Early Sepsis Detection in Adult Patients with Suspected Sepsis in an Emergency Setting: A Sequential Strategy of Monocyte Distribution Width and Presepsin
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Measurement of MDW and Presepsin
2.3. Statistical Analysis
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Singer, M.; Deutschman, C.S.; Seymour, C.W.; Shankar-Hari, M.; Annane, D.; Bauer, M.; Bellomo, R.; Bernard, G.R.; Chiche, J.D.; Coopersmith, C.M.; et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA 2016, 315, 801–810. [Google Scholar] [CrossRef]
- Long, B.; Gottlieb, M. Emergency medicine updates: Evaluation and diagnosis of sepsis and septic shock. Am. J. Emerg. Med. 2025, 90, 169–178. [Google Scholar] [CrossRef] [PubMed]
- Long, B.; Gottlieb, M. Emergency medicine updates: Management of sepsis and septic shock. Am. J. Emerg. Med. 2025, 90, 179–191. [Google Scholar] [CrossRef] [PubMed]
- Vincent, J.L.; Moreno, R.; Takala, J.; Willatts, S.; De Mendonca, A.; Bruining, H.; Reinhart, C.K.; Suter, P.M.; Thijs, L.G. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med. 1996, 22, 707–710. [Google Scholar]
- Fernando, S.M.; Tran, A.; Taljaard, M.; Cheng, W.; Rochwerg, B.; Seely, A.J.E.; Perry, J.J. Prognostic accuracy of the quick sequential organ failure assessment for mortality in patients with suspected infection: A systematic review and meta-analysis. Ann. Intern. Med. 2018, 168, 266–275. [Google Scholar] [PubMed]
- Liu, V.X.; Lu, Y.; Carey, K.A.; Gilbert, E.R.; Afshar, M.; Akel, M.; Shah, N.S.; Dolan, J.; Winslow, C.; Kipnis, P.; et al. Comparison of early warning scoring systems for hospitalized patients with and without infection at risk for in-hospital mortality and transfer to the intensive care unit. JAMA Netw. Open. 2020, 3, e205191. [Google Scholar] [CrossRef]
- Bolanaki, M.; Winning, J.; Slagman, A.; Lehmann, T.; Kiehntopf, M.; Stacke, A.; Neumann, C.; Reinhart, K.; Möckel, M.; Bauer, M. Biomarkers improve diagnostics of sepsis in adult patients with suspected organ dysfunction based on the quick sepsis-related organ failure assessment (qSOFA) score in the emergency department. Crit. Care Med. 2024, 52, 887–899. [Google Scholar] [CrossRef]
- Lafon, T.; Cazalis, M.A.; Hart, K.W.; Hennessy, C.; Tazarourte, K.; Self, W.H.; Akhavan, A.R.; Laribi, S.; Viglino, D.; Douplat, M.; et al. SEPSIGN: Early identification of sepsis signs in emergency department. Intern. Emerg. Med. 2025, 20, 1575–1587. [Google Scholar] [CrossRef]
- Devia-Jaramillo, G.A.; Erazo-Guerrero, L.; Laguado-Castro, V.; Alfonso-Parada, J.M. Evaluating sepsis mortality predictions from the emergency department: A retrospective cohort study comparing qSOFA, the National Early Warning Score, and the International Early Warning Score. J. Clin. Med. 2025, 14, 4869. [Google Scholar] [CrossRef]
- Magnani, L.; Colantuoni, M.; Mortellaro, A. Gasdermins: New therapeutic targets in host defense, inflammatory diseases, and cancer. Front. Immunol. 2022, 13, 898298. [Google Scholar] [CrossRef]
- Devant, P.; Kagan, J.C. Molecular mechanisms of gasdermin D pore-forming activity. Nat. Immunol. 2023, 24, 1064–1075. [Google Scholar] [CrossRef]
- Crouser, E.D.; Parrillo, J.E.; Seymour, C.; Angus, D.C.; Bicking, K.; Esguerra, V.E.; Peck-Palmer, O.M.; Magari, R.T.; Julian, M.W.; Kleven, J.M.; et al. Monocyte distribution width: A novel indicator of Sepsis-2 and Sepsis-3 in high-risk emergency department patients. Crit. Care Med. 2019, 47, 1018–1025. [Google Scholar] [CrossRef] [PubMed]
- U.S. Food and Drug Administration. 510(k) Substantial Equivalence Determination Decision Summary: UniCel DxH 800 Coulter Cellular Analysis System with Early Sepsis Indicator Application (K181599). Available online: https://www.accessdata.fda.gov/cdrh_docs/reviews/K181599.pdf (accessed on 22 August 2025).
- Hausfater, P.; Robert Boter, N.; Morales Indiano, C.; Cancella de Abreu, M.; Marin, A.M.; Pernet, J.; Quesada, D.; Castro, I.; Careaga, D.; Arock, M.; et al. Monocyte distribution width (MDW) performance as an early sepsis indicator in the emergency department: Comparison with CRP and procalcitonin in a multicenter international European prospective study. Crit. Care 2021, 25, 227. [Google Scholar] [CrossRef] [PubMed]
- Formenti, P.; Gotti, M.; Palmieri, F.; Pastori, S.; Roccaforte, V.; Menozzi, A.; Galimberti, A.; Umbrello, M.; Sabbatini, G.; Pezzi, A. Presepsin in critical illness: Current knowledge and future perspectives. Diagnostics 2024, 14, 1311. [Google Scholar] [CrossRef]
- Masson, S.; Caironi, P.; Fanizza, C.; Thomae, R.; Bernasconi, R.; Noto, A.; Oggioni, R.; Pasetti, G.S.; Romero, M.; Tognoni, G.; et al. Circulating presepsin (soluble CD14 subtype) as a marker of host response in patients with severe sepsis or septic shock: Data from the multicenter, randomized ALBIOS trial. Intensive Care Med. 2015, 41, 12–20. [Google Scholar] [CrossRef] [PubMed]
- Galliera, E.; Massaccesi, L.; de Vecchi, E.; Banfi, G.; Romanelli, M.M.C. Clinical application of presepsin as diagnostic biomarker of infection: Overview and updates. Clin. Chem. Lab. Med. 2019, 58, 11–17. [Google Scholar] [CrossRef]
- Kim, H.; Hur, M.; Moon, H.W.; Yun, Y.M.; Di Somma, S.; Network, G. Multi-marker approach using procalcitonin, presepsin, galectin-3, and soluble suppression of tumorigenicity 2 for the prediction of mortality in sepsis. Ann. Intensive Care 2017, 7, 27. [Google Scholar] [CrossRef]
- Yang, H.S.; Hur, M.; Yi, A.; Kim, H.; Lee, S.; Kim, S.N. Prognostic value of presepsin in adult patients with sepsis: Systematic review and meta-analysis. PLoS ONE 2018, 13, e0191486. [Google Scholar] [CrossRef]
- Park, M.; Hur, M.; Kim, H.; Lee, C.H.; Lee, J.H.; Kim, H.W.; Nam, M. Prognostic utility of procalcitonin, presepsin, and the VACO index for predicting 30-day mortality in hospitalized COVID-19 patients. Ann. Lab. Med. 2022, 42, 406–414. [Google Scholar] [CrossRef]
- Lee, G.H.; Park, M.; Hur, M.; Kim, H.; Lee, S.; Moon, H.W.; Yun, Y.M. Utility of presepsin and interferon-lambda 3 for predicting disease severity and clinical outcomes in COVID-19 patients. Diagnostics 2023, 13, 2372. [Google Scholar] [CrossRef]
- National Institute for Health and Care Excellence. Sepsis: Recognition, Diagnosis and Early Management. Available online: https://www.nice.org.uk/guidance/ng51 (accessed on 22 August 2025).
- Unterberg, M.; Rahmel, T.; Rump, K.; Wolf, A.; Haberl, H.; von Busch, A.; Bergmann, L.; Bracht, T.; Zarbock, A.; Ehrentraut, S.F.; et al. The impact of the COVID-19 pandemic on non-COVID induced sepsis survival. BMC Anesthesiol. 2022, 22, 12. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.; Hur, M.; Yi, J.H.; Lee, G.H.; Lee, S.; Moon, H.W.; Yun, Y.M. Detection of blasts using flags and cell population data rules on Beckman Coulter DxH 900 hematology analyzer in patients with hematologic diseases. Clin. Chem. Lab. Med. 2024, 62, 958–966. [Google Scholar] [CrossRef] [PubMed]
- Okamura, Y.; Yokoi, H. Development of a point-of-care assay system for measurement of presepsin (sCD14-ST). Clin. Chim. Acta 2011, 412, 2157–2161. [Google Scholar] [CrossRef]
- Kang, T.; Yoo, J.; Choi, H.; Lee, S.; Jekarl, D.W.; Kim, Y. Performance evaluation of presepsin using a Sysmex HISCL-5000 analyzer and determination of reference interval. J. Clin. Lab. Anal. 2022, 36, e24618. [Google Scholar] [CrossRef]
- de Moura, E.L.B.; Pereira, R.W. Crossing age boundaries: The unifying potential of presepsin in sepsis diagnosis across diverse age groups. J. Clin. Med. 2024, 13, 7038. [Google Scholar] [CrossRef]
- Lu, K. Multiple imputation score tests and an application to Cochran-Mantel-Haenszel statistics. Stat. Med. 2020, 39, 4025–4036. [Google Scholar] [CrossRef]
- Mukaka, M.M. Statistics corner: A guide to appropriate use of correlation coefficient in medical research. Malawi. Med. J. 2012, 24, 69–71. [Google Scholar]
- Cole, T.J. Too many digits: The presentation of numerical data. Arch. Dis. Child. 2015, 100, 608–609. [Google Scholar] [CrossRef]
- Huang, Y.H.; Chen, C.J.; Shao, S.C.; Li, C.H.; Hsiao, C.H.; Niu, K.Y.; Yen, C.C. Comparison of the diagnostic accuracies of monocyte distribution width, procalcitonin, and C-reactive protein for sepsis: A systematic review and meta-analysis. Crit. Care Med. 2023, 51, e106–e114. [Google Scholar] [CrossRef]
- Agnello, L.; Vidali, M.; Lo Sasso, B.; Giglio, R.V.; Gambino, C.M.; Scazzone, C.; Ciaccio, A.M.; Bivona, G.; Ciaccio, M. Monocyte distribution width (MDW) as a screening tool for early detecting sepsis: A systematic review and meta-analysis. Clin. Chem. Lab. Med. 2022, 60, 786–792. [Google Scholar] [CrossRef] [PubMed]
- Agnello, L.; Ciaccio, A.M.; Vidali, M.; Cortegiani, A.; Biundo, G.; Gambino, C.M.; Scazzone, C.; Lo Sasso, B.; Ciaccio, M. Monocyte distribution width (MDW) in sepsis. Clin. Chim. Acta. 2023, 548, 117511. [Google Scholar] [CrossRef] [PubMed]
- Kralovcova, M.; Muller, J.; Hajsmanova, Z.; Sigutova, P.; Bultasova, L.; Palatova, J.; Matejovic, M. Understanding the value of monocyte distribution width (MDW) in acutely ill medical patients presenting to the emergency department: A prospective single center evaluation. Sci. Rep. 2024, 14, 15255. [Google Scholar] [CrossRef]
- Chenevier-Gobeaux, C.; Borderie, D.; Weiss, N.; Mallet-Coste, T.; Claessens, Y.E. Presepsin (sCD14-ST), an innate immune response marker in sepsis. Clin. Chim. Acta 2015, 450, 97–103. [Google Scholar] [CrossRef] [PubMed]
- Ligi, D.; Sasso, B.L.; Franca, C.D.; Giglio, R.V.; Agnello, L.; Ciaccio, M.; Mannello, F. Monocyte distribution width alterations and cytokine storm are modulated by circulating histones. Clin. Chem. Lab. Med. 2023, 61, 1525–1535. [Google Scholar] [CrossRef]
- Ligi, D.; Franca, C.D.; Pelloso, M.; Martinez-Iribarren, A.; Leis, A.; Fabbri, E.; Salvatori, F.; Sukhacheva, E.A.; Brandi, G.; Schiavano, G.F.; et al. Comparative analysis of monocyte distribution width alterations in Escherichia coli sepsis: Insights from in vivo and ex vivo models. Clin. Chem. Lab. Med. 2025. Online ahead of print. [Google Scholar] [CrossRef]
- Campagner, A.; Agnello, L.; Carobene, A.; Padoan, A.; Del Ben, F.; Locatelli, M.; Plebani, M.; Ognibene, A.; Lorubbio, M.; De Vecchi, E.; et al. Complete blood count and monocyte distribution width-based machine learning algorithms for sepsis detection: Multicentric development and external validation study. J. Med. Internet Res. 2025, 27, e55492. [Google Scholar] [CrossRef]
- Leon-Justel, A.; Bustos, C.N.; Noval-Padillo, J.A.; Perez, S.M.; Gomez, M.D.A.; Valencia, N.J.; Castilla, J.M.G.; Muñoz, M.D.; Vizcaino, M.A.R.; Heredia, L.A.; et al. Point-of-care testing improves care timeliness in the emergency department. A multicenter randomized clinical trial (study POCTUR). Clin. Chem. Lab. Med. 2025, 63, 942–951. [Google Scholar] [CrossRef]
- Kudu, E.; Kucukardali, A.E.; Altun, M.; Öztürk, Ü.; Altunbaş, E.; Karacabey, S.; Sanri, E.; Denizbasi, A. The diagnostic accuracy of the ESC 0/1-hour algorithm in non-ST-segment elevation myocardial infarction in a crowded emergency department: A real-world experience from a single-center in Türkiye. BMC. Emerg. Med. 2025, 25, 129. [Google Scholar] [CrossRef]
- Saxena, J.; Das, S.; Kumar, A.; Sharma, A.; Sharma, L.; Kaushik, S.; Srivastava, V.K.; Siddiqui, A.J.; Jyoti, A. Biomarkers in sepsis. Clin. Chim. Acta 2024, 562, 119891. [Google Scholar] [CrossRef] [PubMed]
- Schuetz, P.; Beishuizen, A.; Broyles, M.; Ferrer, R.; Gavazzi, G.; Gluck, E.H.; del Castillo, J.G.; Jensen, J.U.; Kanizsai, P.L.; Kwa, A.L.H.; et al. Procalcitonin (PCT)-guided antibiotic stewardship: An international experts consensus on optimized clinical use. Clin. Chem. Lab. Med. 2019, 57, 1308–1318. [Google Scholar] [CrossRef]
- Auriti, C.; De Rose, D.U.; Maddaloni, C.; Ravà, L.; Martini, L.; Di Tommaso, E.; Bernaschi, P.; Paionni, E.; Porzio, O.; Piersigilli, F.; et al. The accuracy of presepsin in diagnosing neonatal late-onset sepsis in critically ill neonates: A prospective study. Clin. Chem. Lab. Med. 2025, 63, 1876–1887. [Google Scholar] [CrossRef] [PubMed]
- Jeong, J.S.; Kang, T.; Ju, H.; Cho, C.H. Novel approach exploring the correlation between presepsin and routine laboratory parameters using explainable artificial intelligence. Heliyon 2024, 10, e33826. [Google Scholar] [CrossRef] [PubMed]
| Variable | Total (n = 281) | Non-Sepsis (n = 153) | Sepsis (n = 128) | p |
|---|---|---|---|---|
| Age (years) | 68 (58–78) | 65 (54–75) | 72 (61–83) | <0.001 |
| Males | 172 (61.2) | 88 (31.3) | 84 (29.9) | 0.76 |
| Clinical outcomes | ||||
| ICU admission | 77 (27.4) | 29 (10.3) | 48 (17.1) | <0.001 |
| ICU stay (days) | 3 (2–13) | 2 (1–3) | 5 (2–21) | 0.002 |
| Hospital stay (days) | 16 (9–44) | 12 (7–24) | 29 (13–53) | <0.001 |
| In-hospital mortality | 43 (15.4) | 10 (3.6) | 33 (11.8) | <0.001 |
| 30-day mortality | 38 (13.5) | 9 (3.2) | 29 (10.3) | <0.001 |
| Comorbidities | ||||
| Cardiac diseases | 18 (6.4) | 12 (4.3) | 6 (2.1) | 0.283 |
| Cerebrovascular accidents | 117 (41.6) | 50 (17.8) | 67 (23.8) | <0.001 |
| Chronic kidney diseases | 25 (8.9) | 12 (4.3) | 13 (4.6) | 0.498 |
| DM/Metabolic syndromes | 105 (37.4) | 42 (15.0) | 63 (22.4) | <0.001 |
| Gastrointestinal diseases | 50 (17.8) | 18 (6.4) | 32 (11.4) | 0.004 |
| Hematologic diseases | 9 (3.2) | 4 (1.4) | 5 (1.8) | 0.541 |
| Hepatopancreatic diseases | 22 (7.8) | 14 (5.0) | 8 (2.8) | 0.145 |
| Pulmonary diseases | 76 (27.0) | 28 (1.0) | 48 (17.1) | <0.001 |
| Solid cancers | 31 (11.0) | 17 (6.0) | 14 (5.0) | 0.963 |
| qSOFA score | 1 (1–2) | 1 (1–1) | 2 (1–2) | <0.001 |
| SOFA score | 2 (0–4) | 1 (0–1) | 4 (3–6) | <0.001 |
| Cardiovascular | 0 (0–0) | 0 (0–0) | 0 (0–2) | <0.001 |
| Central nervous system | 0 (0–1) | 0 (0–0) | 0 (0–2) | <0.001 |
| Coagulation | 0 (0–0) | 0 (0–0) | 0 (0–1) | <0.001 |
| Liver | 0 (0–0) | 0 (0–0) | 0 (0–1) | <0.001 |
| Renal | 0 (0–1) | 0 (0–0) | 0 (0–1) | <0.001 |
| Respiratory | 0 (0–1) | 0 (0–0) | 0 (0–1) | <0.001 |
| Laboratory parameters | ||||
| CRP (mg/L) | 15.8 (12.4–21.3) | 15.8 (12.4–22.1) | 15.8 (12.5–20.9) | 0.688 |
| Lactate (mmol/L) | 1.82 (1.31–2.59) | 1.61 (1.19–2.08) | 2.05 (1.39–2.92) | <0.001 |
| Procalcitonin (ng/mL) | 0.59 (0.20–2.44) | 0.28 (0.15–1.14) | 0.79 (0.33–4.50) | <0.001 |
| Hb (g/dL) | 10.3 (9.0–11.9) | 10.6 (9.7–12.7) | 9.7 (8.6–11.0) | <0.001 |
| WBC (×109/L) | 10.9 (8.0–14.2) | 10.3 (7.6–13.8) | 11.3 (8.6–15.4) | 0.045 |
| PLT (×109/L) | 219 (152–292) | 245 (178–318) | 187 (121–269) | <0.001 |
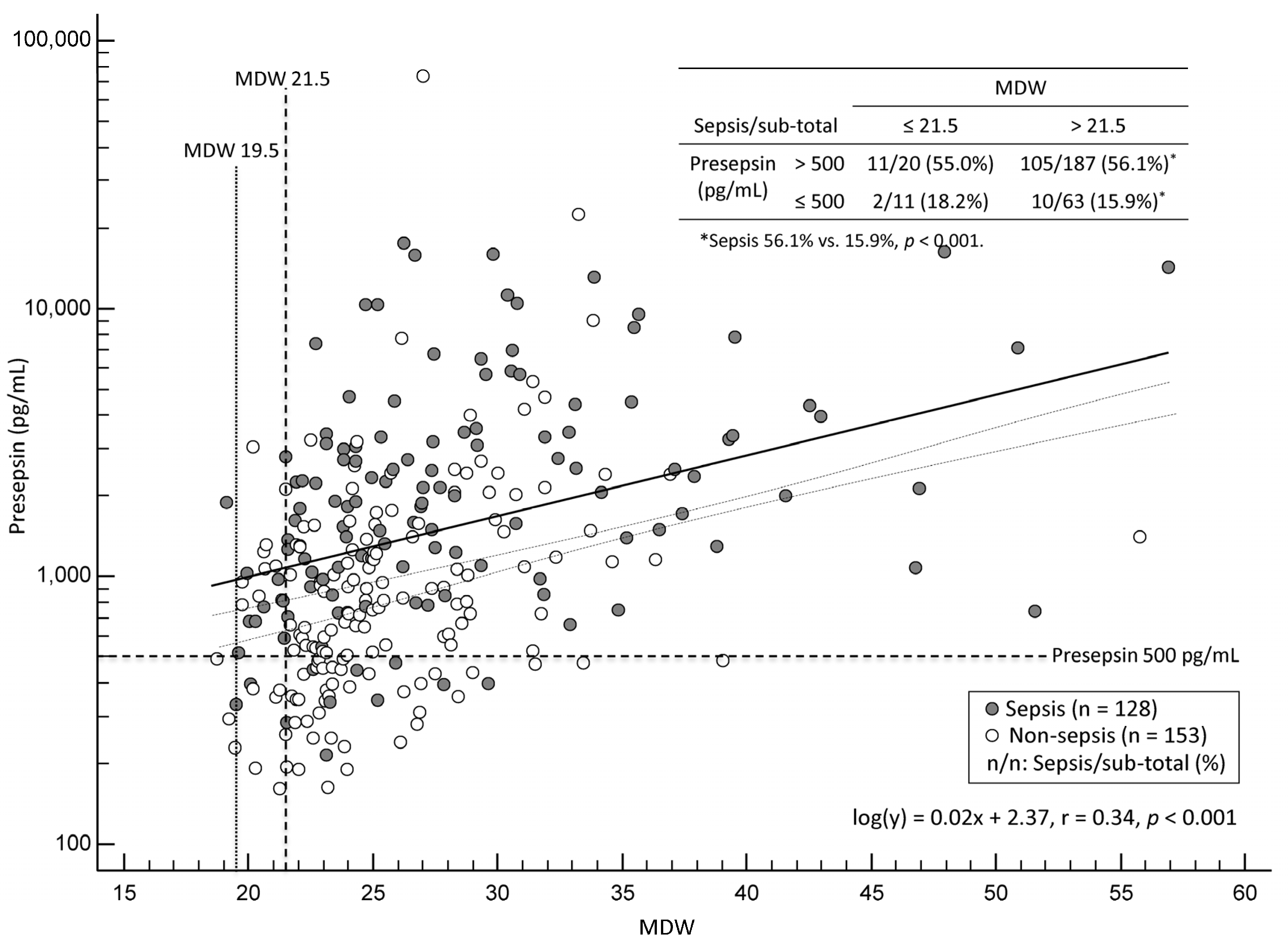
| MDW | 25.2 (22.8–29.2) | 24.5 (22.6–28.3) | 26.5 (23.2–31.5) | 0.001 |
| Presepsin (pg/mL) | 878 (494–1660) | 590 (377–1059) | 1384 (776–2350) | <0.001 |
| qSOFA < 2 (n = 184) | qSOFA ≥ 2 (n = 97) | |||
|---|---|---|---|---|
| Non-Sepsis (n = 129) | Sepsis (n = 55) | Non-Sepsis (n = 24) | Sepsis (n = 73) | |
| MDW | ||||
| Q1 (n = 71) | 37 | 15 | 7 | 12 |
| Q2–Q4 (n = 210) | 92 | 40 | 17 | 61 |
| OR (95% CI) | 4.2 (1.4–12.8) | 8.3 (4.3–15.9) | ||
| Presepsin | ||||
| Q1 (n = 73) | 55 | 4 | 6 | 8 |
| Q2–Q4 (n = 208) | 74 | 51 | 18 | 65 |
| OR (95% CI) | 18.3 (4.2–79.5) | 5.2 (2.8–9.9) | ||
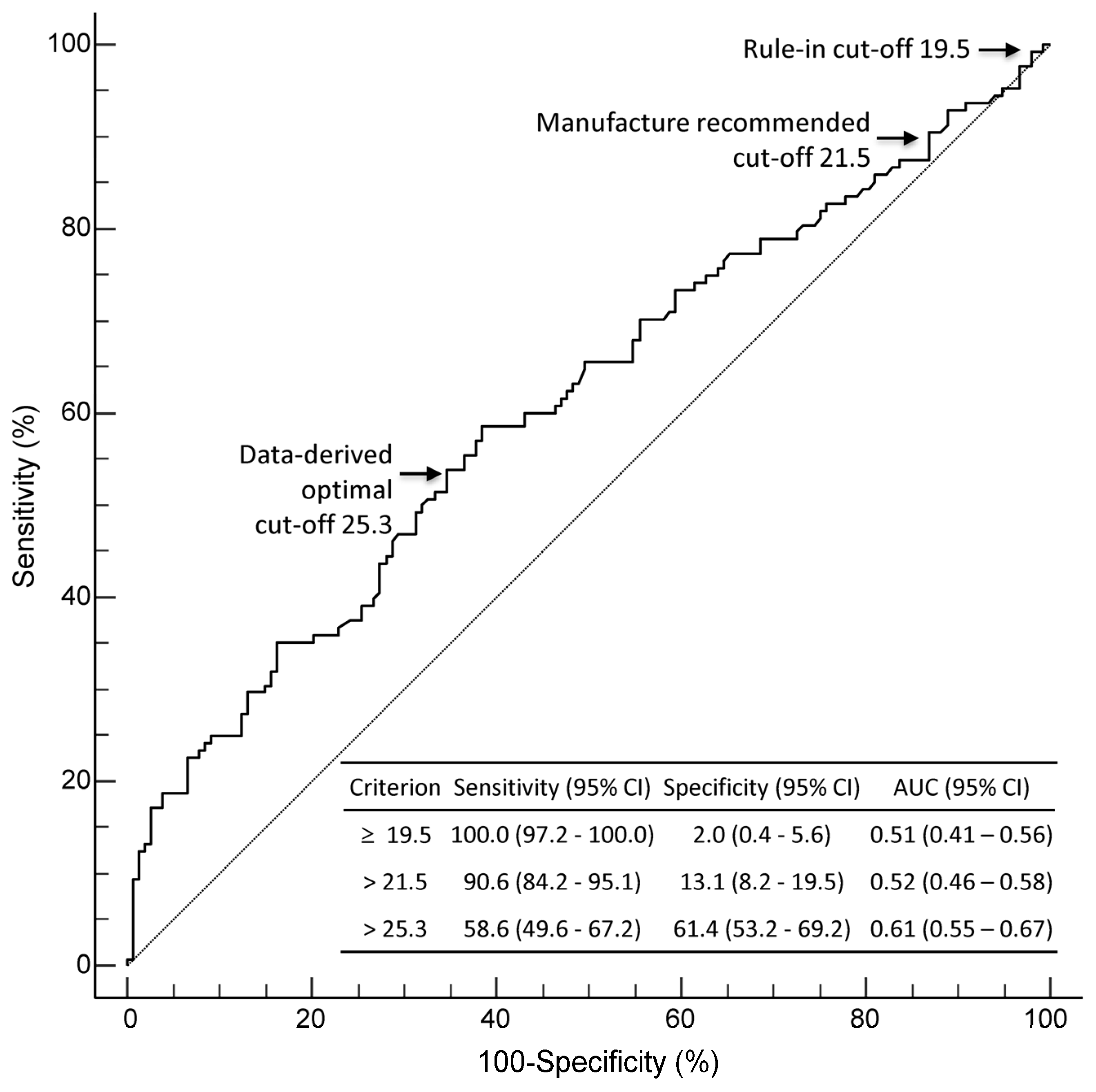
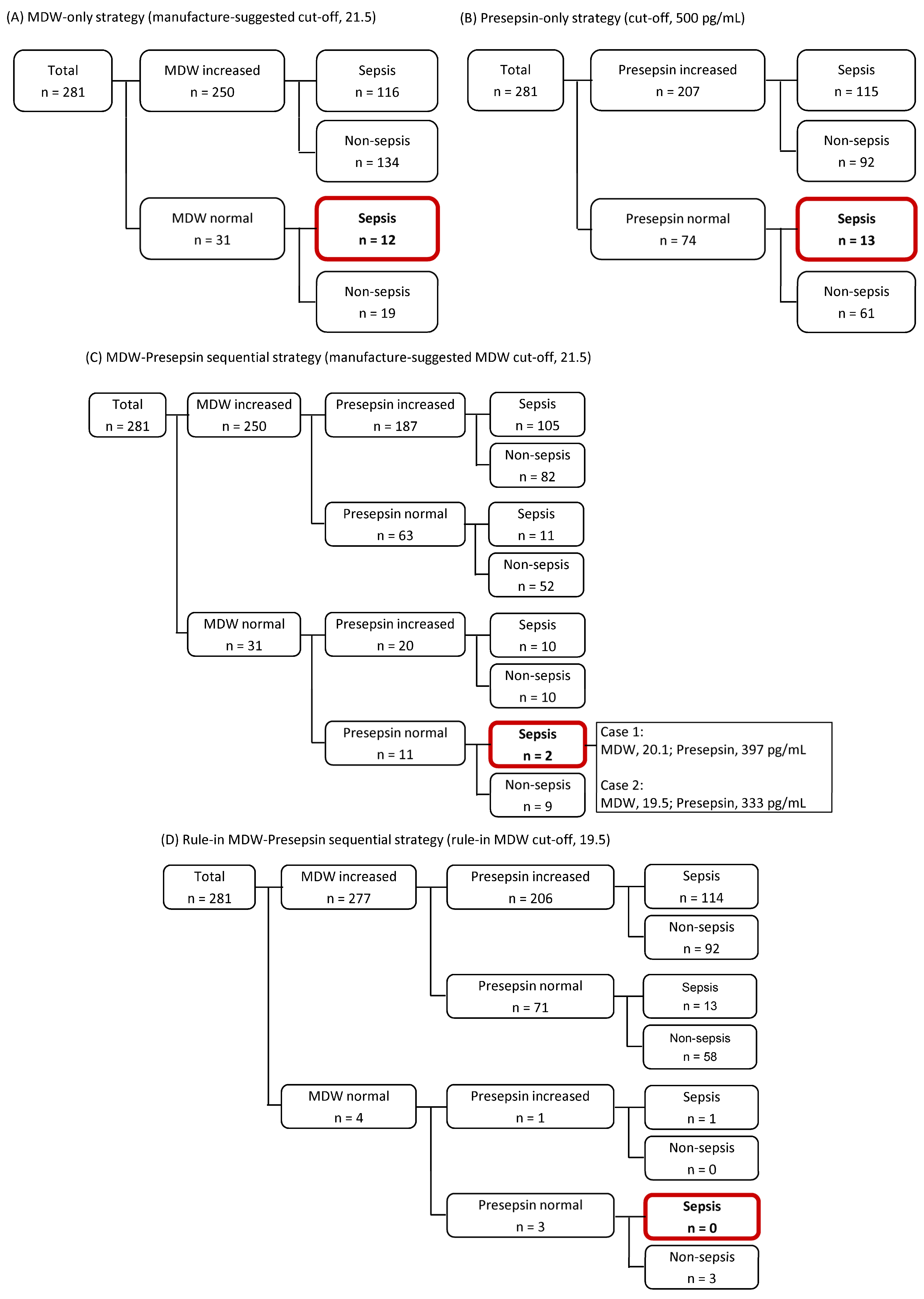
| Non-Sepsis (n = 153) | Sepsis (n = 128) | Sensitivity (%, 95% CI) | Specificity (%, 95% CI) | AUC (95% CI) | Accuracy (%, 95% CI) | |
|---|---|---|---|---|---|---|
| MDW | ||||||
| Increased (n = 250) | 134 | 116 | 90.6 (84.2–95.1) | 12.4 (7.7–18.7) | 0.52 (0.46–0.58) | 48.0 (42.1–54.1) |
| Normal (n = 31) | 19 | 12 | ||||
| Presepsin | ||||||
| Increased (n = 207) | 92 | 115 | 89.8 (83.3–94.5) | 39.9 (32.1–48.1) | 0.65 (0.59–0.70) | 62.6 (56.7–68.3) |
| Normal (n = 74) | 61 | 13 | ||||
| MDW + Presepsin | ||||||
| Increased (n = 270) | 144 | 126 | 98.4 (94.5–99.8) | 5.9 (2.7–10.9) | 0.52 (0.46–0.58) | 48.0 (42.1–54.1) |
| Normal (n = 11) | 9 | 24 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, H.; Hur, M.; Lee, H.; Lee, G.-H.; Lee, K.R.; Mannello, F. Early Sepsis Detection in Adult Patients with Suspected Sepsis in an Emergency Setting: A Sequential Strategy of Monocyte Distribution Width and Presepsin. Diagnostics 2025, 15, 2574. https://doi.org/10.3390/diagnostics15202574
Kim H, Hur M, Lee H, Lee G-H, Lee KR, Mannello F. Early Sepsis Detection in Adult Patients with Suspected Sepsis in an Emergency Setting: A Sequential Strategy of Monocyte Distribution Width and Presepsin. Diagnostics. 2025; 15(20):2574. https://doi.org/10.3390/diagnostics15202574
Chicago/Turabian StyleKim, Hanah, Mina Hur, Hyejung Lee, Gun-Hyuk Lee, Kyeong Ryong Lee, and Ferdinando Mannello. 2025. "Early Sepsis Detection in Adult Patients with Suspected Sepsis in an Emergency Setting: A Sequential Strategy of Monocyte Distribution Width and Presepsin" Diagnostics 15, no. 20: 2574. https://doi.org/10.3390/diagnostics15202574
APA StyleKim, H., Hur, M., Lee, H., Lee, G.-H., Lee, K. R., & Mannello, F. (2025). Early Sepsis Detection in Adult Patients with Suspected Sepsis in an Emergency Setting: A Sequential Strategy of Monocyte Distribution Width and Presepsin. Diagnostics, 15(20), 2574. https://doi.org/10.3390/diagnostics15202574








