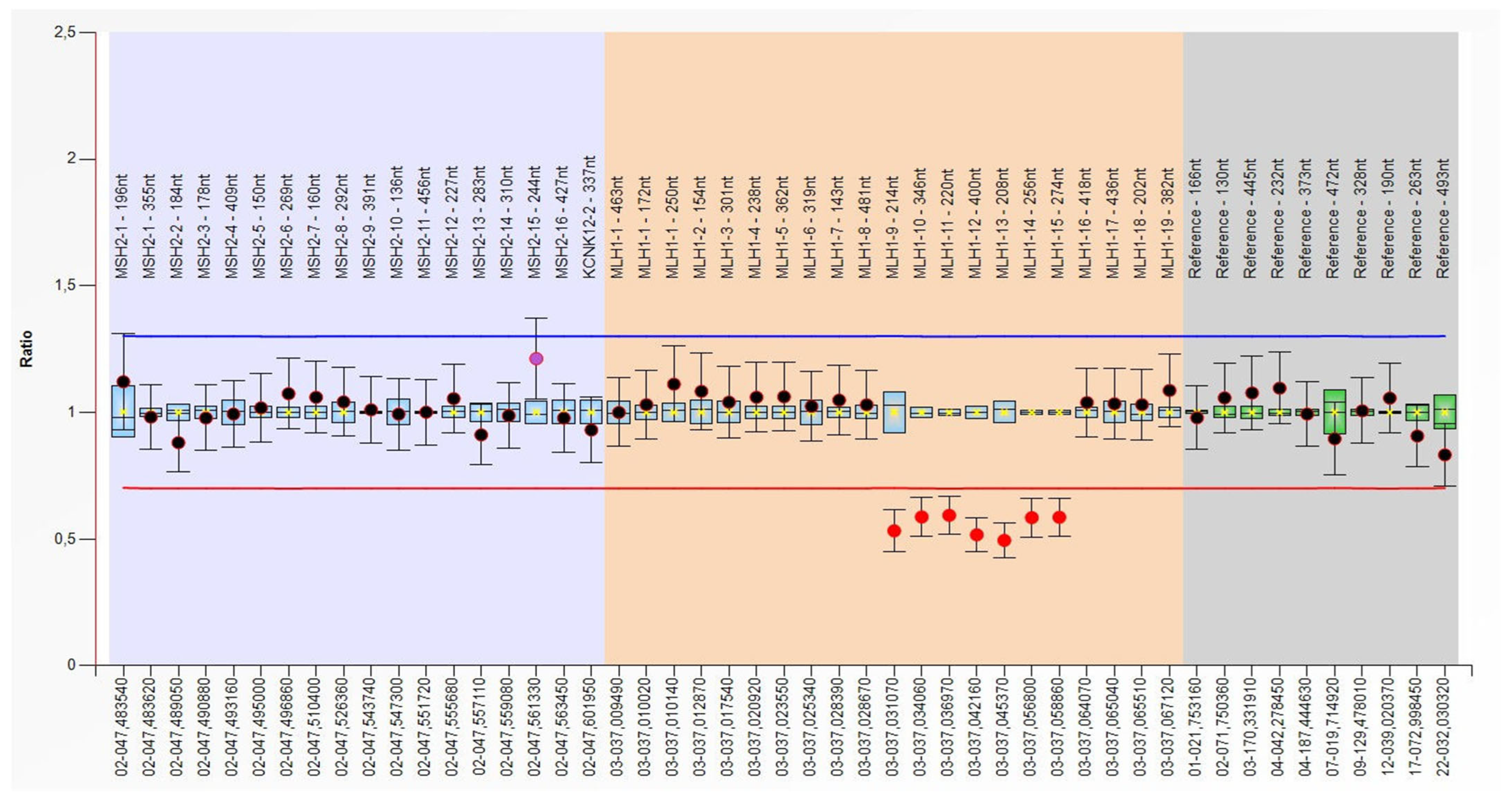
Figure 2 shows positive MLPA results for a large heterozygous deletion that includes seven exons (exon 9–15) in the
MLH1 gene. For the same patient (Sample number 4), a lack of MLH1 protein expression was demonstrated in their tumor tissue (colon cancer).
4. Discussion
In Lynch syndrome, the risk for tumor development is inherited, rather than the disease itself [
8]. The risk of developing CRC varies depending on gender and the affected MMR gene [
1]. In addition to CRC, there is also a significantly increased risk for the development of other cancers outside the colon, again depending on the affected MMR gene and gender [
1]. Endometrial cancer (EC) is the most common cancer outside the colon associated with LS, occurring in women at a rate comparable to that of colorectal cancer. The risk of developing EC ranges from 14 to 54% when the
MLH1 gene is mutated, 17–71% when the
MSH6 gene is mutated, and 15% when the
PMS2 gene is mutated. The risk for ovarian cancer is lower, at 4–20%, and is mainly associated with mutations in the
MSH2 gene.
In our cohort of 60 patients, LS was confirmed in 17 patients who had germline PV in one of the MMR genes. In genetic counseling, 15 of the 17 patients already had a diagnosis of cancer, mostly colon cancer (11/17) and endometrial cancer (4/17), but also breast, urothelial, ovarian, gastric, and cervical cancer, where five patients had two or three different primary cancers necessarily including colon or endometrial cancer. Two patients with detected PVs in MMR genes were healthy but with extremely positive family histories of LS cancers (see
Table 1).
According to the literature, in approximately 80–90% of LS cases, the mutations affect the
MLH1 and
MSH2 genes, while in the remaining 10–20% of LS cases, mutations involve the
MSH6 or
PMS2 genes. Mutations in the
EPCAM gene are extremely rare, occurring in only about 3% of cases [
2]. A 3′ deletion of the terminal exons of the
EPCAM gene, which is located upstream of
MSH2 gene, causes epigenetic silencing of
MSH2, resulting in a tissue-specific deficiency of the MSH2 protein [
9]. The most common point mutations in MMR genes are missense mutations which lead to single amino acid substitutions. Additionally, there are nonsense mutations, where the substitution of a single nucleotide introduces a stop codon, leading to truncation of the polypeptide chain, again resulting in a nonfunctional protein [
10] (pp. 63–67). The frequency of missense mutations for all four genes (
MLH1, MSH2, MSH6, PMS2) ranges from 30% (
MSH2) to 60% (
PMS2). Also, common pathogenic variants in
MLH1,
MSH2, and
MSH6 are truncating variants (predominantly nonsense or frameshift mutations) with a frequency from 40% (
MLH1) to 49% (
MSH2), while splice-site pathogenic variants occur least frequently, from 3% (
MSH6) to 11% (
MLH1) [
11]. A significant proportion of changes in MMR genes are copy number variants or large genomic rearrangements. According to Cohen et al. (2019), large deletions account for 22% of
MLH1 and
PMS2 mutations, 26% of
MSH2 mutations, and about 7% of
MSH6 mutations [
12]. In the
EPCAM gene, large genomic changes are the only alterations reported in the literature to date [
13].
In this study, the highest number of PVs were found in the
MSH2 gene (8/17; 47.1%) of which four large deletions were detected by the MLPA method and four PVs detected by the NGS method: two nonsense, one missense, and one splice donor. In the
MLH1 gene, six variants were detected (6/17; 35.3%), including three large genomic deletions, while the remaining three PVs were detected by the NGS method: one frameshift, one missense, and one splice donor. Additionally, in the
MSH6 gene, three PVs were detected by NGS (3/17, 17.6%), two frameshift and one nonsense, while no genomic changes were detected in the
PMS2 and
EPCAM genes (see
Figure 1).
To detect all possible molecular changes in MMR genes, it is advisable to use a method that covers as many genes as possible. The most commonly used method is NGS multigene panel testing, which can detect point mutations, as well as small deletions and insertions/duplications in several hundred genes simultaneously [
2]. However, depending on the software package used for analyzing NGS data and known software limitations, this method cannot reliably detect SVs, such as large deletions and/or insertions/duplications, structural rearrangements, or genetic changes in gene regions not covered by the multigene panel applied. Therefore, supplementary methods should be used to detect the presence of SVs as these changes account for a significant portion (>20%) of all changes in MMR genes. In our sample, out of seventeen detected variants, three were nonsense, three frameshift, two missense, two splice donor variants, and seven CNVs. As a first molecular method, we used NGS multigene panel testing (NGS) and, as a second method, we used MLPA, which can detect SVs such as exon-level CNVs. With such a combination of methods, we detected 17 pathogenic variants, where 10 variants were detected by NGS, and 7 were large deletions from 1 to 6 exons in size, detected by MLPA.
Our results are similar to data in the literature. We performed genetic testing on a group of 60 patients. Pathogenic or likely pathogenic variants were identified in the
MLH1 and
MSH2 genes of 21 patients (21/60, 35%), and approximately one-third of these changes were large deletions. In our study, 17 pathogenic changes were detected, which corresponds to 28.3% (17/60), and is in line with the results of other studies available in the literature [
14]. Gylling et al. (2009) [
15] examined changes in MMR genes in 45 patients who did not have point mutations identified by sequencing. They found a large genomic change in 12 out of 45 patients (27%): deletions were present in 3/25 (12%), 9/16 (56%), and 0/4 (0%) of patients with missing expression of MLH1, MSH2, and PMS2 proteins, respectively [
15].
The clinical criteria for the initial identification of LS cases are summed up by the Amsterdam criteria and the revised Bethesda guidelines [
2]. In 1990, the International Collaborative Group on Hereditary Non-Polyposis Colorectal Cancer (HNPCC) developed the Amsterdam Criteria I for identifying families that could be candidates for genetic testing. These criteria were later expanded to include cancers outside the colon that occur as part of LS (Amsterdam Criteria II). However, these criteria proved to be very restrictive, resulting in missed identification of some carriers of mutations in MMR genes [
5]. The revised Bethesda guidelines for microsatellite instability (MSI) testing provide detailed instructions on when to test a patient for MSI [
2]. Nevertheless, the Amsterdam criteria (I and II) and the revised Bethesda guidelines are not always sufficient for identifying LS patients, which is why they are not fully implemented in clinical practice [
9]. When a patient meets the Amsterdam criteria or at least one of the revised Bethesda guidelines, testing for microsatellite instability (MSI) and/or immunohistochemical staining (IHC) is recommended if tumor tissue is available [
2]. However, today, a more widely accepted approach is universal IHC/MSI testing for all newly diagnosed colorectal cancers, regardless of whether the guidelines are met, as it has been observed that strict adherence to the guidelines can lead to misdiagnosis of LS [
1]. In patients with MSI-high (MSI-H) tumors or loss of MMR protein expression in tumor tissue, further genetic testing is performed to identify the mutation or change in the specific gene that caused MSI or loss of MMR protein expression [
2]. Genetic testing can detect mutations in tumor tissue or peripheral blood. Since confirmation of the LS diagnosis is based on identifying the hereditary mutation, the preferred sample is peripheral blood, which is followed by targeted testing of family members of the proband with the purpose of disease prevention [
2]. Robinson et al. (2007) [
16] investigated the presence of hereditary mutations in MMR genes in a group of 112 patients. Patients were selected based on the Amsterdam criteria, the presence of microsatellite instability (MSI) in the tumor, and the results of immunohistochemical analysis. They identified a hereditary mutation in 69 out of 112 patients. They found pathogenic hereditary mutations in MMR genes not only in patients with MSI-H tumors but also in patients with MSI-negative tumors. This demonstrated that hereditary mutations in MMR genes can be found in patients with MSI-negative tumors, and also that patients with MSI-H colorectal cancer (CRC) or loss of MMR protein expression in their tumor may not necessarily show hereditary mutations in MMR genes through genetic testing, which would exclude the diagnosis of Lynch syndrome [
16]. Out of the 60 patients recruited in our study, MSI and/or IHC testing results were available for 13 patients. For 11 of them, MSI and/or positive IHC testing results (lack of MMR protein expression) were confirmed in tumor tissue, but in 2 patients, MSI was negative (sustained MMR protein expression) in tumor tissue. Furthermore, out of 60 patients, 6 patients had tumors with MSI and/or positive IHC results but no detected pathogenic variants in MMR genes. Out of 17 patients with a confirmed pathogenic variant in one of the MMR genes, 5 patients had available MSI and/or IHC testing results in tumor tissue (see
Table 1), and in those 5 cases, MSI and/or IHC testing results perfectly correlated with NGS and/or MLPA results (lack of certain protein expression in tumor tissue corresponds to the mutation in the gene). The six patients displaying a deficient MMR (dMMR) tumor phenotype (positive MSI/IHC findings) without a detectable germline pathogenic variant (PV) represent the clinical challenge of ‘Lynch-like Syndrome.’ These findings warrant extended genetic investigation for alternative causes, most notably acquired somatic hypermethylation (epimutation) of the MLH1 promoter in cases of MLH1/PMS2 loss, or the presence of PVs in less common MMR genes or in intronic/deep regulatory regions not covered by current molecular methods.
The MLPA method for MMR gene testing has an IVD (In Vitro Diagnostic) certificate that demonstrates that a medical device used to test samples taken from the human body (like blood or tissue) complies with the requirements of the European Union’s In Vitro Diagnostic Regulation (IVDR). It signifies that the device is safe and performs as intended for its intended use, allowing it to be legally commercialized within the EU, establishing a quality management system (QMS), preparing technical documentation, and ensuring that the device undergoes conformity assessment. However, the MLPA method has certain limitations that need to be considered before its implementation in routine diagnostics. For example, the presence of a single nucleotide polymorphism (SNP) or point mutation at the probe binding site can prevent the probe from binding and amplifying, which could then be interpreted as a false-positive deletion. Further, MLPA method cannot detect balanced gene rearrangements and mutations in parts of the genome that are not covered by the probes, so a negative result does not exclude translocation or inversions or the presence of a genomic change at a genomic position not covered by the probes. The greatest advantage of the MLPA method is the ability to simultaneously test whole genes and a large number of samples, which facilitates routine application. Additionally, the test manufacturer provides users with appropriate software for processing data obtained through capillary electrophoresis. However, in the future, the MLPA method could be replaced by long read sequencing technology, which generates long, continuous DNA sequences (kilobases to megabases), making it ideal for resolving complex structural variations and repetitive regions, whereas MLPA is a more targeted and sensitive method for detecting specific, known CNVs like deletions or duplications at specific locations in a gene.