Characterization of Peripheral Retinal Degenerations and Rhegmatogenous Lesions Using Ultra-Widefield Swept Source OCT Integrated with a Novel Scanning Laser Ophthalmoscope
Abstract
1. Introduction
2. Material and Methods
3. Results
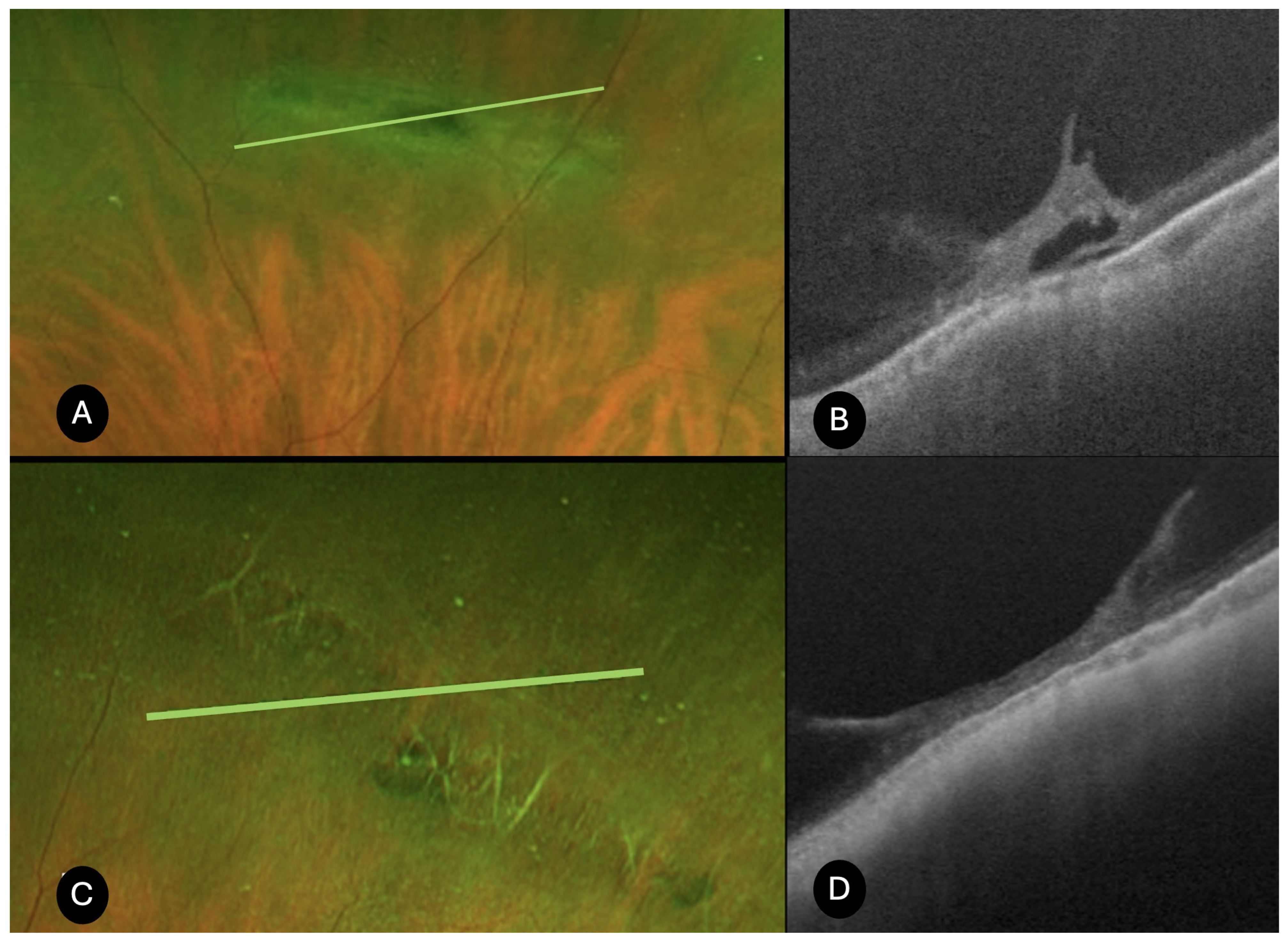
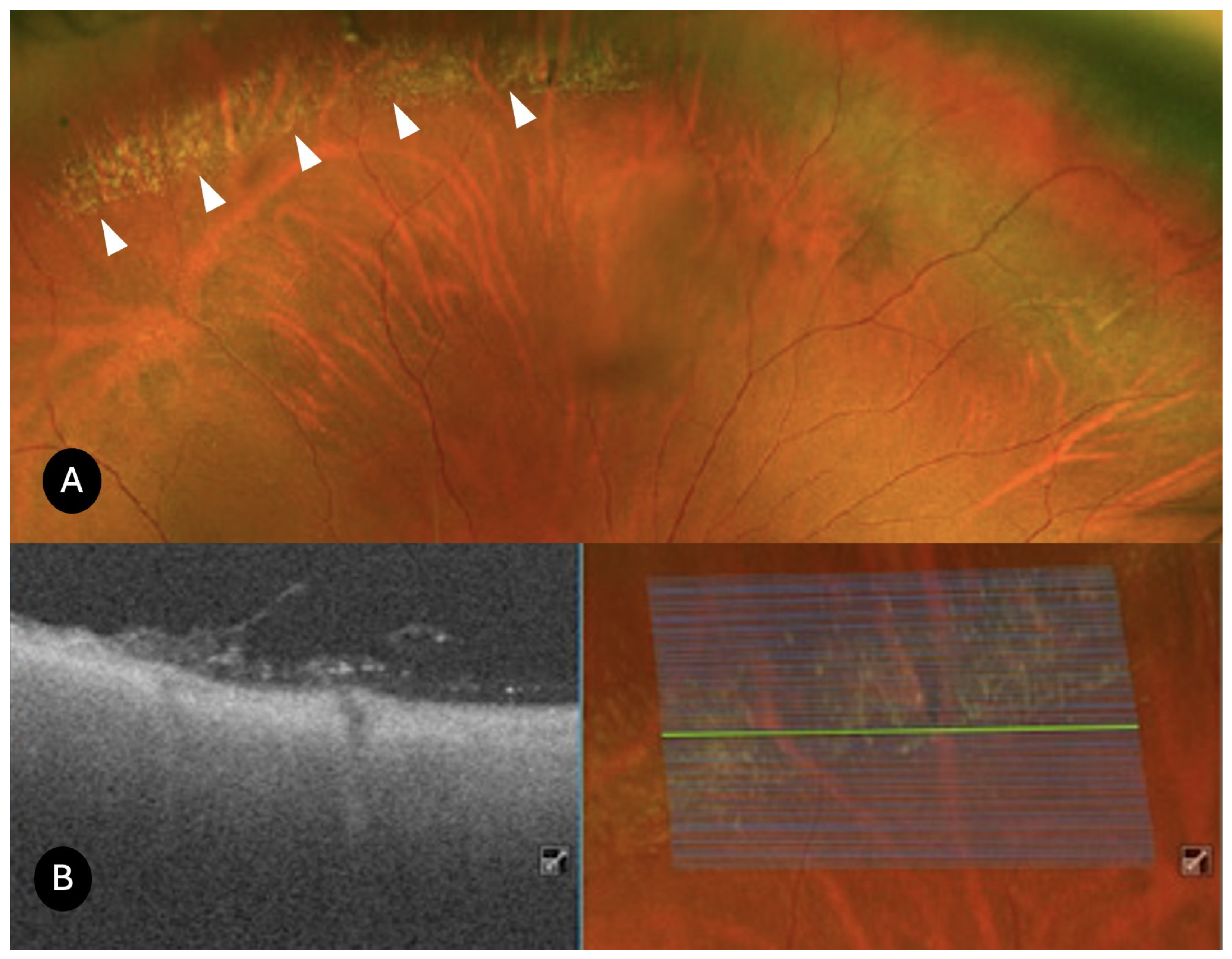
- Lattice degeneration (N = 25)
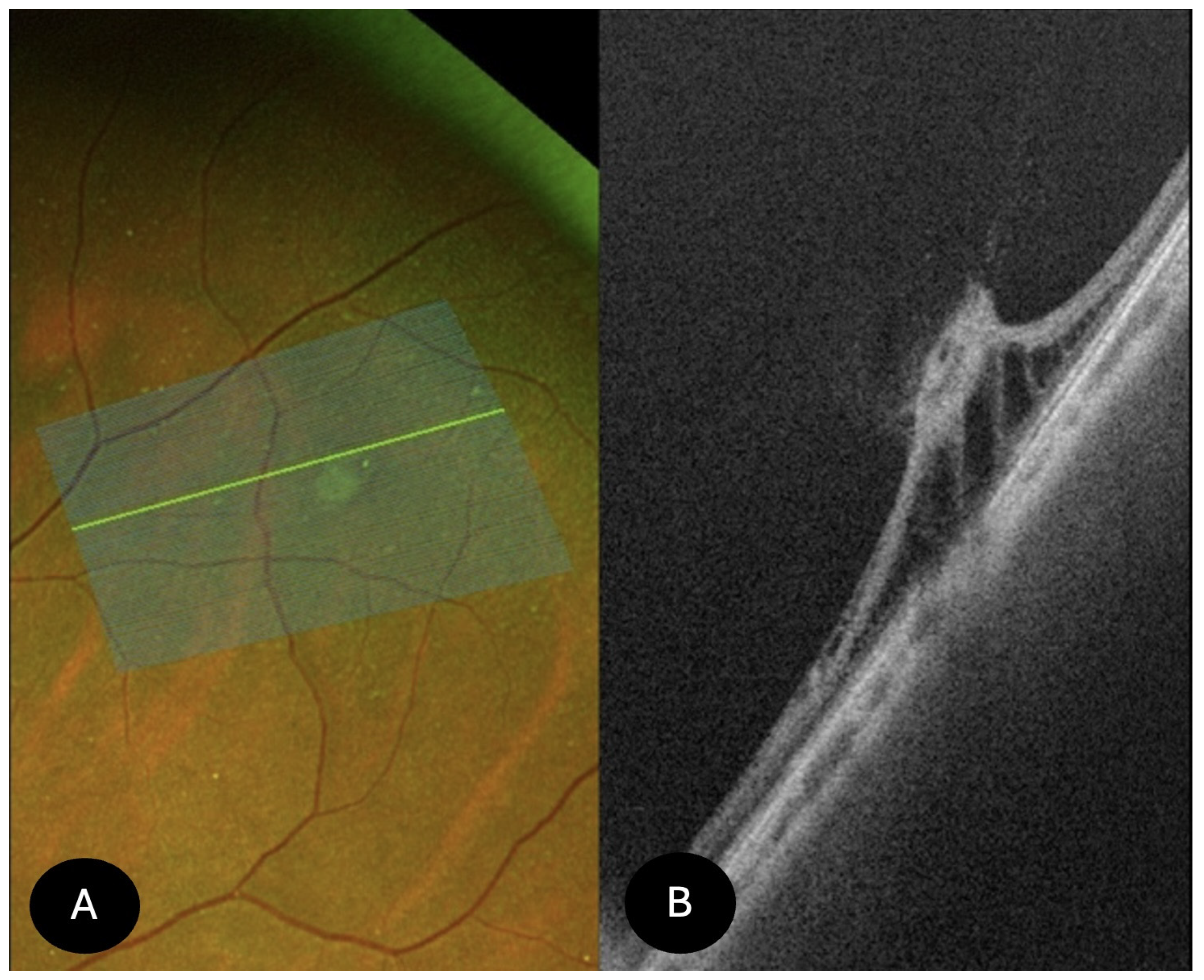
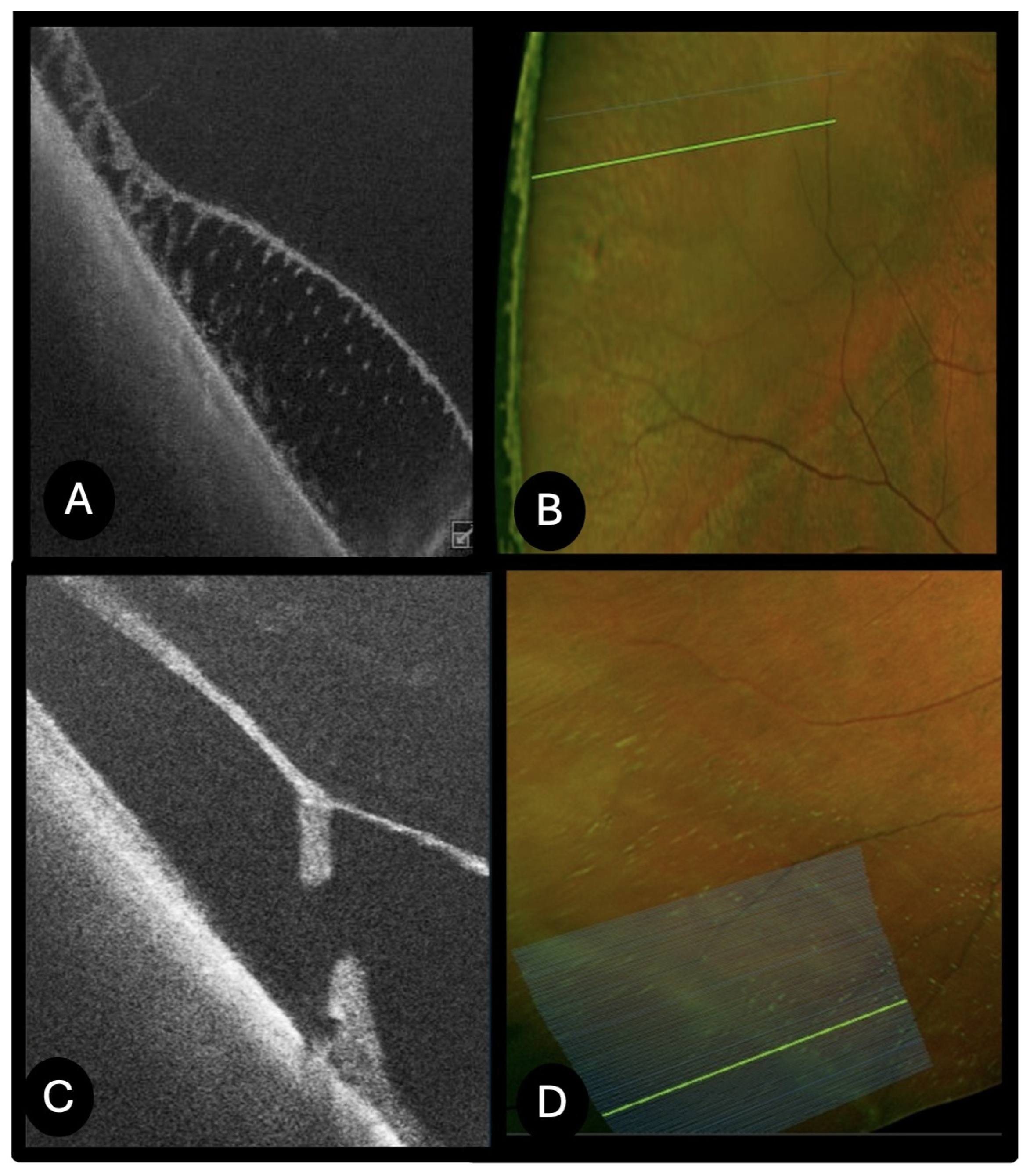
- Retinal Cystic Tufts (N = 11)
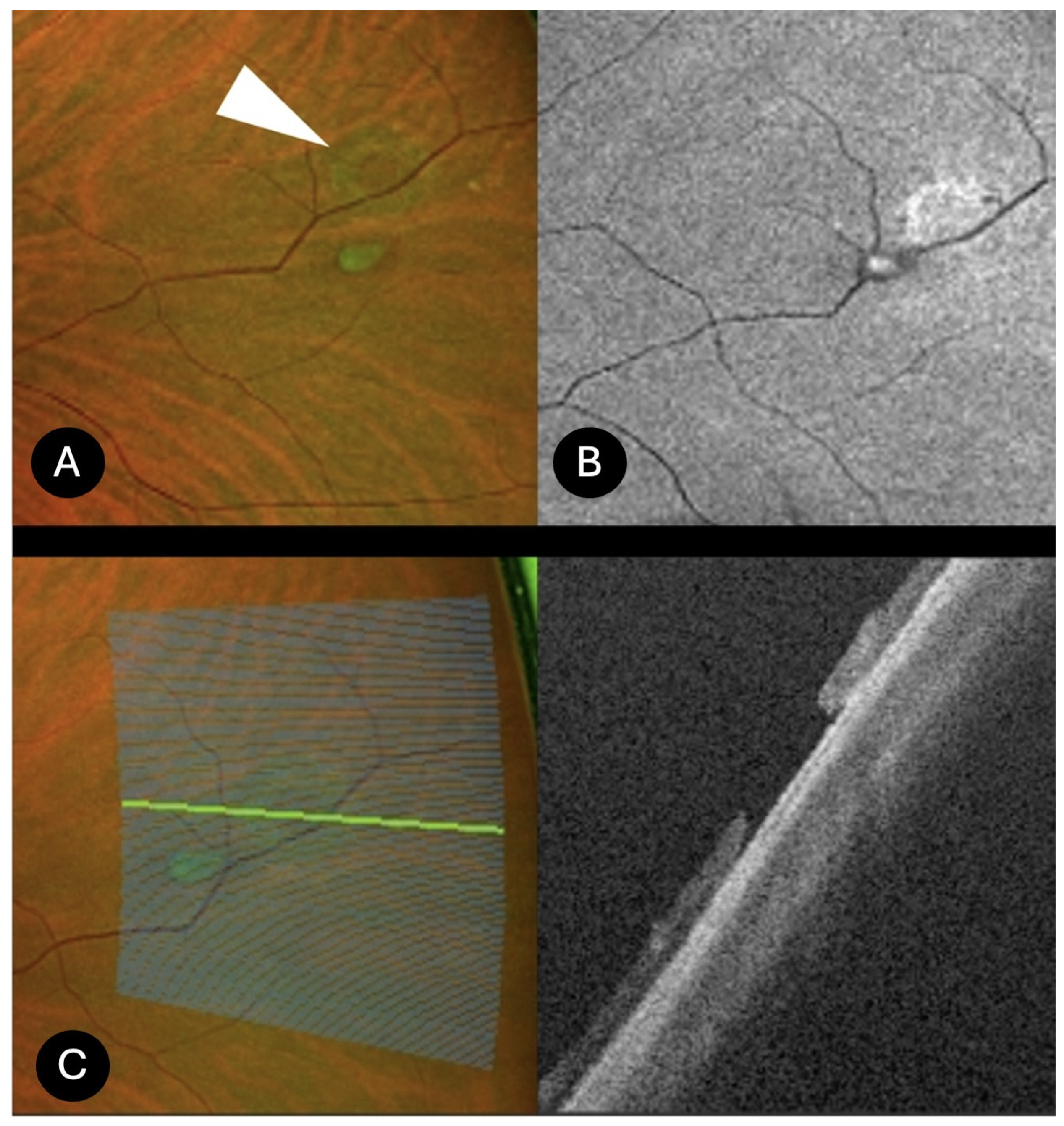
- Peripheral Retinal Holes (N = 21)
- Snail track degeneration (N = 4)
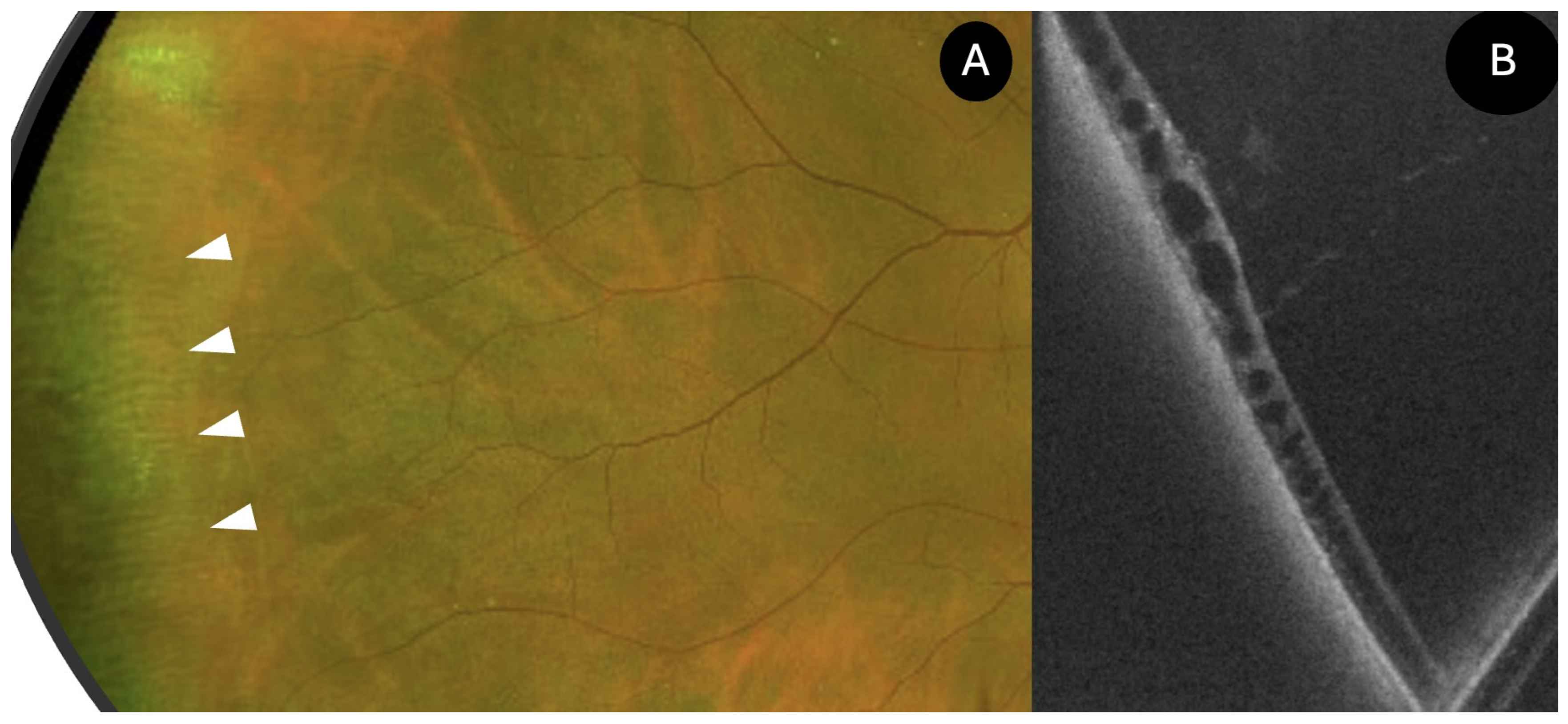
- White Without Pressure (N = 4)
- Peripheral retinoschisis (N = 24)
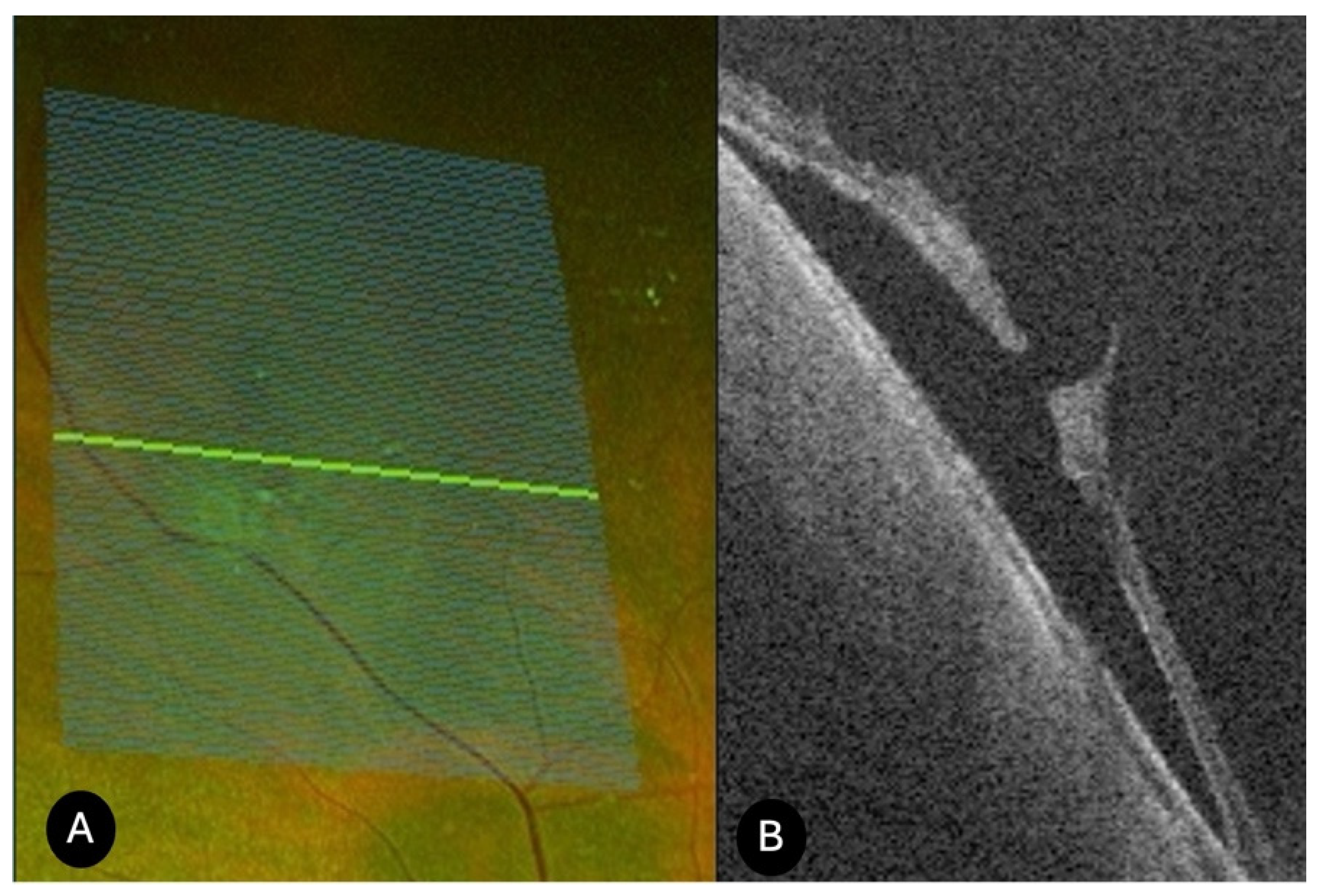
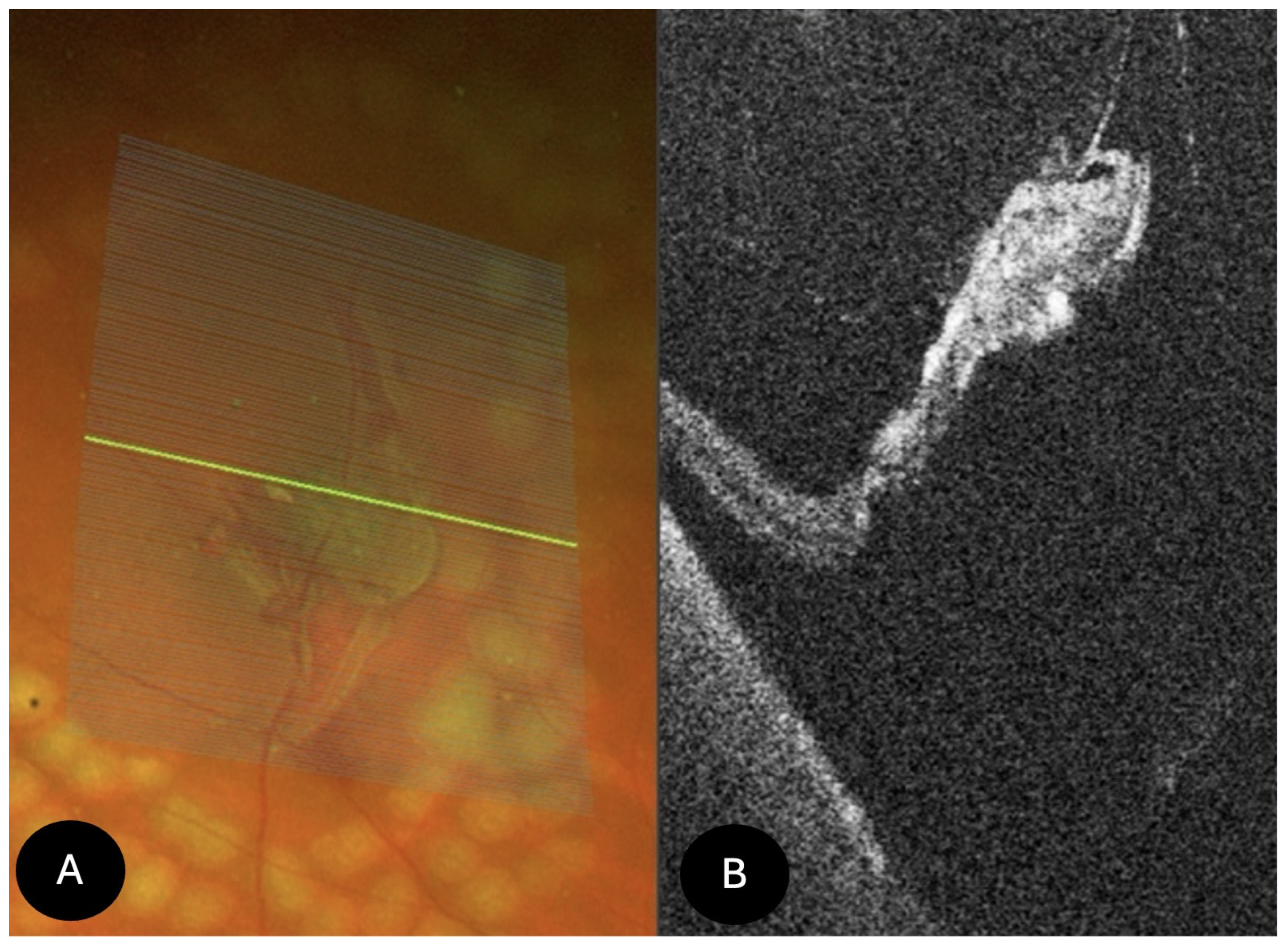
- Retinal tears (N = 34)
- Retinal dialysis (N = 2)
- Microcystic degeneration (N = 2)
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Fujimoto, J.; Swanson, E. The Development, Commercialization, and Impact of Optical Coherence Tomography. Investig. Ophthalmol. Vis. Sci. 2016, 57, OCT1–OCT13. [Google Scholar] [CrossRef]
- Huang, D.; Swanson, E.A.; Lin, C.P.; Schuman, J.S.; Stinson, W.G.; Chang, W.; Hee, M.R.; Flotte, T.; Gregory, K.; Puliafito, C.A.; et al. Optical Coherence Tomography. Science 1991, 254, 1178–1181. [Google Scholar] [CrossRef] [PubMed]
- Pattathil, N.; Choudhry, N. Optical Coherence Tomography Imaging of the Peripheral Retina. Saudi J. Ophthalmol. 2024, 38, 132–137. [Google Scholar] [CrossRef]
- Govetto, A.; Sebag, J.; Lucchini, S.; Ballabio, C.; Matteucci, M.; Ranno, S.; Carini, E.; Virgili, G.; Bacherini, D.; Radice, P. Imaging Rhegmatogenous Retinal Lesions and Peripheral Vitreoretinal Interface with Widefield Optical Coherence Tomography. Retina 2024, 44, 269–279. [Google Scholar] [CrossRef]
- Nagiel, A.; Lalane, R.A.; Sadda, S.R.; Schwartz, S.D. Ultra-Widefield Fundus Imaging: A Review of Clinical Applications and Future Trends. Retina 2016, 36, 660–678. [Google Scholar] [CrossRef]
- Choudhry, N.; Duker, J.S.; Freund, K.B.; Kiss, S.; Querques, G.; Rosen, R.; Sarraf, D.; Souied, E.H.; Stanga, P.E.; Staurenghi, G.; et al. Classification and Guidelines for Widefield Imaging. Ophthalmol. Retin. 2019, 3, 843–849. [Google Scholar] [CrossRef]
- Choudhry, N.; Golding, J.; Manry, M.W.; Rao, R.C. Ultra-Widefield Steering-Based Spectral-Domain Optical Coherence Tomography Imaging of the Retinal Periphery. Ophthalmology 2016, 123, 1368–1374. [Google Scholar] [CrossRef] [PubMed]
- Nadelmann, J.B.; Gupta, M.P.; Kiss, S.; Askin, G.; Chan, R.V.P.; Papakostas, T.; D’Amico, D.J.; Orlin, A. Ultra-Widefield Autofluorescence Imaging of Retinal Detachment Compared to Retinoschisis. Ophthalmic Surg. Lasers Imaging Retin. 2019, 50, 550–556. [Google Scholar] [CrossRef] [PubMed]
- Kumar, V.; Surve, A.; Kumawat, D.; Takkar, B.; Azad, S.; Chawla, R.; Shroff, D.; Arora, A.; Singh, R.; Venkatesh, P. Ultra-Wide Field Retinal Imaging: A Wider Clinical Perspective. Indian J. Ophthalmol. 2021, 69, 824–835. [Google Scholar] [CrossRef]
- Lewis, H. Peripheral Retinal Degenerations and the Risk of Retinal Detachment. Am. J. Ophthalmol. 2003, 136, 155–160. [Google Scholar] [CrossRef]
- Flaxel, C.J.; Adelman, R.A.; Bailey, S.T.; Fawzi, A.; Lim, J.I.; Vemulakonda, G.A.; Ying, G. Posterior Vitreous Detachment, Retinal Breaks, and Lattice Degeneration Preferred Practice Pattern®. Ophthalmology 2020, 127, P146–P181. [Google Scholar] [CrossRef] [PubMed]
- Al-Dwairi, R.; Saleh, O.; Mohidat, H.; Al Beiruti, S.; Alshami, A.; El Taani, L.; Sharayah, A.; Al Sharie, A.H.; Aleshawi, A. Characteristics, Risks, and Prevention of Rhegmatogenous Retinal Detachment in the Contralateral Eye. J. Clin. Med. 2025, 14, 222. [Google Scholar] [CrossRef]
- Byer, N.E. Long-Term Natural History of Lattice Degeneration of the Retina. Ophthalmology 1989, 96, 1396–1402. [Google Scholar] [CrossRef] [PubMed]
- Bec, P.; Malecaze, F.; Arne, J.L.; Mathis, A. Dégénérescence Givrée (Snail-Track, Snowflake Degeneration) de La Périphérie Rétinienne: Etude Ultrastructurale. Ophthalmologica 1985, 191, 107–113. [Google Scholar] [CrossRef]
- Kurobe, R.; Hirano, Y.; Ogura, S.; Yasukawa, T.; Ogura, Y. Ultra-Widefield Swept-Source Optical Coherence Tomography Findings of Peripheral Retinal Degenerations and Breaks. Clin. Ophthalmol. 2021, 15, 4739–4745. [Google Scholar] [CrossRef] [PubMed]
- Maltsev, D.S.; Kulikov, A.N.; Burnasheva, M.A. Lattice Degeneration Imaging with Optical Coherence Tomography Angiography. J. Curr. Ophthalmol. 2022, 34, 379–383. [Google Scholar] [CrossRef]
- Tsai, C.-Y.; Hung, K.-C.; Wang, S.-W.; Chen, M.-S.; Ho, T.-C. Spectral-Domain Optical Coherence Tomography of Peripheral Lattice Degeneration of Myopic Eyes before and after Laser Photocoagulation. J. Formos. Med. Assoc. 2019, 118, 679–685. [Google Scholar] [CrossRef]
- Maltsev, D.S.; Kulikov, A.N.; Shaimova, V.A.; Burnasheva, M.A.; Vasiliev, A.S. Spotlight on Lattice Degeneration Imaging Techniques. Clin. Ophthalmol. 2023, 17, 2383–2395. [Google Scholar] [CrossRef]
- Gonzales, C.R.; Gupta, A.; Schwartz, S.D.; Kreiger, A.E. The Fellow Eye of Patients with Phakic Rhegmatogenous Retinal Detachment from Atrophic Holes of Lattice Degeneration without Posterior Vitreous Detachment. Br. J. Ophthalmol. 2004, 88, 1400–1402. [Google Scholar] [CrossRef]
- Byer, N.E. Cystic Retinal Tufts and Their Relationship to Retinal Detachment. Arch. Ophthalmol. 1981, 99, 1788–1790. [Google Scholar] [CrossRef]
- Yu, H.; Luo, H.; Zhang, X.; Sun, J.; Zhong, Z.; Sun, X. Analysis of White and Dark without Pressure in a Young Myopic Group Based on Ultra-Wide Swept-Source Optical Coherence Tomography Angiography. J. Clin. Med. 2022, 11, 4830. [Google Scholar] [CrossRef] [PubMed]
- Diaz, R.I.; Sigler, E.J.; Randolph, J.C.; Rafieetary, M.R.; Calzada, J.I. Spectral Domain Optical Coherence Tomography Characteristics of White-Without-Pressure. Retina 2014, 34, 1020–1021. [Google Scholar] [CrossRef]
- Ho, V.Y.; Wehmeier, J.M.; Shah, G.K. Wide-Field Infrared Imaging: A Descriptive Review of Characteristics of Retinoschisis, Retinal Detachment, and Schisis Detachments. Retina 2016, 36, 1439–1445. [Google Scholar] [CrossRef] [PubMed]
- Jalalizadeh, R.A.; Smith, B.T. Characterization and Diagnosis of Retinoschisis and Schisis Detachments Using Spectral Domain Optical Coherence Tomography. Graefes Arch. Clin. Exp. Ophthalmol. 2023, 261, 375–380. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.J.; Bailey, S.T.; Kovach, J.L.; Lim, J.I.; Vemulakonda, G.A.; Ying, G.; Flaxel, C.J. Posterior Vitreous Detachment, Retinal Breaks, and Lattice Degeneration Preferred Practice Pattern®. Ophthalmology 2025, 132, P163–P196. [Google Scholar] [CrossRef]

| Patients, Eyes | 95 Patients (107 Eyes) |
|---|---|
| Age (years), mean ± SD | 50.8 ± 14.8 |
| Gender (M/F) | 46 (48.4%)/49 (51.6%) |
| Refractive error (diopters), mean ± SD | −2.18 ± 2.5 |
| Median BCVA (LogMAR) | 0.0 |
| Lens Status (phakia/pseudophakia) | 91 (95.8%)/4 (4.2%) |
| Type of Retinal Degeneration | n (%) |
|---|---|
| Retinal tear | 34 (26.2) |
| Lattice degeneration | 25 (19.2) |
| Retinal hole | 21 (16.2) |
| Peripheral Retinoschisis | 17 (13.1) |
| Retinal tuft | 11 (8.5) |
| Schisis/Detachment | 7 (5.4) |
| Snail track degeneration | 4 (3.1) |
| White without pressure | 4 (3.1) |
| Dialysis | 2 (1.5) |
| Condensed vitreous | 2 (1.5) |
| Microcystic degeneration | 2 (1.5) |
| Paving stone degeneration | 1 (0.8) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bacherini, D.; Rizzo, C.; Vicini, G.; Luciani, D.; Vannozzi, L.; Virgili, G.; Giansanti, F.; Nicolosi, C. Characterization of Peripheral Retinal Degenerations and Rhegmatogenous Lesions Using Ultra-Widefield Swept Source OCT Integrated with a Novel Scanning Laser Ophthalmoscope. Diagnostics 2025, 15, 2930. https://doi.org/10.3390/diagnostics15222930
Bacherini D, Rizzo C, Vicini G, Luciani D, Vannozzi L, Virgili G, Giansanti F, Nicolosi C. Characterization of Peripheral Retinal Degenerations and Rhegmatogenous Lesions Using Ultra-Widefield Swept Source OCT Integrated with a Novel Scanning Laser Ophthalmoscope. Diagnostics. 2025; 15(22):2930. https://doi.org/10.3390/diagnostics15222930
Chicago/Turabian StyleBacherini, Daniela, Clara Rizzo, Giulio Vicini, Diego Luciani, Lorenzo Vannozzi, Gianni Virgili, Fabrizio Giansanti, and Cristina Nicolosi. 2025. "Characterization of Peripheral Retinal Degenerations and Rhegmatogenous Lesions Using Ultra-Widefield Swept Source OCT Integrated with a Novel Scanning Laser Ophthalmoscope" Diagnostics 15, no. 22: 2930. https://doi.org/10.3390/diagnostics15222930
APA StyleBacherini, D., Rizzo, C., Vicini, G., Luciani, D., Vannozzi, L., Virgili, G., Giansanti, F., & Nicolosi, C. (2025). Characterization of Peripheral Retinal Degenerations and Rhegmatogenous Lesions Using Ultra-Widefield Swept Source OCT Integrated with a Novel Scanning Laser Ophthalmoscope. Diagnostics, 15(22), 2930. https://doi.org/10.3390/diagnostics15222930








