Implant Migration and Clinical Outcomes in Pediatric Symptomatic Flexible Flatfoot Treated with Subtalar Arthroereisis: A Cohort Study with Long-Term Follow-Up Results
Abstract
1. Introduction
2. Materials and Methods
2.1. Criteria and Patient Selection
2.2. Surgical Technique and Postoperative Management
2.3. Clinical and Radiological Evaluation
2.4. Statistical Analysis
3. Results
3.1. Patient Demographics and Clinical Characteristics
3.2. Radiological Outcomes
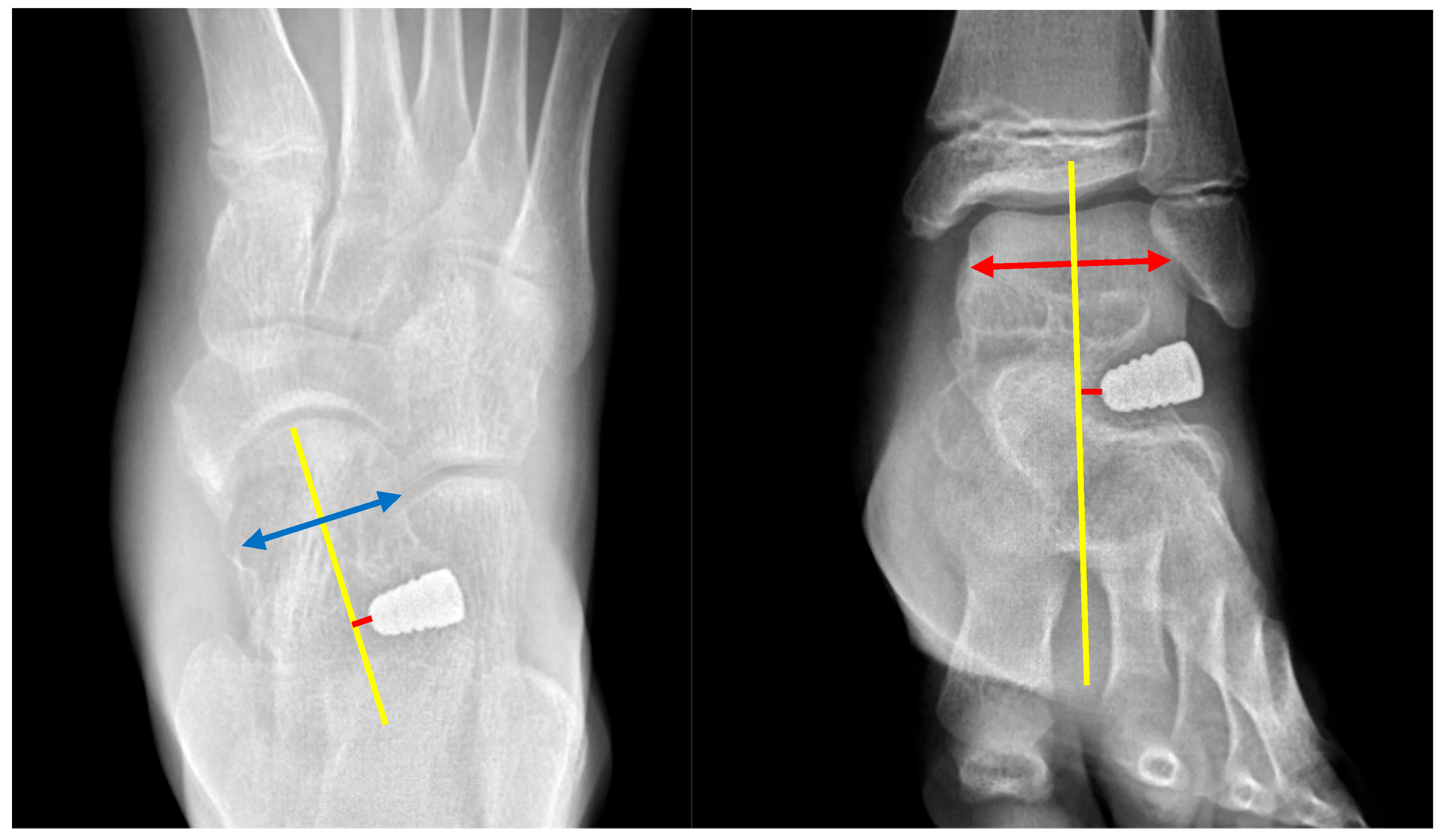
3.3. Implant Position and Migration
3.4. Complications
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| STA | Subtalar arthroereisis |
| AP | Anteroposterior |
| SD | Standard deviation |
| IQR | Interquartile range |
References
- Uden, H.; Scharfbillig, R.; Causby, R. The Typically Developing Paediatric Foot: How Flat Should It Be? A Systematic Review. J. Foot Ankle Res. 2017, 10, 37. [Google Scholar] [CrossRef] [PubMed]
- Banwell, H.A.; Paris, M.E.; Mackintosh, S.; Williams, C.M. Paediatric Flexible Flat Foot: How Are We Measuring It and Are We Getting It Right? A Systematic Review. J. Foot Ankle Res. 2018, 11, 21. [Google Scholar] [CrossRef]
- Highlander, P.; Sung, W.; Weil, L., Jr. Subtalar Arthroereisis. Clin. Podiatr. Med. Surg. 2011, 28, 745–754. [Google Scholar] [CrossRef]
- Mosca, V.S. Flexible Flatfoot in Children and Adolescents. J. Child. Orthop. 2010, 4, 107–121. [Google Scholar] [CrossRef]
- Turner, C.; Gardiner, M.D.; Midgley, A.; Stefanis, A. A Guide to the Management of Paediatric Pes Planus. Aust. J. Gen. Pract. 2020, 49, 245–249. [Google Scholar] [CrossRef] [PubMed]
- Carr, J.B.; Yang, S.; Lather, L.A. Pediatric Pes Planus: A State-of-the-Art Review. Pediatrics 2016, 137, e20151230. [Google Scholar] [CrossRef]
- Halabchi, F.; Mazaheri, R.; Mirshahi, M.; Abbasian, L. Pediatric Flexible Flatfoot: Clinical Aspects and Algorithmic Approach. Iran J. Pediatr. 2013, 23, 247–260. [Google Scholar] [PubMed] [PubMed Central]
- Nemeth, B. The Diagnosis and Management of Common Childhood Orthopedic Disorders. Curr. Probl. Pediatr. Adolesc. Health Care 2011, 41, 2–28. [Google Scholar] [CrossRef] [PubMed]
- Sadeghi-Demneh, E.; Azadinia, F.; Jafarian, F.; Shamsi, F.; Melvin, J.M.; Jafarpishe, M.; Rezaeian, Z. Flatfoot and Obesity in School-Age Children: A Cross-Sectional Study. Clin. Obes. 2016, 6, 42–50. [Google Scholar] [CrossRef]
- Kothari, A.; Dixon, P.C.; Stebbins, J.; Zavatsky, A.B.; Theologis, T. The Relationship between Quality of Life and Foot Function in Children with Flexible Flatfeet. Gait Posture 2015, 41, 786–790. [Google Scholar] [CrossRef]
- Lin, C.J.; Lai, K.A.; Kuan, T.S.; Chou, Y.L. Correlating Factors and Clinical Significance of Flexible Flatfoot in Preschool Children. J. Pediatr. Orthop. 2001, 21, 378–382. [Google Scholar] [CrossRef] [PubMed]
- Nelson, S.C.; Haycock, D.M.; Little, E.R. Flexible Flatfoot Treatment with Arthroereisis: Radiographic Improvement and Child Health Survey Analysis. J. Foot Ankle Surg. 2004, 43, 144–155. [Google Scholar] [CrossRef]
- Toullec, E. Adult Flatfoot. Orthop. Traumatol. Surg. Res. 2015, 101, S11–S17. [Google Scholar] [CrossRef]
- Duan, X.J.; Fan, H.Q.; Wang, F.Y.; He, P.; Yang, L. Application of 3D-Printed Customized Guides in Subtalar Joint Arthrodesis. Orthop. Surg. 2019, 11, 405–413. [Google Scholar] [CrossRef] [PubMed]
- Fernández de Retana, P.; Alvarez, F.; Bacca, G. Is there a Role for Subtalar Arthroereisis in the Management of Adult Acquired Flatfoot? Foot Ankle Clin. 2012, 17, 271–281. [Google Scholar] [CrossRef] [PubMed]
- Bouchard, M.; Mosca, V.S. Flatfoot Deformity in Children and Adolescents: Surgical Indications and Management. J. Am. Acad. Orthop. Surg. 2014, 22, 623–632. [Google Scholar] [CrossRef]
- Metcalfe, S.A.; Bowling, F.L.; Reeves, N.D. Subtalar Joint Arthroereisis in the Management of Pediatric Flexible Flatfoot: A Critical Review of the Literature. Foot Ankle Int. 2011, 32, 1127–1139. [Google Scholar] [CrossRef]
- Chen, W.M.; Lee, S.J.; Lee, P.V.S. Plantar Pressure Relief under the Metatarsal Heads: Therapeutic Insole Design Using Three-Dimensional Finite Element Model of the Foot. J. Biomech. 2015, 48, 659–665. [Google Scholar] [CrossRef]
- Wang, J.H.; Chu, C.H.; Chuang, H.C.; Chen, Y.Y. Long-Term Results of Subtalar Arthroereisis for Symptomatic Flexible Flatfoot in Paediatrics. Int. Orthop. 2025, 49, 1175–1183. [Google Scholar] [CrossRef]
- Alkhatatba, M.; Bani Essa, S.; Khatatbeh, M.; Radaideh, A.; Audat, H.Z.; Bani Younes, A.; Alrawashdeh, M.; Abualadas, J.; Obeidat, N.; Al-Omari, J.; et al. Subtalar Arthroereisis for Symptomatic Flexible Flatfoot in Adolescents: A Prospective Study of 26 Feet. Mater. Sociomed. 2024, 36, 131–136. [Google Scholar] [CrossRef]
- Suh, D.H.; Park, J.H.; Lee, S.H.; Kim, H.J.; Park, Y.H.; Jang, W.Y.; Baek, J.H.; Sung, H.J.; Choi, G.W. Lateral Column Lengthening versus Subtalar Arthroereisis for Paediatric Flatfeet: A Systematic Review. Int. Orthop. 2019, 43, 1179–1192. [Google Scholar] [CrossRef] [PubMed]
- Black, P.R.; Betts, R.P.; Duckworth, T.; Smith, T.W. The Viladot Implant in Flatfooted Children. Foot Ankle Int. 2000, 21, 478–481. [Google Scholar] [CrossRef]
- Smith, R.D.; Rappaport, M.J. Subtalar Arthroereisis. A Four-Year Follow-Up Study. J. Am. Podiatr. Assoc. 1983, 73, 356–361. [Google Scholar] [CrossRef] [PubMed]
- Pinney, S.J.; Sangeorzan, B.J.; Hansen, S.T. Surgical Anatomy of the Gastrocnemius Recession (Strayer Procedure). Foot Ankle Int. 2004, 25, 247–250. [Google Scholar] [CrossRef]
- Strayer, L.M. Recession of the Gastrocnemius: An Operation to Relieve Spastic Contracture of the Calf Muscles. J. Bone Jt. Surg. 1950, 32, 671–676. [Google Scholar] [CrossRef]
- Leonard, M.H.; Gonzalez, S.; Breck, L.W.; Basom, C.; Palafox, M.; Kosicki, Z.W. Lateral Transfer of the Posterior Tibial Tendon in Certain Selected Cases of Pes Plano Valgus (Kidner Operation). Clin. Orthop. Relat. Res. 1965, 40, 139–144. [Google Scholar] [CrossRef]
- Prichasuk, S.; Sinphurmsukskul, O. Kidner Procedure for Symptomatic Accessory Navicular and Its Relation to Pes Planus. Foot Ankle Int. 1995, 16, 500–503. [Google Scholar] [CrossRef] [PubMed]
- Mazzotti, A.; Viglione, V.; Gerardi, S.; Artioli, E.; Rocca, G.; Faldini, C. Subtalar Arthroereisis Post-operative Management in Children: A Literature Review. Foot 2023, 56, 102037. [Google Scholar] [CrossRef]
- Lamm, B.M.; Stasko, P.A.; Gesheff, M.G.; Bhave, A. Normal Foot and Ankle Radiographic Angles, Measurements, and Reference Points. J. Foot Ankle Surg. 2016, 55, 991–998. [Google Scholar] [CrossRef]
- Smolle, M.A.; Svehlik, M.; Regvar, K.; Leithner, A.; Kraus, T. Long-Term Clinical and Radiological Outcomes Following Surgical Treatment for Symptomatic Pediatric Flexible Flat Feet: A Systematic Review. Acta Orthop. 2022, 93, 367–374. [Google Scholar] [CrossRef]
- Bernasconi, A.; Lintz, F.; Sadile, F. The Role of Arthroereisis of the Subtalar Joint for Flatfoot in Children and Adults. EFORT Open Rev. 2017, 2, 438–446. [Google Scholar] [CrossRef] [PubMed]
- Rome, K.; Ashford, R.L.; Evans, A. Non-Surgical Interventions for Paediatric Pes Planus. Cochrane Database Syst. Rev. 2010, 1, CD006311. [Google Scholar] [CrossRef] [PubMed]
- Vogt, B.; Toporowski, G.; Gosheger, G.; Rölfing, J.D.; Rosenbaum, D.; Schiedel, F.; Laufer, A.; Kleine-Koenig, M.T.; Theil, C.; Roedl, R.; et al. Subtalar Arthroereisis for Flexible Flatfoot in Children—Clinical, Radiographic and Pedobarographic Outcome Comparing Three Different Methods. Children 2021, 8, 359. [Google Scholar] [CrossRef] [PubMed]
- Mazzotti, A.; Di Martino, A.; Geraci, G.; Casadei, C.; Panciera, A.; Giannini, S.; Faldini, C. Long-Term Results of Subtalar Arthroereisis for the Treatment of Symptomatic Flexible Flatfoot in Children: An Average Fifteen Year Follow-Up Study. Int. Orthop. 2021, 45, 657–664. [Google Scholar] [CrossRef]
- Smith, C.; Zaidi, R.; Bhamra, J.; Bridgens, A.; Wek, C.; Kokkinakis, M. Subtalar Arthroereisis for the Treatment of the Symptomatic Paediatric Flexible Pes Planus: A Systematic Review. EFORT Open Rev. 2021, 6, 118–129. [Google Scholar] [CrossRef]
- Berkowitz, M.J.; Clare, M.P.; Walling, A.K.; Sanders, R. Salvage of Failed Total Ankle Arthroplasty with Fusion Using Structural Allograft and Internal Fixation. Foot Ankle Int. 2011, 32, S493–S502. [Google Scholar] [CrossRef]
- Needleman, R.L. A Surgical Approach for Flexible Flatfeet in Adults Including a Subtalar Arthroereisis with the MBA Sinus Tarsi Implant. Foot Ankle Int. 2006, 27, 9–18. [Google Scholar] [CrossRef]
- Graham, M.E.; Jawrani, N.T.; Chikka, A. Extraosseous Talotarsal Stabilization Using HyProCure® in Adults: A 5-Year Retrospective Follow-Up. J. Foot Ankle Surg. 2012, 51, 23–29. [Google Scholar] [CrossRef]
- Tan, J.H.I.; Tan, S.H.S.; Lim, A.K.S.; Hui, J.H. The Outcomes of Subtalar Arthroereisis in Pes Planus: A Systemic Review and Meta-Analysis. Arch. Orthop. Trauma Surg. 2021, 141, 761–773. [Google Scholar] [CrossRef]
- Corpuz, M.; Woon, C.Y.L.; Chong, K.W. A Delayed Talar Neck Fracture after Subtalar Arthroereisis in an Adolescent. J. Pediatr. Orthop. B 2011, 20, 325–328. [Google Scholar]
- Cook, E.A.; Cook, J.J.; Basile, P. Identifying Risk Factors in Subtalar Arthroereisis Explantation: A Propensity-Matched Analysis. J. Foot Ankle Surg. 2011, 50, 395–401. [Google Scholar] [CrossRef] [PubMed]




| Total (n = 47) | p Value | |
|---|---|---|
| Age (years) Mean ± SD Range | 11.1 ± 1.29 8–13 | |
| Gender (Male–Female) | 39:8 | <0.01 |
| Affected side (Left–Right) | 23:24 | 0.52 |
| Bilateral foot cases | 21 | |
| Soft tissue procedure | ||
| Medial capsule plication | 31 (66%) | |
| Kidner procedure | 16 (34%) | |
| Gastronomes lengthening (Strayer) | 25 (53%) |
| Timepoint | AP Meary’s Angle | Lateral Meary’s Angle | Calcaneal Pitch | |||
|---|---|---|---|---|---|---|
| Mean ± SD (°) | p Value | Mean ± SD (°) | p Value | Mean ± SD (°) | p Value | |
| Preoperative | 13.09 ± 7.19 | 9.77 ± 5.37 | 14.52 ± 3.19 | |||
| PO | 4.79 ± 4.58 | <0.001 a | 4.13 ± 3.13 | <0.001 a | 17.45 ± 2.23 | <0.001 a |
| PO1M | 5.26 ± 4.08 | <0.001 a | 4.06 ± 3.12 | <0.001 a | 16.87 ± 2.19 | <0.001 a |
| PO3M | 6.03 ± 4.18 | <0.001 a | 4.34 ± 3.23 | <0.001 a | 16.65 ± 2.31 | <0.001 a |
| PO6M | 6.32 ± 4.27 | <0.001 a | 5.10 ± 3.97 | <0.001 a | 16.64 ± 2.56 | <0.001 a |
| PO1Y | 6.83 ± 4.80 | <0.001 a | 4.86 ± 4.25 | <0.001 a | 16.68 ± 2.50 | <0.001 a |
| PO5Y | 6.69 ± 4.46 | <0.001 a; 0.002 b | 4.88 ± 4.31 | <0.001 a; 0.283 b | 16.89 ± 2.50 | <0.001 a; 0.084 b |
| Timepoint | Ankle AP a | Foot AP a | ||||||
|---|---|---|---|---|---|---|---|---|
| Position b | Mean c Migration (mm) | IQR (mm) | p Value | Position b | Mean c Migration (mm) | IQR (mm) | p Value | |
| Implant position | ||||||||
| PO d | −4.46 | +1.17 | ||||||
| PO1M | −1.55 | +2.89 | ||||||
| PO3M | −1.77 | +3.21 | ||||||
| PO6M | −1.73 | +3.40 | ||||||
| PO1Y | −1.74 | +3.53 | ||||||
| PO5Y | −2.05 | +3.67 | ||||||
| Migration distance | <0.001 e | <0.001 e | ||||||
| PO–PO1M | 3.24 | 1.68–4.6 | 3.01 | 1.25–3.63 | ||||
| PO1M–PO3M | 0.93 | 0.38–1.05 | 1.21 | 0.38–1.23 | ||||
| PO3M–PO6M | 0.49 | 0.1–0.7 | 0.54 | 0.1–0.73 | ||||
| PO6M–PO1Y | 0.51 | 0.1–0.73 | 0.64 | 0.1–0.9 | ||||
| PO1Y–PO5Y | 0.78 | 0.2–1.03 | 0.76 | 0.2–0.8 | ||||
| No. | Complication Type | Patient Details | Timing | Management | Outcome |
|---|---|---|---|---|---|
| 1 | Early implant dislodgement | 13-year-old boy with low-energy ankle sprain | 1 month | Revision STA with implant reinsertion | Complete symptom resolution was achieved with no sequelae, and the implant remained well-positioned at the 5-year follow-up |
| 2 | Implant subsidence | 10-year-old female who received STA + Kidner procedure suffered from sprain injury | 7 months | Lateral column lengthening | Bone union achieved at 1 year |
| 3 | Persistent sinus tarsi discomfort | 8-year-old male without any trauma | 12 months | Implant removal | Hindfoot and forefoot alignment were maintained with satisfactory correction at the 5-year follow-up |
| 4 | Persistent sinus tarsi discomfort | 12-year-old male without any trauma | Symptoms persisted after surgery | Corticosteroid injection | Complete symptom resolution was achieved following corticosteroid injection at 6 months |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Huang, Y.-P.; Wu, N.-J.; Cheng, S.-E.; Lin, S.-M.; Lan, T.-Y. Implant Migration and Clinical Outcomes in Pediatric Symptomatic Flexible Flatfoot Treated with Subtalar Arthroereisis: A Cohort Study with Long-Term Follow-Up Results. Diagnostics 2025, 15, 1761. https://doi.org/10.3390/diagnostics15141761
Huang Y-P, Wu N-J, Cheng S-E, Lin S-M, Lan T-Y. Implant Migration and Clinical Outcomes in Pediatric Symptomatic Flexible Flatfoot Treated with Subtalar Arthroereisis: A Cohort Study with Long-Term Follow-Up Results. Diagnostics. 2025; 15(14):1761. https://doi.org/10.3390/diagnostics15141761
Chicago/Turabian StyleHuang, Yu-Po, Nian-Jhen Wu, Shou-En Cheng, Shang-Ming Lin, and Tsung-Yu Lan. 2025. "Implant Migration and Clinical Outcomes in Pediatric Symptomatic Flexible Flatfoot Treated with Subtalar Arthroereisis: A Cohort Study with Long-Term Follow-Up Results" Diagnostics 15, no. 14: 1761. https://doi.org/10.3390/diagnostics15141761
APA StyleHuang, Y.-P., Wu, N.-J., Cheng, S.-E., Lin, S.-M., & Lan, T.-Y. (2025). Implant Migration and Clinical Outcomes in Pediatric Symptomatic Flexible Flatfoot Treated with Subtalar Arthroereisis: A Cohort Study with Long-Term Follow-Up Results. Diagnostics, 15(14), 1761. https://doi.org/10.3390/diagnostics15141761






