Heart vs. Brain in a Warzone: The Effects of War on Acute Cardiovascular and Neurological Emergencies
Abstract
1. Introduction
2. Methods
2.1. Study Design and Population
2.2. Data Collection
2.3. Outcomes
2.4. Statistical Analysis
3. Results
3.1. Study Population
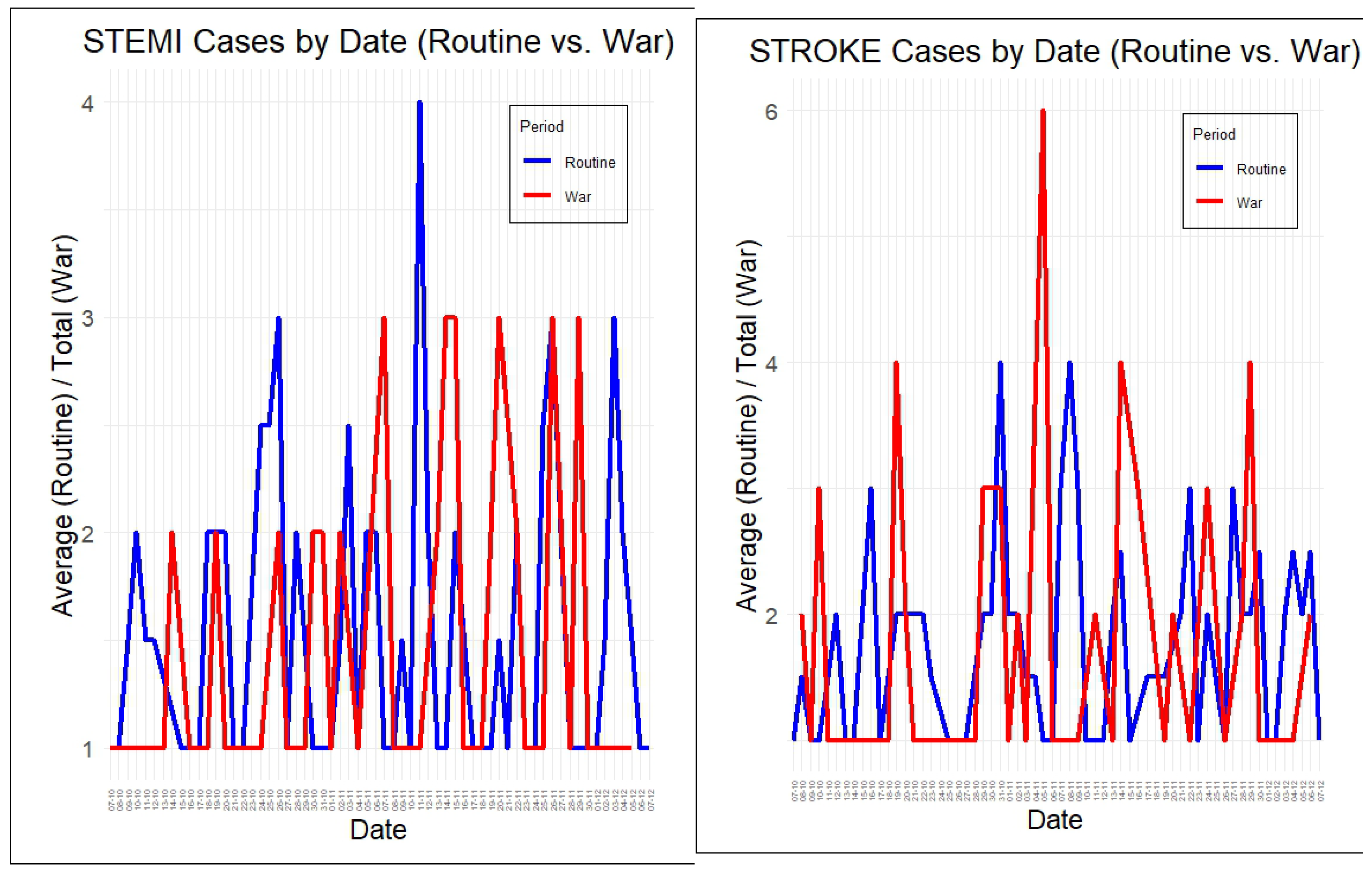
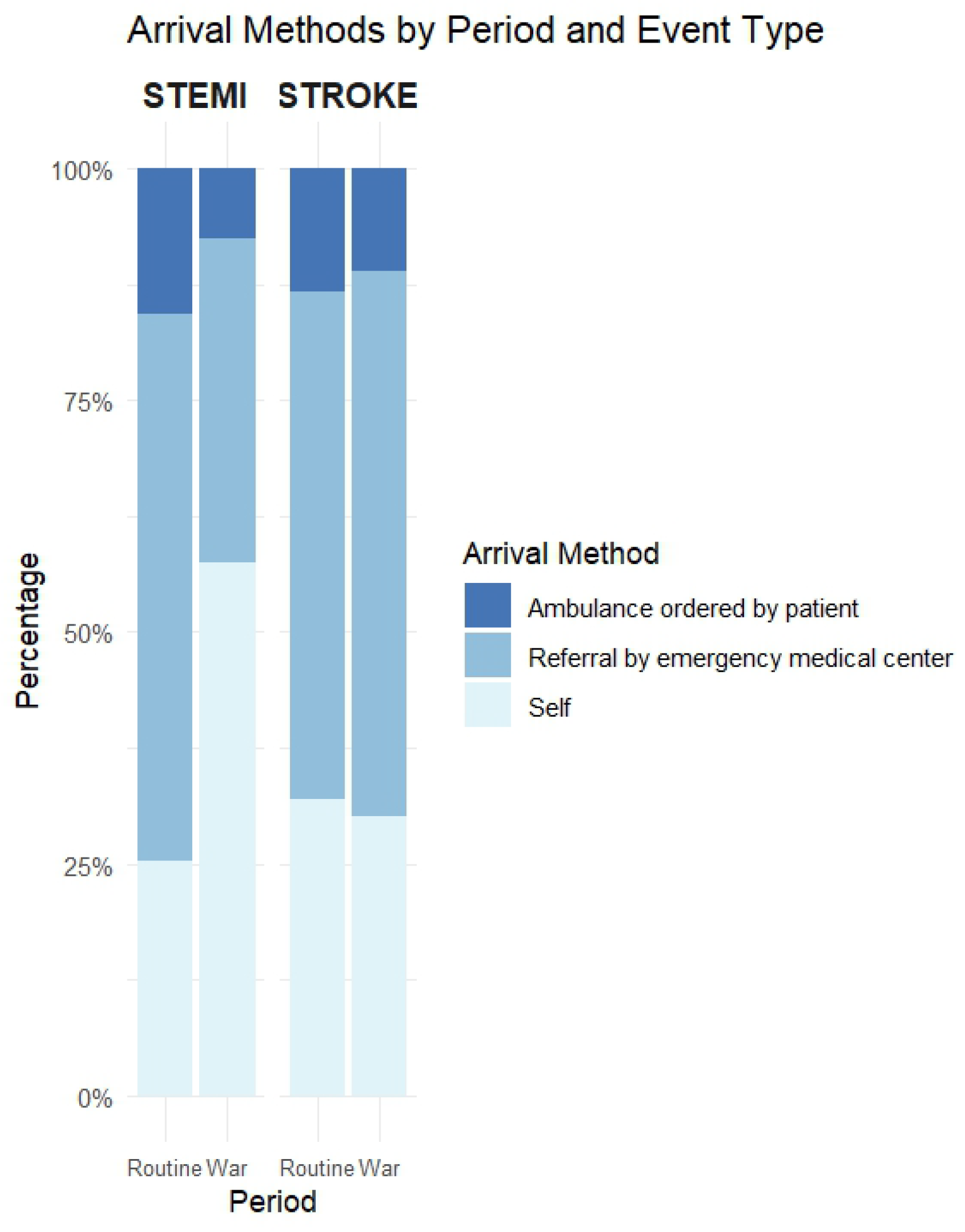
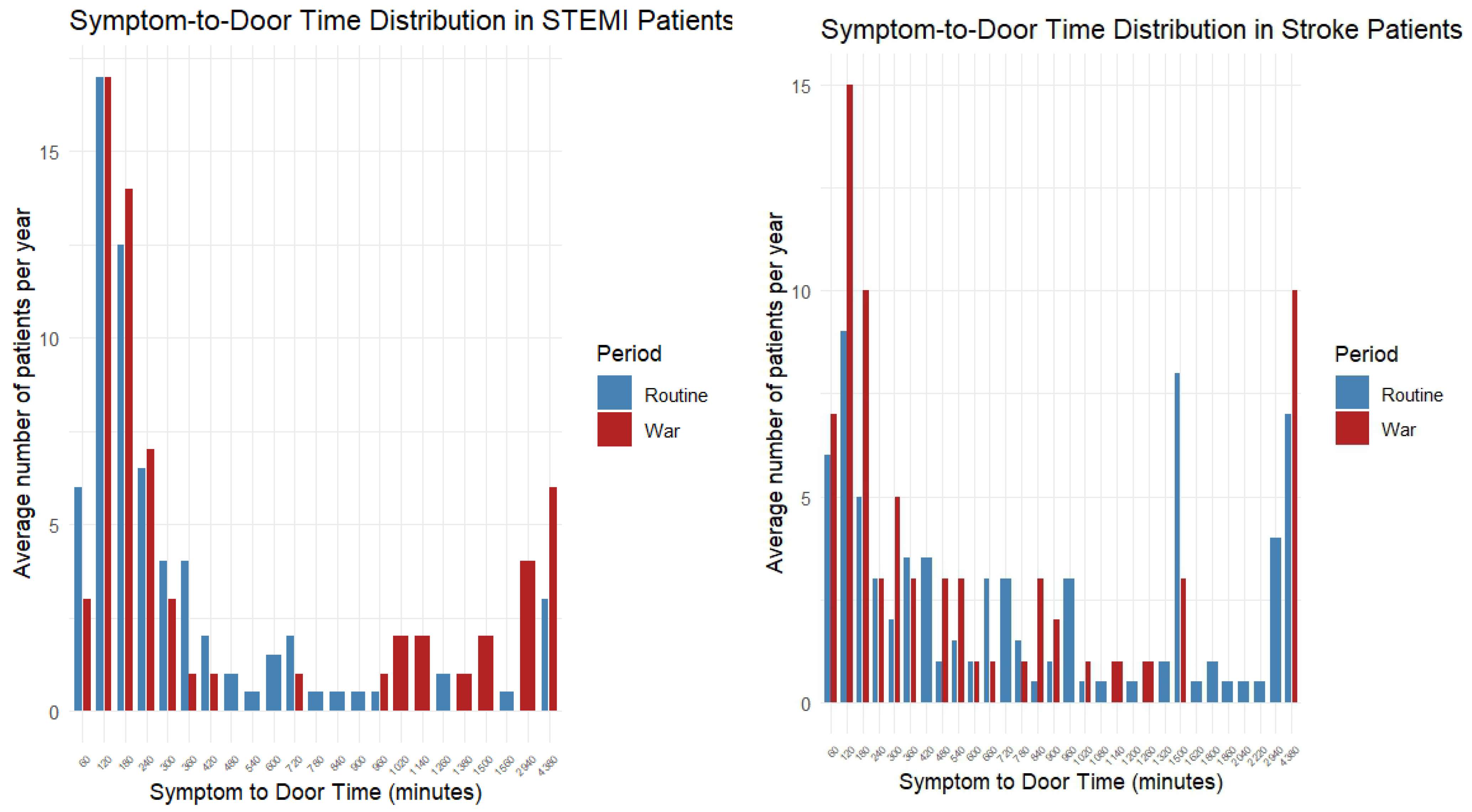
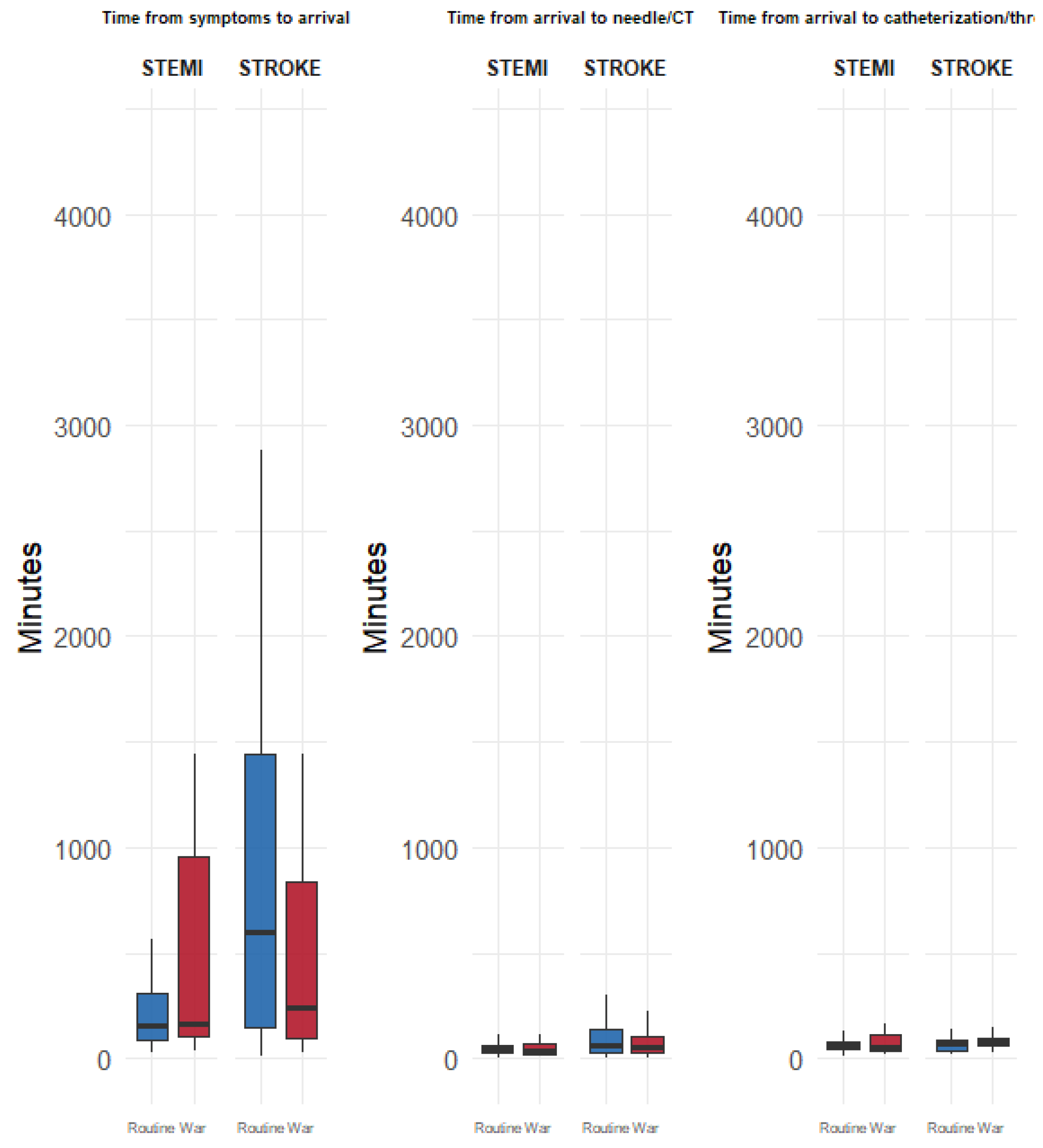
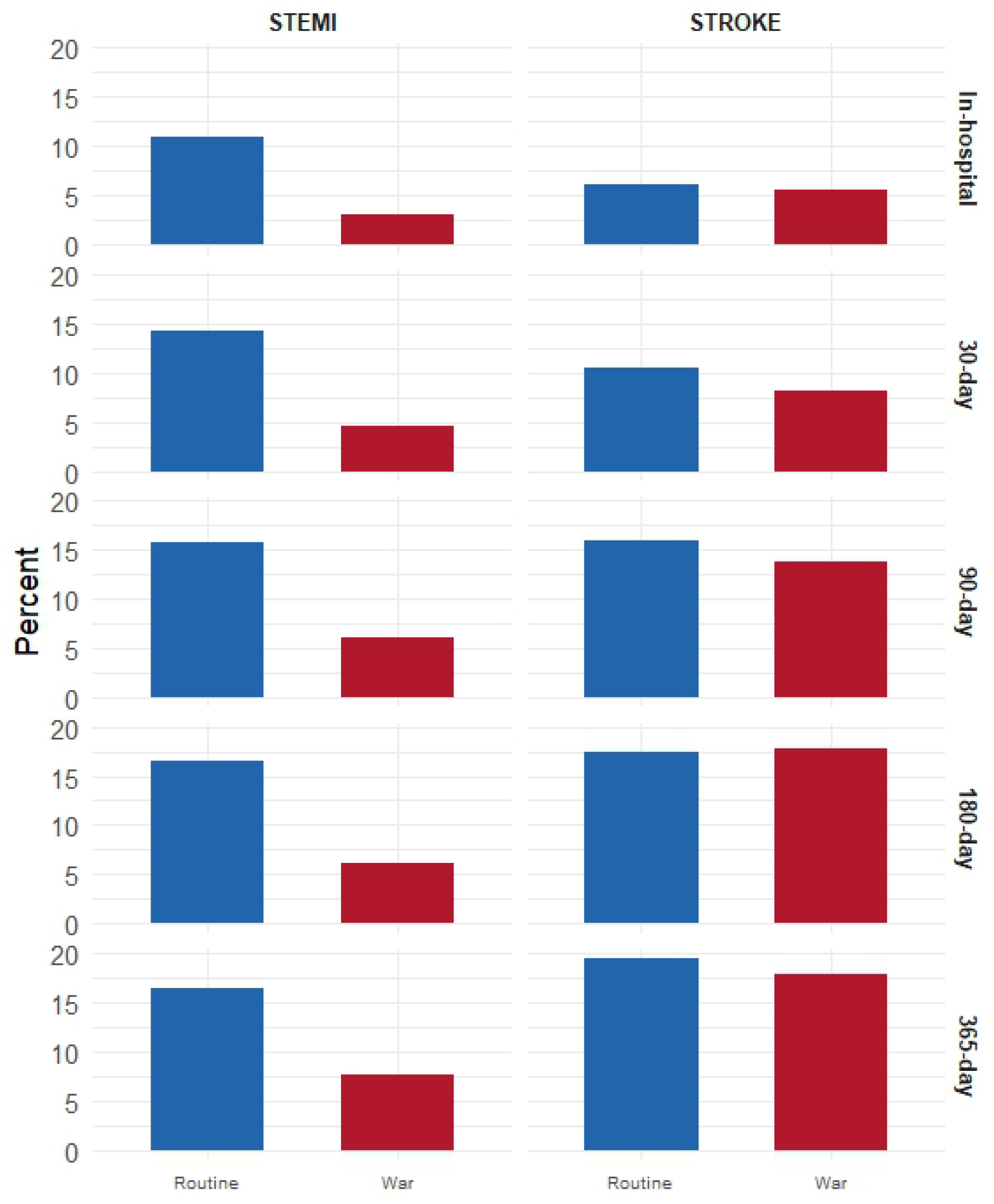
3.2. Comparison Between Routine and War Periods (Within Diagnosis)
3.3. Comparison Between Diagnoses (Stroke vs. STEMI)
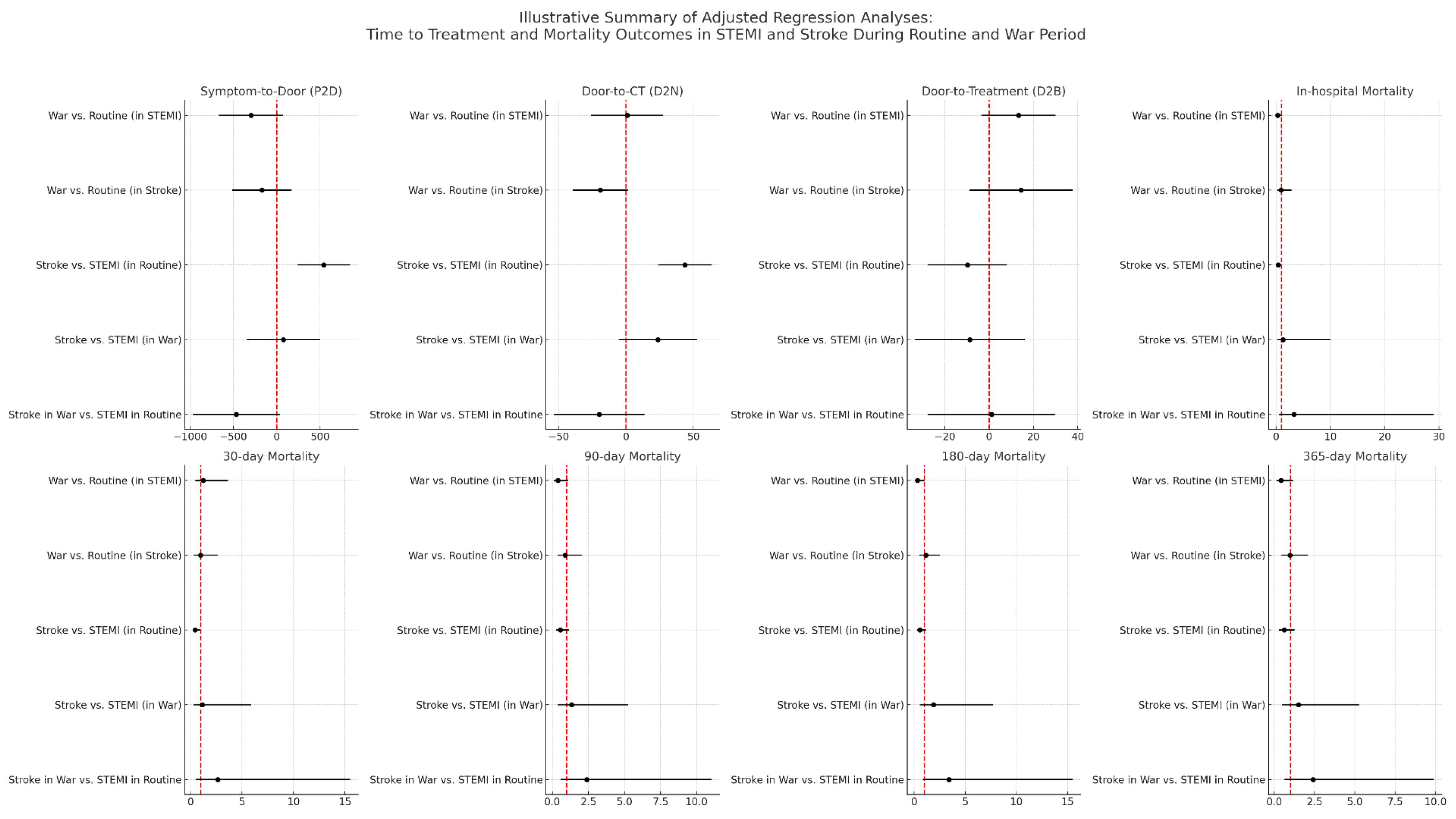
3.4. Adjusted Regression Models
4. Discussion
4.1. Overview and Interpretation of Main Findings
4.2. Physiological, Logistical, and Behavioral Differences Between Diagnoses
4.3. Biological Mechanisms and Conflict Comparison
4.4. Convergence of STEMI and Stroke Pathways During Wartime
4.5. Comparison with Prior Literature
4.6. Practical and Policy Implications
4.7. Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| Abbreviation | Full Term |
| STEMI | ST-Elevation Myocardial Infarction |
| ED | Emergency Department |
| EMS | Emergency Medical Services |
| CT | Computed Tomography |
| ICCU | Intensive Cardiac Care Unit |
| CCI | Charlson Comorbidity Index |
| P2D | Symptom-to-Door Time |
| D2N | Door-to-Needle (for STEMI)/Door-to-CT (for stroke) |
| D2B | Door-to-Balloon (for STEMI)/Door-to-Treatment |
| SUMC | Soroka University Medical Center |
| SD | Standard deviation |
| OR | Odds Ratio |
| CI | Confidence Interval |
| LOS | Length of Stay |
References
- Powers, W.J.; Rabinstein, A.A.; Ackerson, T.; Adeoye, O.M.; Bambakidis, N.C.; Becker, K.; Biller, J.; Brown, M.; Demaerschalk, B.M.; Hoh, B.; et al. 2018 Guidelines for the Early Management of Patients with Acute Ischemic Stroke: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke 2018, 49, e46–e110. [Google Scholar] [CrossRef] [PubMed]
- Zubair, A.S.; Sheth, K.N. Emergency Care of Patients with Acute Ischemic Stroke. Neurol. Clin. 2021, 39, 391–404. [Google Scholar] [CrossRef]
- Alharthi, S.; Al-Moteri, M.; Plummer, V.; Thobiaty, A.A. The impact of COVID-19 on the service of emergency department. Healthcare 2021, 9, 1295. [Google Scholar] [CrossRef]
- Zeldetz, V.; Shashar, S.; Cafri, C.; Shamia, D.; Slutsky, T.; Abu Abed, N.; Schwarzfuchs, D. STEMI in Times of Crisis: Comparative Analysis During Pandemic and War. J. Clin. Med. 2025, 14, 1720. [Google Scholar] [CrossRef]
- Garcia, S.; Albaghdadi, M.S.; Meraj, P.M.; Schmidt, C.; Garberich, R.; Jaffer, F.A.; Dixon, S.; Rade, J.J.; Tannenbaum, M.; Chambers, J.; et al. Reduction in ST-Segment Elevation Cardiac Catheterization Laboratory Activations in the United States During COVID-19 Pandemic. J. Am. Coll. Cardiol. 2020, 75, 2871–2872. [Google Scholar] [CrossRef]
- Clifford, C.R.; Le May, M.; Chow, A.; Boudreau, R.; Fu, A.Y.N.; Barry, Q.; Chong, A.Y.; So, D.Y. Delays in ST-Elevation Myocardial Infarction Care During the COVID-19 Lockdown: An Observational Study. CJC Open 2020, 3, 565. [Google Scholar] [CrossRef] [PubMed]
- Kansagra, A.P.; Goyal, M.S.; Hamilton, S.; Albers, G.W. Collateral Effect of Covid-19 on Stroke Evaluation in the United States. N. Engl. J. Med. 2020, 383, 400–401. [Google Scholar] [CrossRef] [PubMed]
- Zhao, J.; Li, H.; Kung, D.; Fisher, M.; Shen, Y.; Liu, R. Impact of the COVID-19 Epidemic on Stroke Care and Potential Solutions. Stroke 2020, 51, 1996–2001. [Google Scholar] [CrossRef]
- Barragán-Prieto, A.; Pérez-Sánchez, S.; Moniche, F.; Moyano, R.V.; Delgado, F.; Martínez-Sánchez, P.; Moya, M.; Oropesa, J.M.; Mínguez-Castellanos, A.; Villegas, I.; et al. Express improvement of acute stroke care accessibility in large regions using a centralized telestroke network. Eur. Stroke J. 2022, 7, 259–266. [Google Scholar] [CrossRef]
- Héja, M.; Fekete, I.; Márton, S.; Horváth, L.; Fekete, K. Impact of COVID-19 pandemic on acute stroke care in a tertiary stroke centre. Sci. Rep. 2024, 14, 31408. [Google Scholar] [CrossRef]
- Kontos, M.C.; Gunderson, M.R.; Zegre-Hemsey, J.K.; Lange, D.C.; French, W.J.; Henry, T.D.; McCarthy, J.J.; Corbett, C.; Jacobs, A.K.; Jollis, J.G.; et al. Prehospital Activation of Hospital Resources (PreAct) ST-Segment–Elevation Myocardial Infarction (STEMI): A Standardized Approach to Prehospital Activation and Direct to the Catheterization Laboratory for STEMI Recommendations From the American Heart Association’s Mission: Lifeline Program. J. Am. Heart Assoc. 2020, 9, e011963. [Google Scholar]
- Ganti, L. Management of acute ischemic stroke in the emergency department: Optimizing the brain. Int. J. Emerg. Med. 2025, 18, 7. [Google Scholar] [CrossRef]
- Galper, A.; Magnezi, R.; Ekka Zohar, A.; Oberman, B.; Zimlichman, E. COVID-19 lockdown impact on quality of treatment and outcomes of STEMI and stroke patients in a large tertiary medical center: An observational study. Int. J. Qual. Health Care 2022, 34, mzac074. Available online: https://pubmed.ncbi.nlm.nih.gov/36103366/ (accessed on 1 May 2025). [CrossRef]
- Bernstine, T.; Spitzer, S.; Pleban, R.; Armon-Omer, A.; Ron, A.; Kains, I.; Hamudi, J.; Shahien, R.; Edelstein, M. Impact of the COVID-19 pandemic on acute cardiology and neurology services in a secondary peripheral hospital. Sci. Rep. 2024, 14, 29291. Available online: https://www.nature.com/articles/s41598-024-80872-7 (accessed on 8 May 2025). [CrossRef]
- Buitrago-Garcia, D.; Egli-Gany, D.; Counotte, M.J.; Hossmann, S.; Imeri, H.; Ipekci, A.M.; Salanti, G.; Low, N.; Ford, N. Occurrence and transmission potential of asymptomatic and presymptomatic SARSCoV-2 infections: A living systematic review and meta-analysis. PLoS Med. 2020, 17, e1003346. Available online: https://pubmed.ncbi.nlm.nih.gov/32960881/ (accessed on 1 May 2025). [CrossRef]
- Shashar, S.; Zeldetz, V.; Henkin, Y.; Schwarzfuchs, D.; Slutsky, T.; Regev, N.F.; Plakht, Y. Assessing ethnicity as a factor in myocardial infarction emergency response and recovery: A study from the Negev Desert. J. Epidemiol. Community Health 2025, 79, 678–683. [Google Scholar] [CrossRef] [PubMed]
- Shashar, S.; Zeldetz, V.; Shalev, A.; Barret, O.; Press, Y.; Shamia, D.; Punchik, B. Ethnic disparities in STEMI outcomes among older adults: A comparative study of bedouins and jews. Int. J. Equity Health 2025, 24, 66. [Google Scholar] [CrossRef]
- Zeldetz, V.; Shashar, S.; Cafri, C.; Shamia, D.; Slutsky, T.; Regev, N.F.; Abu Abed, N.; Schwarzfuchs, D. STEMI under fire: Evaluating management and challenges in a warzone amidst the 2023 Israeli conflict. BMC Health Serv. Res. 2025, 25, 661. [Google Scholar] [CrossRef] [PubMed]
- O’Gara, P.T.; Kushner, F.G.; Ascheim, D.D.; Casey, D.E.; Chung, M.K.; de Lemos, J.A.; Ettinger, S.M.; Fang, J.C.; Fesmire, F.M.; Frankli, B.A.; et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation 2013, 127, e362–e425. [Google Scholar] [CrossRef]
- Fransen, P.S.S.; Beumer, D.; Berkhemer, O.A.; van den Berg, L.A.; Lingsma, H.; van der Lugt, A.; van Zwam, W.H.; van Oostenbrugge, R.J.; Roos, Y.B.W.E.M.; Majoie, C.B.; et al. MR CLEAN, a multicenter randomized clinical trial of endovascular treatment for acute ischemic stroke in the Netherlands: Study protocol for a randomized controlled trial. Trials 2014, 15, 343. [Google Scholar] [CrossRef] [PubMed]
- Saver, J.L.; Fonarow, G.C.; Smith, E.E.; Reeves, M.J.; Grau-Sepulveda, M.V.; Pan, W.; Olson, D.M.; Hernandez, A.F.; Peterson, E.D.; Schwamm, L.H. Time to treatment with intravenous tissue plasminogen activator and outcome from acute ischemic stroke. JAMA 2013, 309, 2480–2488. [Google Scholar] [CrossRef]
- De Rosa, S.; Spaccarotella, C.; Basso, C.; Calabrò, M.P.; Curcio, A.; Filardi, P.P.; Mancone, M.; Mercuro, G.; Muscoli, S.; Nodari, S.; et al. Reduction of hospitalizations for myocardial infarction in Italy in the COVID-19 era. Eur. Heart J. 2020, 41, 2083–2088. [Google Scholar] [CrossRef] [PubMed]
- Where Are All the Patients? Addressing COVID-19 Fear to Encourage Sick Patients to Seek Emergency Care|NEJM Catalyst. Available online: https://catalyst.nejm.org/doi/full/10.1056/CAT.20.0193 (accessed on 8 May 2025).
- Khosravani, H.; Rajendram, P.; Notario, L.; Chapman, M.G.; Menon, B.K. Protected Code Stroke: Hyperacute Stroke Management During the Coronavirus Disease 2019 (COVID-19) Pandemic. Stroke 2020, 51, 1891–1895. [Google Scholar] [CrossRef] [PubMed]
- Zasiekina, L.; Duchyminska, T.; Bifulco, A.; Bignardi, G. War trauma impacts in Ukrainian combat and civilian populations: Moral injury and associated mental health symptoms. Mil. Psychol. 2023, 36, 555. Available online: https://pmc.ncbi.nlm.nih.gov/articles/PMC11407378/ (accessed on 22 July 2025). [CrossRef]
- EMERGING FROM CRISIS Health Sector Response and Lessons Learned from the 2024 War on Lebanon. Available online: https://www.moph.gov.lb/userfiles/files/About%20MOPH/StrategicPlans/Emerging%20from%20Crisis%20Lessons%20Learned%20from%20Lebanon%E2%80%99s%20Recent%20Emergency%20Response.pdf (accessed on 22 July 2025).
- Steptoe, A.; Kivimäki, M. Stress and cardiovascular disease: An update on current knowledge. Annu. Rev. Public Health 2013, 34, 337–354. Available online: https://pubmed.ncbi.nlm.nih.gov/23297662/ (accessed on 22 July 2025). [CrossRef]
- Esler, M. Mental stress and human cardiovascular disease. Neurosci. Biobehav. Rev. 2017, 74 Pt B, 269–276. Available online: https://pubmed.ncbi.nlm.nih.gov/27751732/ (accessed on 22 July 2025). [CrossRef] [PubMed]
- Libby, P. Mechanisms of Acute Coronary Syndromes and Their Implications for Therapy. N. Engl. J. Med. 2013, 368, 2004–2013. Available online: https://pubmed.ncbi.nlm.nih.gov/23697515/ (accessed on 22 July 2025). [CrossRef]
- Hanafi, I.; Munder, E.; Ahmad, S.; Arabhamo, I.; Alziab, S.; Badin, N.; Omarain, A.; Jawish, M.K.; Saleh, M.; Nickl, V.; et al. War-related traumatic brain injuries during the Syrian armed conflict in Damascus 2014–2017: A cohort study and a literature review. BMC Emerg. Med. 2023, 23, 35. Available online: https://bmcemergmed.biomedcentral.com/articles/10.1186/s12873-023-00799-6 (accessed on 15 August 2025). [CrossRef]
- Dimitrijević, J.; Dzirlo, K.; Bratić, M.; Hrnjica, M.; Hebib, L.; Alajbegović, A.; Heco, S.; Bulić, G. Deset godina cerebrovaskularnog insulta na Neuroloskoj klinici u Sarajevu (prije, tokom i nakon rata) [10-year analysis of cerebrovascular accidents at the Neurology Clinic in Sarajevo (before, during and after the war)]. Med. Arh. 2002, 56, 151–153. (In Croatian) [Google Scholar] [PubMed]
- Dimitrijevic, J.; Gavranovic, M.; Dzirlo, K.; Bratic, M.; Hrnjica, M.; Bulic, G.; Hebib, L.J. Accidents vasculaires cérébraux à Sarajevo pendant la guerre [Cerebrovascular accidents in Sarajevo during the war]. Rev. Neurol. (Paris) 1999, 155, 359–364. (In French) [Google Scholar] [PubMed]
- Siegler, J.E.; Zha, A.M.; Czap, A.L.; Ortega-Gutierrez, S.; Farooqui, M.; Liebeskind, D.S.; Desai, S.M.; Hassan, A.E.; Starosciak, A.K.; Linfante, I.; et al. Influence of the COVID-19 Pandemic on Treatment Times for Acute Ischemic Stroke: The Society of Vascular and Interventional Neurology Multicenter Collaboration. Stroke 2021, 52, 40–47. [Google Scholar] [CrossRef]
- Van Diepen, S.; Katz, J.N.; Albert, N.M.; Henry, T.D.; Jacobs, A.K.; Kapur, N.K.; Kilic, A.; Menon, V.; Ohman, E.M.; Sweitzer, N.K.; et al. Contemporary Management of Cardiogenic Shock: A Scientific Statement from the American Heart Association. Circulation 2017, 136, e232–e268. [Google Scholar] [CrossRef]
- Ibanez, B.; James, S.; Agewall, S.; Antunes, M.J.; Bucciarelli-Ducci, C.; Bueno, H.; Caforio, A.L.P.; Crea, F.; Goudevenos, J.A.; Halvorsen, S.; et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur. Heart J. 2018, 39, 119–177. Available online: https://pubmed.ncbi.nlm.nih.gov/28886621/ (accessed on 28 April 2022).
- Broderick, J.; Brott, T.; Kothari, R.; Miller, R.; Khoury, J.; Pancioli, A.; Gebel, J.; Mills, D.; Minneci, L.; Shukla, R. The Greater Cincinnati/Northern Kentucky Stroke Study: Preliminary first-ever and total incidence rates of stroke among blacks. Stroke 1998, 29, 415–421. [Google Scholar] [CrossRef] [PubMed]
- Goyal, M.; Menon, B.K.; Van Zwam, W.H.; Dippel, D.W.J.; Mitchell, P.J.; Demchuk, A.M.; Dávalos, A.; Majoie, C.B.L.M.; Van Der Lugt, A.; De Miquel, M.A.; et al. Endovascular thrombectomy after large-vessel ischaemic stroke: A meta-analysis of individual patient data from five randomised trials. Lancet 2016, 387, 1723–1731. Available online: https://www.thelancet.com/action/showFullText?pii=S014067361600163X (accessed on 23 July 2025). [CrossRef] [PubMed]
- Wolfe, C.D.A. Incidence of stroke in Europe at the beginning of the 21st century. Stroke 2009, 40, 1557–1563. [Google Scholar] [CrossRef] [PubMed]
- Bhatt, A.S.; Moscone, A.; McElrath, E.E.; Varshney, A.S.; Claggett, B.L.; Bhatt, D.L.; Januzzi, J.L.; Butler, J.; Adler, D.S.; Solomon, S.D.; et al. Fewer Hospitalizations for Acute Cardiovascular Conditions During the COVID-19 Pandemic. J. Am. Coll. Cardiol. 2020, 76, 280–288. [Google Scholar] [CrossRef]
- “We Changed Mentally”: How 3 Years of War Have Squeezed Ukraine’s Health Workers|Euronews. Available online: https://euronewssource.com/health/we-changed-mentally-how-3-years-of-war-have-squeezed-ukraines-health-workers/ (accessed on 23 July 2025).
- Kamal, H.; Assaf, S.; Kabalan, M.; El Maissi, R.; Salhab, D.; Rahme, D.; Lahoud, N. Evaluation of stroke pre-hospital management in Lebanon from symptoms onset to hospital arrival and impact on patients’ status at discharge: A pilot study. BMC Neurol. 2022, 22, 494. Available online: https://pubmed.ncbi.nlm.nih.gov/36539720/ (accessed on 23 July 2025). [CrossRef] [PubMed]
- Francis, F.; Lesaine, E.; Domecq, S.; Cetran, L.; Coste, P.; Hadi, S.M.; Pradeau, C.; Rouanet, F.; Sevin, F.; Sibon, I.; et al. Impact of the Covid-19 pandemic on stroke and ST-segment elevation myocardial infarction patient management: French regional registry. Popul. Med. 2023, 5, A346. [Google Scholar] [CrossRef]
- Baskin, R.G.; Bartlett, R. Healthcare worker resilience during the COVID-19 pandemic: An integrative review. J. Nurs. Manag. 2021, 29, 2329. [Google Scholar] [CrossRef]
- Mehta, S.; Granger, C.B.; Henry, T.D.; Grines, C.L.; Lansky, A.; Rokos, I.; Botelho, R.; Baumbach, A.; Mishra, S.; Cheem, T.H.; et al. Reducing system delays in treatment of ST elevation myocardial infarction and confronting the challenges of late presentation in low and middle-income countries. Indian Heart J. 2017, 69 (Suppl. S1), S1–S5. [Google Scholar] [CrossRef]
- Wechsler, L.R.; Demaerschalk, B.M.; Schwamm, L.H.; Adeoye, O.M.; Audebert, H.J.; Fanale, C.V.; Hess, D.C.; Majersik, J.J.; Nystrom, K.V.; Reeves, M.J.; et al. Telemedicine quality and outcomes in stroke: A scientific statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2017, 48, e3–e25. [Google Scholar] [CrossRef]
- Hick, J.L.; Hanfling, D.; Wynia, M.K.; Pavia, A.T. Duty to Plan: Health Care, Crisis Standards of Care, and Novel Coronavirus SARS-CoV-2. NAM Perspect. 2020, 2020, 10-31478. [Google Scholar] [CrossRef] [PubMed]
- Awojobi, O.N. The impact of conflict on health outcomes: A systematic evidence from sub-saharan Africa. J. Afr. Stud. 2019, 8, 88–100. [Google Scholar]
- Rodríguez, I.G.; Sáez, M.P.; Prieto, D.C. Have Health Inequalities Increased during the COVID-19 Pandemic? Evidence from Recent Years for Older European Union Citizens. Int. J. Environ. Res. Public Health 2022, 19, 7812. [Google Scholar] [CrossRef] [PubMed]
- Joachim, M.V.; Atia Joachim, D.; Korn, L.; Shapiro, Y.; Laviv, A.; Zigdon, A. Emotional resilience and sense of danger among doctors in hospitals during periods of heightened tensions and warfare in Israel. Isr. J. Health Policy Res. 2024, 13, 68. [Google Scholar] [CrossRef]
| (a) | ||||||||||||
| Entire population | Stroke | STEMI | Stroke vs. STEMI (p-value) | |||||||||
| Overall | Overall | Routine | War | p-value | Overall | Routine | War | p-value | Routine | War | ||
| n | 410 | 217 | 144 | 73 | 193 | 127 | 66 | |||||
| Demographic characteristics and background diseases | Male gender, n (%) | 87 (40.1) | 54 (37.5) | 33 (45.2) | 0.343 | 32 (16.6) | 25 (19.7) | 7 (10.6) | 0.16 | 0.002 | <0.001 | |
| Age (mean (SD)) | 119 (29.0) | 70.97 (12.53) | 70.99 (12.78) | 70.93 (12.12) | 0.976 | 62.87 (11.90) | 63.72 (11.97) | 61.23 (11.69) | 0.169 | <0.001 | <0.001 | |
| Jew ethnicity, n (%) | 67.15 (12.88) | 38 (17.5) | 23 (16.0) | 15 (20.5) | 0.516 | 46 (23.8) | 30 (23.6) | 16 (24.2) | 1 | 0.152 | 0.75 | |
| CCI (median [range]) | 84 (20.5) | 4.00 [0.00, 7.00] | 4.00 [0.00, 7.00] | 4.00 [0.00, 6.00] | 0.427 | 2.00 [0.00, 9.00] | 2.00 [0.00, 9.00] | 2.00 [0.00, 7.00] | 0.23 | <0.001 | <0.001 | |
| CIHD, n (%) | 3.00 [0.00, 9.00] | 49 (22.6) | 34 (23.6) | 15 (20.5) | 0.735 | 43 (22.3) | 24 (18.9) | 19 (28.8) | 0.166 | 0.426 | 0.352 | |
| DM, n (%) | 92 (22.4) | 105 (48.4) | 76 (52.8) | 29 (39.7) | 0.094 | 78 (40.4) | 50 (39.4) | 28 (42.4) | 0.798 | 0.037 | 0.881 | |
| HTN, n (%) | 183 (44.6) | 156 (71.9) | 101 (70.1) | 55 (75.3) | 0.518 | 92 (47.7) | 55 (43.3) | 37 (56.1) | 0.126 | <0.001 | 0.026 | |
| Dyslipidemia, n (%) | 248 (60.5) | 121 (55.8) | 73 (50.7) | 48 (65.8) | 0.049 | 146 (75.6) | 91 (71.7) | 55 (83.3) | 0.106 | <0.001 | 0.03 | |
| Previous stroke, n (%) | 54 (24.9) | 30 (20.8) | 24 (32.9) | 0.076 | ||||||||
| (b) | ||||||||||||
| Entire population | Stroke | STEMI | Stroke vs. STEMI (p-value) | |||||||||
| Overall | Overall | Routine | War | p-value | Overall | Routine | War | p-value | Routine | War | ||
| n | 410 | 217 | 144 | 73 | 193 | 127 | 66 | |||||
| Arrival characteristics | Arrival by, n (%) | |||||||||||
| Ambulance ordered by patient | 52 (12.7) | 27 (12.4) | 19 (13.2) | 8 (11.0) | 0.825 | 25 (13.0) | 20 (15.7) | 5 (7.6) | <0.001 | 0.453 | 0.005 | |
| Referral by an emergency medical center | 220 (53.7) | 122 (56.2) | 79 (54.9) | 43 (58.9) | 98 (50.8) | 75 (59.1) | 23 (34.8) | |||||
| Self | 138 (33.7) | 68 (31.3) | 46 (31.9) | 22 (30.1) | 70 (36.3) | 32 (25.2) | 38 (57.6) | |||||
| Late arrivals, n (%) | 115 (28.0) | 83 (38.2) | 61 (42.4) | 22 (30.1) | 0.109 | 32 (16.6) | 13 (10.2) | 19 (28.8) | 0.002 | <0.001 | 1 | |
| Timelines | Time from symptoms to Arrival (median [range]) | 237.00 [12.00, 4370.00] | 440.00 [12.00, 4320.00] | 600.00 [12.00, 4320.00] | 246.00 [30.00, 4320.00] | 0.026 | 165.50 [29.00, 4370.00] | 160.00 [29.00, 4370.00] | 170.00 [40.00, 4320.00] | 0.100 | <0.001 | 0.656 |
| Time from arrival to needle/CT (median [range]) | 54.50 [5.00, 450.00] | 63.00 [5.00, 450.00] | 66.00 [5.00, 450.00] | 59.00 [5.00, 355.00] | 0.186 | 45.00 [7.00, 360.00] | 50.00 [7.00, 270.00] | 35.00 [10.00, 360.00] | 0.385 | <0.001 | 0.062 | |
| Time from arrival to cardiac catheterization/thrombolysis or cerebral catheterization (median [range]) | 67.00 [9.00, 365.00] | 72.00 [20.00, 184.00] | 69.00 [20.00, 163.00] | 84.00 [30.00, 184.00] | 0.116 | 63.00 [9.00, 365.00] | 67.50 [9.00, 280.00] | 52.00 [20.00, 365.00] | 0.457 | 0.925 | 0.099 | |
| (c) | ||||||||||||
| Entire population | Stroke | STEMI | Stroke vs. STEMI (p-value) | |||||||||
| Overall | Overall | Routine | War | p-value | Overall | Routine | War | p-value | Routine | War | ||
| n | 410 | 217 | 144 | 73 | 193 | 127 | 66 | |||||
| Outcomes | In hospital death, n (%) | 29 (7.1) | 13 (6.0) | 9 (6.2) | 4 (5.5) | 1 | 16 (8.3) | 14 (11.0) | 2 (3.0) | 0.102 | 0.449 | 0.771 |
| Death within 30 days, n (%) | 42 (10.2) | 21 (9.7) | 15 (10.4) | 6 (8.2) | 0.784 | 21 (10.9) | 18 (14.2) | 3 (4.5) | 0.073 | 1 | 0.593 | |
| Death within 90 days, n (%) | 57 (13.9) | 33 (15.2) | 23 (16.0) | 10 (13.7) | 0.81 | 24 (12.4) | 20 (15.7) | 4 (6.1) | 0.088 | 0.985 | 0.226 | |
| Death within 180 days, n (%) | 63 (15.4) | 38 (17.5) | 25 (17.4) | 13 (17.8) | 1 | 25 (13.0) | 21 (16.5) | 4 (6.1) | 0.067 | 0.644 | 0.064 | |
| Death within 365 days, n (%) | 67 (16.3) | 41 (18.9) | 28 (19.4) | 13 (17.8) | 0.914 | 26 (13.5) | 21 (16.5) | 5 (7.6) | 0.132 | 0.449 | 0.123 | |
| LOS (median [range]) | 4.00 [0.00, 40.00] | 5.00 [0.00, 40.00] | 6.00 [0.00, 40.00] | 5.00 [0.00, 24.00] | 0.241 | 4.00 [1.00, 15.00] | 4.00 [1.00, 15.00] | 4.00 [1.00, 9.00] | 0.834 | <0.001 | 0.005 | |
| P2D (Symptom to Door) | D2N (Door to CT) | D2B (Door to Treatment) | In-Hospital Death | 30-Day Mortality | 90-Day Mortality | 180-Day Mortality | 365-Day Mortality | |
|---|---|---|---|---|---|---|---|---|
| War vs. Routine (in STEMI) | −295.42 (−665.34, 74.50); p = 0.117 | 0.88 (−25.81, 27.57); p = 0.94 | 13.24 (−3.55, 30.03); p = 0.12 | 0.27 (0.04, 1.04); p = 0.10 | 1.23 (0.47, 3.65; p = 0.68 | 0.38 (0.10, 1.12); p = 0.10 | 0.33 (0.09, 0.99); p = 0.07 | 0.41 (0.12, 1.16); p = 0.11 |
| War vs. Routine (in Stroke) | −171.38 (−513.17, 170.42); p = 0.325 | −19.05 (−39.42, 1.31); p = 0.07 | 14.33 (−9.01, 37.67); p = 0.23 | 0.88 (0.23, 2.86); p = 0.85 | 0.96 (0.32, 2.63); p = 0.94 | 0.89 (0.37, 2.04); p = 0.79 | 1.15 (0.51, 2.50); p = 0.74 | 0.98 (0.44, 2.08); p = 0.97 |
| Stroke vs. STEMI (in Routine) | 543.07 (239.68, 846.47); p < 0.001 | 43.62 (23.94, 63.30); p < 0.001 | −9.79 (−27.55, 7.98); p = 0.28 | 0.39 (0.15, 0.97); p = 0.05 | 0.43 (0.19, 0.94); p = 0.04 | 0.55 (0.26, 1.14); p = 0.11 | 0.56 (0.27, 1.14); p = 0.11 | 0.62 (0.30, 1.26); p = 0.18 |
| Stroke vs. STEMI (in War) | 76.28 (−349.84 502.40); p = 0.725 | 23.69 (−5.14, 52.52); p = 0.11 | −8.69 (−33.46, 16.08); p = 0.49 | 1.27 (0.22, 10.00); p = 0.80 | 1.14 (0.27, 5.88); p = 0.87 | 1.32 (0.38, 5.26); p = 0.68 | 1.89 (0.57, 7.69); p = 0.32 | 1.49 (0.47, 5.26); p = 0.52 |
| Stroke in War vs. STEMI in Routine | −466.79 (−971.25, 37.67); p = 0.07 | −19.93 (−53.56, 13.71); p = 0.24 | 1.09 (−27.65, 29.83); p = 0.94 | 3.27 (0.48, 29.07); p = 0.24 | 2.64 (0.53, 15.49); p = 0.25 | 2.37 (0.58, 11.02); p = 0.24 | 3.40 (0.87, 15.48); p = 0.09 | 2.40 (0.64, 9.90); p = 0.21 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zeldetz, V.; Shashar, S.; Cafri, C.; Shamia, D.; Slutsky, T.; Peretz, T.; Regev, N.F.; Abu Abed, N.; Schwarzfuchs, D. Heart vs. Brain in a Warzone: The Effects of War on Acute Cardiovascular and Neurological Emergencies. Diagnostics 2025, 15, 2081. https://doi.org/10.3390/diagnostics15162081
Zeldetz V, Shashar S, Cafri C, Shamia D, Slutsky T, Peretz T, Regev NF, Abu Abed N, Schwarzfuchs D. Heart vs. Brain in a Warzone: The Effects of War on Acute Cardiovascular and Neurological Emergencies. Diagnostics. 2025; 15(16):2081. https://doi.org/10.3390/diagnostics15162081
Chicago/Turabian StyleZeldetz, Vladimir, Sagi Shashar, Carlos Cafri, David Shamia, Tzachi Slutsky, Tal Peretz, Noa Fried Regev, Naif Abu Abed, and Dan Schwarzfuchs. 2025. "Heart vs. Brain in a Warzone: The Effects of War on Acute Cardiovascular and Neurological Emergencies" Diagnostics 15, no. 16: 2081. https://doi.org/10.3390/diagnostics15162081
APA StyleZeldetz, V., Shashar, S., Cafri, C., Shamia, D., Slutsky, T., Peretz, T., Regev, N. F., Abu Abed, N., & Schwarzfuchs, D. (2025). Heart vs. Brain in a Warzone: The Effects of War on Acute Cardiovascular and Neurological Emergencies. Diagnostics, 15(16), 2081. https://doi.org/10.3390/diagnostics15162081






