Clinical and CT Features of HIV-Negative and HIV-Positive Patients with Abdominal Tuberculous Lymphadenopathy
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Imaging Protocol and Analysis
2.3. Statistical Analysis
3. Results
3.1. Demographic Features and Clinical Features
3.2. Patient Laboratory Features
3.3. CT Characteristics of ATBL
3.4. Post Hoc Power Analysis
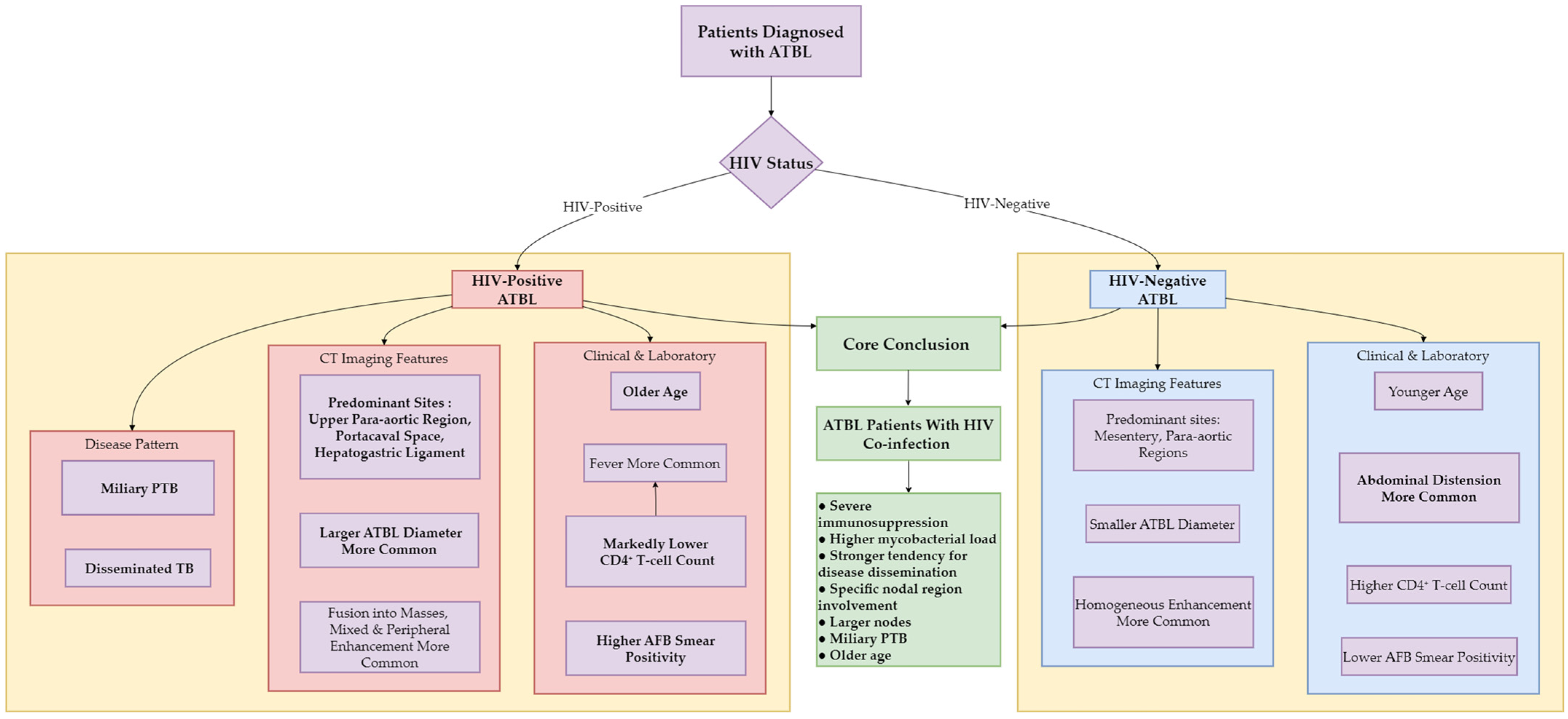
3.5. Visualization of Core Clinical-Radiologic Associations
4. Discussion
4.1. Demographic Features and Clinical Symptoms
4.2. Laboratory Features
4.3. CT Imaging Analysis
4.4. Co-Involvement of Other Sites
5. Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ATBL | abdominal tuberculous lymphadenopathy |
| TB | tuberculosis |
| PTB | pulmonary TB |
| EPTB | extrapulmonary TB |
| ATB | abdominal TB |
| AFB | acid-fast bacilli |
| M.tuberculosis | Mycobacterium tuberculosis |
References
- World Health Organization (WHO). The WHO Global Tuberculosis 2022 Report. Available online: https://www.who.int/publications/i/item/9789240061729 (accessed on 15 July 2023).
- Kahn, D.; Pool, K.L.; Phiri, L.; Chibwana, F.; Schwab, K.; Longwe, L.; Banda, B.A.; Gama, K.; Chimombo, M.; Chipungu, C.; et al. Diagnostic Utility and Impact on Clinical Decision Making of Focused Assessment With Sonography for HIV-Associated Tuberculosis in Malawi: A Prospective Cohort Study. Glob. Health Sci. Pract. 2020, 8, 28–37. [Google Scholar] [CrossRef]
- Tiemersma, E.W.; van der Werf, M.J.; Borgdorff, M.W.; Williams, B.G.; Nagelkerke, N.J. Natural history of tuberculosis: Duration and fatality of untreated pulmonary tuberculosis in HIV negative patients: A systematic review. PLoS ONE 2011, 6, e17601. [Google Scholar] [CrossRef]
- Rathi, P.; Gambhire, P. Abdominal Tuberculosis. J. Assoc. Physicians India 2016, 64, 38–47. [Google Scholar]
- Al-Zanbagi, A.B.; Shariff, M.K. Gastrointestinal tuberculosis: A systematic review of epidemiology, presentation, diagnosis and treatment. Saudi J. Gastroenterol. 2021, 27, 261–274. [Google Scholar] [CrossRef]
- Li, Y.; Yang, Z.G.; Guo, Y.K.; Min, P.Q.; Yu, J.Q.; Ma, E.S.; Hu, J. Distribution and characteristics of hematogenous disseminated tuberculosis within the abdomen on contrast-enhanced CT. Abdom. Imaging 2007, 32, 484–488. [Google Scholar] [CrossRef]
- Abu-Zidan, F.M.; Sheek-Hussein, M. Diagnosis of abdominal tuberculosis: Lessons learned over 30 years: Pectoral assay. World J. Emerg. Surg. 2019, 14, 33. [Google Scholar] [CrossRef] [PubMed]
- Zhang, M.; Li, M.; Xu, G.P.; Liu, H.J. Neoplasm-like abdominal nonhematogenous disseminated tuberculous lymphadenopathy: CT evaluation of 12 cases and literature review. World J. Gastroenterol. 2011, 17, 4038–4043. [Google Scholar] [CrossRef] [PubMed]
- Zhang, G.; Yang, Z.G.; Yao, J.; Deng, W.; Zhang, S.; Xu, H.Y.; Long, Q.H. Differentiation between tuberculosis and leukemia in abdominal and pelvic lymph nodes: Evaluation with contrast-enhanced multidetector computed tomography. Clinics 2015, 70, 162–168. [Google Scholar] [CrossRef] [PubMed]
- Deshpande, S.S.; Joshi, A.R.; Deshpande, S.S.; Phajlani, S.A. Computed tomographic features of abdominal tuberculosis: Unmask the impersonator! Abdom. Radiol. 2019, 44, 11–21. [Google Scholar] [CrossRef]
- Raut, A.A.; Naphade, P.S.; Ramakantan, R. Imaging Spectrum of Extrathoracic Tuberculosis. Radiol. Clin. N. Am. 2016, 54, 475–501. [Google Scholar] [CrossRef]
- Perenboom, R.M.; Richter, C.; Swai, A.B.; Kitinya, J.; Mtoni, I.; Chande, H.; Kazema, R. Clinical features of HIV seropositive and HIV seronegative patients with tuberculous lymphadenitis in Dar es Salaam. Tuber. Lung Dis. 1995, 76, 401–406. [Google Scholar] [CrossRef]
- Zhu, X.L.; Liu, X.Y.; Wen, L.; Li, R.; Lv, S.X.; Wang, G.X. Clinical and CT characteristics of abdominal tuberculous lymphadenopathy: A comparative analysis of hematogenous and non-hematogenous dissemination. BMC Infect. Dis. 2025, 25, 710. [Google Scholar] [CrossRef] [PubMed]
- Zhu, X.L.; Tang, G.X.; Liu, X.Y.; Li, R.; Lv, S.X.; Wang, G.X. CT findings of Talaromyces marneffei infection among HIV patients with lymphadenopathy. Front Med. 2022, 9, 930678. [Google Scholar] [CrossRef] [PubMed]
- Guler, S.A.; Bozkus, F.; Inci, M.F.; Kokoglu, O.F.; Ucmak, H.; Ozden, S.; Yuksel, M. Evaluation of pulmonary and extrapulmonary tuberculosis in immunocompetent adults: A retrospective case series analysis. Med. Princ. Pract. 2015, 24, 75–79. [Google Scholar] [CrossRef] [PubMed]
- Kang, W.; Yu, J.; Du, J.; Yang, S.; Chen, H.; Liu, J.; Ma, J.; Li, M.; Qin, J.; Shu, W.; et al. The epidemiology of extrapulmonary tuberculosis in China: A large-scale multi-center observational study. PLoS ONE 2020, 15, e0237753. [Google Scholar] [CrossRef]
- Forssbohm, M.; Zwahlen, M.; Loddenkemper, R.; Rieder, H.L. Demographic characteristics of patients with extrapulmonary tuberculosis in Germany. Eur. Respir. J. 2008, 31, 99–105. [Google Scholar] [CrossRef]
- Lee, W.K.; Van Tonder, F.; Tartaglia, C.J.; Dagia, C.; Cazzato, R.L.; Duddalwar, V.A.; Chang, S.D. CT appearances of abdominal tuberculosis. Clin. Radiol. 2012, 67, 596–604. [Google Scholar] [CrossRef]
- Kapoor, V.K. Abdominal tuberculosis. Postgrad. Med. J. 1998, 74, 459–467. [Google Scholar] [CrossRef]
- Cechin, L.; Norcross, C.; Oliveira, A.; Hopkins, D.; McGowan, B.; Post, F.A. Obesity and diabetes in people of African ancestry with HIV. HIV Med. 2023, 24, 380–388. [Google Scholar] [CrossRef]
- Gulati, M.S.; Sarma, D.; Paul, S.B. CT appearances in abdominal tuberculosis. A pictorial essay. Clin. Imaging 1999, 23, 51–59. [Google Scholar] [CrossRef]
- Sinan, T.; Sheikh, M.; Ramadan, S.; Sahwney, S.; Behbehani, A. CT features in abdominal tuberculosis: 20 years experience. BMC Med. Imaging 2002, 2, 3. [Google Scholar] [CrossRef] [PubMed]
- Pombo, F.; Rodríguez, E.; Mato, J.; Pérez-Fontán, J.; Rivera, E.; Valvuena, L. Patterns of contrast enhancement of tuberculous lymph nodes demonstrated by computed tomography. Clin. Radiol. 1992, 46, 13–17. [Google Scholar] [CrossRef] [PubMed]


| HIV-Negative Group (n = 152) | HIV-Positive Group (n = 26) | ORs/ΔM [95% CIs] | Raw p | Adjusted p | |
|---|---|---|---|---|---|
| † Age (years) | 27.0 (22.0–46.0) | 42.5 (29.8–50.3) | 8.0 [3.0, 15.0] | 0.003 | 0.030 |
| Males | 89 (58.6%) | 21 (80.8%) | 2.973 [1.064, 8.305] | 0.048 | 0.203 |
| Smoking history | 48 (31.6%) | 10 (38.5%) | 1.354 [0.572, 3.203] | 0.503 | 1.000 |
| Alcohol intake | 31 (20.4%) | 4 (15.4%) | 0.710 [0.228, 2.210] | 0.790 | 1.000 |
| Clinical Symptoms | |||||
| Abdominal pain | 97 (63.8%) | 10 (38.5%) | 0.354 [0.150, 0.835] | 0.015 | 0.095 |
| † Abdominal distension | 62 (40.8%) | 3 (11.5%) | 0.189 [0.054, 0.658] | 0.004 | 0.036 |
| Diabetes mellitus | 3 (2.0%) | 3 (11.5%) | 6.478 [1.232, 34.052] | 0.041 | 0.182 |
| Malignant tumor | 4 (2.6%) | 0 (0%) | N/A ^ | 1.000 | 1.000 |
| Solid-organ or hematopoietic stem cell transplantation | 1 (0.7%) | 0 (0%) | N/A ^ | 1.000 | 1.000 |
| Chronic liver disease | 22 (14.5%) | 6 (23.1%) | 1.773 [0.640, 4.907] | 0.255 | 0.672 |
| Chronic heart disease | 4 (2.6%) | 0 (0%) | N/A ^ | 1.000 | 1.000 |
| Chronic pulmonary disease | 2 (1.3%) | 0 (0%) | N/A ^ | 1.000 | 1.000 |
| Chronic kidney disease | 5 (3.3%) | 0 (0%) | N/A ^ | 1.000 | 1.000 |
| † CD4+ T-cell counts (cells/µL) * | 301 (207–383) | 66 (22–130) | −214 [−260, −165] | <0.001 | 0.015 |
| Lymphocyte counts (×109/L) # | 0.877 (0.623–1.253) | 0.860 (0.415–1.490) | 0.067 [−0.226, 0.308] | 0.599 | 1.000 |
| Tuberculin skin test (positive) & | 93 (61.2%) | 10 (38.5%) | 0.397 [0.169, 0.932] | 0.034 | 0.160 |
| † Smear microscopy test for AFB (positive) $ | 28 (18.4%) | 14 (53.8%) | 5.167 [2.157, 12.373] | <0.001 | 0.015 |
| HIV-Negative Group (n = 152) | HIV-Positive Group (n = 26) | ORs/ΔM [95% CIs] | Raw p | Adjusted p | |
|---|---|---|---|---|---|
| Pericardial TB | 0 (0%) | 2 (7.7%) | N/A ^ | 0.021 | 0.109 |
| † Miliary PTB | 13 (8.6%) | 12 (46.2%) | 9.165 [3.516, 23.886] | <0.001 | 0.015 |
| Active PTB | 94 (61.8%) | 19 (73.1%) | 1.675 [0.663, 4.229] | 0.378 | 0.812 |
| Pleural effusion | 54 (35.5%) | 12 (46.2%) | 1.556 [0.672, 3.602] | 0.380 | 0.812 |
| Ascites | 90 (59.2%) | 14 (53.8%) | 0.804 [0.348, 1.855] | 0.669 | 1.000 |
| Peritonitis | 85 (55.9%) | 16 (61.5%) | 1.261 [0.538, 2.958] | 0.671 | 1.000 |
| Greater omentum infiltration | 75 (49.3%) | 6 (23.1%) | 0.308 [0.117, 0.809] | 0.018 | 0.107 |
| † Disseminated TB | 56 (36.8%) | 19 (73.1%) | 4.653 [1.841, 11.759] | 0.001 | 0.015 |
| Hepatosplenomegaly | 8 (5.3%) | 2 (7.7%) | 1.500 [0.300, 7.494] | 0.642 | 1.000 |
| Location | |||||
| † Upper para-aortic regions | 75 (49.3%) | 24 (92.3%) | 12.320 [2.813, 53.966] | <0.001 | 0.015 |
| Lower para-aortic regions | 48 (31.6%) | 11 (42.3%) | 1.589 [0.679, 3.717] | 0.367 | 0.812 |
| Hepatoduodenal ligament | 35 (23.0%) | 13 (50.0%) | 3.343 [1.420, 7.872] | 0.007 | 0.057 |
| † Portacaval space | 23 (15.1%) | 15 (57.7%) | 7.648 [3.123, 18.729] | 0.001 | 0.015 |
| Peripancreatic region | 24 (15.8%) | 4 (15.4%) | 0.970 [0.307, 3.066] | 1.000 | 1.000 |
| Mesentery | 135 (88.8%) | 21 (80.8%) | 0.529 [0.176, 1.586] | 0.328 | 0.775 |
| Iliac vessels regions | 18 (11.8%) | 3 (11.5%) | 0.971 [0.265, 3.562] | 1.000 | 1.000 |
| † Hepatogastric ligament | 30 (19.7%) | 13 (50.0%) | 4.067 [1.710, 9.671] | 0.002 | 0.025 |
| Gastrosplenic ligament | 3 (2.0%) | 0 (0%) | N/A ^ | 1.000 | 1.000 |
| Greater omentum | 12 (7.9%) | 1 (3.8%) | 0.467 [0.058, 3.750] | 0.695 | 1.000 |
| Pelvic cavity | 1 (0.7%) | 0 (0%) | N/A ^ | 1.000 | 1.000 |
| Inguinal region | 2 (1.3%) | 0 (0%) | N/A ^ | 1.000 | 1.000 |
| Single ATBL | 2 (1.3%) | 0 (0%) | N/A ^ | 1.000 | 1.000 |
| † Diameter of ATBL (cm) | 1.60 (1.20–2.10) | 2.25 (1.60–2.85) | 0.50 [0.20, 0.90] | 0.003 | 0.030 |
| Fused into mass | 55 (36.2%) | 17 (65.4%) | 3.331 [1.391, 7.976] | 0.008 | 0.059 |
| Enhancement pattern | |||||
| Peripheral rim | 11 (7.2%) | 6 (23.1%) | 3.845 [1.281, 11.546] | 0.022 | 0.109 |
| Homogeneous | 79 (52.0%) | 6 (23.1%) | 0.277 [0.105, 0.729] | 0.010 | 0.068 |
| Nonhomogeneous | 8 (5.3%) | 0 (0%) | N/A ^ | 0.606 | 1.000 |
| Homogeneous nonenhancement | 1 (0.7%) | 0 (0%) | N/A ^ | 1.000 | 1.000 |
| Mixed enhancement | 53 (34.9%) | 14 (53.8%) | 2.179 [0.941, 5.049] | 0.080 | 0.284 |
| Enhancement degree | |||||
| Low density | 18 (11.8%) | 7 (26.9%) | 2.743 [1.013, 7.429] | 0.062 | 0.251 |
| Iso-density | 49 (32.2%) | 10 (38.5%) | 1.314 [0.556, 3.105] | 0.653 | 1.000 |
| High density | 101 (66.4%) | 15 (57.7%) | 0.689 [0.295, 1.607] | 0.383 | 0.812 |
| Variable | Actual Power ** |
|---|---|
| CD4+ T-cell counts | 1.000 |
| Upper para-aortic regions | 0.998 |
| Portacaval space | 0.992 |
| Miliary PTB | 0.989 |
| Smear microscopy test for AFB (positive) | 0.948 |
| Disseminated TB | 0.940 |
| Abdominal distension | 0.904 |
| Hepatogastric ligament | 0.865 |
| Diameter of ATBL | 0.769 |
| Age | 0.597 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhu, X.-L.; Lv, S.-X.; Wen, L.; Li, R.; Liu, X.-Y.; Wang, G.-X. Clinical and CT Features of HIV-Negative and HIV-Positive Patients with Abdominal Tuberculous Lymphadenopathy. Diagnostics 2025, 15, 2931. https://doi.org/10.3390/diagnostics15222931
Zhu X-L, Lv S-X, Wen L, Li R, Liu X-Y, Wang G-X. Clinical and CT Features of HIV-Negative and HIV-Positive Patients with Abdominal Tuberculous Lymphadenopathy. Diagnostics. 2025; 15(22):2931. https://doi.org/10.3390/diagnostics15222931
Chicago/Turabian StyleZhu, Xiao-Ling, Sheng-Xiu Lv, Li Wen, Ran Li, Xue-Yan Liu, and Guang-Xian Wang. 2025. "Clinical and CT Features of HIV-Negative and HIV-Positive Patients with Abdominal Tuberculous Lymphadenopathy" Diagnostics 15, no. 22: 2931. https://doi.org/10.3390/diagnostics15222931
APA StyleZhu, X.-L., Lv, S.-X., Wen, L., Li, R., Liu, X.-Y., & Wang, G.-X. (2025). Clinical and CT Features of HIV-Negative and HIV-Positive Patients with Abdominal Tuberculous Lymphadenopathy. Diagnostics, 15(22), 2931. https://doi.org/10.3390/diagnostics15222931




