Reconstructing the Gait Pattern of a Korean Cadaver with Bilateral Lower Limb Asymmetry Using a Virtual Humanoid Modeling Program
Abstract
1. Introduction
2. Materials and Methods
2.1. Cadaveric Specimen
2.2. Osteometrical Analysis
2.3. Meta Motivo Analysis
| Bones | Parameters | Reference |
|---|---|---|
| Femur | Maximum length | Martin and Knussmann, 1988 [12] |
| Head diameter | Moore-Jansen et al., 1994 [13] | |
| Midshaft transverse diameter | Moore-Jansen et al., 1994 [13] | |
| Midshaft sagittal diameter | Moore-Jansen et al., 1994 [13] | |
| Epicondylar breadth | Martin and Knussmann, 1988 [12] | |
| Patella | Maximum length | Byrd and Adams, 2003 [14] |
| Breadth | Byrd and Adams, 2003 [14] | |
| Thickness | Byrd and Adams, 2003 [14] | |
| Tibia | Maximum length | Martin and Knussmann, 1988 [12] |
| Proximal epiphyseal breadth | Martin and Knussmann, 1988 [12] | |
| Distal epiphyseal breadth | Martin and Knussmann, 1988 [12] | |
| Nutrient foramen transverse diameter | Moore-Jansen et al., 1994 [13] | |
| Fibula | Maximum length | Martin and Knussmann, 1988 [12] |
| Midshaft diameter | Martin and Knussmann, 1988 [12] |
3. Results
3.1. Osteometric Results
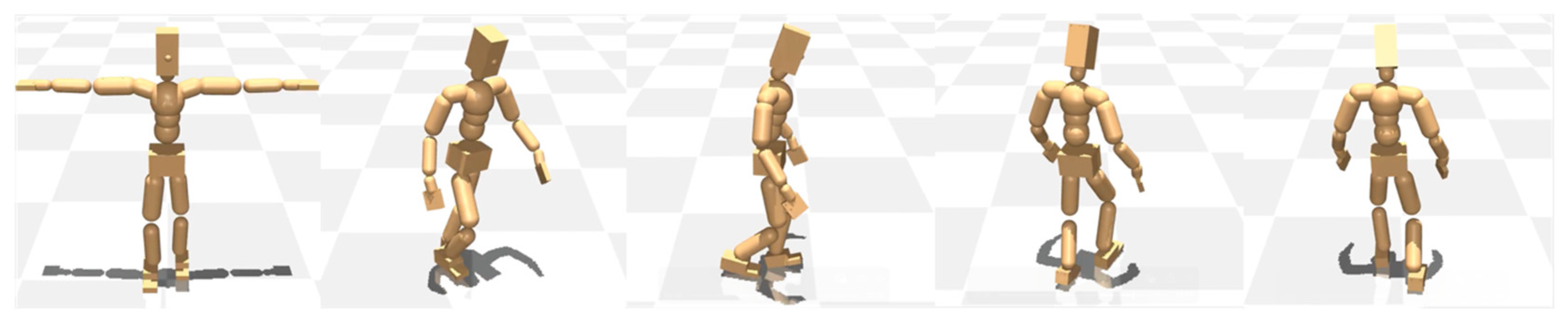
3.2. Gait Analysis
3.2.1. Normal
3.2.2. Unbalanced: Non-Learned
3.2.3. Unbalanced: Learned
4. Discussion
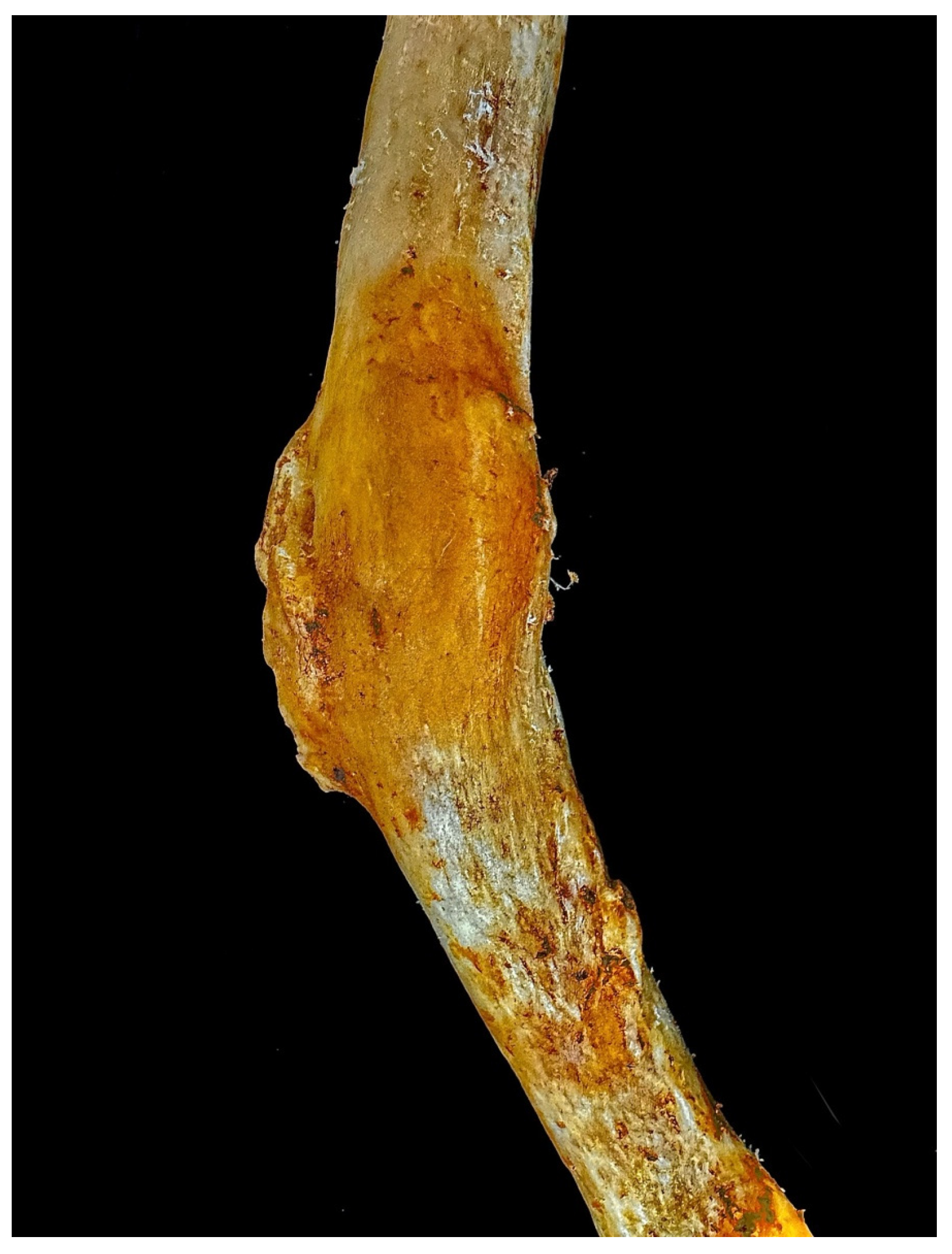
4.1. Cause of the Femoral Curvature and Its Timing
4.2. Gait Patterns
4.3. Limitations
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Dikovski, B.; Madjarov, G.; Gjorgjevikj, D. Evaluation of Different Feature Sets for Gait Recognition Using Skeletal Data from Kinect. In Proceedings of the 2014 37th International Convention on Information and Communication Technology, Electronics and Microelectronics (MIPRO), Opatija, Croatia, 26–30 May 2014; IEEE: Los Alamitos, CA USA, 2014; pp. 1304–1308. [Google Scholar] [CrossRef]
- Hulleck, A.A.; Menoth Mohan, D.; Abdallah, N.; El Rich, M.; Khalaf, K. Present and Future of Gait Assessment in Clinical Practice: Towards the Application of Novel Trends and Technologies. Front. Med. Technol. 2022, 4, 901331. [Google Scholar] [CrossRef]
- Yun, S.-S.; Kim, J.-W. Gait Analysis Based on 3D Reconstruction Using Human Skeleton Detection and Humanoid Model with a Monocular Camera. J. Korean Inst. Intell. Syst. 2025, 35, 43–49. [Google Scholar] [CrossRef]
- Prathap, C.; Sakkara, S. Gait Recognition Using Skeleton Data. In Proceedings of the 2015 International Conference on Advances in Computing, Communications and Informatics (ICACCI), Kochi, India, 10–13 August 2015; IEEE: Los Alamitos, CA USA, 2015; pp. 2302–2306. [Google Scholar] [CrossRef]
- Li, N.; Zhao, X. A Strong and Robust Skeleton-Based Gait Recognition Method with Gait Periodicity Priors. IEEE Trans. Multimed. 2023, 25, 3046–3058. [Google Scholar] [CrossRef]
- Trinler, U.; Schwameder, H.; Baker, R.; Alexander, N. Muscle Force Estimation in Clinical Gait Analysis Using AnyBody and OpenSim. J. Biomech. 2019, 86, 55–63. [Google Scholar] [CrossRef] [PubMed]
- Alexander, N.; Schwameder, H.; Baker, R.; Trinler, U. Effect of Different Walking Speeds on Joint and Muscle Force Estimation Using AnyBody and OpenSim. Gait Posture 2021, 90, 197–203. [Google Scholar] [CrossRef] [PubMed]
- Alharthi, A.S.; Yunas, S.U.; Ozanyan, K.B. Deep Learning for Monitoring of Human Gait: A Review. IEEE Sens. J. 2019, 19, 9575–9591. [Google Scholar] [CrossRef]
- Jun, K.; Lee, K.; Lee, S.; Lee, H.; Kim, M.S. Hybrid Deep Neural Network Framework Combining Skeleton and Gait Features for Pathological Gait Recognition. Bioengineering 2023, 10, 1133. [Google Scholar] [CrossRef]
- Park, H.J.; HU, K.-S.; Jin, W.E. The Effect of Maceration Techniques for Surface and Outline Analysis Using Human Bones. Anat. Biol. Anthropol. 2024, 37, 253–259. [Google Scholar] [CrossRef]
- Tirinzoni, A.; Touati, A.; Farebrother, J.; Guzek, M.; Kanervisto, A.; Xu, Y.; Lazaric, A.; Pirotta, M. Zero-Shot Whole-Body Humanoid Control via Behavioral Foundation Models. arXiv 2025. [Google Scholar] [CrossRef]
- Martin, R.; Knussmann, R. Anthropologie. Handbuch der vergleichenden Biologie des Menschen; Gustav Fischer: Nueva York, Stuttgart, 1988. [Google Scholar]
- Moore-Jansen, P.H.; Ousley, S.D.; Jantz, R.L. Data Collection Procedures for Forensic Skeletal Materials; University of Tennesse: Knoxville, TN, USA, 1994. [Google Scholar]
- Byrd, J.; Adams, B. Osteometric Sorting of Commingled Human Remains. J. Forensic Sci. 2003, 48, 1–8. [Google Scholar] [CrossRef]
- Jung, I.J.; Kim, J.W. Differences in Femur Geometry and Bone Markers in Atypical Femur Fractures and the General Population. Sci. Rep. 2021, 11, 24149. [Google Scholar] [CrossRef] [PubMed]
- Nepal, S.; Jarusriwanna, A.; Unnanuntana, A. Stress Fracture of the Femoral Shaft in Paget’s Disease of Bone: A Case Report. J. Bone Metab. 2021, 28, 171–178. [Google Scholar] [CrossRef] [PubMed]
- Khan, A.R.; Rehan, F.; Nasrumminallah, M.; Kumar, H. Bilateral Femoral Shaft Fractures in Osteomalacia: A Case Report and Literature Review. Int. J. Surg. Case Rep. 2024, 123, 110302. [Google Scholar] [CrossRef]
- Gupta, A.; Saurabh, S.; Trikha, T.; Karpe, A.; Mittal, S. Femoral Shaft Fracture in Post-Polio Syndrome Patients: Case Series from a Level-I Trauma Center and Review of Literature. Indian J. Orthop. 2022, 56, 1339–1346. [Google Scholar] [CrossRef]
- Frick, S.L. Skeletal Growth, Development, and Healing as Related to Pediatric Trauma. In Green’s Skeletal Trauma in Children; Elsevier: Amsterdam, The Netherlands, 2015; pp. 1–15. [Google Scholar] [CrossRef]
- Riseborough, E.J.; Barrett, I.R.; Shapiro, F. Growth Disturbances Following Distal Femoral Physeal Fracture-Separations. J. Bone Jt. Surg. Am. 1983, 65, 885–893. [Google Scholar] [CrossRef]
- Johnson, E.E. Acute Lengthening of Shortened Lower Extremities after Malunion or Non-Union of a Fracture. J. Bone Jt. Surg. 1994, 76, 379–389. [Google Scholar] [CrossRef] [PubMed]
- Ghaly, H.M.; El-Rosasy, M.A.-M.; Marei, A.E.; El-Gebaly, O.A. Simultaneous Femoral and Tibial Lengthening for Severe Limb Length Discrepancy in Fibular Hemimelia. J. Orthop. Surg. 2023, 18, 844. [Google Scholar] [CrossRef]
- Licata, M.; Iorio, S.; Benaglia, P.; Tosi, A.; Borgo, M.; Armocida, G.; Ronga, M.; Ruspi, A.; Verzeletti, A.; Rossetti, C. Biomechanical Analysis of a Femur Fracture in Osteoarchaeology: Reconstruction of Pathomechanics, Treatment and Gait. J. Forensic Leg. Med. 2019, 61, 115–121. [Google Scholar] [CrossRef]
- Walsh, M.; Connolly, P.; Jenkinson, A.; O’Brien, T. Leg Length Discrepancy—An Experimental Study of Compensatory Changes in Three Dimensions Using Gait Analysis. Gait Posture 2000, 12, 156–161. [Google Scholar] [CrossRef]
- Khamis, S.; Carmeli, E. Relationship and Significance of Gait Deviations Associated with Limb Length Discrepancy: A Systematic Review. Gait Posture 2017, 57, 115–123. [Google Scholar] [CrossRef]
- Knutson, G.A. Anatomic and Functional Leg-Length Inequality: A Review and Recommendation for Clinical Decision-Making. Part I, Anatomic Leg-Length Inequality: Prevalence, Magnitude, Effects and Clinical Significance. Chiropr. Man. Ther. 2005, 13, 11. [Google Scholar] [CrossRef] [PubMed]
- Aiona, M.; Do, K.P.; Emara, K.; Dorociak, R.; Pierce, R. Gait Patterns in Children With Limb Length Discrepancy. J. Pediatr. Orthop. 2015, 35, 280–284. [Google Scholar] [CrossRef] [PubMed]
- Gurney, B.; Mermier, C.; Robergs, R.; Gibson, A.; Rivero, D. Effects of Limb-Length Discrepancy on Gait Economy and Lower-Extremity Muscle Activity in Older Adults. J. Bone Jt. Surg. 2001, 83, 907–915. [Google Scholar] [CrossRef]
- Misu, S.; Asai, T.; Murata, S.; Nakamura, R.; Isa, T.; Tsuboi, Y.; Oshima, K.; Koyama, S.; Sawa, R.; Fukumoto, Y.; et al. Association between Abnormal Gait Patterns and an Elevated Degree of Pain after Daily Walking: A Preliminary Study. Int. J. Environ. Res. Public Health 2022, 19, 2842. [Google Scholar] [CrossRef] [PubMed]


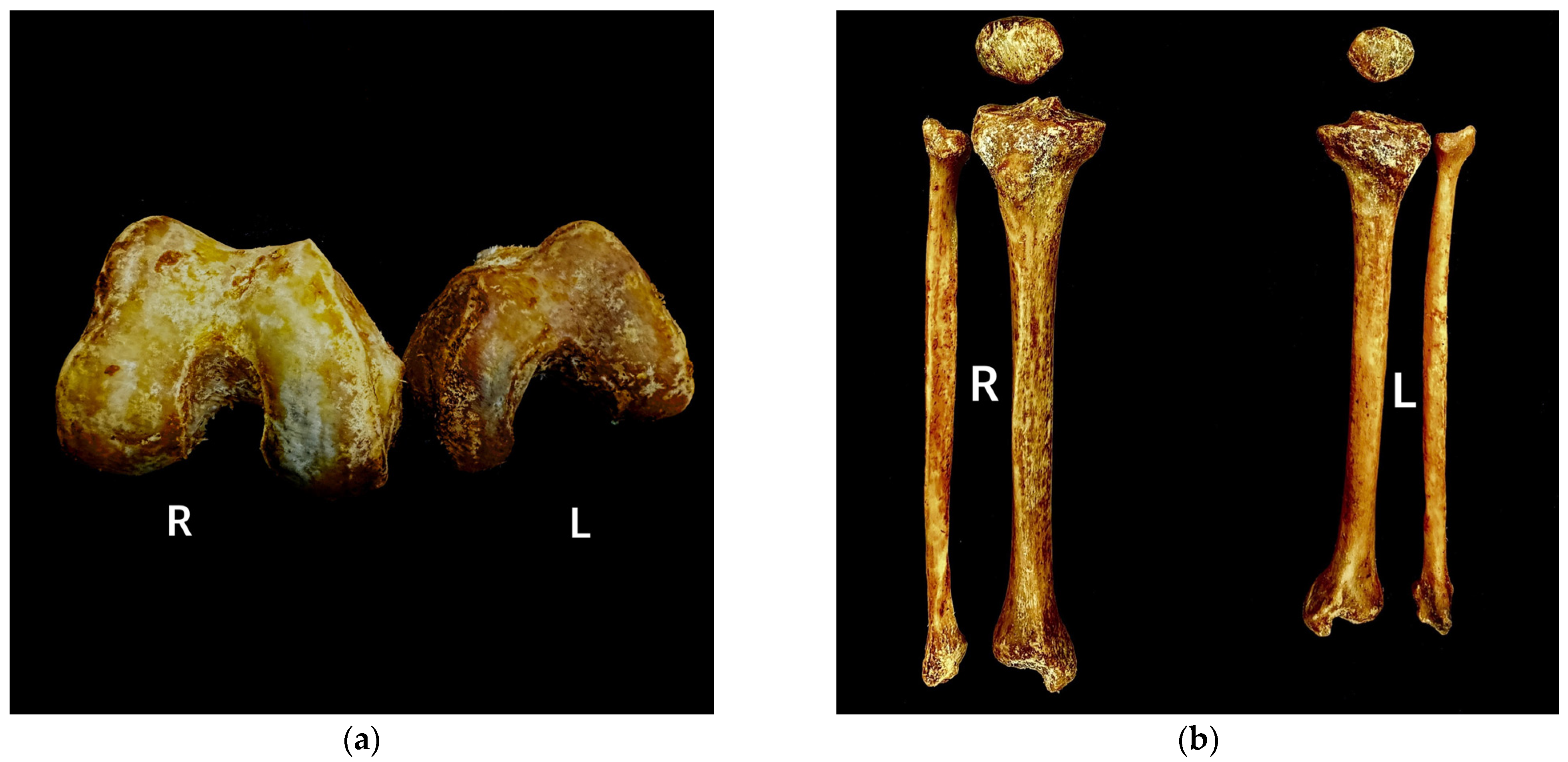

| Bones | Parameters | Results (mm) | |
|---|---|---|---|
| Right | Left | ||
| Femur | Maximum length | 400 | 394 |
| Head diameter | 47 | 43 | |
| Midshaft transverse diameter | 27 | 24 | |
| Midshaft sagittal diameter | 24 | 17 | |
| Epicondylar breadth | 83 | 69 | |
| Patella | Maximum length | 41 | 33 |
| Breadth | 54 | 41 | |
| Thickness | 19 | 16 | |
| Tibia | Maximum length | 331 | 298 |
| Proximal epiphyseal breadth | 75 | 63 | |
| Distal epiphyseal breadth | 48 | 45 | |
| Nutrient foramen transverse diameter | 29 | 21 | |
| Fibula | Maximum length | 332 | 296 |
| Midshaft diameter | 16 | 13 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Seo, M.W.; Lee, C.; Park, H.J. Reconstructing the Gait Pattern of a Korean Cadaver with Bilateral Lower Limb Asymmetry Using a Virtual Humanoid Modeling Program. Diagnostics 2025, 15, 1943. https://doi.org/10.3390/diagnostics15151943
Seo MW, Lee C, Park HJ. Reconstructing the Gait Pattern of a Korean Cadaver with Bilateral Lower Limb Asymmetry Using a Virtual Humanoid Modeling Program. Diagnostics. 2025; 15(15):1943. https://doi.org/10.3390/diagnostics15151943
Chicago/Turabian StyleSeo, Min Woo, Changmin Lee, and Hyun Jin Park. 2025. "Reconstructing the Gait Pattern of a Korean Cadaver with Bilateral Lower Limb Asymmetry Using a Virtual Humanoid Modeling Program" Diagnostics 15, no. 15: 1943. https://doi.org/10.3390/diagnostics15151943
APA StyleSeo, M. W., Lee, C., & Park, H. J. (2025). Reconstructing the Gait Pattern of a Korean Cadaver with Bilateral Lower Limb Asymmetry Using a Virtual Humanoid Modeling Program. Diagnostics, 15(15), 1943. https://doi.org/10.3390/diagnostics15151943






