Prevalence of Diabetes Among First-Time Ophthalmology Patients at a Nonprofit Hospital in Mexico
Abstract
1. Introduction
2. Materials and Methods
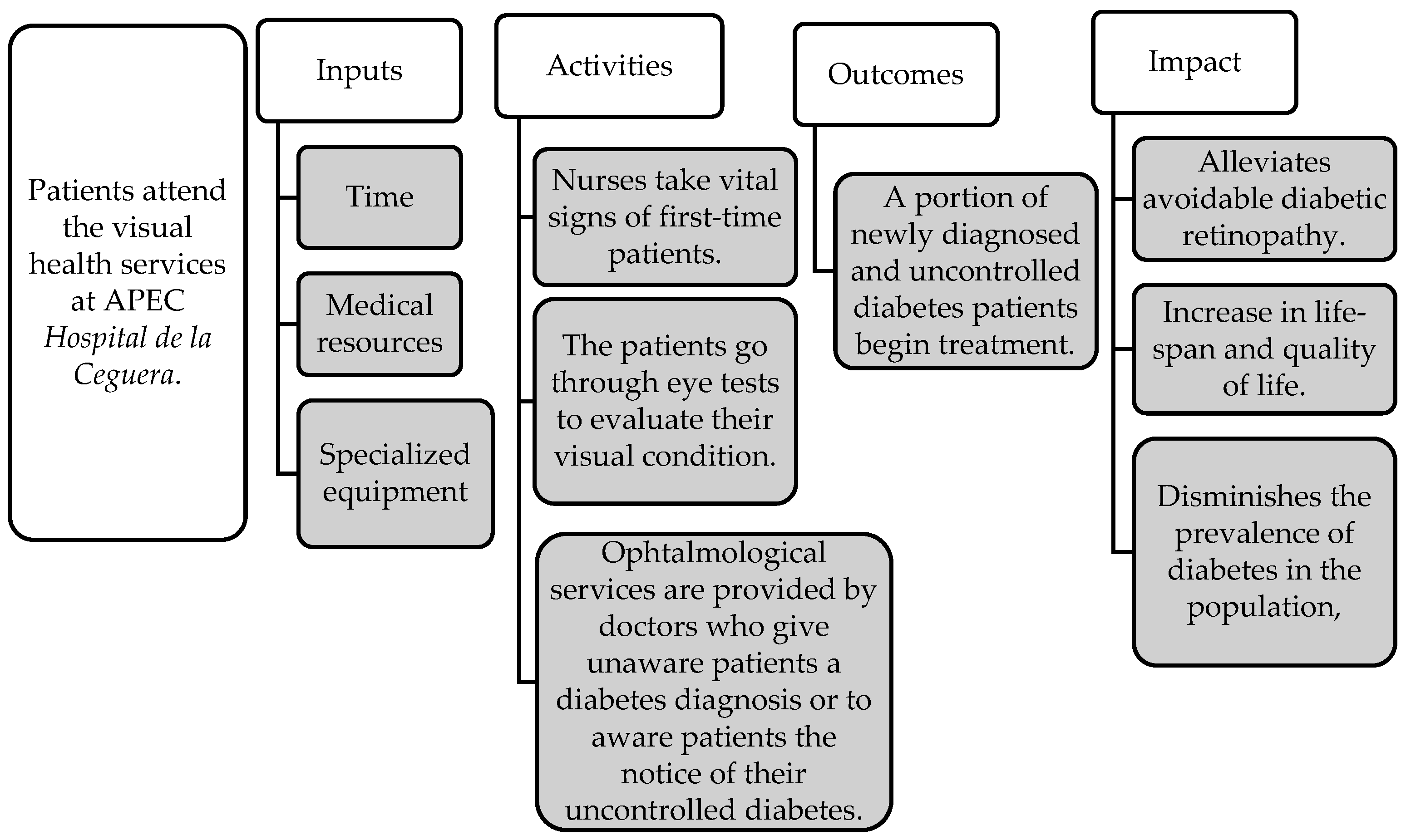
2.1. Theory of Change
2.2. Data and Statistical Analysis
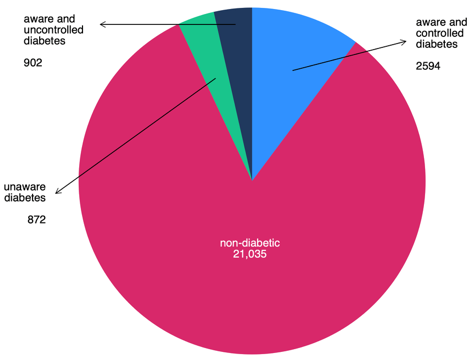
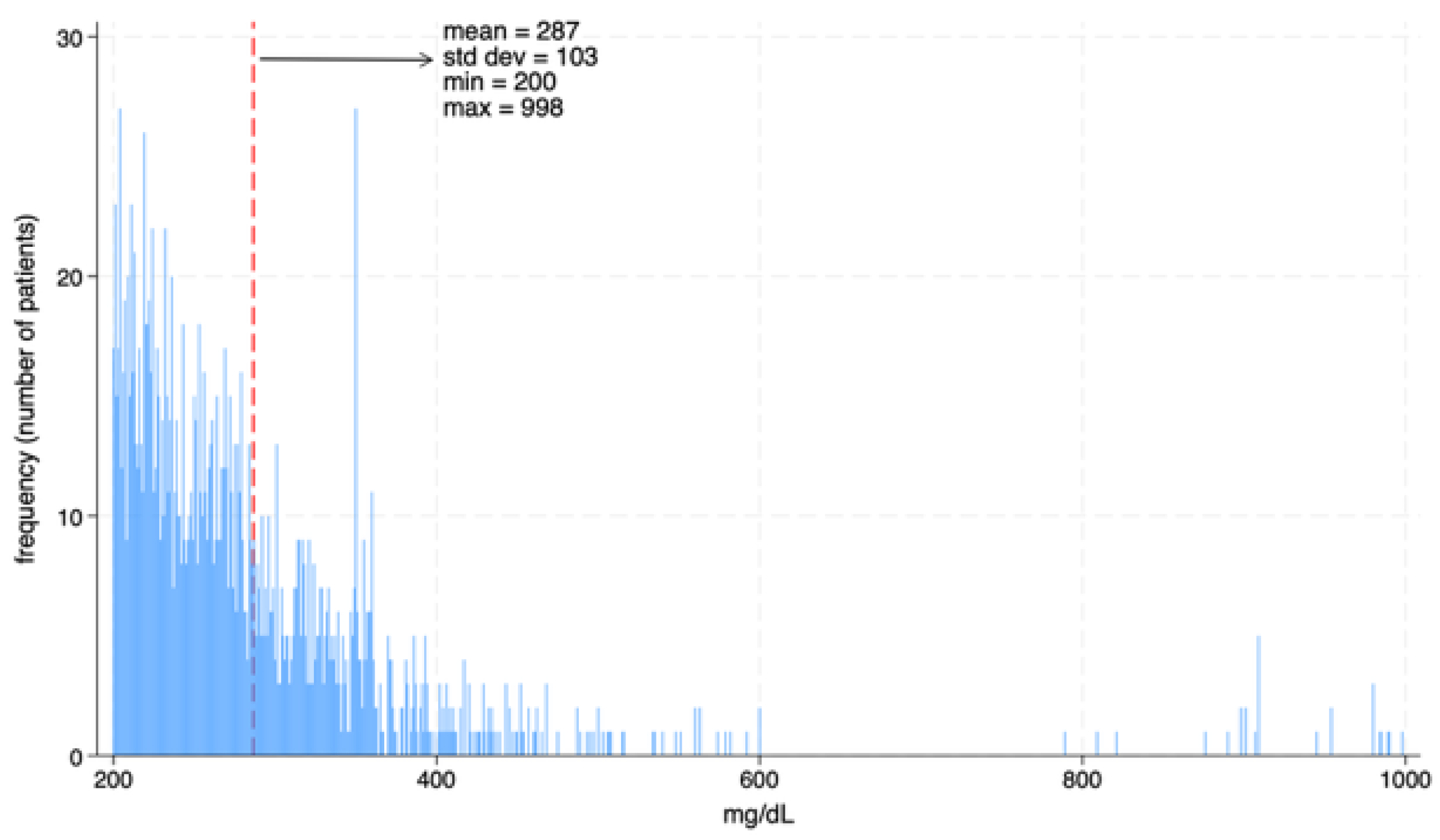
- Uncontrolled diagnosed diabetes: individuals who reported a prior medical diagnosis of diabetes and presented a casual capillary blood glucose level ≥ 200 mg/dL.
- Controlled diagnosed diabetes: individuals with a prior medical diagnosis and a blood glucose level ≤ 200 mg/dL.
- Undiagnosed diabetes: individuals who had never received a diabetes diagnosis but presented a blood glucose level ≥ 200 mg/dL.
2.3. Inputs
| Mean | Std. Dev | |
|---|---|---|
| Time 2 | $8.51 | $13.16 |
| Special equipment 3 | $0.01 | $0.02 |
| Medical resources 4 | $5.96 | $16.66 |
2.4. Outcomes
3. Results
3.1. Benefit–Cost Ratio
3.2. Sensitivity Analysis
- Probability of initiating treatment after diagnosis or notification of uncontrolled diabetes: In the baseline scenario, it is assumed that 74.2% of patients will seek treatment after receiving a new diagnosis or being informed that their diabetes is uncontrolled, based on observed patterns in the dataset. To assess the sensitivity of our results to this parameter, we adjust this probability to 10%, 25%, 50% and 100%, as shown in case (a) of Table 3. The benefit–cost ratio changes by −86.5%, −66.1%, −32.6%, and +34.8%, respectively, relative to the baseline. In contrast, remains virtually unchanged across all these values.
- Disability weights: As previously mentioned, we used an average disability weight (ADW = 0.25) associated with various diabetes-related complications, based on estimates from the Global Burden of Disease Study 2021. To test the sensitivity of the BCRs to this parameter, we replace the baseline ADW with a lower bound of 0.17 and an upper bound of 0.32. As shown in case (b) of Table 3, this results in changes in of −30.4% and +30.6%, respectively. exhibits a similar response to these variations.
- Discount rate: We also evaluate the effect of changing the discount rate. The baseline scenario assumes a 10% discount rate, following the official guidelines for socioeconomic evaluation of investment projects issued by Mexico’s Ministry of Finance. To assess its importance, we adjust the rate to 3%, 5%, and 15%, as shown in case (c) of Table 3. These changes yield variations in of +80.8%, +48.6%, and −26.1%, respectively. remains basically constant, as the discount rate affects both the value of outcomes and the cost of treatment (Equations (1) and (2) above), while the costs of screening per person are considerably low.
- Value per Statistical Life (VSL): Finally, as explained in the Outcomes section above, our baseline scenario uses the VSL of 2.0 million U.S. dollars for Mexico, based on the estimate by Becerra-Pérez et al. [25]. In case (d) of the sensitivity analysis, we vary this parameter to 1.0 million, 1.5 million, and 2.5 million U.S. dollars. The responds with changes of −50.0%, −25.0%, and +25.0%, respectively, while follows a similar proportional pattern. This is so because the VSL enters the BCR linearly in the numerator of the calculation of total benefits.
4. Discussion and Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- WHO. Diabetes [Internet]. 2024. Available online: https://www.who.int/news-room/fact-sheets/detail/diabetes (accessed on 24 May 2025).
- American Diabetes Association. Standards of Care in Diabetes-2025. Diabetes Care [Internet]. 2025, p. 48. Available online: https://diabetesjournals.org/care/issue/48/Supplement_1 (accessed on 24 May 2025).
- International Diabetes Federation. IDF Diabetes Atlas 11th Edition [Internet]. 2025. Available online: https://diabetesatlas.org (accessed on 12 May 2025).
- Basto-Abreu, A.; López-Olmedo, N.; Rojas-Martínez, R.; Aguilar-Salinas, C.A.; Moreno-Banda, G.L.; Carnalla, M.; Rivera-Dommarco, J.A.; Romero-Martínez, M.; Barquera, S.; Barrientos-Gutiérrez, T. Prevalence of prediabetes and diabetes in Mexico: Ensanut 2022. Salud Pública De México 2023, 65. [Google Scholar] [CrossRef]
- González-Villalpando, C.; Dávila-Cervantes, C.A.; Zamora-Macorra, M.; Trejo-Valdivia, B.; González-Villalpando, M.E. Incidence of type 2 diabetes in Mexico. Results of The Mexico City Diabetes Study after 18 years of follow-up. Salud Pública De México 2014, 56, 11–17. [Google Scholar] [CrossRef] [PubMed]
- INEGI. Nota Técnica Estadísticas de Defunciones Registradas (EDR) 2023 [Internet]. November 2024. Available online: https://www.inegi.org.mx/contenidos/programas/edr/doc/defunciones_registradas_2023_nota_tecnica.pdf (accessed on 24 May 2025).
- Shamah-Levy, T.; Lazcano-Ponce, E.C.; Cuevas-Nasu, L.; Romero-Martínez, M.; Gaona-Pineda, E.B.; Gómez-Acosta, L.M.; Mendoza-Alvarado, L.R.; Méndez-Gómez-Humarán, I.; Encuesta Nacional de Salud y Nutrición Continua 2023. Resultados Nacionales [Internet]. Available online: https://ensanut.insp.mx/encuestas/ensanutcontinua2023/doctos/informes/ensanut_23_112024.pdf (accessed on 24 May 2025).
- Basto-Abreu, A.; Reyes-Garcia, A.; Stern, D.; Torres-Ibarra, L.; Rojas-Martinez, R.; Aguilar-Salinas, C.A.; Romero-Martinez, M.; Campos-Nonato, I.; Lopez-Ridaura, R.; Barrientos-Gutierrez, T. Type 2 diabetes srceening and care in Mexico. Salud Pública De México 2024, 66, 530–538. [Google Scholar] [PubMed]
- Bautista Rodríguez, L.M.; Zambrano Plata, G.E. La calidad de vida percibida en pacientes diabéticos tipo 2. Investigación en Enfermería: Imagen y Desarrollo 2015, 17, 131–148. [Google Scholar] [CrossRef]
- Rojas-Martínez, R.; Escamilla-Núñez, C.; Castro-Porras, L.; Gómez-Velasco, D.; Romero-Martínez, M.; Hernández-Serrato, M.I.; López-Ridaura, R.; Díaz, M.Á.; Aguilar-Salinas, C. Detection of prediabetes and diabetes. Salud Pública De México 2024, 66, 520–529. [Google Scholar] [CrossRef]
- World Health Organization. Guidance on Global Monitoring for Diabetes Prevention and CONTROL FRAMEWORK, INDICATORS and Application [Internet]. 2024. Available online: https://www.who.int/publications/i/item/9789240102248 (accessed on 25 May 2025).
- Secretaría de Salud. Norma Oficial Mexicana NOM-015-SSA2-2010, para la prevención, tratamiento y control de la diabetes mellitus. Diario Oficial de la Federación Mexico, 3 November 2010. [Google Scholar]
- Benhamza, M.; Dahlui, M.; Said, M.A. Determining direct, indirect healthcare and social costs for diabetic retinopathy management: A systematic review. BMC Ophthalmol. 2024, 24, 424. [Google Scholar] [CrossRef] [PubMed]
- Vivanco-Rojas, O.; López-Letayf, S.; Londoño-Angarita, V.; Magaña-Guerrero, F.S.; Buentello-Volante, B.; Garfias, Y. Risk Factors for Diabetic Retinopathy in Latin America (Mexico) and the World: A Systematic Review and Meta-Analysis. J. Clin. Med. 2023, 12, 6583. [Google Scholar] [CrossRef] [PubMed]
- Olafsdottir, E.; Andersson, D.K.G.; Dedorsson, I.; Svärdsudd, K.; Jansson, S.P.O.; Stefánsson, E. Early detection of type 2 diabetes mellitus and screening for retinopathy are associated with reduced prevalence and severity of retinopathy. Acta Ophthalmol. 2016, 94, 232–239. [Google Scholar] [CrossRef] [PubMed]
- Nicholls, J.; Lawlor, E.; Neitzert, E.; Goodspeed, T. A Guide to Social Return on Investment [Internet]. The SROI Network. 2012. Available online: https://socialvalueselfassessmenttool.org/wp-content/uploads/intranet/758/pdf-guide.pdf (accessed on 24 May 2025).
- Instituto Nacional de Estadística y Geografía (INEGI). Principales resultados del Censo de Población y Vivienda 2020. Estados Unidos Mexicanos [Internet], 2022. Available online: https://www.inegi.org.mx/contenidos/productos/prod_serv/contenidos/espanol/bvinegi/productos/nueva_estruc/702825198060.pdf (accessed on 31 October 2025).
- World Health Organization (WHO). Obesity and Overweight 2025. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 31 October 2025).
- International Diabetes Federation. IDF Diabetes Atlas, 10th ed.; International Diabetes Federation: Amsterdam, The Netherlands, 2021. [Google Scholar]
- Ross, S.A.; Westerfield, R.W.; Jaffe, J.F. Finanzas Corporativas, 5th ed.; McGraw-Hill: Mexico City, Mexico, 1999; pp. 1–1049. [Google Scholar]
- World Bank. World Development Indicators [Internet]. 2023. Available online: https://databank.worldbank.org/source/world-development-indicators (accessed on 30 March 2025).
- INEGI Esperanza de vida al nacimiento por entidad federativa según sexo, serie anual de 2010 a 2025 [Internet]. 2023. Available online: https://www.inegi.org.mx/app/tabulados/interactivos/?pxq=Mortalidad_Mortalidad_09_25171f46-857b-4d3a-aeae-c61235598f32 (accessed on 30 March 2025).
- SHCP. Oficio No. 400.1.410.22.234. 2022. Determinación de la Tasa Social de Descuento Aplicable a Programas y Proyectos de Inversión. Available online: https://www.gob.mx/shcp/documentos/tasa-social-de-descuento-tsd (accessed on 9 March 2023).
- Institute for Health Metrics and Evaluation (IHME). Global Burden of Disease 2021: Findings from the GBD 2021 Study; IHME: Seattle, WA, USA, 2024. [Google Scholar]
- Becerra-Pérez, L.A.; Ramos-Alvarez, R.A.; DelaCruz, J.J.; García-Páez, B. Value per Statistical Life at the Sub-National Level as a Tool for Assessing Public Health and Environmental Problems. Inq. J. Health Care Organ. Provis. Financ. 2024, 61, 00469580241246476. [Google Scholar] [CrossRef] [PubMed]
- OECD. Mortality Risk Valuation in Environment, Health and Transport Policies; OECD Publishing: Paris, France, 2012. [Google Scholar]
- Banco de México. Economic Information System (SIE)/Exchange Rates and Auctions Historical Information [Internet]. 2021. Available online: https://www.banxico.org.mx/SieInternet/consultarDirectorioInternetAction.do?sector=6&idCuadro=CF102&accion=consultarCuadro&locale=en (accessed on 27 September 2025).
- Prado-Serrano, A.; Marilu, D.; Guido-Jiménez, A.; Jiny, D.; Camas-Benítez, T. Prevalencia de retinopatía diabética en población mexicana. Rev. Mex. De Oftalmol. 2009, 83, 261–266. [Google Scholar]
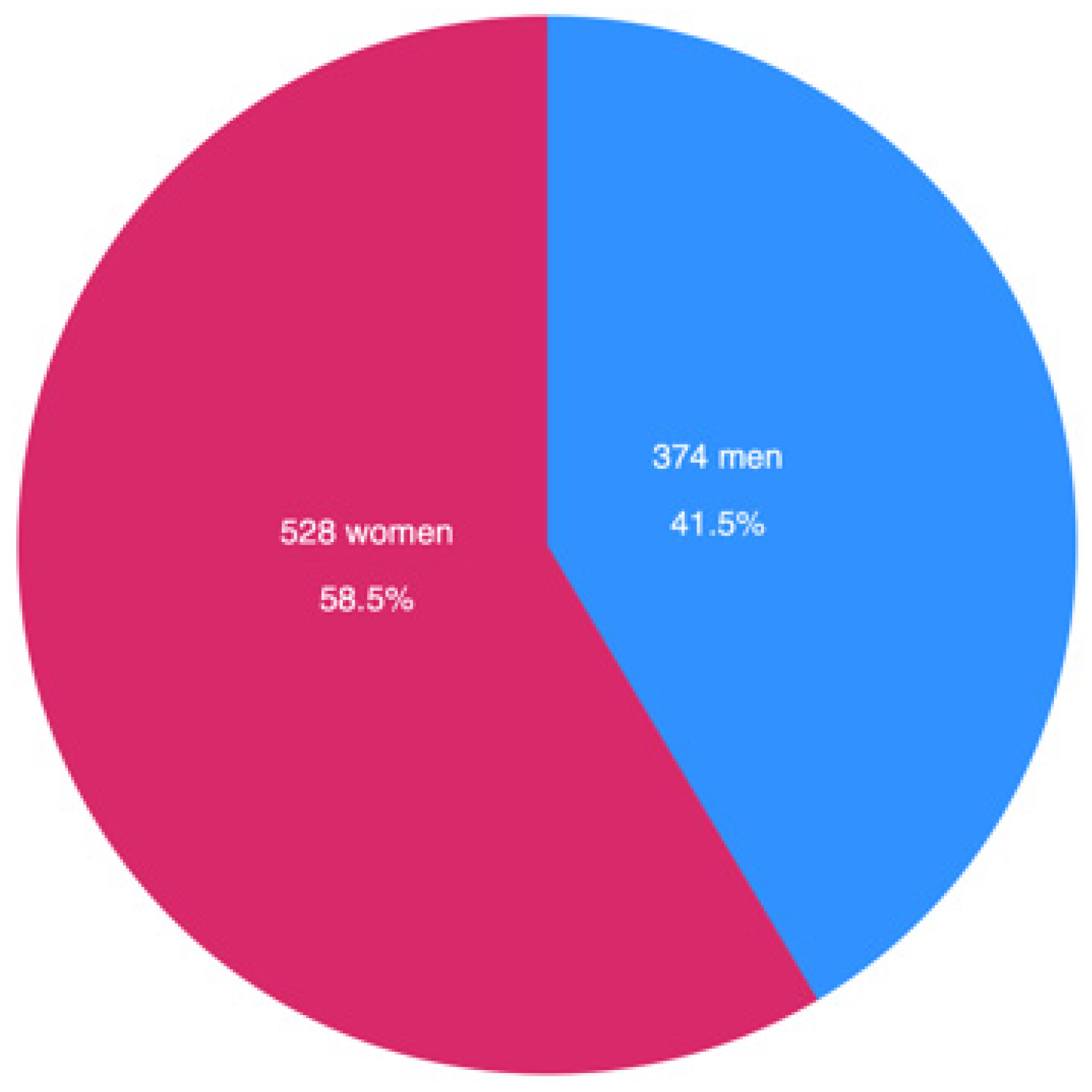
| Variable | Observations | Mean | Std. Dev | 95% Confidence Interval |
|---|---|---|---|---|
| Woman 1 | 25,411 | 0.63 | 0.48 | 0.63–0.64 |
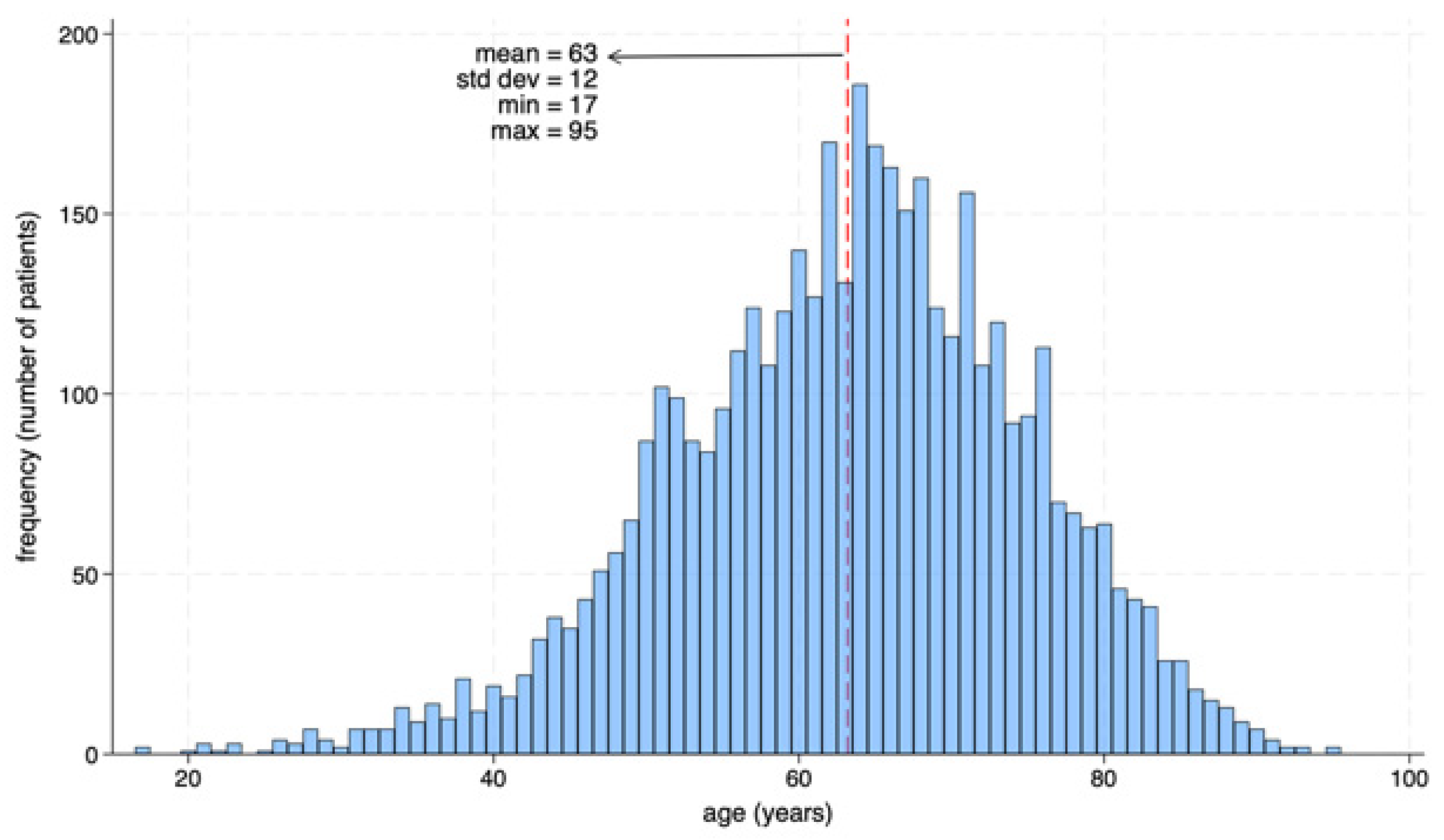
| Age (years) | 25,411 | 55.09 | 18.74 | 54.86–55.32 |
| Height (meters) | 12,512 | 1.59 | 0.14 | 1.589–1.594 |
| Weight (kilograms) | 12,144 | 70.56 | 15.79 | 70.28–70.84 |
| Body Mass Index (kgs/m2) | 9501 | 28.20 | 16.07 | 27.88–28.52 |
| Heart Rate (beats per minute) | 21,121 | 75.08 | 12.48 | 74.91–75.25 |
| Respiratory Rate (breaths per minute) | 13,240 | 22.35 | 17.88 | 22.05–22.66 |
| Capillary glycemia (mg/dL) 2 | 15,081 | 129.98 | 72.34 | 129.46–131.76 |
| Capillary glycemia > 200 3 | 15,081 | 0.12 | 0.32 | 0.11–0.12 |
| Case | Parameter | BCRAPEC | BCRFULL | |||||
|---|---|---|---|---|---|---|---|---|
| Mean | Mean Difference vs. Baseline Scenario (%) | 95% Confidence Interval | Mean | Mean Difference vs. Baseline Scenario (%) | 95% Confidence Interval | |||
| (a) | Probability of initiating treatment after diagnosis or notification of uncontrolled diabetes | 10% | 73.1 | −86.5 | 69.76–76.41 | 8.9 | −0.8 | 8.85–8.93 |
| 25% | 182.7 | −66.3 | 174.40–191.04 | 8.9 | −0.2 | 8.89–8.98 | ||
| 50% | 365.4 | −32.6 | 348.81–382.07 | 9.0 | −0.1 | 8.91–9.00 | ||
| 100% | 730.9 | 34.8 | 697.61–764.14 | 9.0 | 0.0 | 8.92–9.01 | ||
| (b) | Disability weight | 0.17 | 377.6 | −30.4 | 360.45–394.83 | 6.2 | −30.4 | 6.21–6.27 |
| 0.32 | 708.0 | 30.6 | 675.80–740.25 | 11.7 | 30.6 | 11.64–11.75 | ||
| (c) | Discount rate | 3% | 980.2 | 80.8 | 934.54–1025.93 | 9.0 | 0.0 | 8.92–9.01 |
| 5% | 805.8 | 48.6 | 768.63–842.93 | 9.0 | 0.0 | 8.92–9.01 | ||
| 15% | 400.8 | −26.1 | 382.66–418.97 | 9.0 | 0.0 | 8.91–9.00 | ||
| (d) | Value per Statistical Life (VSL) for Mexico (million USD) | $1.0 | 271.2 | −50.0 | 258.81–283.50 | 4.5 | −50.0 | 4.46–4.50 |
| $1.5 | 406.7 | −25.0 | 388.22–425.24 | 6.7 | −25.0 | 6.69–6.75 | ||
| $2.5 | 677.9 | 25.0 | 647.04–708.74 | 11.2 | 25.0 | 11.14–11.25 | ||
| Average | 498.5 | −8.1 | 8.6 | −98.4 | ||||
| Std. Dev. | 276.1 | 2.0 | ||||||
| Minimum | 73.4 | −86.5 | 4.5 | −50.0 | ||||
| Maximum | 980.2 | 80.8 | 11.7 | 30.6 | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sánchez-Huerta, V.; González Suriel, M.L.; Randolph, H.; Barragán Álvarez, M.J.; Aleman-Castilla, B. Prevalence of Diabetes Among First-Time Ophthalmology Patients at a Nonprofit Hospital in Mexico. Diagnostics 2025, 15, 2922. https://doi.org/10.3390/diagnostics15222922
Sánchez-Huerta V, González Suriel ML, Randolph H, Barragán Álvarez MJ, Aleman-Castilla B. Prevalence of Diabetes Among First-Time Ophthalmology Patients at a Nonprofit Hospital in Mexico. Diagnostics. 2025; 15(22):2922. https://doi.org/10.3390/diagnostics15222922
Chicago/Turabian StyleSánchez-Huerta, Valeria, Mary Lady González Suriel, Héctor Randolph, María José Barragán Álvarez, and Benjamin Aleman-Castilla. 2025. "Prevalence of Diabetes Among First-Time Ophthalmology Patients at a Nonprofit Hospital in Mexico" Diagnostics 15, no. 22: 2922. https://doi.org/10.3390/diagnostics15222922
APA StyleSánchez-Huerta, V., González Suriel, M. L., Randolph, H., Barragán Álvarez, M. J., & Aleman-Castilla, B. (2025). Prevalence of Diabetes Among First-Time Ophthalmology Patients at a Nonprofit Hospital in Mexico. Diagnostics, 15(22), 2922. https://doi.org/10.3390/diagnostics15222922







