Mechanical Versus Restrictive Kinematic Alignment in Robotic-Assisted Total Knee Arthroplasty: A Randomized Controlled Trial
Abstract
1. Introduction
2. Methods
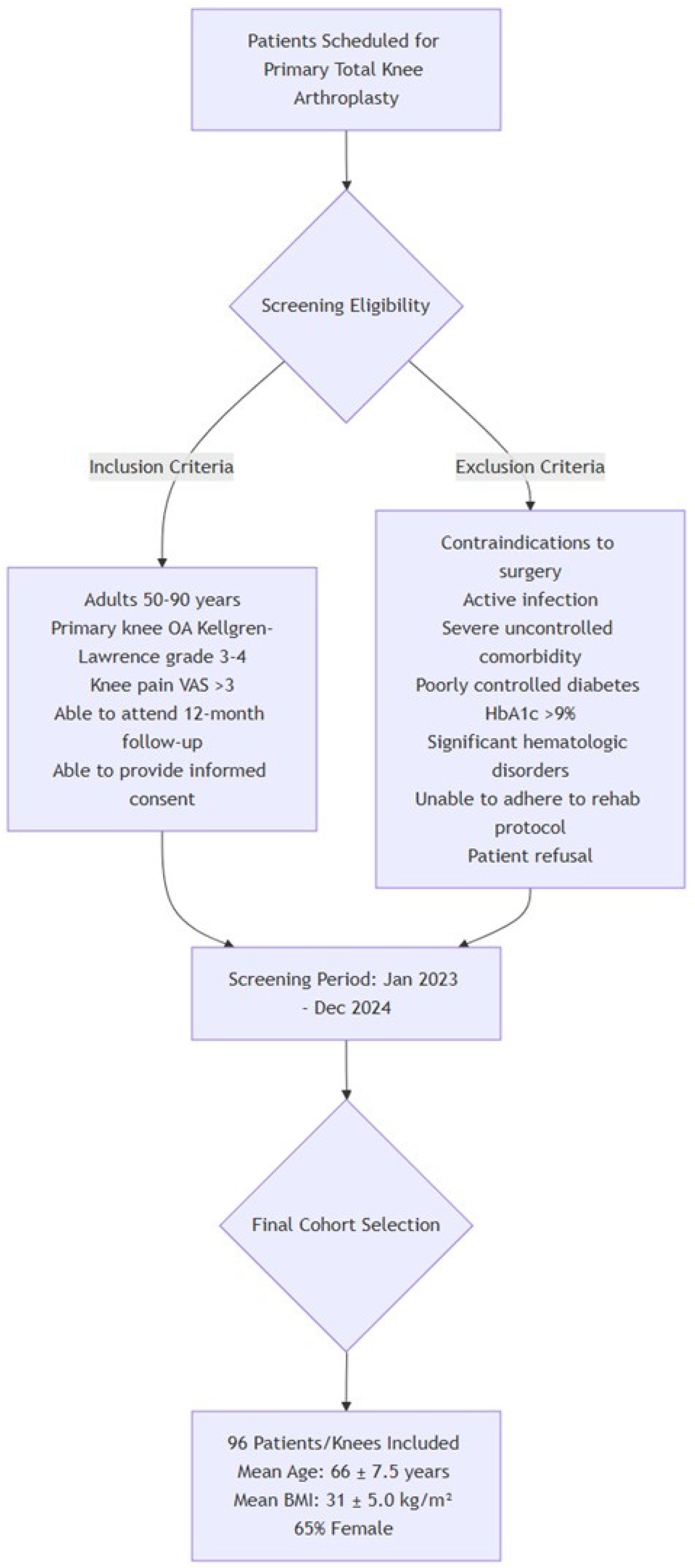
2.1. Study Design
2.2. Participants
2.3. Randomization and Group Assignment
2.4. Surgical Technique
2.5. Outcome Measures
2.6. Radiological Evaluation
2.7. Statistical Analysis
3. Results
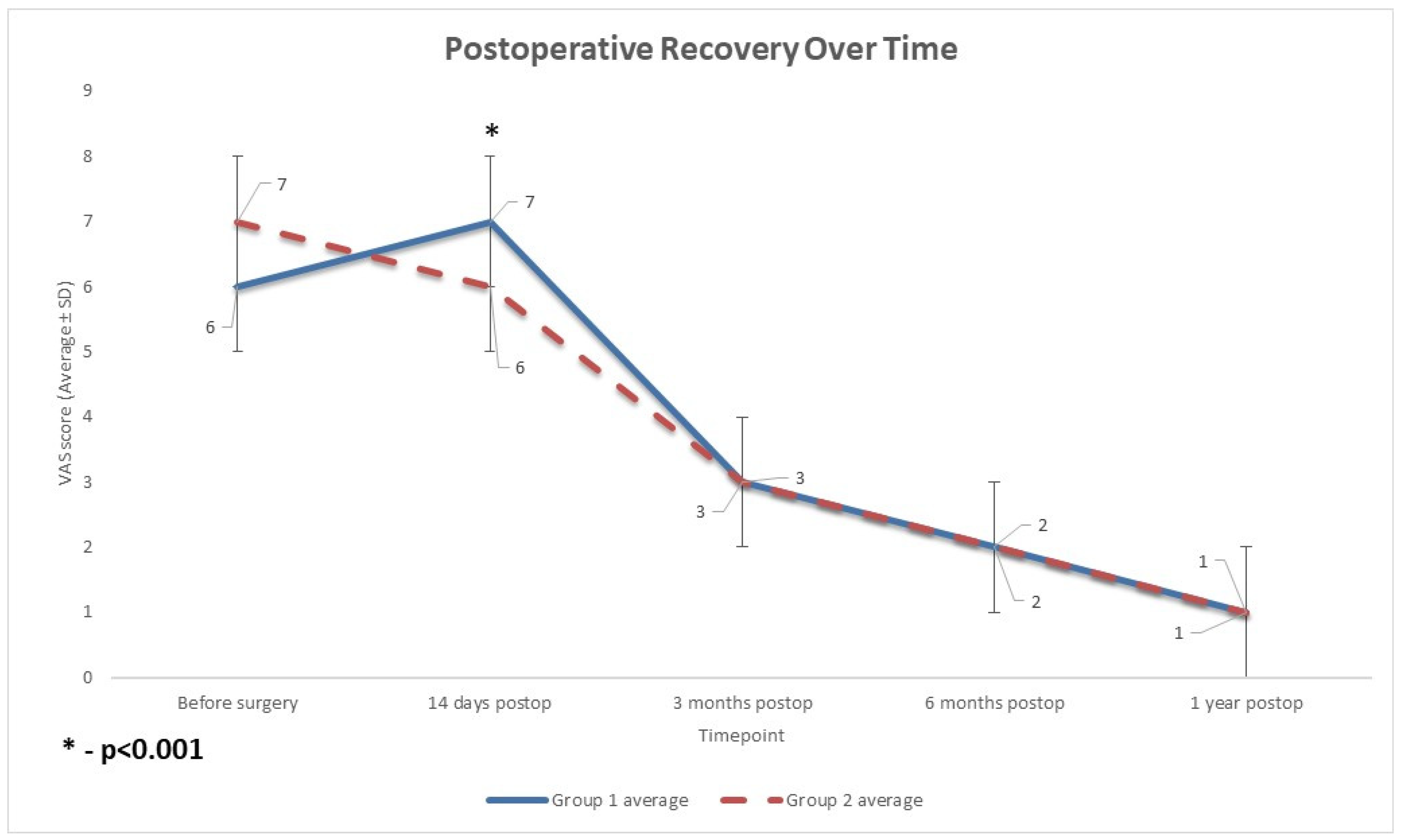
3.1. Pain
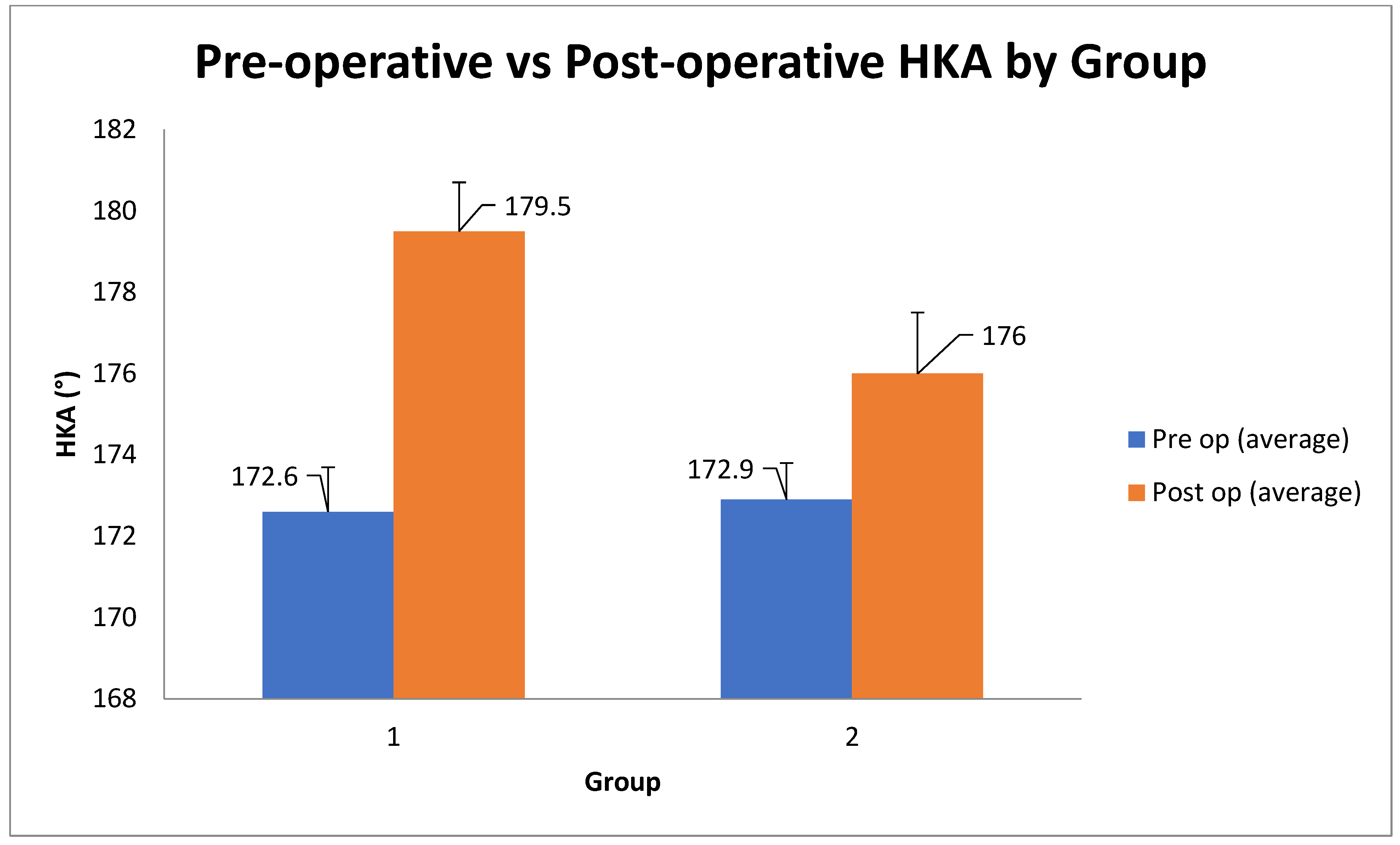
3.2. Radiographic Alignment
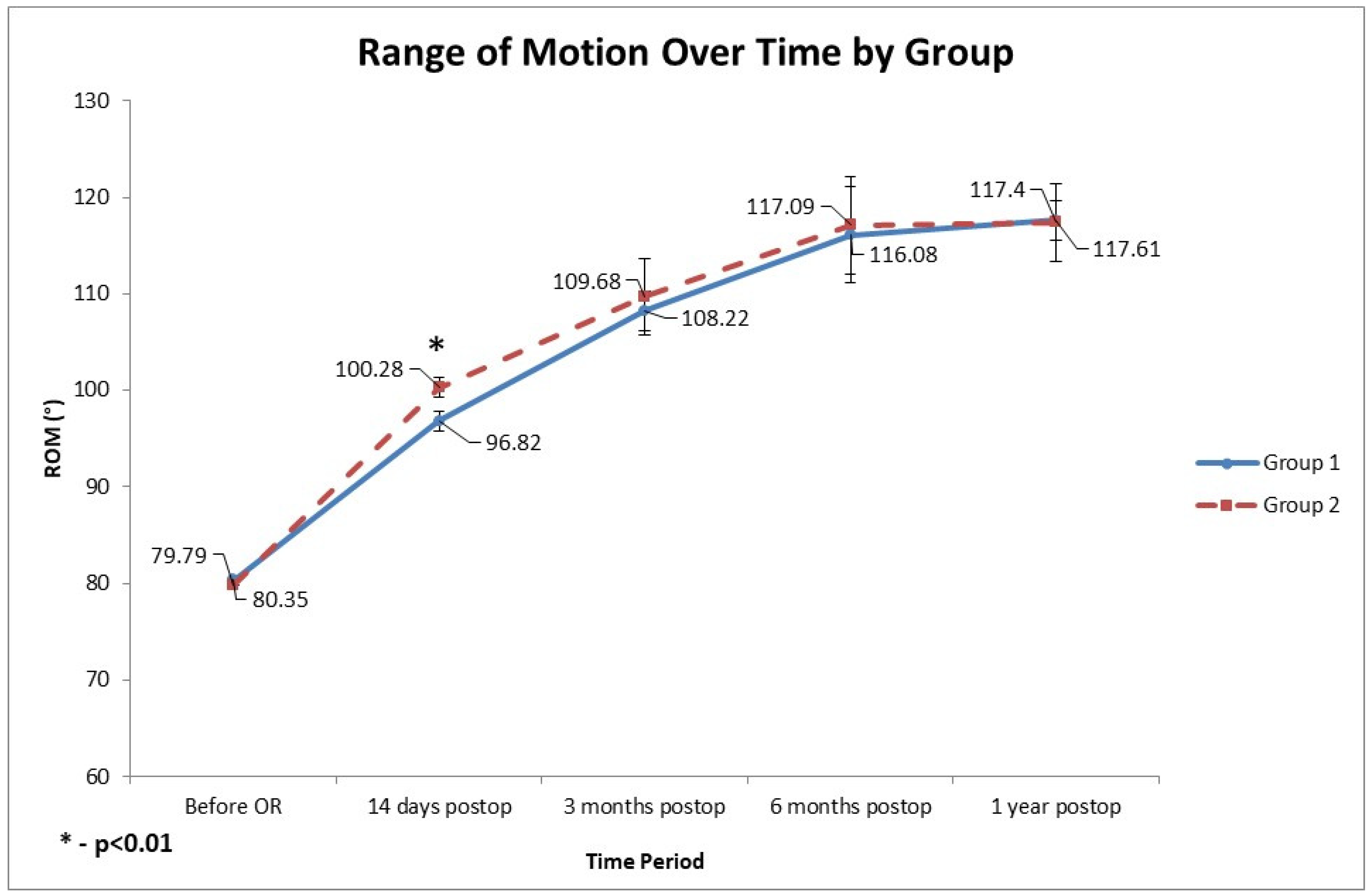
3.3. Range of Motion
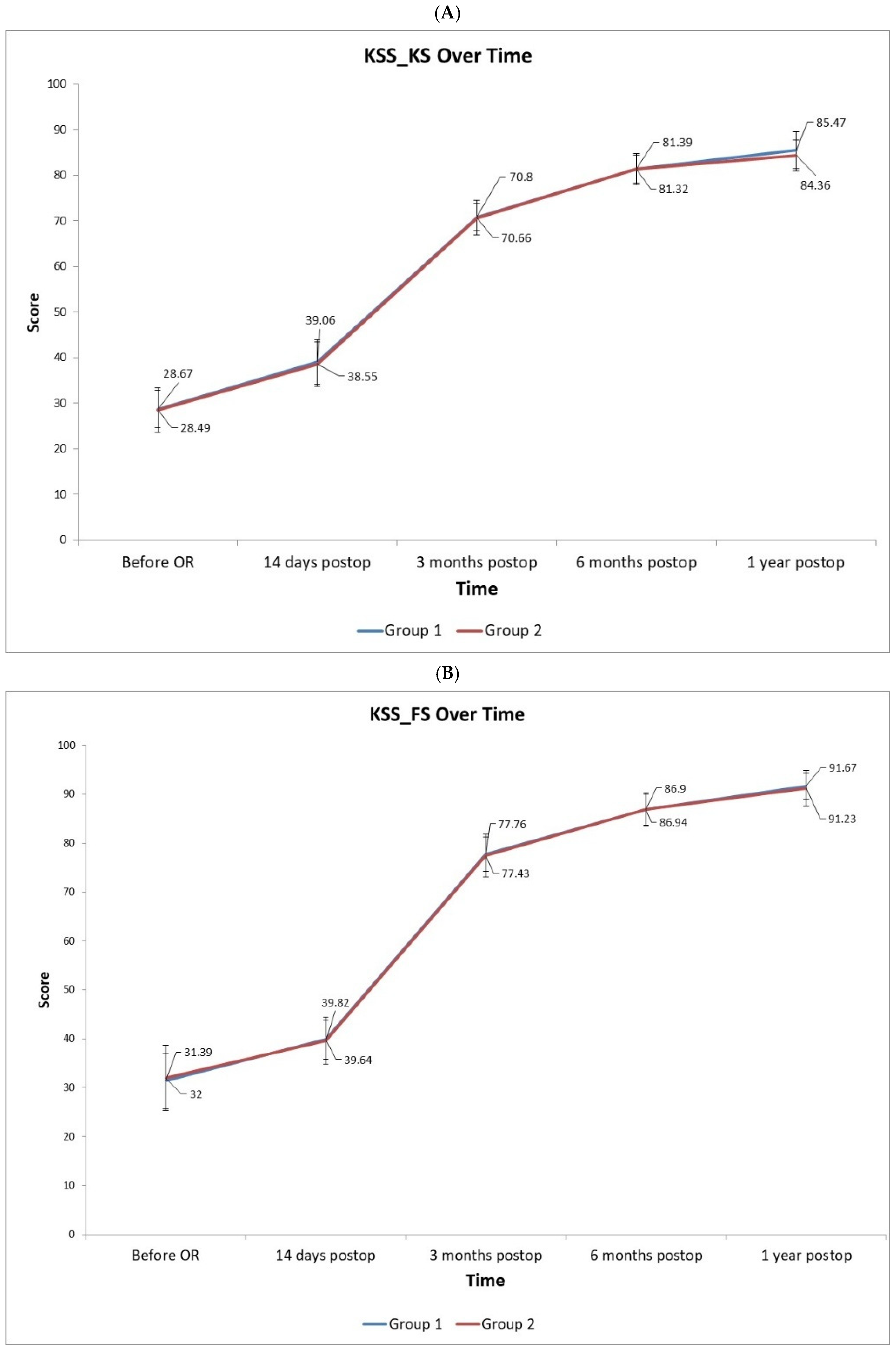
3.4. Functional Scores
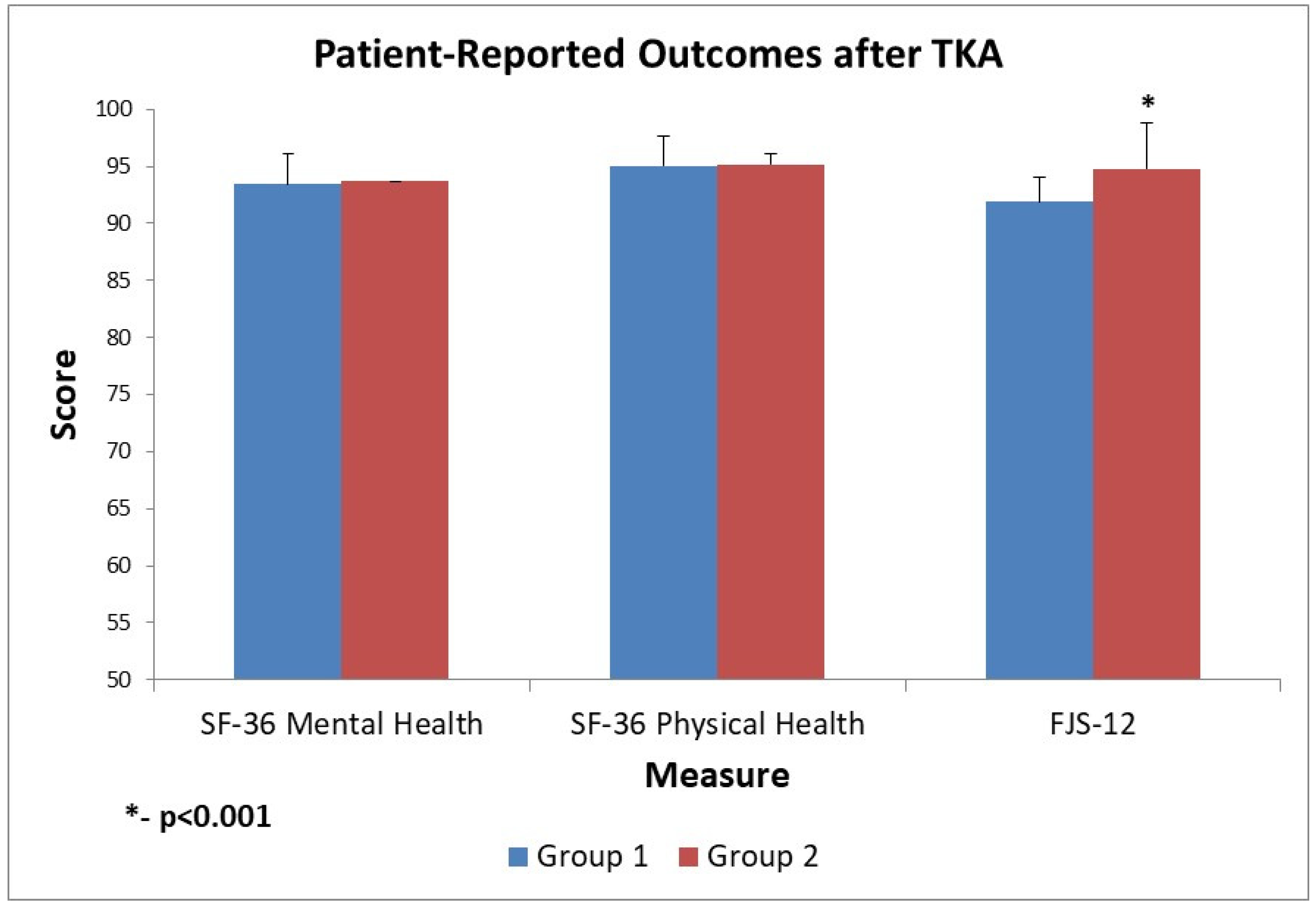
3.5. Quality of Life and Satisfaction Scores
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Singh, J.A.; Yu, S.; Chen, L.; Cleveland, J.D. Rates of Total Joint Replacement in the United States: Future Projections to 2020-2040 Using the National Inpatient Sample. J. Rheumatol. 2019, 46, 1134–1140. [Google Scholar] [CrossRef] [PubMed]
- Singh, S., Jr.; Mehta, H.; Gupta, S.; Singh, J.; Bakshi, A.S. Comparison of Clinical and Radiological Outcomes of Total Knee Arthroplasty in Osteoarthritic Patients. Cureus 2024, 16, e60933. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Matassi, F.; Pettinari, F.; Frasconà, F.; Innocenti, M.; Civinini, R. Coronal alignment in total knee arthroplasty: A review. J. Orthop. Traumatol. 2023, 24, 24. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Shekhar, A.; Dungy, D.; Stewart, S.L.; Jamali, A.A. Patient-Reported Outcomes of Kinematic vs Mechanical Alignment in Total Knee Arthroplasty: A Systematic Review and Meta-analysis of Randomized Controlled Trials. Arthroplast. Today 2023, 21, 101127. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Hiranaka, T. Current concept: Personalized alignment total knee arthroplasty as a contrast to classical mechanical alignment total knee arthroplasty. Arthroplasty 2024, 6, 23. [Google Scholar] [CrossRef] [PubMed]
- Vendittoli, P.A.; Martinov, S.; Blakeney, W.G. Restricted Kinematic Alignment, the Fundamentals, and Clinical Applications. Front. Surg. 2021, 8, 697020. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Howell, S.M.; Papadopoulos, S.; Kuznik, K.T.; Hull, M.L. Accurate alignment and high function after kinematically aligned TKA performed with generic instruments. Knee Surg. Sports Traumatol. Arthrosc. 2013, 21, 2271–2280. [Google Scholar] [CrossRef] [PubMed]
- Narkbunnam, R.; Pornrattanamaneewong, C.; Ruangsomboon, P.; Chareancholvanich, K. Alignment accuracy and functional outcomes between hand-held navigation and conventional instruments in TKA: A randomized controlled trial. BMC Musculoskelet. Disord. 2022, 23, 1017. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Marques Luís, N.; Varatojo, R. Radiological assessment of lower limb alignment. EFORT Open Rev. 2021, 6, 487–494. [Google Scholar] [CrossRef]
- Vajapey, S.P.; Pettit, R.J.; Li, M.; Chen, A.F.; Spitzer, A.I.; Glassman, A.H. Risk Factors for Mid-Flexion Instability After Total Knee Arthroplasty: A Systematic Review. J. Arthroplast. 2020, 35, 3046–3054. [Google Scholar] [CrossRef] [PubMed]
- Young, S.W.; Tay, M.L.; Kawaguchi, K.; van Rooyen, R.; Walker, M.L.; Farrington, W.J.; Bayan, A. The John N. Insall Award: Functional Versus Mechanical Alignment in Total Knee Arthroplasty: A Randomized Controlled Trial. J. Arthroplast. 2025, 40 (Suppl. S1), S20–S30.e2. [Google Scholar] [CrossRef] [PubMed]
- Dossett, H.G.; Arthur, J.R.; Makovicka, J.L.; Mara, K.C.; Bingham, J.S.; Clarke, H.D.; Spangehl, M.J. A Randomized Controlled Trial of Kinematically and Mechanically Aligned Total Knee Arthroplasties: Long-Term Follow-Up. J. Arthroplast. 2023, 38, S209–S214. [Google Scholar] [CrossRef] [PubMed]
- Lustig, S.; Sappey-Marinier, E.; Fary, C.; Servien, E.; Parratte, S.; Batailler, C. Personalized alignment in total knee arthroplasty: Current concepts. SICOT J. 2021, 7, 19. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Rivière, C.; Villet, L.; Jeremic, D.; Vendittoli, P.A. What you need to know about kinematic alignment for total knee arthroplasty. Orthop. Traumatol. Surg. Res. 2021, 107, 102773. [Google Scholar] [CrossRef] [PubMed]
- Karasavvidis, T.; Pagan Moldenhauer, C.A.; Lustig, S.; Vigdorchik, J.M.; Hirschmann, M.T. Definitions and consequences of current alignment techniques and phenotypes in total knee arthroplasty (TKA)–There is no winner yet. J. Exp. Orthop. 2023, 22, 120. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Karuppal, R. Kinematic alignment in total knee arthroplasty: Does it really matter? J. Orthop. 2016, 13, A1–A3. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Hsu, C.E.; Chen, C.P.; Wang, S.P.; Huang, J.T.; Tong, K.M.; Huang, K.C. Validation and modification of the Coronal Plane Alignment of the Knee classification in the Asian population. Bone Jt. Open 2022, 3, 211–217. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- MacDessi, S.J.; Griffiths-Jones, W.; Harris, I.A.; Bellemans, J.; Chen, D.B. The arithmetic HKA (aHKA) predicts the constitutional alignment of the arthritic knee compared to the normal contralateral knee: A matched-pairs radiographic study. Bone Jt. Open 2020, 1, 339–345. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Baek, J.H.; Lee, S.C.; Ryu, S.; Ahn, H.S.; Nam, C.H. Coronal Correction for Post-Traumatic Malalignment Using Robot-Assisted Total Knee Arthroplasty: A Case Series. Orthop. Res. Rev. 2022, 14, 445–451. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Roussot, M.A.; Vles, G.F.; Oussedik, S. Clinical outcomes of kinematic alignment versus mechanical alignment in total knee arthroplasty: A systematic review. EFORT Open Rev. 2020, 5, 486–497. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Howell, S.M.; Papadopoulos, S.; Kuznik, K.; Ghaly, L.R.; Hull, M.L. Does varus alignment adversely affect implant survival and function six years after kinematically aligned total knee arthroplasty? Int. Orthop. 2015, 39, 2117–2124. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.-H.; Park, J.-W.; Kim, J.-S.; Park, S.-D. The relationship between the survival of total knee arthroplasty and postoperative coronal, sagittal and rotational alignment of knee prosthesis. Int. Orthop. 2013, 38, 379. [Google Scholar] [CrossRef] [PubMed]
- Hourlier, H.; Fennema, P. Intraoperative fluoroscopy improves surgical precision in conventional TKA. Knee Surg. Sports Traumatol. Arthrosc. 2014, 22, 1619–1625. [Google Scholar] [CrossRef] [PubMed]
- Abdelnasser, M.K.; Elsherif, M.E.; Bakr, H.; Mahran, M.; Othman, M.H.M.; Khalifa, Y. All types of component malrotation affect the early patient-reported outcome measures after total knee arthroplasty. Knee. Surg. Relat. Res. 2019, 31, 5. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Tian, G.; Wang, L.; Liu, L.; Zhang, Y.; Zuo, L.; Li, J. Kinematic alignment versus mechanical alignment in total knee arthroplasty: An up-to-date meta-analysis. J. Orthop. Surg. 2022, 30, 10225536221125952. [Google Scholar] [CrossRef] [PubMed]
- Kohn, M.D.; Sassoon, A.A.; Fernando, N.D. Classifications in Brief: Kellgren-Lawrence Classification of Osteoarthritis. Clin. Orthop. Relat. Res. 2016, 474, 1886–1893. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Luger, M.; Schopper, C.; Krottenthaler, E.S.; Mahmoud, M.; Heyse, T.; Gotterbarm, T.; Klasan, A. Not all questions are created equal: The weight of the Oxford Knee Scores questions in a multicentric validation study. J. Orthop. Traumatol. 2023, 24, 44. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Culliton, S.E.; Bryant, D.M.; MacDonald, S.J.; Hibbert, K.M.; Chesworth, B.M. Validity and Internal Consistency of the New Knee Society Knee Scoring System. Clin. Orthop. Relat. Res. 2018, 476, 77–84. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Sava, M.P.; Schelker, B.L.; Khan, Z.A.; Amsler, F.; Hirschmann, M.T. Use of the forgotten joint score (FJS)-12 to evaluate knee awareness after quadriceps tendon reconstruction. BMC Musculoskelet. Disord. 2023, 24, 431. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ware JEJr Sherbourne, C.D. The MOS 36-item short-form health survey (SF–36). I. Conceptual framework and item selection. Med. Care 1992, 30, 473–483. [Google Scholar] [CrossRef] [PubMed]
- Clement, N.D.; Afzal, I.; Demetriou, C.; Deehan, D.J.; Field, R.E.; Kader, D. There is no clinically important difference in the Oxford knee scores between one and two years after total knee arthroplasty: The one-year score could be used as the benchmark timepoint to assess outcome. Knee 2020, 27, 1212–1218. [Google Scholar] [CrossRef] [PubMed]
- Sheehy, L.; Felson, D.; Zhang, Y.; Niu, J.; Lam, Y.M.; Segal, N.; Lynch, J.; Cooke, T.D. Does measurement of the anatomic axis consistently predict hip-knee-ankle angle (HKA) for knee alignment studies in osteoarthritis? Analysis of long limb radiographs from the multicenter osteoarthritis (MOST) study. Osteoarthr. Cartil. 2011, 19, 58–64. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Vickers, A.J.; Altman, D.G. Statistics notes: Analysing controlled trials with baseline and follow up measurements. BMJ 2001, 323, 1123–1124. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Biau, D.J.; Kernéis, S.; Porcher, R. Statistics in brief: The importance of sample size in the planning and interpretation of medical research. Clin. Orthop. Relat Res. 2008, 466, 2282–2288. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Rosenberg, N.; Soudry, M. Survivorship analysis of orthopedic procedures–practical approach. Arthroscopy 2011, 27 (Suppl. S4), 16–24. [Google Scholar]
- Greene, W.B. (Ed.) Essentials of Musculoskeletal Care, 5th ed.; American Academy of Orthopaedic Surgeons: Rosemont, IL, USA, 2016; p. 655. [Google Scholar]
- Kayani, B.; Konan, S.; Huq, S.S.; Tahmassebi, J.; Haddad, F.S. Robotic-arm assisted total knee arthroplasty has a learning curve of seven cases for integration into the surgical workflow but no learning curve effect for accuracy of implant positioning. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 1132–1141. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Alrajeb, R.; Zarti, M.; Shuia, Z.; Alzobi, O.; Ahmed, G.; Elmhiregh, A. Robotic-assisted versus conventional total knee arthroplasty: A systematic review and meta-analysis of randomized controlled trials. Eur. J. Orthop. Surg. Traumatol. 2024, 34, 1333–1343. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Winnock de Grave, P.; Luyckx, T.; Claeys, K.; Tampere, T.; Kellens, J.; Müller, J.; Gunst, P. Higher satisfaction after total knee arthroplasty using restricted inverse kinematic alignment compared to adjusted mechanical alignment. Knee Surg. Sports Traumatol. Arthrosc. 2022, 30, 488–499. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Van Essen, J.; Stevens, J.; Dowsey, M.M.; Choong, P.F.; Babazadeh, S. Kinematic alignment results in clinically similar outcomes to mechanical alignment: Systematic review and meta-analysis. Knee 2023, 40, 24–41. [Google Scholar] [CrossRef] [PubMed]
- Young, S.W.; Walker, M.L.; Bayan, A.; Briant-Evans, T.; Pavlou, P.; Farrington, B. The Chitranjan S. Ranawat Award: No Difference in 2-year Functional Outcomes Using Kinematic versus Mechanical Alignment in TKA: A Randomized Controlled Clinical Trial. Clin. Orthop. Relat. Res. 2017, 475, 9–20. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Dossett, H.G.; Estrada, N.A.; Swartz, G.J.; LeFevre, G.W.; Kwasman, B.G. A randomised controlled trial of kinematically and mechanically aligned total knee replacements: Two-year clinical results. Bone Jt. J. 2014, 96-B, 907–913. [Google Scholar] [CrossRef] [PubMed]
- Waterson, H.B.; Clement, N.D.; Eyres, K.S.; Mandalia, V.I.; Toms, A.D. The early outcome of kinematic versus mechanical alignment in total knee arthroplasty: A prospective randomised control trial. Bone Jt. J. 2016, 98-B, 1360–1368. [Google Scholar] [CrossRef] [PubMed]
- Vaidya, N.V.; Deshpande, A.N.; Panjwani, T.; Patil, R.; Jaysingani, T.; Patil, P. Robotic-assisted TKA leads to a better prosthesis alignment and better joint line restoration as compared to conventional TKA: A prospective randomized controlled trial. Knee Surg. Sports Traumatol. Arthrosc. 2022, 30, 621–626. [Google Scholar] [CrossRef]
- Miura, T.; Otani, T.; Mawatari, M. Range of motion following mechanical and kinematic alignment in total knee arthroplasty: A systematic review and meta-analysis. J. Orthop. Sci. 2023, 28, 237–245. [Google Scholar] [CrossRef]
- Liu, B.; Feng, C.; Tu, C. Kinematic alignment versus mechanical alignment in primary total knee arthroplasty: An updated meta-analysis of randomized controlled trials. J. Orthop. Surg. Res. 2022, 17, 201. [Google Scholar] [CrossRef]
- Kafelov, M.; Batailler, C.; Shatrov, J.; Al-Jufaili, J.; Farhat, J.; Servien, E.; Lustig, S. Functional positioning principles for image-based robotic-assisted TKA achieved a higher Forgotten Joint Score at 1 year compared to conventional TKA with restricted kinematic alignment. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 5591–5602. [Google Scholar] [CrossRef]
- Clement, N.D.; Scott, C.E.H.; Hamilton, D.F.; MacDonald, D.; Howie, C.R. Meaningful values in the Forgotten Joint Score after total knee arthroplasty. Bone Jt. J. 2021, 103-B, 846–854. [Google Scholar] [CrossRef] [PubMed]


| Group | n | Average | Standard Deviation | p (t-Test) | |
|---|---|---|---|---|---|
| Age (years) | 1 | 49 | 67 | 9 | 0.58 |
| 2 | 47 | 66 | 7 | ||
| Female | 1 | 36 (73%) | - | - | |
| 2 | 35 (74%) | - | - | ||
| Male | 1 | 13 (27%) | - | - | |
| 2 | 12 (26%) | - | - | ||
| BMI (kg/m2) | 1 | 49 | 30.45 | 5.07 | 0.39 |
| 2 | 47 | 31.31 | 4.65 | ||
| HKA prior operation (°) | 1 | 49 | 172.61 | 1.08 | 0.14 |
| 2 | 47 | 172.91 | 0.88 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lychagin, A.V.; Gritsyuk, A.A.; Elizarov, M.P.; Gritsuk, A.A., Jr.; Gavlovsky, M.Y.; Tomboidi, K.K.; Kalinsky, E.B.; Rosenberg, N. Mechanical Versus Restrictive Kinematic Alignment in Robotic-Assisted Total Knee Arthroplasty: A Randomized Controlled Trial. Diagnostics 2025, 15, 2524. https://doi.org/10.3390/diagnostics15192524
Lychagin AV, Gritsyuk AA, Elizarov MP, Gritsuk AA Jr., Gavlovsky MY, Tomboidi KK, Kalinsky EB, Rosenberg N. Mechanical Versus Restrictive Kinematic Alignment in Robotic-Assisted Total Knee Arthroplasty: A Randomized Controlled Trial. Diagnostics. 2025; 15(19):2524. https://doi.org/10.3390/diagnostics15192524
Chicago/Turabian StyleLychagin, Alexey V., Andrey A. Gritsyuk, Mikhail P. Elizarov, Andrey A. Gritsuk, Jr., Maxim Y. Gavlovsky, Konstantin K. Tomboidi, Eugene B. Kalinsky, and Nahum Rosenberg. 2025. "Mechanical Versus Restrictive Kinematic Alignment in Robotic-Assisted Total Knee Arthroplasty: A Randomized Controlled Trial" Diagnostics 15, no. 19: 2524. https://doi.org/10.3390/diagnostics15192524
APA StyleLychagin, A. V., Gritsyuk, A. A., Elizarov, M. P., Gritsuk, A. A., Jr., Gavlovsky, M. Y., Tomboidi, K. K., Kalinsky, E. B., & Rosenberg, N. (2025). Mechanical Versus Restrictive Kinematic Alignment in Robotic-Assisted Total Knee Arthroplasty: A Randomized Controlled Trial. Diagnostics, 15(19), 2524. https://doi.org/10.3390/diagnostics15192524








