Radar-Based Detection of Obstructive Sleep Apnea: A Systematic Review and Network Meta-Analysis of Diagnostic Accuracy Across Frequency Bands
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy and Selection Criteria
2.2. Inclusion and Exclusion Criteria
2.3. Data Extraction and Analysis
3. Results
3.1. Study Selections and Quality Assessment
| Lead Author and Year | Design | Country | Mean Age (Years) | Sex (% Male) | Radar | Comparison | Target | Total N | Purpose | Classification System or Algorithm | Distance (Sensor–Bed/Participant) | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Type | Band | Frequency | Setup | |||||||||||
| Zaffaroni 2009 [57] | Cross-sectional | Ireland | 53.9 | 82.2 | Pulsed | C | 5.8 GHz | Single | PSG | OSA | 157 | Algorithm development and initial validation | Proprietary software, including sleep/wake algorithm | 0.2 m from subject, 0.5 m elevation from bed edge |
| Zaffaroni 2012 [58] | Cross-sectional | Ireland | 49.9 | 79.7 | Pulsed | C | 5.8 GHz | Single | PSG | OSA | 75 | Clinical performance validation | Proprietary software, including sleep/wake algorithm, and respiratory envelope analysis | ≤1.5 m |
| Gotoh 2016 [59] | Cross-sectional | Japan | 49.8 | 80 | CW | X | 10.525 GHz | Dual | PSG, SpO2 | OSA | 20 | Clinical performance validation | Event detection based on respiratory amplitude change and phase angle filtering; moving average baseline comparison | Two radar sensors placed under mattress, approx. 30 cm below shoulders, and 20 cm laterally from center line |
| Wein-reich 2017 [53] | Cross-sectional | Germany | 56.4 | 80.7 | Pulsed | C | 5.8 GHz | Single | PSG | OSA, PLMS, CSR | 57 | Clinical validation in detecting combined SDB and PLMS using SDI as a unified index | Movement-based analysis using Doppler phase shifts; SDI (AHI and PLMI); rule-out screening approach | Device placed <1 m from bed, 0.25–0.5 m above mattress, aimed at the torso |
| Gotoh 2018 [60] | Cross-sectional | Japan | 49 | 81.5 | CW | X | 10.525 GHz | Dual | PSG | OSA | 27 | Clinical validation with adaptive hypopnea threshold optimization | Custom rule-based algorithm with ROC-based K-value optimization for hypopnea threshold | Sensors placed beneath mattress, each 20 cm left and right from the body midline, near the iliac bone |
| Crinion 2019 [41] | Cross-sectional | Ireland | 54.7 | 84.4 | Pulsed | C | 5.8 GHz | Single | PSG, HSAT | OSA, Hypertension | 125 | Clinical validation in both sleep clinic and hypertensive populations | Proprietary signal processing software (non-AI), includes respiration and motion analysis to estimate the AHI | Device placed on bedside table, approximately 1 m from patient |
| Kang 2020 [43] | Cross-sectional | South Korea | 45.7 | 80.9 | IR-UWB | C | 6.5–8.0 GHz | Single | PSG | OSA | 99 | Development and validation of an IR-UWB radar algorithm | constant false alarm rate (CFAR) algorithm with additional weight function adaptation; developed using MATLAB | 0.5 m from the head |
| Zhou 2020 [61] | Cross-sectional | China | 38.1 | 71 | UWB | C | 6–8 GHz | Single | PSG | OSA | 176 | Clinical performance validation | Embedded chip in radar for automatic AHI calculation (based on respiratory motion and body movement signals) | 1.5 m from patient, placed 15–25 cm above mattress on a bedside table |
| Anish-chenko 2021 [62] | Cross-sectional | Russia | 51.3 | 64.5 | NR | K | 24.0 and 24.1 GHz | Dual | PSG | OSA | 31 | Clinical performance validation | Ensemble ML classifier (Gentle Boost) trained on time/frequency features and entropy/Lyapunov measures from radar signals | Two radars: BRL1: 1.5 m lateral from bed, 1.2 m above floor, BRL2: wall-mounted above bed, 1.6 m high; both targeting chest |
| Kwon 2021 [63] | Cross-sectional | South Korea | 38.7 | 61.1 | IR-UWB | C | fc = 7.29 GHz, BW = 1.5 GHz | Single | PSG | OSA | 36 | Clinical validation of real-time AHI estimation using radar and deep learning without handcrafted features | Hybrid deep learning: CNN and BiLSTM for segment classification, with sliding 20 s window, and event detector based on consecutive AH-labeled segments | 0.84–1.32 m (mean 0.98 ± 0.31 m), placed on tripod facing chest |
| Li 2021 [39] | Cross-sectional | China | 47.8 | 80.3 | NR | NR | NR | Single | PSG | OSA | 71 | Clinical performance validation | Built-in automatic analysis system in radar device | 1 m away from the body; radar placed beside bed, with fingertip oxygen ring attached |
| Wei 2021 [40] | Cross-sectional | China | 43 | 83.6 | UWB | C | 6–8 GHz | Single | PSG | OSA | 67 | Clinical performance validation of a novel UWB radar device combined with a pulse oximeter ring | Fully automated analysis by the UWB device; uses respiratory motion and blood oxygen signals | 1 m from edge of bed, 0.5 m height, aligned with subject’s chest |
| Choi 2022 [64] | Cross-sectional | South Korea | 53.5 | 56.8 | FMCW | V | 60 GHz | Single | PSG | OSA | 44 | Clinical performance validation combined with deep learning | Deep learning: convolutional recurrent neural network (CRNN) | 2 m, ceiling-mounted above patient’s chest |
| Koda 2023 [54] | Cross-sectional | Japan | NR | NR | FMCW | W | 79 GHz | Single | PSG | OSA | 5 | Development of a radar-based, non-contact system using EM algorithm | Expectation–maximization (EM) algorithm on radar-derived respiratory displacement amplitude (non-AI, unsupervised statistical model) | 1.5 m (from radar echoes and hospital room setup); radar mounted to capture full body motion via array imaging |
| Lin 2024 [65] | Cross-sectional | Taiwan | 44.8 | 74.5 | CW | K | 24 GHz | Single | PSG | OSA | 196 | Development and validation of a non-contact 24-GHz radar system with deep learning (DL) | Hybrid DL (deep neural decision trees); machine learning techniques for respiratory event and sleep stage classification | 1–1.5 m |
| Gross-Isselmann 2024 [66] | Cross-sectional | Germany | 51.98 | 57 | CW | K | 24 GHz | Single | PSG | OSA | 141 | Performance validation in clinical and home environs | Proprietary automatic scoring algorithm (not DL) with optional SpO2 integration | 50 cm from thorax, mounted beside the bed slightly above mattress level |
| Wang 2024 [55] | Cross-sectional | China | NR | NR | FMCW | V | fc = 60 GHz, BW = 3 GHz | Single | PSG | OSA | 100 | Development and validation of ROSA—a radar plus SpO2 fusion system combined with deep learning | Deep learning: RASA R-CNN for event detection, RassNet for sleep staging, soft fusion of radar and SpO2 | Radar mounted above the head of the bed, facing the chest |
| Li-Chenyang 2024 [67] | Cross-sectional | China | 35.3 | 51.7 | NR | mm | NR | Single | PSG | OSA | 155 | Clinical performance validation | Signal fusion of radar and oximeter data using ML-based classification algorithms | Device placed beside bed in sleep lab |
| Li-Siheng 2024 [68] | Cross-sectional | China | NR | 76 | IR-UWB | C | fc = 7.3 GHz, BW = 1.4 GHz | Single | PSG | OSA | 18 | Development and validation of Respnea, a non-intrusive, fine-grained respiration monitoring system using radar and DL | CNN-based encoder, multi-head self-attention, contrastive learning; AI-based model | 40–100 cm (optimal range tested); device placed on nightstand beside bed |
| Röcken 2025 [69] | Cross-sectional | Switzer-land | 55.3 | 60.8 | CW | K | 24 GHz | Single | PSG | OSA | 102 | Clinical performance validation | Proprietary signal processing by manufacturer | 40–50 cm |
| AHI Threshold | Test Accuracy Summary | Participants (n Studies) | Subgroup Results | Results per 1000 Patients (95% CI) | Factors that May Decrease Certainty of the Evidence | Certainty of Evidence (GRADE) |
|---|---|---|---|---|---|---|
| AHI ≥ 5 | Pooled sensitivity: 0.944 (0.912–0.964) Pooled specificity: 0.699 (0. 519–0. 833) AUC: 0.941 I2 = 10.7% | 1435 (18) | Prevalence: 77.42% | Risk of bias: Not serious; Indirectness: Not serious; Inconsistency: Not serious; Imprecision: Not serious Publication bias: Strongly detected | ⊕⊕⊕⊝ Moderate | |
| TPs: 1055 FNs: 56 TNs: 233 FPs: 91 | TPs: 731 (706–747) FNs: 44 (28–68) TNs: 158 (117–188) FPs: 68 (38–109) | |||||
| AHI ≥ 15 | Pooled sensitivity: 0.879 (0.827–0.916) Pooled specificity: 0.897 (0.818–0. 944) AUC: 0.935 I2 = 12.8% | 1468 (18) | Prevalence: 51.57% | Risk of bias: Not serious; Indirectness: Not serious; Inconsistency: Not serious; Imprecision: Not serious Publication bias: Strongly detected | ⊕⊕⊕⊝ Moderate | |
| TPs: 678 FNs: 79 TNs: 631 FPs: 80 | TPs: 453 (426–473) FNs: 63 (43–89) TNs: 434 (396–457) FPs: 50 (27–88) | |||||
| AHI ≥ 30 | Pooled sensitivity: 0.827 (0.699–0.908) Pooled specificity: 0.950 (0.900–0.976) AUC: 0.957 I2 = 17.8% | 1289 (15) | Prevalence: 32.12% | Risk of bias: Not serious; Indirectness: Not serious; Inconsistency: Not serious; Imprecision: Not serious Publication bias: Strongly detected | ⊕⊕⊕⊝ Moderate | |
| TPs: 347 FNs: 67 TNs: 832 FPs: 43 | TPs: 266 (224–292) FNs: 56 (30–97) TNs: 645 (611–662) FPs: 34 (16–68) | |||||
3.2. Study Characteristics
3.3. Summary Statistics
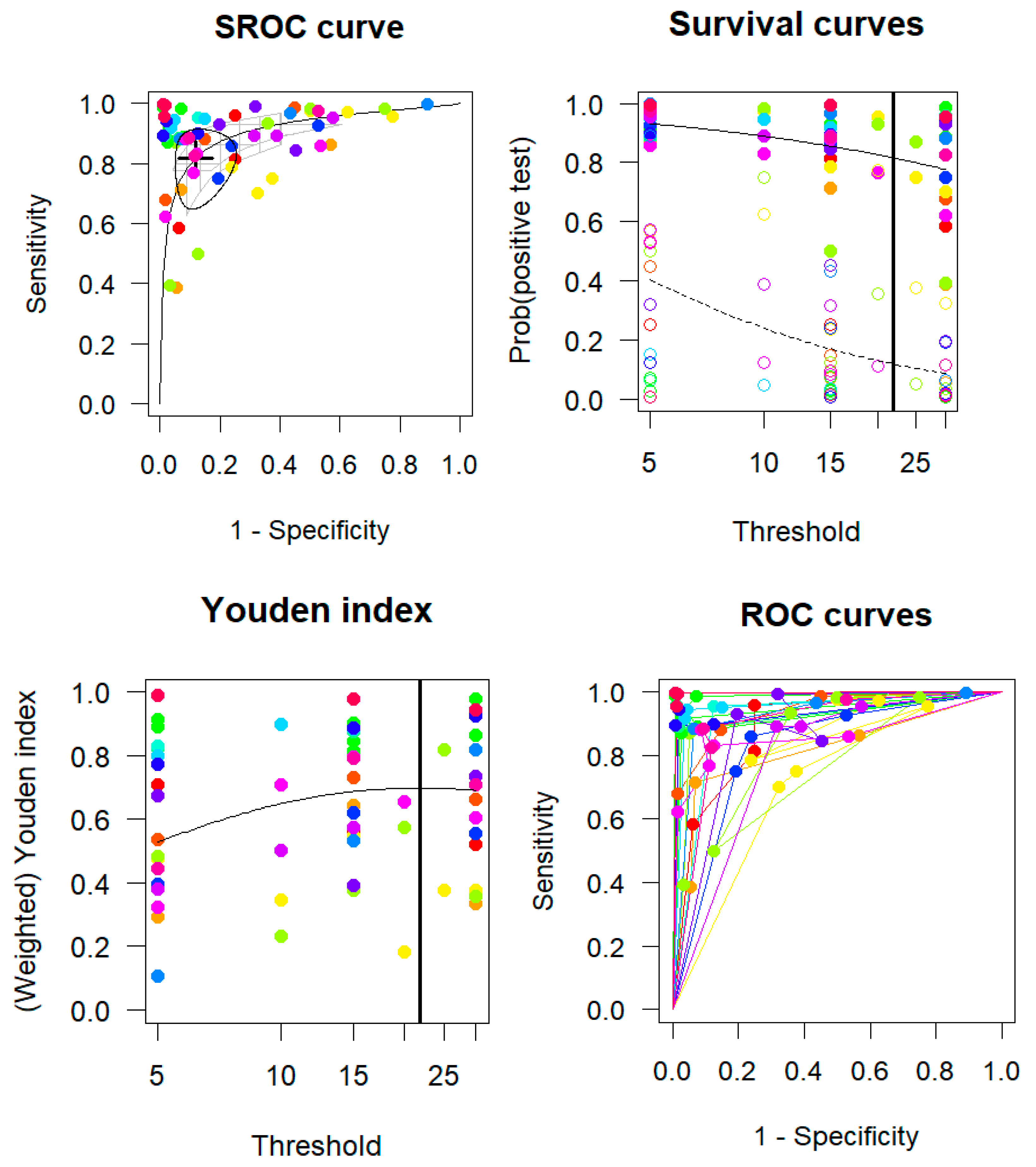
3.4. Multiple Cutoffs Model
3.5. Network Meta-Analysis of Radar Bands
3.6. Sensitivity Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AHI | Apnea–hypopnea index |
| AI | Artificial intelligence |
| AUC | Area under the curve |
| BW | Bandwidth |
| CI | Confidence interval |
| CW | Continuous wave |
| DL | Deep learning |
| fc | Center frequency |
| FMCW | Frequency-modulated continuous wave |
| FN | False negative |
| FP | False positive |
| HSAT | Home sleep apnea testing |
| IEEE | Institute of Electrical and Electronics Engineers |
| IRUWB | Impulse radio ultra-wideband |
| LFMCW | Linear frequency-modulated continuous wave |
| ML | Machine learning |
| OSA | Obstructive sleep apnea |
| PLMS | Periodic limb movement in sleep |
| PSG | Polysomnography |
| ROC | Receiver operating characteristic |
| SDI | Sleep disorder index |
| SFCW | Step frequency continuous wave |
| TN | True negative |
| TP | True positive |
| VHF | Very high frequency |
References
- Yaggi, H.K.; Concato, J.; Kernan, W.N.; Lichtman, J.H.; Brass, L.M.; Mohsenin, V. Obstructive sleep apnea as a risk factor for stroke and death. N. Engl. J. Med. 2005, 353, 2034–2041. [Google Scholar] [CrossRef]
- Cappuccio, F.P.; D’Elia, L.; Strazzullo, P.; Miller, M.A. Sleep duration and all-cause mortality: A systematic review and meta-analysis of prospective studies. Sleep 2010, 33, 585–592. [Google Scholar] [CrossRef]
- Zheng, N.S.; Annis, J.; Master, H.; Han, L.; Gleichauf, K.; Ching, J.H.; Nasser, M.; Coleman, P.; Desine, S.; Ruderfer, D.M.; et al. Sleep patterns and risk of chronic disease as measured by long-term monitoring with commercial wearable devices in the All of Us Research Program. Nat. Med. 2024, 30, 2648–2656. [Google Scholar] [CrossRef] [PubMed]
- von Ruesten, A.; Weikert, C.; Fietze, I.; Boeing, H. Association of sleep duration with chronic diseases in the European Prospective Investigation into Cancer and Nutrition (EPIC)-Potsdam study. PLoS ONE 2012, 7, e30972. [Google Scholar] [CrossRef] [PubMed]
- Drager, L.F.; Togeiro, S.M.; Polotsky, V.Y.; Lorenzi-Filho, G. Obstructive sleep apnea: A cardiometabolic risk in obesity and the metabolic syndrome. J. Am. Coll. Cardiol. 2013, 62, 569–576. [Google Scholar] [CrossRef] [PubMed]
- Gangwisch, J.E.; Heymsfield, S.B.; Boden-Albala, B.; Buijs, R.M.; Kreier, F.; Pickering, T.G.; Rundle, A.G.; Zammit, G.K.; Malaspina, D. Short Sleep Duration as a Risk Factor for Hypertension. Hypertension 2006, 47, 833–839. [Google Scholar] [CrossRef]
- Cappuccio, F.P.; D’Elia, L.; Strazzullo, P.; Miller, M.A. Quantity and quality of sleep and incidence of type 2 diabetes: A systematic review and meta-analysis. Diabetes Care 2010, 33, 414–420. [Google Scholar] [CrossRef]
- Ghavami, T.; Kazeminia, M.; Ahmadi, N.; Rajati, F. Global Prevalence of Obstructive Sleep Apnea in the Elderly and Related Factors: A Systematic Review and Meta-Analysis Study. J. PeriAnesthesia Nurs. 2023, 38, 865–875. [Google Scholar] [CrossRef]
- Zasadzińska-Stempniak, K.; Zajączkiewicz, H.; Kukwa, A. Prevalence of Obstructive Sleep Apnea in the Young Adult Population: A Systematic Review. J. Clin. Med. 2024, 13, 1386. [Google Scholar] [CrossRef]
- Gottlieb, D.J.; Punjabi, N.M. Diagnosis and Management of Obstructive Sleep Apnea: A Review. JAMA 2020, 323, 1389–1400. [Google Scholar] [CrossRef]
- Benjafield, A.V.; Ayas, N.T.; Eastwood, P.R.; Heinzer, R.; Ip, M.S.M.; Morrell, M.J.; Nunez, C.M.; Patel, S.R.; Penzel, T.; Pépin, J.L.; et al. Estimation of the global prevalence and burden of obstructive sleep apnoea: A literature-based analysis. Lancet Respir. Med. 2019, 7, 687–698. [Google Scholar] [CrossRef]
- Young, T.; Evans, L.; Finn, L.; Palta, M. Estimation of the Clinically Diagnosed Proportion of Sleep Apnea Syndrome in Middle-aged Men and Women. Sleep 1997, 20, 705–706. [Google Scholar] [CrossRef]
- Bradicich, M.; Pengo, M.F.; Steier, J.; Schwarz, E.I. Cardiovascular effects of obstructive sleep apnoea and effects of continuous positive airway pressure therapy: Evidence from different study models. ERJ Open Res. 2025, 11, 00718–2024. [Google Scholar] [CrossRef]
- Loke, Y.K.; Brown, J.W.; Kwok, C.S.; Niruban, A.; Myint, P.K. Association of obstructive sleep apnea with risk of serious cardiovascular events: A systematic review and meta-analysis. Circ. Cardiovasc. Qual. Outcomes 2012, 5, 720–728. [Google Scholar] [CrossRef]
- McNicholas, W.T.; Bonsigore, M.R. Sleep apnoea as an independent risk factor for cardiovascular disease: Current evidence, basic mechanisms and research priorities. Eur. Respir. J. 2007, 29, 156–178. [Google Scholar] [CrossRef] [PubMed]
- Gami, A.S.; Olson, E.J.; Shen, W.K.; Wright, R.S.; Ballman, K.V.; Hodge, D.O.; Herges, R.M.; Howard, D.E.; Somers, V.K. Obstructive sleep apnea and the risk of sudden cardiac death: A longitudinal study of 10,701 adults. J. Am. Coll. Cardiol. 2013, 62, 610–616. [Google Scholar] [CrossRef] [PubMed]
- Kapur, V.K.; Auckley, D.H.; Chowdhuri, S.; Kuhlmann, D.C.; Mehra, R.; Ramar, K.; Harrod, C.G. Clinical Practice Guideline for Diagnostic Testing for Adult Obstructive Sleep Apnea: An American Academy of Sleep Medicine Clinical Practice Guideline. J. Clin. Sleep Med. 2017, 13, 479–504. [Google Scholar] [CrossRef] [PubMed]
- Corral, J.; Sánchez-Quiroga, M.; Carmona-Bernal, C.; Sánchez-Armengol, Á.; de la Torre, A.S.; Durán-Cantolla, J.; Egea, C.J.; Salord, N.; Monasterio, C.; Terán, J.; et al. Conventional Polysomnography Is Not Necessary for the Management of Most Patients with Suspected Obstructive Sleep Apnea. Noninferiority, Randomized Controlled Trial. Am. J. Respir. Crit. Care Med. 2017, 196, 1181–1190. [Google Scholar] [CrossRef]
- Le Bon, O.; Hoffmann, G.; Tecco, J.; Staner, L.; Noseda, A.; Pelc, I.; Linkowski, P. Mild to moderate sleep respiratory events: One negative night may not be enough. Chest 2000, 118, 353–359. [Google Scholar] [CrossRef]
- Marty, S.; Pantanella, F.; Ronco, A.; Dheman, K.; Magno, M. Investigation of mmWave Radar Technology For Non-contact Vital Sign Monitoring. In Proceedings of the 2023 IEEE International Symposium on Medical Measurements and Applications (MeMeA), Jeju, Republic of Korea, 14–16 June 2023; pp. 1–6. [Google Scholar]
- Boiko, A.; Martínez Madrid, N.; Seepold, R. Contactless Technologies, Sensors, and Systems for Cardiac and Respiratory Measurement during Sleep: A Systematic Review. Sensors 2023, 23, 5038. [Google Scholar] [CrossRef]
- Iqbal, F.M.; Lam, K.; Joshi, M.; Khan, S.; Ashrafian, H.; Darzi, A. Clinical outcomes of digital sensor alerting systems in remote monitoring: A systematic review and meta-analysis. npj Digit. Med. 2021, 4, 7. [Google Scholar] [CrossRef] [PubMed]
- Will, C.; Shi, K.; Schellenberger, S.; Steigleder, T.; Michler, F.; Fuchs, J.; Weigel, R.; Ostgathe, C.; Koelpin, A. Radar-Based Heart Sound Detection. Sci. Rep. 2018, 8, 11551. [Google Scholar] [CrossRef] [PubMed]
- Rong, Y.; Theofanopoulos, P.C.; Trichopoulos, G.C.; Bliss, D.W. A new principle of pulse detection based on terahertz wave plethysmography. Sci. Rep. 2022, 12, 6347. [Google Scholar] [CrossRef] [PubMed]
- Manullang, M.C.T.; Lin, Y.H.; Lai, S.J.; Chou, N.K. Implementation of Thermal Camera for Non-Contact Physiological Measurement: A Systematic Review. Sensors 2021, 21, 7777. [Google Scholar] [CrossRef]
- Park, J.-Y.; Lee, Y.; Heo, R.; Park, H.-K.; Cho, S.-H.; Cho, S.H.; Lim, Y.-H. Preclinical evaluation of noncontact vital signs monitoring using real-time IR-UWB radar and factors affecting its accuracy. Sci. Rep. 2021, 11, 23602. [Google Scholar] [CrossRef]
- Obadi, A.B.; Soh, P.J.; Aldayel, O.; Al-Doori, M.H.; Mercuri, M.; Schreurs, D. A Survey on Vital Signs Detection Using Radar Techniques and Processing With FPGA Implementation. IEEE Circuits Syst. Mag. 2021, 21, 41–74. [Google Scholar] [CrossRef]
- Li, B.; Zhou, Z.; Zou, W.; Li, D.; Zhao, C. Optimal waveforms design for ultra-wideband impulse radio sensors. Sensors 2010, 10, 11038–11063. [Google Scholar] [CrossRef]
- Fontana, R.J. Recent system applications of short-pulse ultra-wideband (UWB) technology. IEEE Trans. Microw. Theory Tech. 2004, 52, 2087–2104. [Google Scholar] [CrossRef]
- IEEE Std 521-2019 (Revision of IEEE Std 521-2002); IEEE Standard Letter Designations for Radar-Frequency Bands. IEEE: New York City, NY, USA, 2020. [CrossRef]
- Schires, E.; Georgiou, P.; Lande, T.S. Vital Sign Monitoring Through the Back Using an UWB Impulse Radar With Body Coupled Antennas. IEEE Trans. Biomed. Circuits Syst. 2018, 12, 292–302. [Google Scholar] [CrossRef]
- Lei, Q.; Tian, J.; Jun, Z.; Biying, L.; Zhimin, Z. A singular spectrum analysis based human life signal detection. In Proceedings of the 2016 Progress in Electromagnetic Research Symposium (PIERS), Shanghai, China, 8-11 August 2016; pp. 4295–4298. [Google Scholar]
- El Zein, G.; Zaharia, G.; Obeid, D.; Samad, S.; Sadek, S. Position-Free Vital Sign Monitoring: Measurements and Processing. In Advanced Biosignal Processing and Diagnostic Methods; Hintermüller, C., Ed.; IntechOpen: Rijeka, Croatia, 2016. [Google Scholar]
- Vorobyov, A.; Daskalaki, E.; Farserotu, J. Feasibility of Remote Vital Signs Sensing with a mm-Wave CW Reflectometer. In Proceedings of the 2018 IEEE 38th International Conference on Electronics and Nanotechnology (ELNANO), Kyiv, Ukraine, 24–26 April 2018; pp. 417–421. [Google Scholar]
- Alizadeh, M.; Shaker, G.; Almeida, J.C.M.D.; Morita, P.P.; Safavi-Naeini, S. Remote Monitoring of Human Vital Signs Using mm-Wave FMCW Radar. IEEE Access 2019, 7, 54958–54968. [Google Scholar] [CrossRef]
- Gaikwad, A.N.; Dongre, K.S. Improvement in detection of human life sign signal hidden behind the wall using clutter reduction technique. In Proceedings of the 2016 International Conference on Emerging Trends in Communication Technologies (ETCT), Dehradun, India, 18–19 November 2016; pp. 1–5. [Google Scholar]
- Phan, T.; Kilic, O.; Nahar, S.; Ren, L.; Fathy, A.E. Accuracy investigation of SFCW radar in human vital signs detection for subject’s relative position. In Proceedings of the 2017 IEEE International Symposium on Antennas and Propagation & USNC/URSI National Radio Science Meeting, San Diego, CA, USA, 9–14 July 2017; pp. 577–578. [Google Scholar]
- Fathy, A.E.; Ren, L.; Nahar, S.; Kilic, O. Overview of human vital signs detection using radar techniques. In Proceedings of the 2017 IEEE International Symposium on Antennas and Propagation & USNC/URSI National Radio Science Meeting, San Diego, CA, USA, 9–14 July 2017; pp. 1229–1230. [Google Scholar]
- Li, Y.; Song, Y.; Tian, C.; Liu, Y.; Liang, K.; Zhang, Y.; Qin, M.; Zha, D. Evaluation of clinical application of new remote radar monitoring equipment for obstructive sleep apnea. J. Clin. Otorhinolaryngol. Head Neck Surg. 2021, 35, 293–296. [Google Scholar] [CrossRef]
- Wei, Z.; Xu, J.; Li, W.Y.; Wang, X.; Qin, Z.; Zhou, J.; Wang, W. Evaluation of a non-contact ultra-wideband bio-radar sleep monitoring device for screening of sleep breathing disease. Sleep Breath. 2022, 26, 689–696. [Google Scholar] [CrossRef] [PubMed]
- Crinion, S.J.; Tiron, R.; Lyon, G.; Zaffaroni, A.; Kilroy, H.; Doheny, E.; O’Hare, E.; Boyle, P.; Russell, A.; Traynor, M.; et al. Ambulatory detection of sleep apnea using a non-contact biomotion sensor. J. Sleep Res. 2020, 29, e12889. [Google Scholar] [CrossRef] [PubMed]
- Khalil, C.; Zarabi, S.; Kirkham, K.; Soni, V.; Li, Q.; Huszti, E.; Yadollahi, A.; Taati, B.; Englesakis, M.; Singh, M. Validity of non-contact methods for diagnosis of Obstructive Sleep Apnea: A systematic review and meta-analysis. J. Clin. Anesth. 2023, 87, 111087. [Google Scholar] [CrossRef]
- Kang, S.; Kim, D.-K.; Lee, Y.; Lim, Y.-H.; Park, H.-K.; Cho, S.H.; Cho, S.H. Non-contact diagnosis of obstructive sleep apnea using impulse-radio ultra-wideband radar. Sci. Rep. 2020, 10, 5261. [Google Scholar] [CrossRef]
- Husaini, M.; Kamarudin, L.M.; Zakaria, A.; Kamarudin, I.K.; Ibrahim, M.A.; Nishizaki, H.; Toyoura, M.; Mao, X. Non-Contact Breathing Monitoring Using Sleep Breathing Detection Algorithm (SBDA) Based on UWB Radar Sensors. Sensors 2022, 22, 5249. [Google Scholar] [CrossRef]
- Hutton, B.; Salanti, G.; Caldwell, D.M.; Chaimani, A.; Schmid, C.H.; Cameron, C.; Ioannidis, J.P.; Straus, S.; Thorlund, K.; Jansen, J.P.; et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: Checklist and explanations. Ann. Intern. Med. 2015, 162, 777–784. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Macaskill, P.; Takwoingi, Y.; Deeks, J.J.; Gatsonis, C. Understanding meta-analysis. In Cochrane Handbook for Systematic Reviews of Diagnostic Test Accuracy; John Wiley & Sons: Hoboken, NJ, USA, 2023; pp. 203–247. [Google Scholar]
- Takwoingi, Y.; Dendukuri, N.; Schiller, I.; Rücker, G.; Jones, H.E.; Partlett, C.; Macaskill, P. Undertaking meta-analysis. In Cochrane Handbook for Systematic Reviews of Diagnostic Test Accuracy; John Wiley & Sons: Hoboken, NJ, USA, 2023; pp. 249–325. [Google Scholar]
- Troester, M.M.; Quan, S.F.; Berry, R.B.; Abreu, A.; Alzoubaidi, M.; Bandyopadhyay, A.; DelRosso, L.; Ebben, M.; Kwon, Y.; Mao, M.M.; et al. Home sleep apnea test (HSAT) rules for adults: Part 1—HSAT utilizing respiratory flow and/or effort parameters. In The AASM Manual for the Scoring of Sleep and Associated Events: Rules, Terminology and Technical Specifications, Version 3 ed.; American Academy of Sleep Medicine, Ed.; American Academy of Sleep Medicine: Darien, IL, USA, 2023. [Google Scholar]
- Lin, L.; Chu, H.; Murad, M.H.; Hong, C.; Qu, Z.; Cole, S.R.; Chen, Y. Empirical Comparison of Publication Bias Tests in Meta-Analysis. J. Gen. Intern. Med. 2018, 33, 1260–1267. [Google Scholar] [CrossRef]
- Leeflang, M.M.; Steingart, K.R.; Scholten, R.J.; Davenport, C. Drawing conclusions. In Cochrane Handbook for Systematic Reviews of Diagnostic Test Accuracy; John Wiley & Sons: Hoboken, NJ, USA, 2023; pp. 349–376. [Google Scholar]
- Reitsma, J.B.; Rutjes, A.W.; Whiting, P.; Yang, B.; Leeflang, M.M.; Bossuyt, P.M.; Deeks, J.J. Assessing risk of bias and applicability. In Cochrane Handbook for Systematic Reviews of Diagnostic Test Accuracy; John Wiley & Sons: Hoboken, NJ, USA, 2023; pp. 169–201. [Google Scholar]
- Weinreich, G.; Terjung, S.; Wang, Y.; Werther, S.; Zaffaroni, A.; Teschler, H. Validation of a non-contact screening device for the combination of sleep-disordered breathing and periodic limb movements in sleep. Sleep Breath. 2018, 22, 131–138. [Google Scholar] [CrossRef]
- Koda, T.; Okumura, S.; Taki, H.; Hamada, S.; Sunadome, H.; Sato, S.; Chin, K.; Sakamoto, T. Noncontact Detection of Sleep Apnea Using Radar and Expectation–Maximization Algorithm. IEEE Sens. J. 2024, 24, 32748–32756. [Google Scholar] [CrossRef]
- Wang, W.; Chen, Z.; Zhang, W.; Wang, Z.; Zhao, X.; Li, C.; Guan, J.; Yin, S.; Li, G. Fusion of millimeter-wave radar and pulse oximeter data for low-burden diagnosis of obstructive sleep apnea-hypopnea syndrome. arXiv 2025, arXiv:2501.15264. [Google Scholar] [CrossRef]
- Wang, W.; Li, C.; Chen, Z.; Zhang, W.; Wang, Z.; Guo, X.; Guan, J.; Li, G. Detection of Sleep Apnea-Hypopnea Events Using Millimeter-wave Radar and Pulse Oximeter. In Proceedings of the 2024 46th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Orlando, FL, USA, 15–19 July 2024; pp. 1–5. [Google Scholar] [CrossRef]
- Zaffaroni, A.; de Chazal, P.; Heneghan, C.; Boyle, P.; Mppm, P.R.; McNicholas, W.T. SleepMinder: An innovative contact-free device for the estimation of the apnoea-hypopnoea index. Annu. Int. Conf. IEEE Eng. Med. Biol. Soc. 2009, 2009, 7091–7094. [Google Scholar] [CrossRef] [PubMed]
- Zaffaroni, A.; Kent, B.; O’Hare, E.; Heneghan, C.; Boyle, P.; O’Connell, G.; Pallin, M.; de Chazal, P.; McNicholas, W.T. Assessment of sleep-disordered breathing using a non-contact bio-motion sensor. J. Sleep Res. 2013, 22, 231–236. [Google Scholar] [CrossRef] [PubMed]
- Gotoh, S.; Kaneko, H.; Matsui, T.; Naka, Y.; Kurita, O.; Yamashita, K. Development and clinical application of a non-contact sleep apnea monitoring system using a microwave radar sensor. Jpn. J. Med. Instrum. 2016, 86, 441–449. [Google Scholar] [CrossRef]
- Gotoh, S.; Matsui, T.; Naka, Y.; Kurita, O. The Development of a Dual-Radar System with Automatic Hypopnea Threshold Optimization for Contact-Free Sleep Apnea-Hypopnea Syndrome Screening. J. Sens. 2018, 2018, 8210502. [Google Scholar] [CrossRef]
- Zhou, Y.; Shu, D.; Xu, H.; Qiu, Y.; Zhou, P.; Ruan, W.; Qin, G.; Jin, J.; Zhu, H.; Ying, K.; et al. Validation of novel automatic ultra-wideband radar for sleep apnea detection. J. Thorac. Dis. 2020, 12, 1286–1295. [Google Scholar] [CrossRef]
- Anishchenko, L.; Lobanova, V.; Bochkarev, M.; Korostovtseva, L.; Sviryaev, Y. Two-Channel Bioradar System for Sleep-Disordered Breathing Detection. In Proceedings of the 2021 International Conference on e-Health and Bioengineering (EHB), Iasi, Romania, 18–19 November 2021; pp. 1–4. [Google Scholar]
- Kwon, H.B.; Son, D.; Lee, D.; Yoon, H.; Lee, M.H.; Lee, Y.J.; Choi, S.H.; Park, K.S. Hybrid CNN-LSTM Network for Real-Time Apnea-Hypopnea Event Detection Based on IR-UWB Radar. IEEE Access 2022, 10, 17556–17564. [Google Scholar] [CrossRef]
- Choi, J.W.; Kim, D.H.; Koo, D.L.; Park, Y.; Nam, H.; Lee, J.H.; Kim, H.J.; Hong, S.N.; Jang, G.; Lim, S.; et al. Automated Detection of Sleep Apnea-Hypopnea Events Based on 60 GHz Frequency-Modulated Continuous-Wave Radar Using Convolutional Recurrent Neural Networks: A Preliminary Report of a Prospective Cohort Study. Sensors 2022, 22, 7177. [Google Scholar] [CrossRef]
- Lin, S.Y.; Tsai, C.Y.; Majumdar, A.; Ho, Y.H.; Huang, Y.W.; Kao, C.K.; Yeh, S.M.; Hsu, W.H.; Kuan, Y.C.; Lee, K.Y.; et al. Combining a wireless radar sleep monitoring device with deep machine learning techniques to assess obstructive sleep apnea severity. J. Clin. Sleep Med. 2024, 20, 1267–1277. [Google Scholar] [CrossRef]
- Gross-Isselmann, J.A.; Eggert, T.; Wildenauer, A.; Dietz-Terjung, S.; Grosse Sundrup, M.; Schoebel, C. Validation of the Sleepiz One + as a radar-based sensor for contactless diagnosis of sleep apnea. Sleep Breath. 2024, 28, 1691–1699. [Google Scholar] [CrossRef]
- Li, C.Y.; Wang, W.; Huang, W.J.; Xu, H.H.; Yi, H.L.; Guan, J.; Li, G.; Yin, S.K. Diagnosis of obstructive sleep apnea by a new radar device: A parallel controlled study evaluating agreement with polysomnographic monitoring. Chin. J. Otorhinolaryngol. Head Neck Surg. 2024, 59, 857–863. [Google Scholar] [CrossRef]
- Li, S.; Jin, B.; Wang, Z.; Zhang, F.; Ren, X.; Liu, H. Leveraging Attention-reinforced UWB Signals to Monitor Respiration during Sleep. ACM Trans. Sen. Netw. 2024, 20, 1–28. [Google Scholar] [CrossRef]
- Röcken, J.; Darie, A.M.; Grize, L.; Dexter, C.E.; Herrmann, M.J.; Jahn, K.; Strobel, W.; Tamm, M.; Stolz, D. Diagnostic performance of a doppler radar-based sleep apnoea testing device. BMC Pulm. Med. 2025, 25, 150. [Google Scholar] [CrossRef] [PubMed]
- Dong, S.; Wen, L.; Ye, Y.; Zhang, Z.; Wang, Y.; Liu, Z.; Cao, Q.; Xu, Y.; Li, C.; Gu, C. A Review on Recent Advancements of Biomedical Radar for Clinical Applications. IEEE Open J. Eng. Med. Biol. 2024, 5, 707–724. [Google Scholar] [CrossRef] [PubMed]
- Kwon, M.S.; Park, Y.; Park, J.E.; Lee, G.H.; Jeon, S.H.; Lee, J.H.; Yoon, J.H.; Yang, J.R. Motion Cancellation Technique of Vital Signal Detectors Based on Continuous-Wave Radar Technology. Sensors 2025, 25, 2156. [Google Scholar] [CrossRef]
- Yang, Z.K.; Shi, H.; Zhao, S.; Huang, X.D. Vital Sign Detection during Large-Scale and Fast Body Movements Based on an Adaptive Noise Cancellation Algorithm Using a Single Doppler Radar Sensor. Sensors 2020, 20, 4183. [Google Scholar] [CrossRef]
- Collop Nancy, A.; Tracy Sharon, L.; Kapur, V.; Mehra, R.; Kuhlmann, D.; Fleishman Sam, A.; Ojile Joseph, M. Obstructive Sleep Apnea Devices for Out-Of-Center (OOC) Testing: Technology Evaluation. J. Clin. Sleep Med. 2011, 7, 531–548. [Google Scholar] [CrossRef]
- Pitkänen, M.; Nath, R.K.; Korkalainen, H.; Nikkonen, S.; Mahamid, A.; Oksenberg, A.; Duce, B.; Töyräs, J.; Kainulainen, S.; Leppänen, T. Respiratory event index underestimates severity of sleep apnea compared to apnea-hypopnea index. Sleep Adv. 2024, 5, zpad054. [Google Scholar] [CrossRef]
- Saletu, T.M.; Kotzian, T.K.; Schwarzinger, A.; Haider, S.; Spatt, J.; Saletu, B. Home Sleep Apnea Testing is a Feasible and Accurate Method to Diagnose Obstructive Sleep Apnea in Stroke Patients During In-Hospital Rehabilitation. J. Clin. Sleep Med. 2018, 14, 1495–1501. [Google Scholar] [CrossRef]
- Douglas, J.A.; Chai-Coetzer, C.L.; McEvoy, D.; Naughton, M.T.; Neill, A.M.; Rochford, P.; Wheatley, J.; Worsnop, C. Guidelines for sleep studies in adults—a position statement of the Australasian Sleep Association. Sleep Med. 2017, 36 (Suppl. 1), S2–S22. [Google Scholar] [CrossRef]
- Bazoukis, G.; Bollepalli, S.C.; Chung, C.T.; Li, X.; Tse, G.; Bartley, B.L.; Batool-Anwar, S.; Quan, S.F.; Armoundas, A.A. Application of artificial intelligence in the diagnosis of sleep apnea. J. Clin. Sleep Med. 2023, 19, 1337–1363. [Google Scholar] [CrossRef]
- Dai, R.; Yang, K.; Zhuang, J.; Yao, L.; Hu, Y.; Chen, Q.; Zheng, H.; Zhu, X.; Ke, J.; Zeng, Y.; et al. Enhanced machine learning approaches for OSA patient screening: Model development and validation study. Sci. Rep. 2024, 14, 19756. [Google Scholar] [CrossRef]
- Bandyopadhyay, A.; Oks, M.; Sun, H.; Prasad, B.; Rusk, S.; Jefferson, F.; Malkani Roneil, G.; Haghayegh, S.; Sachdeva, R.; Hwang, D.; et al. Strengths, weaknesses, opportunities, and threats of using AI-enabled technology in sleep medicine: A commentary. J. Clin. Sleep Med. 2024, 20, 1183–1191. [Google Scholar] [CrossRef]
- Kara, M.; Lakner, Z.; Tamás, L.; Molnár, V. Artificial intelligence in the diagnosis of obstructive sleep apnea: A scoping review. Eur. Arch. Oto-Rhino-Laryngol. 2025. [Google Scholar] [CrossRef]
- Hao, Z.; Gao, Y.; Tang, Y.; Wang, Y.; Fan, K.; Li, F. FMCW-based contactless heart rate monitoring. Sci. Rep. 2025, 15, 2616. [Google Scholar] [CrossRef] [PubMed]
- Frazao, A.; Pinho, P.; Albuquerque, D. Radar-Based Heart Cardiac Activity Measurements: A Review. Sensors 2024, 24, 7654. [Google Scholar] [CrossRef] [PubMed]
- Soumya, A.; Krishna Mohan, C.; Cenkeramaddi, L.R. Recent Advances in mmWave-Radar-Based Sensing, Its Applications, and Machine Learning Techniques: A Review. Sensors 2023, 23, 8901. [Google Scholar] [CrossRef] [PubMed]
- Paterniani, G.; Sgreccia, D.; Davoli, A.; Guerzoni, G.; Viesti, P.D.; Valenti, A.C.; Vitolo, M.; Vitetta, G.M.; Boriani, G. Radar-Based Monitoring of Vital Signs: A Tutorial Overview. Proc. IEEE 2023, 111, 277–317. [Google Scholar] [CrossRef]
- Chaimani, A.; Higgins, J.P.T.; Mavridis, D.; Spyridonos, P.; Salanti, G. Graphical Tools for Network Meta-Analysis in STATA. PLoS ONE 2013, 8, e76654. [Google Scholar] [CrossRef]
- Zinchuk, A.V.; Gentry, M.J.; Concato, J.; Yaggi, H.K. Phenotypes in obstructive sleep apnea: A definition, examples and evolution of approaches. Sleep Med. Rev. 2017, 35, 113–123. [Google Scholar] [CrossRef]
- McInnes, M.D.F.; Moher, D.; Thombs, B.D.; McGrath, T.A.; Bossuyt, P.M.; The PRISMA-DTA Group; Clifford, T.; Cohen, J.F.; Deeks., J.J.; Gatsonis, C.; et al. Preferred Reporting Items for a Systematic Review and Meta-analysis of Diagnostic Test Accuracy Studies: The PRISMA-DTA Statement. JAMA 2018, 319, 388–396. [Google Scholar] [CrossRef]





| Treatment | P Score (Common) | P Score (Random) |
|---|---|---|
| PSG | 0.9971 | 0.9861 |
| X-band | 0.736 | 0.6961 |
| K-band | 0.4964 | 0.5007 |
| C-band | 0.2577 | 0.2332 |
| V-band | 0.0128 | 0.0838 |
| PSG | 0.9977 | 0.9904 |
| X-band-CW | 0.7752 | 0.7308 |
| C-band-Pulsed | 0.5309 | 0.5265 |
| K-band-CW | 0.4926 | 0.5096 |
| V-band-FMCW | 0.0742 | 0.1426 |
| C-band-UWB | 0.1294 | 0.1002 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tran, N.B.M.H.; Tran, T.Q.T.; Tsai, C.-Y.; Kang, J.-H. Radar-Based Detection of Obstructive Sleep Apnea: A Systematic Review and Network Meta-Analysis of Diagnostic Accuracy Across Frequency Bands. Diagnostics 2025, 15, 2111. https://doi.org/10.3390/diagnostics15162111
Tran NBMH, Tran TQT, Tsai C-Y, Kang J-H. Radar-Based Detection of Obstructive Sleep Apnea: A Systematic Review and Network Meta-Analysis of Diagnostic Accuracy Across Frequency Bands. Diagnostics. 2025; 15(16):2111. https://doi.org/10.3390/diagnostics15162111
Chicago/Turabian StyleTran, Nguyen Binh Minh Hoang, Thi Quynh Trang Tran, Cheng-Yu Tsai, and Jiunn-Horng Kang. 2025. "Radar-Based Detection of Obstructive Sleep Apnea: A Systematic Review and Network Meta-Analysis of Diagnostic Accuracy Across Frequency Bands" Diagnostics 15, no. 16: 2111. https://doi.org/10.3390/diagnostics15162111
APA StyleTran, N. B. M. H., Tran, T. Q. T., Tsai, C.-Y., & Kang, J.-H. (2025). Radar-Based Detection of Obstructive Sleep Apnea: A Systematic Review and Network Meta-Analysis of Diagnostic Accuracy Across Frequency Bands. Diagnostics, 15(16), 2111. https://doi.org/10.3390/diagnostics15162111







