Periprosthetic Joint Infection Caused by Trichoderma: Is It Plausible?
Abstract
1. Introduction
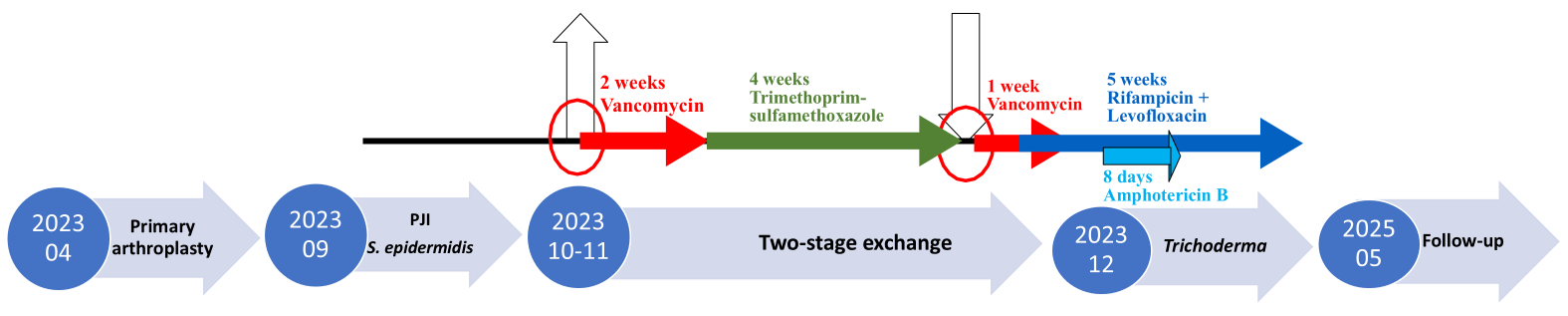
2. Case Report
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Burzio, C.; Balzani, E.; Montrucchio, G.; Trompeo, A.C.; Corcione, S.; Brazzi, L. Trichoderma spp.-Related Pneumonia: A Case Report in Heart–Lung Transplantation Recipient and a Systematic Literature Review. J. Fungi 2023, 9, 195. [Google Scholar] [CrossRef] [PubMed]
- Sal, E.; Stemler, J.; Salmanton-García, J.; Falces-Romero, I.; Kredics, L.; Meyer, E.; Würstl, B.; Lass-Flörl, C.; Racil, Z.; Klimko, N.; et al. Invasive Trichoderma spp. Infections: Clinical Presentation and Outcome of Cases from the Literature and the FungiScope® Registry. J. Antimicrob. Chemother. 2022, 77, 2850–2858. [Google Scholar] [CrossRef] [PubMed]
- Trabelsi, S.; Hariga, D.; Khaled, S. First Case of Trichoderma longibrachiatum Infection in a Renal Transplant Recipient in Tunisia and Review of the Literature. Tunis. Med. 2010, 88, 52–57. [Google Scholar] [PubMed]
- Walsh, T.J.; Groll, A.; Hiemenz, J.; Fleming, R.; Roilides, E.; Anaissie, E. Infections due to emerging and uncommon medically important fungal pathogens. Clin. Microbiol. Infect. 2004, 10, 48–66. [Google Scholar] [CrossRef] [PubMed]
- Dos Santos, U.R.; Dos Santos, J.L. Trichoderma after crossing kingdoms: Infections in human populations. J. Toxicol. Environ. Health Part B 2023, 26, 97–126. [Google Scholar] [CrossRef] [PubMed]
- McNally, M.; Sousa, R.; Wouthuyzen-Bakker, M.; Chen, A.F.; Soriano, A.; Vogely, H.C.; Clauss, M.; Higuera, C.A.; Trebše, R. The EBJIS definition of periprosthetic joint infection. Bone Jt. J. 2021, 103-B, 18–25. [Google Scholar] [CrossRef] [PubMed]
- Sandoval-Denis, M.; Sutton, D.A.; Cano-Lira, J.F.; Gené, J.; Fothergill, A.W.; Wiederhold, N.P.; Guarro, J. Phylogeny of the clinically relevant species of the emerging fungus Trichoderma and their antifungal susceptibilities. J. Clin. Microbiol. 2014, 52, 2112–2125. [Google Scholar] [CrossRef] [PubMed]
- Tascini, C.; Cardinali, G.; Barletta, V.; Di Paolo, A.; Leonildi, A.; Zucchelli, G.; Corte, L.; Colabella, C.; Roscini, L.; Consorte, A.; et al. First Case of Trichoderma longibrachiatum CIED (Cardiac Implantable Electronic Device)-Associated Endocarditis in a Non-Immunocompromised Host: Biofilm Removal and Diagnostic Problems in the Light of the Current Literature. Mycopathologia 2016, 181, 297–303. [Google Scholar] [CrossRef] [PubMed]
- Bustamante-Labarta, M.H.; Caramutti, V.; Allende, G.N.; Weinschelbaum, E.; Torino, A.F. Unsuspected Embolic Fungal Endocarditis of an Aortic Conduit Diagnosed by Transesophageal Echocardiography. J. Am. Soc. Echocardiogr. 2000, 13, 953–954. [Google Scholar] [CrossRef] [PubMed]
- Hatvani, L.; Homa, M.; Chenthamara, K.; Cai, F.; Kocsubé, S.; Atanasova, L.; Mlinaric-Missoni, E.; Manikandan, P.; Revathi, R.; Dóczi, I.; et al. Agricultural Systems as Potential Sources of Emerging Human Mycoses Caused by Trichoderma: A Successful, Common Phylotype of Trichoderma longibrachiatum in the Frontline. FEMS Microbiol. Lett. 2019, 366, fnz246. [Google Scholar] [CrossRef] [PubMed]
- Piens, M.-A.; Célard, M.; de Monbrison, F.; Grando, J.; Vandenesch, F.; Mottolese, C.; Picot, S. Trichoderma infection of cerebrospinal fluid shunt device in a non-immunocompromised patient. J. Mycol. Méd. 2004, 14, 49–51. [Google Scholar]
- Robertson, M.H. Fungi in fluids—A hazard of intravenous therapy. J. Med. Microbiol. 1970, 3, 99–102. [Google Scholar] [CrossRef] [PubMed]
| Clinical Case Report (Author, Year) | Patient Sex and Age | Immuno- Suppression | Microorganism, Samples Positive | Infected Organ/Device | Other Concomitant Pathogens, Samples Positive | Antifungal Treatment | Surgery | Outcome |
|---|---|---|---|---|---|---|---|---|
| Tascsini C 2016 [8] | Male, 30 years old | No | Trichoderma longibrachiatum; Tips of the leads (only sonication) | Implantable cardioverter-defibrillator–endocarditis | Staphylococcus epidermidis; Tips of the leads (standard and sonication) and blood | Oral voriconazole 200 mg bid (after 400 mg bid loading, day 1), 3 d → 200 mg bid IV, 2 d—both stopped due to subtherapeutic levels; switched to liposomal amphotericin B 3 mg/kg/day IV, 25 d, stopped for renal insufficiency | Implantable cardioverter-defibrillator removal and reimplantation (day 10) | Recovered |
| Bustamante-Labarta MH 2000 [9] | Male, 66 years old | No | Trichoderma spp.; Removed material; Number of cultures NA; Blood cultures negative | Aortic graft-endocarditis | No | Antifungal drugs in the postoperative period; Antifungal and duration: NA | The graft was replaced | Recovered |
| Hatvani L 2019 [10] | Male, 71 years old | Not reported | Trichoderma bissettii; Removed aortic valve; Number of cultures NA; Blood cultures negative for fungi | Prosthetic aortic valve endocarditis | Not reported | Voriconazole IV; Duration: NA | Aortic valve removal | Died due to another cause |
| Hatvani L 2019 [10] | Female, 75 years old | Not reported | Trichoderma bissettii; Fluid from the implant; Number of cultures NA | Pacemaker | Not reported | NA | The device was extracted | NA |
| Piens MA 2004 [11] | Male, 61 years old | No | Trichoderma reesei; Cerebrospinal fluid and shunt device culture | Cerebrospinal fluid shunt device | Not reported | Two-months regimen with 3 antifungal drugs | Cysternalventriculostomy | Recovered |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tiepelyte, I.; Kadusauskas, T.; Sirka, A.; Trebse, R.; Esteban, J.; Sinkute, G.; Vaznaisiene, D. Periprosthetic Joint Infection Caused by Trichoderma: Is It Plausible? Diagnostics 2025, 15, 2575. https://doi.org/10.3390/diagnostics15202575
Tiepelyte I, Kadusauskas T, Sirka A, Trebse R, Esteban J, Sinkute G, Vaznaisiene D. Periprosthetic Joint Infection Caused by Trichoderma: Is It Plausible? Diagnostics. 2025; 15(20):2575. https://doi.org/10.3390/diagnostics15202575
Chicago/Turabian StyleTiepelyte, Iveta, Tomas Kadusauskas, Aurimas Sirka, Rihard Trebse, Jaime Esteban, Gintare Sinkute, and Danguole Vaznaisiene. 2025. "Periprosthetic Joint Infection Caused by Trichoderma: Is It Plausible?" Diagnostics 15, no. 20: 2575. https://doi.org/10.3390/diagnostics15202575
APA StyleTiepelyte, I., Kadusauskas, T., Sirka, A., Trebse, R., Esteban, J., Sinkute, G., & Vaznaisiene, D. (2025). Periprosthetic Joint Infection Caused by Trichoderma: Is It Plausible? Diagnostics, 15(20), 2575. https://doi.org/10.3390/diagnostics15202575








