Assessing Hemodynamic Changes During Locoregional Anesthesia in Cesarean Section: The Role of USCOM®
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethics
2.2. Statistics
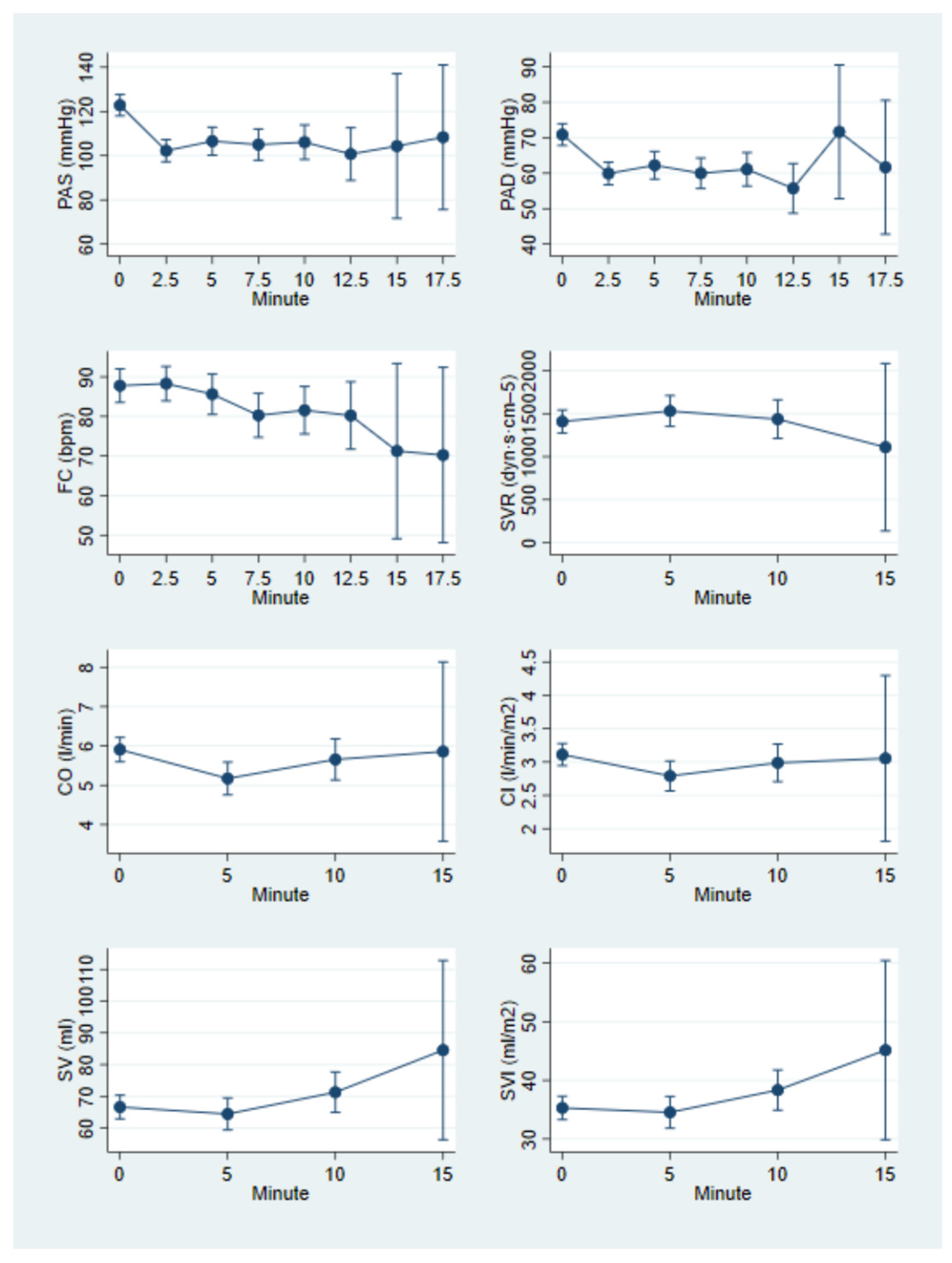
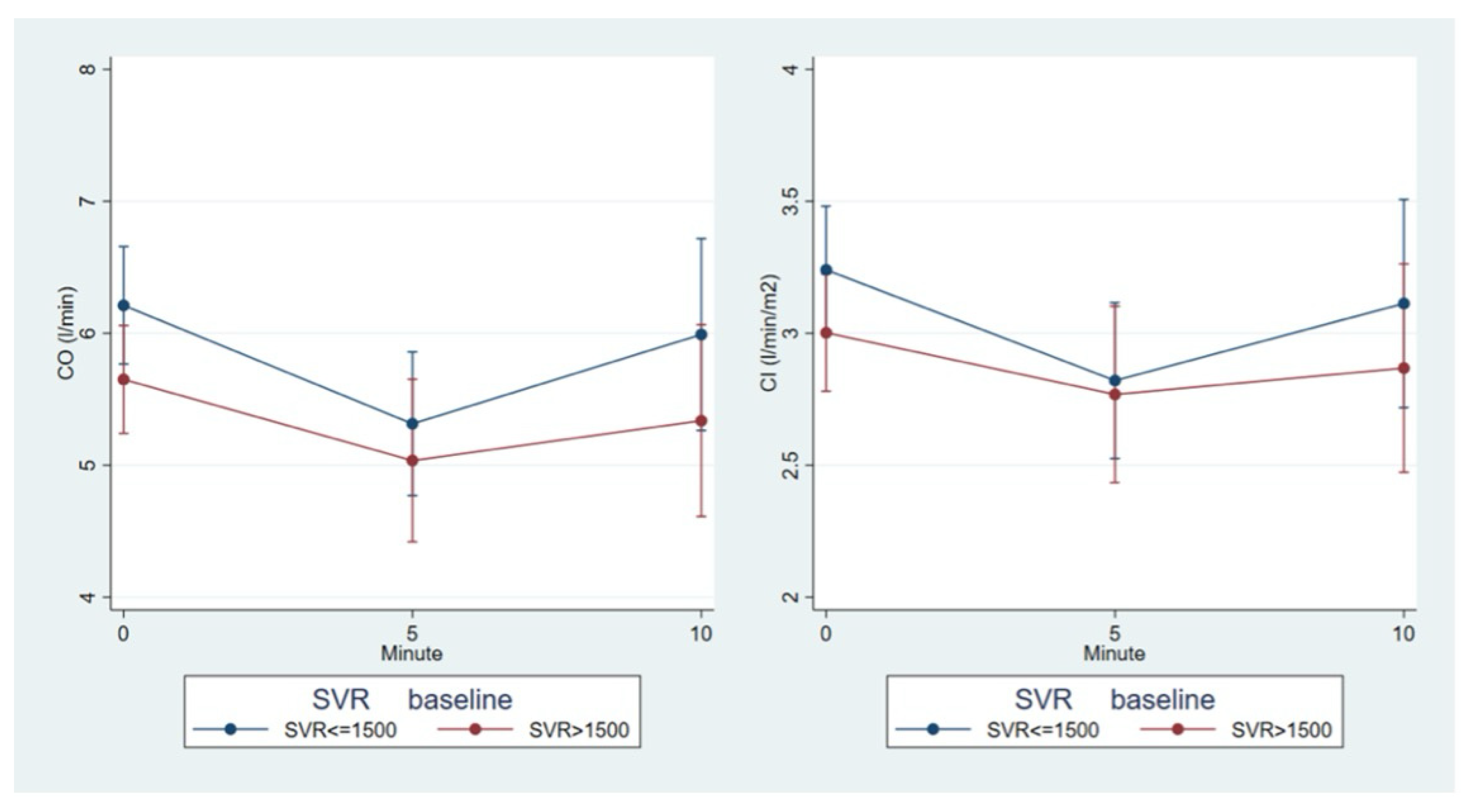
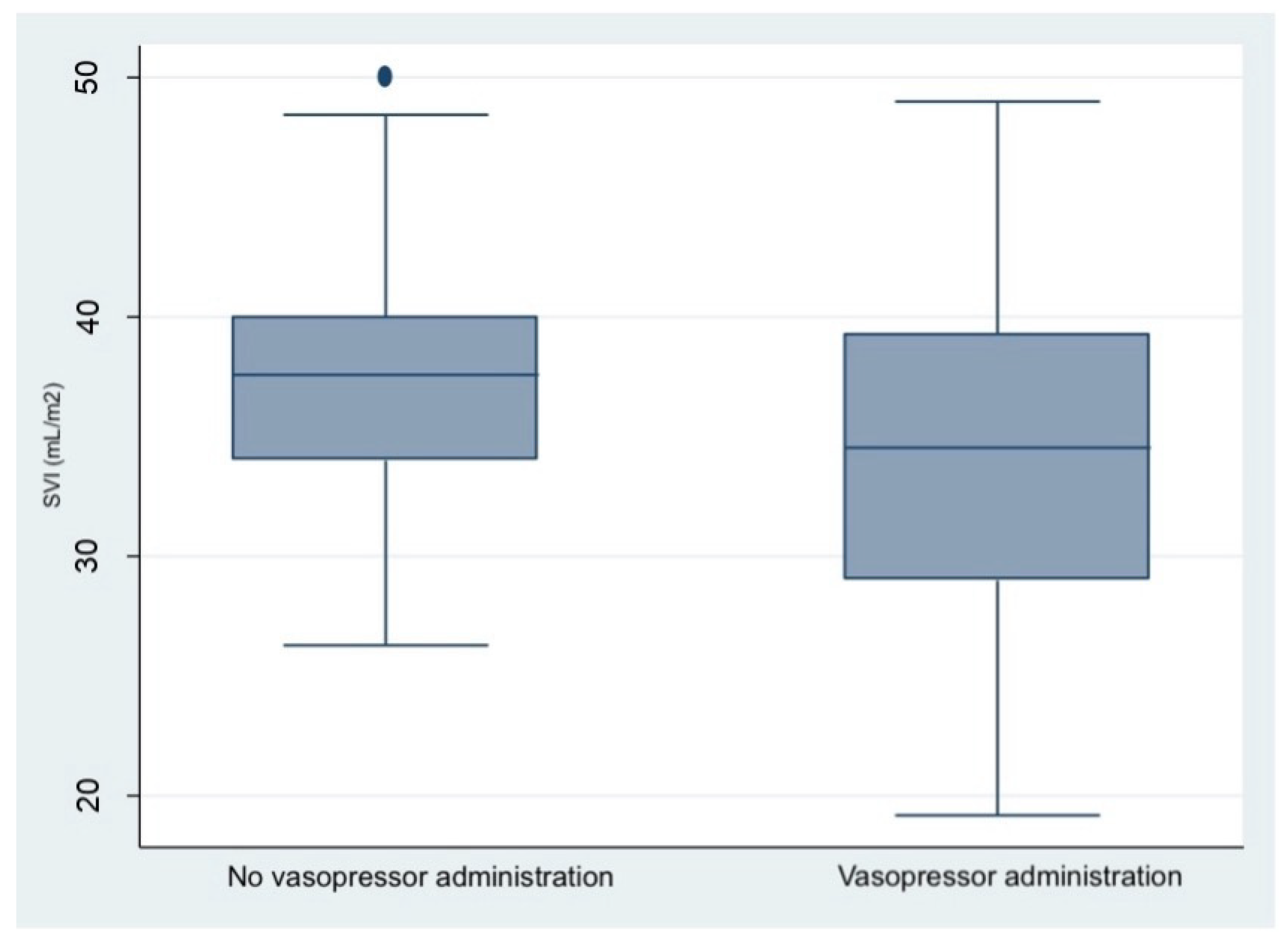
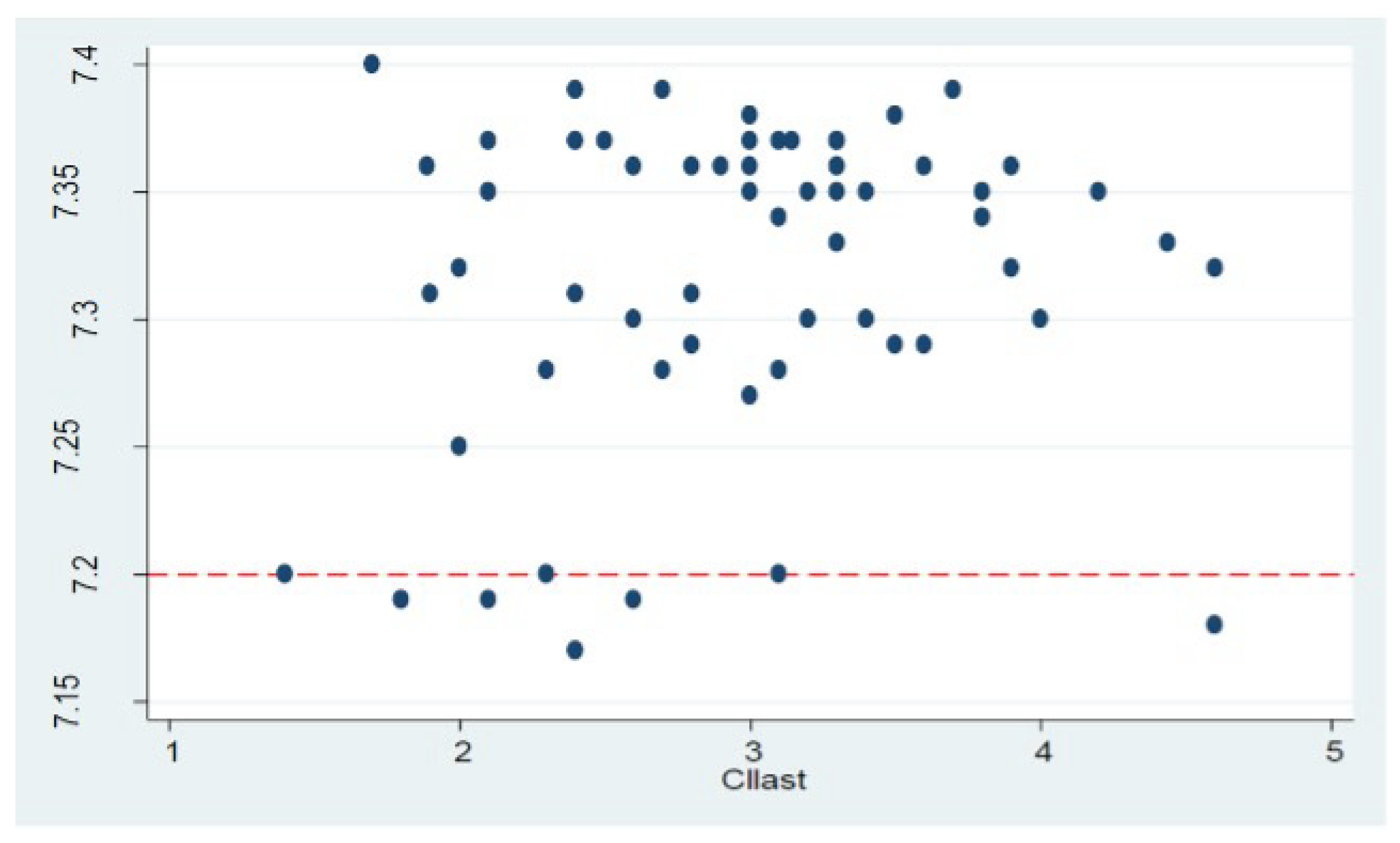
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| CO | Cardiac Output |
| SV | Stroke Volume |
| HR | Heart Rate |
| LRA | Locoregional anesthesia |
| USCOM | Ultrasonic Cardiac Output Monitor |
| CI | Cardiac Index |
| SVI | Stroke Volume Index |
| SVR | Systemic vascular resistance |
References
- Vinayagam, D.; Thilaganathan, B.; Stirrup, O.; Mantovani, E.; Khalil, A. Maternal hemodynamics in normal pregnancy: Reference ranges and role of maternal characteristics. Ultrasound Obstet. Gynecol. 2018, 51, 665–671. [Google Scholar] [CrossRef]
- DeVore, G.R.; Polanco, B. Assessing maternal cardiac function by obstetricians: Technique and reference ranges. Am. J. Obstet. Gynecol. 2023, 229, 155.e1–155.e18. [Google Scholar] [CrossRef]
- Valensise, H.; Tiralongo, G.M.; Pisani, I.; Farsetti, D.; Lo Presti, D.; Gagliardi, G.; Basile, M.R.; Novelli, G.P.; Vasapollo, B. Maternal hemodynamics early in labor: A possible link with obstetric risk? Ultrasound Obstet. Gynecol. 2018, 51, 509–513. [Google Scholar] [CrossRef]
- Montaguti, E.; Di Donna, G.; Youssef, A.; Pilu, G. Hypertensive disorders and maternal hemodynamic changes in pregnancy: Monitoring by USCOM® device. J. Med. Ultrason. 2022, 49, 405–413. [Google Scholar] [CrossRef]
- Melchiorre, K.; Thilaganathan, B. Maternal cardiac function in preeclampsia. Curr. Opin. Obstet. Gynecol. 2011, 23, 440–447. [Google Scholar] [CrossRef] [PubMed]
- Mancuso, A.; De Vivo, A.; Giacobbe, A.; Priola, V.; Maggio Savasta, L.; Guzzo, M.; De Vivo, D.; Mancuso, A. General versus spinal anaesthesia for elective caesarean sections: Effects on neonatal short-term outcome. A prospective randomised study. J. Matern. Fetal Neonatal Med. 2010, 23, 1114–1118. [Google Scholar] [CrossRef]
- Dilesh, P.K.; Eapen, S.; Kiran, S.; Chopra, V. A comparison of intrathecal dexmedetomidine verses intrathecal fentanyl with epidural bupivacaine for combined spinal epidural labor analgesia. J. Obstet. Anaesth. Crit. Care 2014, 4, 69–74. [Google Scholar] [CrossRef]
- Langesæter, E.; Dyer, R.A. Maternal haemodynamic changes during spinal anaesthesia for caesarean section. Curr. Opin. Anaesthesiol. 2011, 24, 242–248. [Google Scholar] [CrossRef]
- Cooper, D.W.; Carpenter, M.; Mowbray, P.; Desira, W.R.; Ryall, D.M.; Kokri, M.S. Fetal and maternal effects of phenylephrine and ephedrine during spinal anesthesia for cesarean delivery. Anesthesiology 2002, 97, 1582–1590. [Google Scholar] [CrossRef]
- Petropoulos, G.; Siristatidis, C.; Salamalekis, E.; Creatsas, G. Spinal and epidural versus general anesthesia for elective cesarean section at term: Effect on the acid-base status of the mother and newborn. J. Matern. Fetal Neonatal Med. 2003, 13, 260–266. [Google Scholar]
- Tawfik, M.M.; Hayes, S.M.; Jacoub, F.Y.; Badran, B.A.; Gohar, F.M.; Shabana, A.M.; Abdelkhalek, M.; Emara, M.M. Comparison between colloid preload and crystalloid co-load in cesarean section under spinal anesthesia: A randomized controlled trial. Int. J. Obstet. Anesth. 2014, 23, 317–323. [Google Scholar] [CrossRef]
- Allen, T.K.; George, R.B.; White, W.D.; Muir, H.A.; Habib, A.S. A double-blind, placebo-controlled trial of four fixed rate infusion regimens of phenylephrine for hemodynamic support during spinal anesthesia for cesarean delivery. Anesth. Analg. 2010, 111, 1221–1229. [Google Scholar] [CrossRef]
- Mulder, E.; Basit, S.; Oben, J.; van Kuijk, S.; Ghossein-Doha, C.; Spaanderman, M. Accuracy and precision of USCOM versus transthoracic echocardiography before and during pregnancy. Pregnancy Hypertens. 2019, 17, 138–143. [Google Scholar] [CrossRef]
- Montaguti, E.; Cofano, M.; Diglio, J.; Fiorentini, M.; Pellegrino, A.; Lenzi, J.; Battaglia, C.; Pilu, G. The prediction of hypertensive disorders by maternal hemodynamic assessment in the first trimester of pregnancy. J. Matern. Fetal Neonatal Med. 2023, 36, 2198063. [Google Scholar] [CrossRef] [PubMed]
- Kalafat, E.; Barratt, I.; Nawaz, A.; Thilaganathan, B.; Khalil, A. Maternal cardiovascular function and risk of intrapartum fetal compromise in women undergoing induction of labor: Pilot study. Ultrasound Obstet. Gynecol. 2020, 56, 233–239. [Google Scholar] [CrossRef] [PubMed]
- Snijders, T.; Bosker, R. Multilevel Analysis: An Introduction to Basic and Advanced Multilevel Modeling; Sage Publications: Thousand Oaks, CA, USA, 1999. [Google Scholar]
- Tiralongo, G.M.; Presti, D.L.; Pisani, I.; Gagliardi, G.; Scala, R.L.; Novelli, G.P.; Vasapollo, B.; Andreoli, A.N.; Valensise, H. Assessment of total vascular resistance and total body water in normotensive women during the first trimester of pregnancy. A key for the prevention of preeclampsia. Pregnancy Hypertens. 2015, 5, 193–197. [Google Scholar] [CrossRef] [PubMed]
- Kinsella, S.M.; Carvalho, B.; Dyer, R.A.; Fernando, R.; McDonnell, N.; Mercier, F.J.; Palanisamy, A.; Sia, A.T.H.; Van de Velde, M.; Vercueil, A. International consensus statement on the management of hypotension with vasopressors during caesarean section under spinal anaesthesia. Anaesthesia 2018, 73, 71–92. [Google Scholar] [CrossRef]
- Xiao, W.; Duan, Q.; Zhao, L.; Chi, X.; Wang, F.; Ma, D.; Wang, T. Goal-directed fluid therapy may improve hemodynamic stability in parturient women under combined spinal epidural anesthesia for cesarean section and newborn well-being. J. Obstet. Gynaecol. Res. 2015, 41, 1547–1555. [Google Scholar] [CrossRef]
- Lee, A.; Ngan Kee, W.D.; Gin, T. A quantitative, systematic review of randomized controlled trials of ephedrine versus phenylephrine for the management of hypotension during spinal anesthesia for cesarean delivery. Anesth. Analg. 2002, 94, 920–926. [Google Scholar] [CrossRef]
- Yin, O.; Woods, A.; Koos, B.; DeVore, G.; Afshar, Y. Central hemodynamics are associated with fetal outcomes in pregnancies of advanced maternal age. Pregnancy Hypertens. 2020, 19, 67–73. [Google Scholar] [CrossRef]
- Valensise, H.; Lo Presti, D.; Tiralongo, G.M.; Pisani, I.; Gagliardi, G.; Vasapollo, B.; Frigo, M.G. Foetal heart rate deceleration with combined spinal-epidural analgesia during labour: A maternal haemodynamic cardiac study. J. Matern. Fetal Neonatal Med. 2016, 29, 1980–1986. [Google Scholar] [CrossRef]
- Cenkowski, M.J.; Maguire, D.; Kowalski, S.; Gurashi, F.A.A.; Funk, D. Hemodynamic effects of low-dose bupivacaine spinal anesthesia for cesarean section: A randomized controlled trial. Saudi J. Anaesth. 2019, 13, 208. [Google Scholar] [CrossRef] [PubMed]
| Baseline Anthropometric Characteristics and Hemodynamic Parameters | n = 60 |
|---|---|
| Age, years | 36.2 ± 6.1 [31, 41] |
| BMI, kg/m2 | 28.0 ± 3.9 [25.7, 29.6] |
| BSA, m2 | 1.88 ± 0.16 [1.77, 1.97] |
| Heart rate, bpm | 85.9 ± 12.6 [77, 96.5] |
| Systolic blood pressure, mmHg | 127.7 ± 13.2 [120, 137] |
| Diastolic blood pressure, mmHg | 78.3 ± 10.7 [70, 84] |
| Cardiac output, L/min | 5.2 ± 1.3 [4.5, 6.1] |
| Cardiac index, L/min/m2 | 2.8 ± 0.7 [2.4, 3.1] |
| Stroke volume, mL | 67.4 ± 13.3 [58, 77] |
| Stroke volume index, mL/m2 | 35.8 ± 6.8 [32, 40] |
| Systemic vascular resistance, dyn·s·cm−5 | 1595 ± 440.5 [1331, 1807.5] |
| Arterial pH at birth | 7.31 ± 0.06 [7.17, 7.4] |
| Venous pH at birth | 7.28 ± 0.06 [7.02, 7.38] |
| Arterial BE at birth | −1.7 ± 2.5 [−7.4, 3.0] |
| Venous BE at birth | −2.0 ± 2.3 [−9.9, 3.0] |
| Baseline Anthropometric Characteristics and Hemodynamic Parameters | No Vasopressor Therapy n = 22 | Vasopressor Therapy n = 38 | p-Value |
|---|---|---|---|
| Age, years | 36.2 ± 6.4 | 36.2 ± 6.0 | 0.992 |
| Weight, kg | 73.7 ± 10.6 | 77.4 ± 11.3 | 0.208 |
| BMI, kg/m2 | 27.0 ± 3.6 | 28.6 ± 3.9 | 0.129 |
| BSA, m2 | 1.88 ± 0.15 | 1.89 ± 0.16 | 0.855 |
| Heart rate, bpm | 84.6 ± 13.9 | 86.6 ± 11.9 | 0.559 |
| Systolic blood pressure, mmHg | 129.4 ± 11.7 | 126.6 ± 14.1 | 0.443 |
| Diastolic blood pressure, mmHg | 80.4 ± 8.9 | 77.1 ± 11.6 | 0.243 |
| Cardiac output, L/min | 5.3 ± 1.3 | 5.2 ± 1.3 | 0.623 |
| Cardiac index, L/min/m2 | 2.8 ± 0.7 | 2.7 ± 0.7 | 0.447 |
| Stroke volume, mL | 70.1 ± 12.8 | 65.3 ± 13.3 | 0.122 |
| Stroke volume index, mL/m2 | 37.9 ± 6.7 | 34.5 ± 6.6 | 0.050 |
| Systemic vascular resistance, dyn·s·cm−5 | 1511 ± 310 | 1643 ± 498 | 0.212 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lambertini, A.; Doroldi, S.; Mucci, S.M.; Porzio, S.; Caramelli, F.; Pilu, G.; Montaguti, E. Assessing Hemodynamic Changes During Locoregional Anesthesia in Cesarean Section: The Role of USCOM®. Diagnostics 2025, 15, 2846. https://doi.org/10.3390/diagnostics15222846
Lambertini A, Doroldi S, Mucci SM, Porzio S, Caramelli F, Pilu G, Montaguti E. Assessing Hemodynamic Changes During Locoregional Anesthesia in Cesarean Section: The Role of USCOM®. Diagnostics. 2025; 15(22):2846. https://doi.org/10.3390/diagnostics15222846
Chicago/Turabian StyleLambertini, Agnese, Sara Doroldi, Stefania Maria Mucci, Silvia Porzio, Fabio Caramelli, Gianluigi Pilu, and Elisa Montaguti. 2025. "Assessing Hemodynamic Changes During Locoregional Anesthesia in Cesarean Section: The Role of USCOM®" Diagnostics 15, no. 22: 2846. https://doi.org/10.3390/diagnostics15222846
APA StyleLambertini, A., Doroldi, S., Mucci, S. M., Porzio, S., Caramelli, F., Pilu, G., & Montaguti, E. (2025). Assessing Hemodynamic Changes During Locoregional Anesthesia in Cesarean Section: The Role of USCOM®. Diagnostics, 15(22), 2846. https://doi.org/10.3390/diagnostics15222846






