A Study on the Diagnosis of Lumbar Spinal Malposition in Chuna Manual Therapy Using X-Ray Images Based on Digital Markers
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethics and Trial Registration
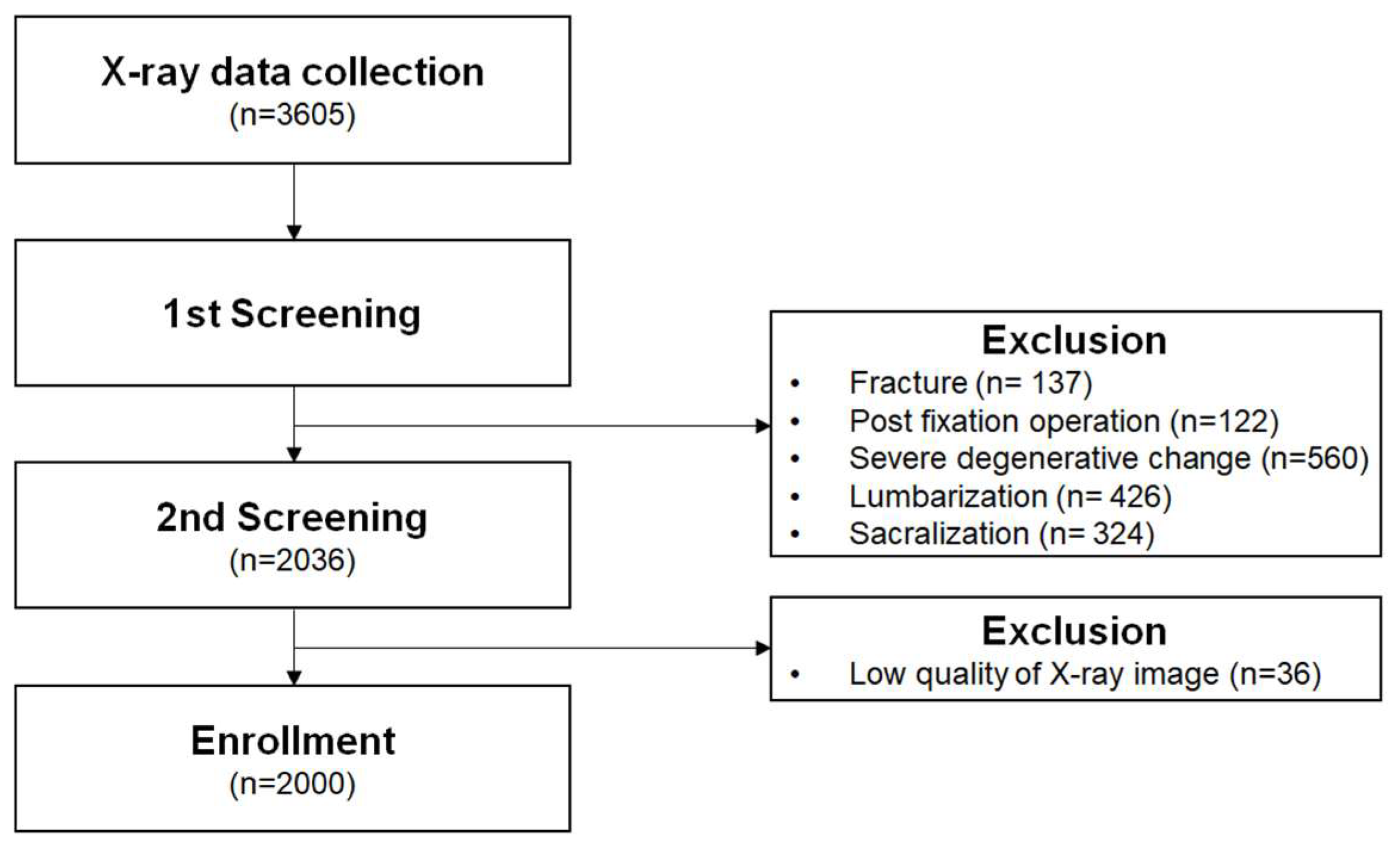
2.2. Study Participants and Collection of Radiographic Cases
2.3. Sample Size Calculation
2.4. Eligibility Criteria
2.4.1. Inclusion Criteria
- (a)
- Adult men and women aged 18–80 years;
- (b)
- Patients who underwent lumbar spine plain radiography at International St. Mary’s Hospital, Catholic Kwandong University, either as part of a clinical visit or during follow-up in the Department of Neurosurgery.
2.4.2. Exclusion Criteria
- (a)
- History of spinal surgery involving instrumentation, such as spinal fusion or screw fixation;
- (b)
- Presence of structural spinal abnormalities that preclude digital marker generation (e.g., tumors, fractures, lumbar sacralization, sacral lumbarization, or severe scoliosis);
- (c)
- Individuals deemed unsuitable for participation by the research investigator.
2.5. CMT Spinal Diagnostic Panel
2.6. Radiographic Analysis
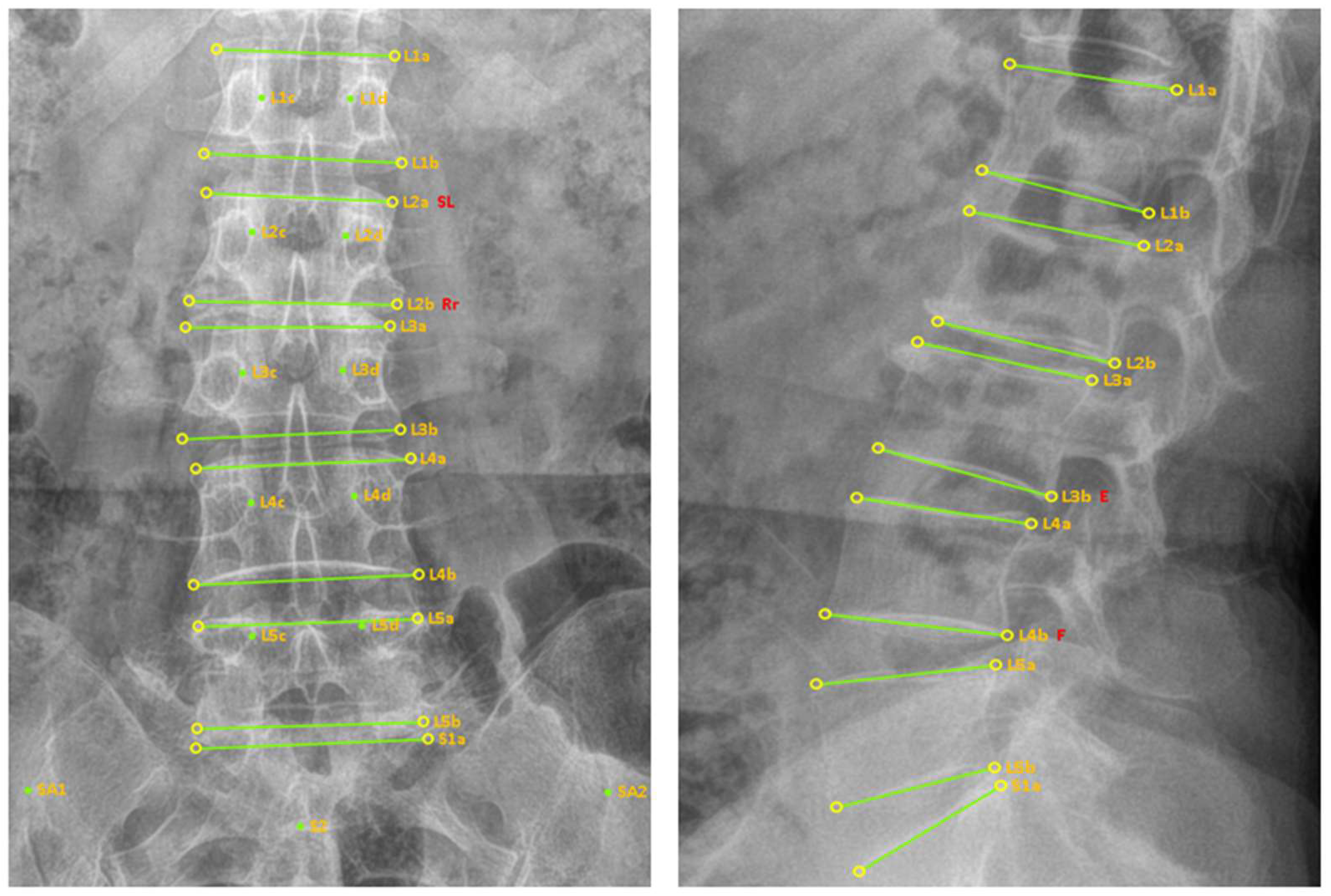
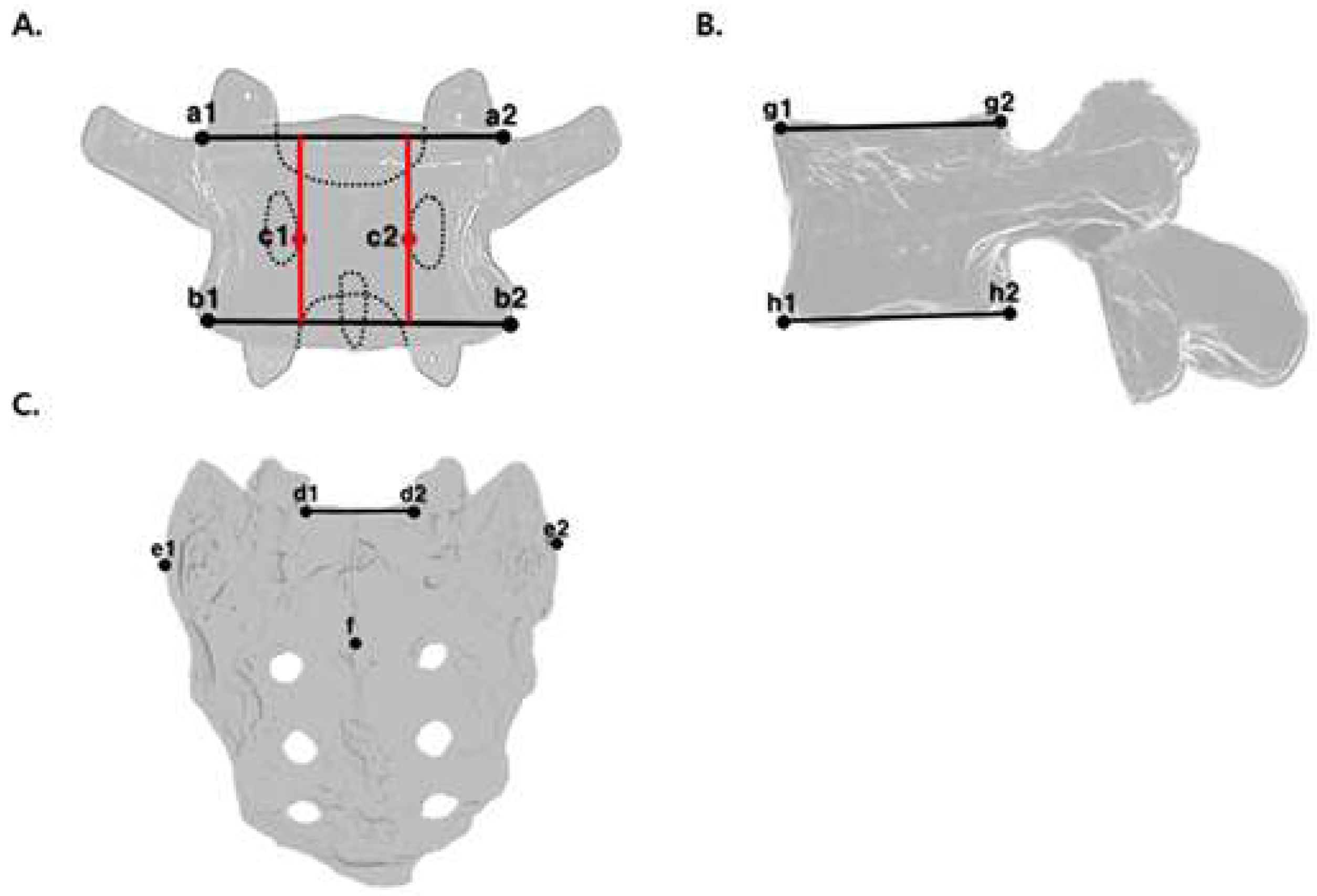
2.7. Digital Marker Generation Method
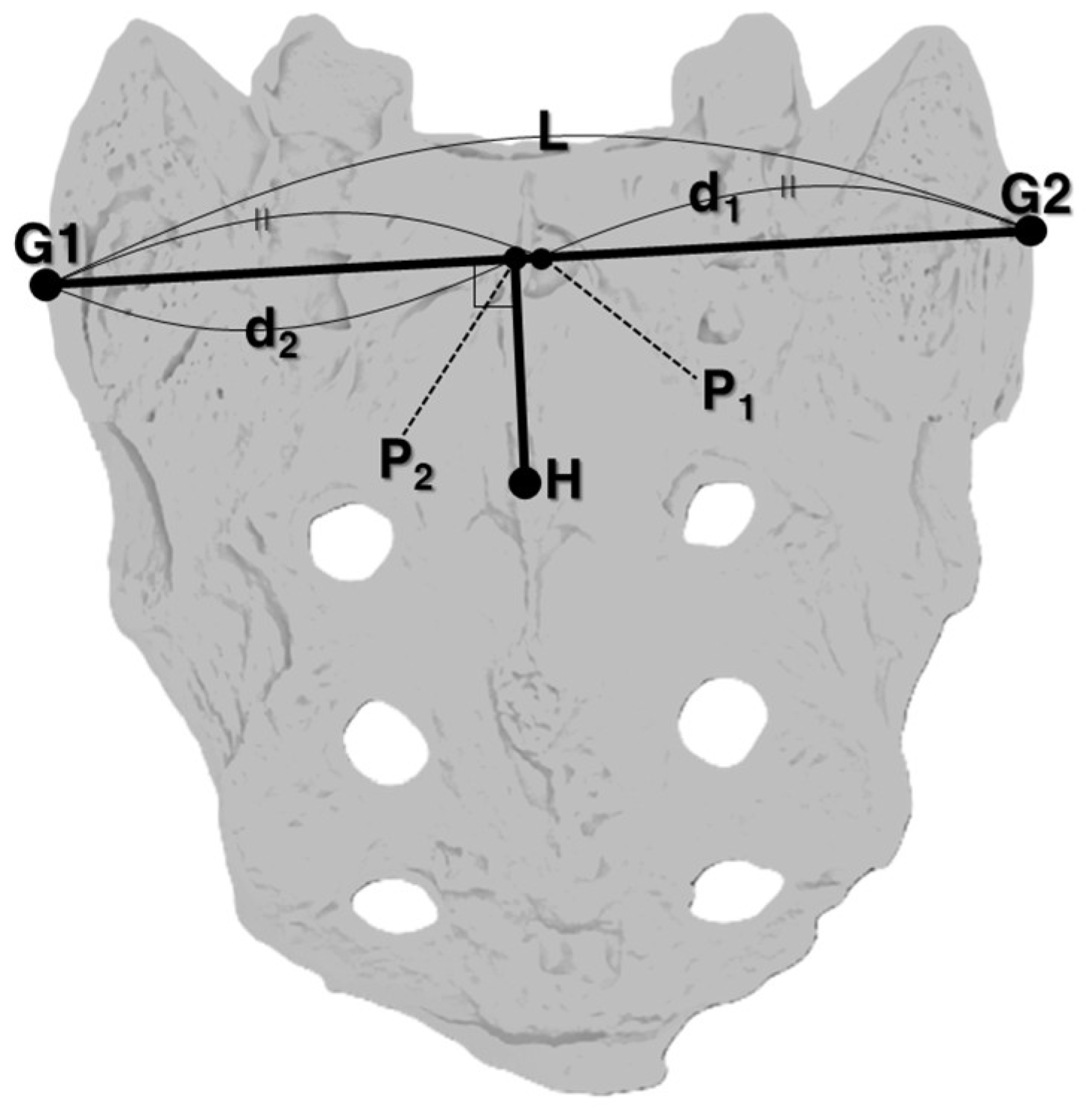
2.7.1. AP View
2.7.2. Lateral View
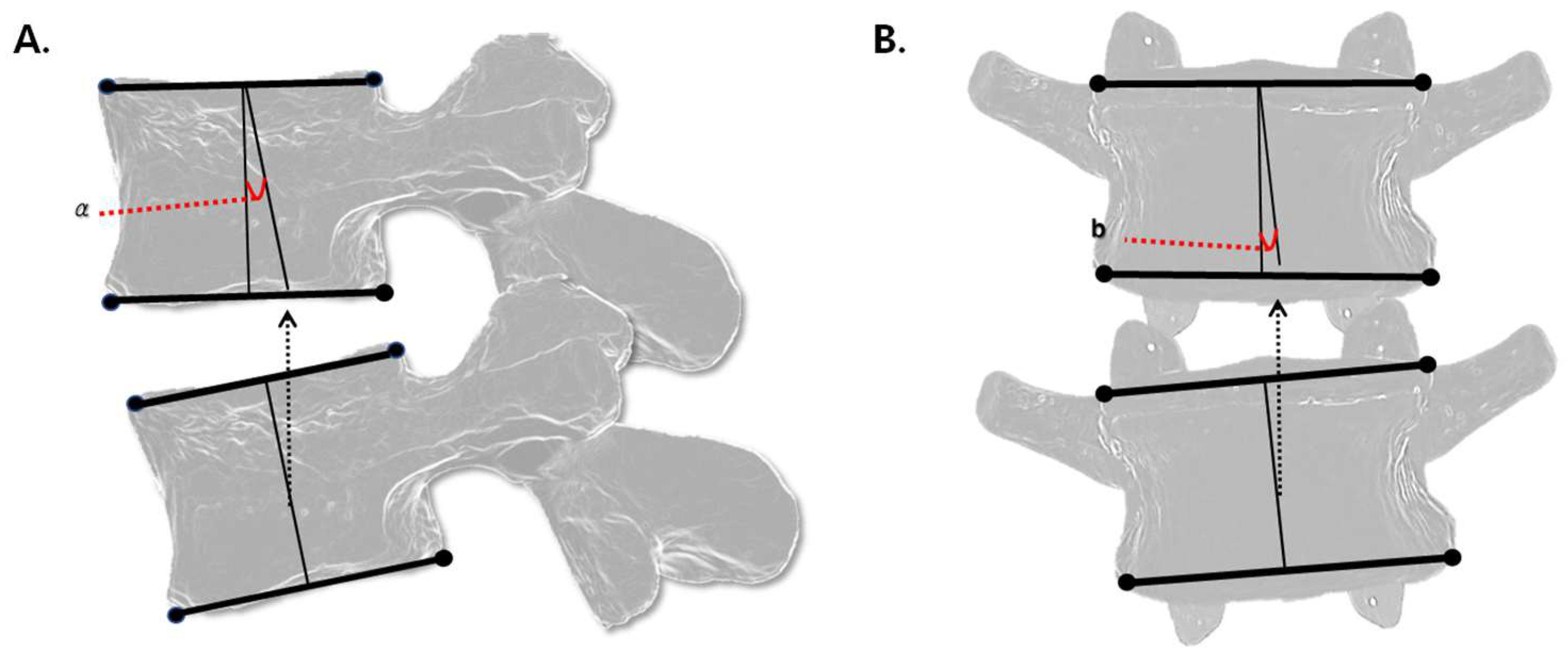
2.8. Method for Malposition Angle Analysis Based on Digital Markers
2.8.1. Flexion/Extension Angle
2.8.2. Lateral Bending Angle
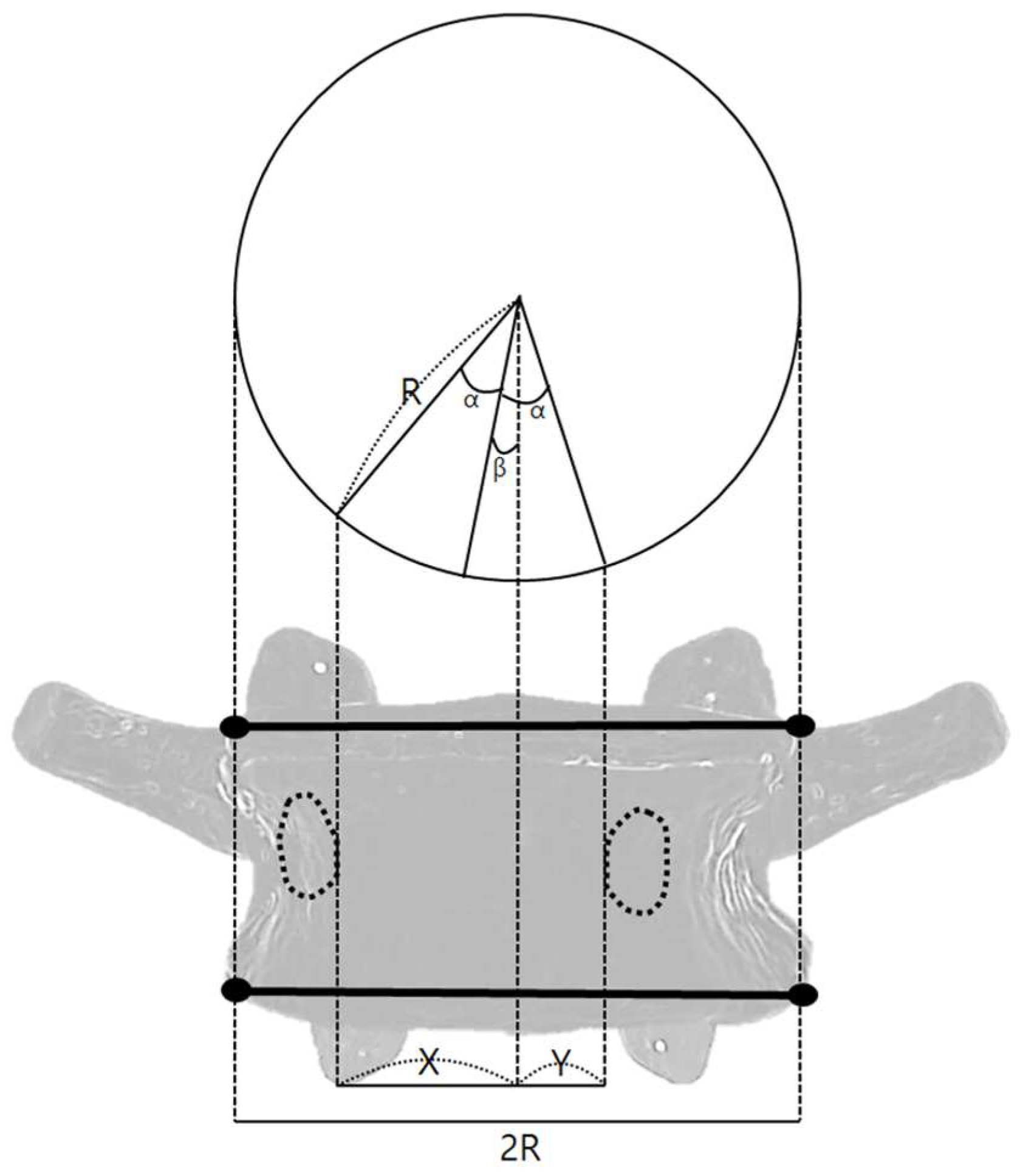
2.8.3. Rotation Angle
2.9. Result Derivation Method
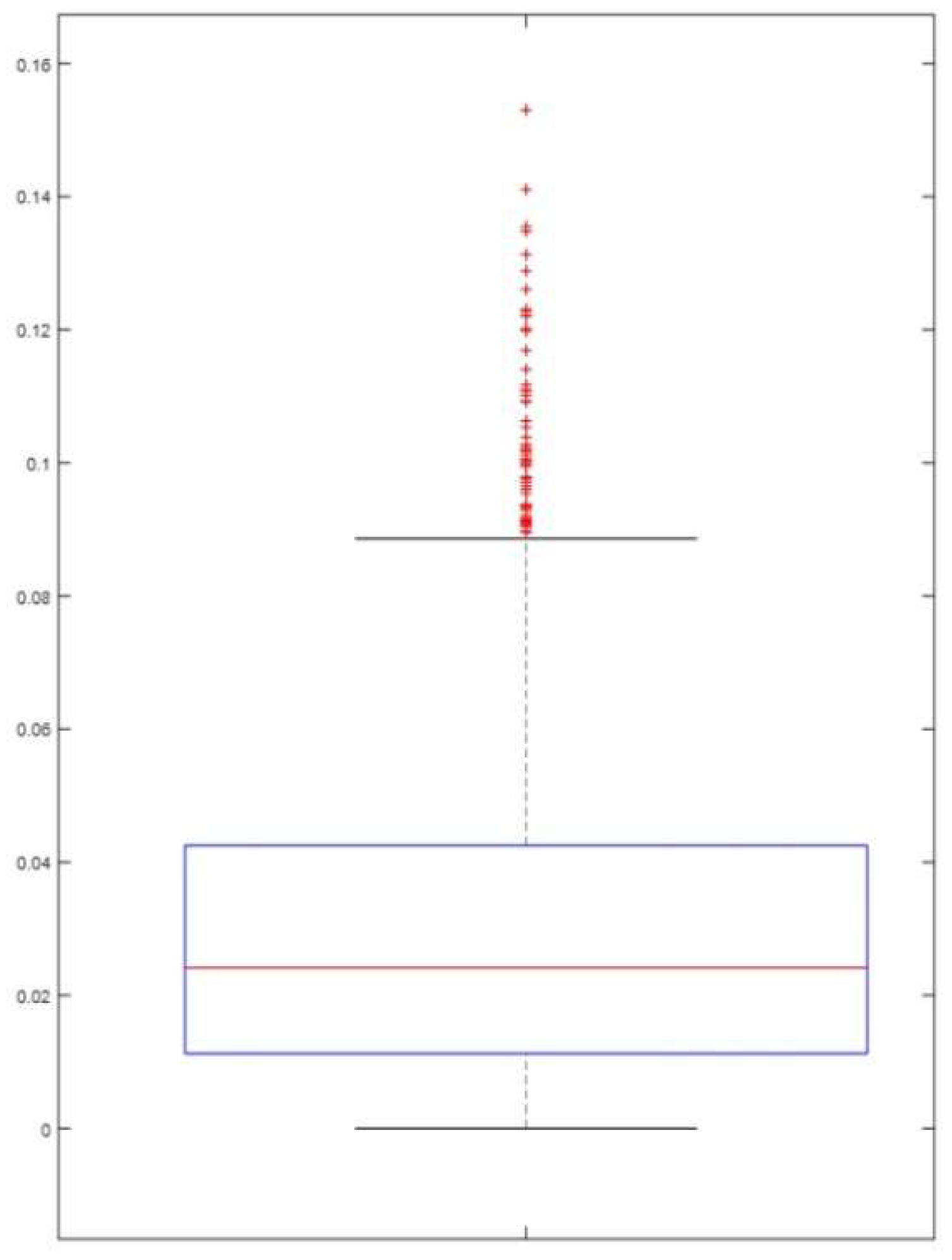
2.10. Statistical Analysis
3. Results
3.1. Sample Selection
3.2. Number of Malpositioned Vertebral Bodies
3.3. Malposition Diagnostic Accuracy
3.3.1. Flexion/Extension Malposition
3.3.2. Lateral Bending Malposition
3.3.3. Rotation Malposition
3.4. Optimal Angles for Maximum Diagnostic Accuracy
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Korean Society of Chuna Manual Medicine for Spine and Nerves. Chuna Manual Medicine, 25th ed.; Korean Society of Chuna Manual Medicine for Spine and Nerves: Seoul, Republic of Korea, 2017; pp. 4, 17, 27–31, 54–64, 75–80. [Google Scholar]
- Park, T.Y.; Moon, T.W.; Cho, D.C.; Lee, J.H.; Ko, Y.S.; Hwang, E.H.; Heo, K.H.; Choi, T.Y.; Shin, B.C. An introduction to Chuna manual medicine in Korea: History, insurance coverage, education, and clinical research in Korean literature. Integr. Med. Res. 2014, 3, 49–59. [Google Scholar] [CrossRef] [PubMed]
- In, H. Chuna manual therapy for spinal scoliosis: A review of clinical study. J. Korean Soc. Chuna Man. Med. Spine Nerves 2019, 14, 39–47. [Google Scholar] [CrossRef]
- Park, S.W.; Byun, J.H.; Lee, C.H.; Ha, I.Y.; Lee, J.H. The trend review of Chuna therapy on neck disorders and cervical disc herniation in Pubmed. J. Korean Soc. Chuna Man. Med. Spine Nerves 2013, 8, 1–19. [Google Scholar]
- Lim, K.T.; Shin, B.C.; Heo, I.; Hwang, M.S. Chuna manual therapy for lumbar spinal stenosis: A systematic review. J. Korean Soc. Chuna Man. Med. Spine Nerves 2018, 13, 1–10. [Google Scholar] [CrossRef]
- Najm, W.I.; Seffinger, M.A.; Mishra, S.I.; Dickerson, V.M.; Adams, A.; Reinsch, S.; Murphy, L.S.; Goodman, A.F. Content validity of manual spinal palpatory exams—A systematic review. BMC Complement. Altern. Med. 2003, 3, 1. [Google Scholar] [CrossRef]
- Nolet, P.S.; Yu, H.; Côté, P.; Meyer, A.L.; Kristman, V.L.; Sutton, D.; Murnaghan, K.; Lemeunier, N. Reliability and validity of manual palpation for the assessment of patients with low back pain: A systematic and critical review. Chiropr. Man. Ther. 2021, 29, 33. [Google Scholar] [CrossRef]
- Hestbaek, L.; Leboeuf-Yde, C. Are chiropractic tests for the lumbo-pelvic spine reliable and valid? A systematic critical literature review. J. Manip. Physiol. Ther. 2000, 23, 258–275. [Google Scholar] [CrossRef]
- Lee, J.H.; Woo, H.; Jang, J.S.; Kim, J.I.; Na, Y.C.; Kim, K.R.; Cho, E.; Lee, J.H.; Park, T.Y. Comparison of concordance between chuna manual therapy diagnostic methods (palpation, X-ray, artificial intelligence program) in lumbar spine: An exploratory, cross-sectional clinical study. Diagnostics 2022, 12, 2732. [Google Scholar] [CrossRef]
- Akeda, K.; Hasegawa, T.; Togo, Y.; Watanabe, K.; Kawaguchi, K.; Yamada, J.; Takegami, N.; Fujiwara, T.; Sudo, A. Quantitative analysis of lumbar disc bulging in patients with lumbar spinal stenosis: Implication for surgical outcomes of decompression surgery. J. Clin. Med. 2023, 12, 6172. [Google Scholar] [CrossRef]
- Lee, J.H.; Kim, C.G.; Jo, D.C.; Moon, S.J.; Park, T.Y.; Ko, Y.S.; Nam, H.W.; Lee, J.H. Diagnostic X-ray from the perspective of Chuna manual medicine, based on the listing system of spinal and pelvic subluxation. J. Korean Soc. Chuna Man. Med. Spine Nerves 2014, 9, 1–14. [Google Scholar]
- Lee, J.H.; Choi, M.H.; Kim, J.I.; Jang, J.S.; Park, T.Y. Radiograph-based diagnostic methods for thoracic and lumbar spine malposition in Chuna manual therapy using biomarkers. J. Churna Man. Med. Spine Nerves 2023, 18, 1–8. [Google Scholar]
- Jang, J.S.; Kim, J.I.; Ku, B.; Lee, J.H. Reliability analysis of vertebral landmark labelling on lumbar spine X-ray images. Diagnostics 2023, 13, 1411. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, A.S.; Ramakrishnan, R.; Ramachandran, V.; Ramachandran, S.S.; Phan, K.; Antonsen, E.L. Ultrasound diagnosis and therapeutic intervention in the spine. J. Spine Surg. 2018, 4, 423–432. [Google Scholar] [CrossRef] [PubMed]
- Roudsari, B.; Jarvik, J.G. Lumbar spine MRI for low back pain: Indications and yield. AJR Am. J. Roentgenol. 2010, 195, 550–559. [Google Scholar] [CrossRef]
- Farshad, M.; Aichmair, A.; Hughes, A.P.; Herzog, R.J.; Farshad-Amacker, N.A. A reliable measurement for identifying a lumbosacral transitional vertebra with a solid bony bridge on a single-slice midsagittal MRI or plain lateral radiograph. Bone Jt. J. 2013, 95-B, 1533–1537. [Google Scholar] [CrossRef]
- Chi, W.M.; Cheng, C.W.; Yeh, W.C.; Chuang, S.C.; Chang, T.S.; Chen, J.H. Vertebral axial rotation measurement method. Comput. Methods Programs Biomed. 2006, 81, 8–17. [Google Scholar] [CrossRef]
- Zhang, R. A state-of-the-art survey of deep learning for lumbar spine image analysis: X-RAY, CT, and MRI. AI Med. 2024, 1, 3. [Google Scholar] [CrossRef]
- Joshi, K.; Kumar, S.; Rawat, J.; Kumari, A.; Gupta, A.; Sharma, N. Fraud app detection of Google Play store apps using decision tree. In Proceedings of the 2022 2nd International Conference on Innovative Practices in Technology and Management (ICIPTM), Gautam Buddha Nagar, India, 23–25 February 2022; pp. 243–246. [Google Scholar]
- Shin, B.C.; Cho, H.W.; Hwang, E.H.; Sul, J.U.; Shin, M.S.; Nam, H.W. An literatural study of listing system of spinal subluxation. J. Chuna Man. Med. Spine Nerves 2011, 6, 141–148. [Google Scholar]
- Seffinger, M.A.; Najm, W.I.; Mishra, S.I.; Adams, A.; Dickerson, V.M.; Murphy, L.S.; Reinsch, S. Reliability of spinal palpation for diagnosis of back and neck pain: A systematic review of the literature. Spine 2004, 29, E413–E425. [Google Scholar] [CrossRef]
- Inoue, N.; Orías, A.A.E.; Segami, K. Biomechanics of the lumbar facet joint. Spine Surg. Relat. Res. 2020, 4, 1–7. [Google Scholar] [CrossRef]
- O’Sullivan, P.B. Lumbar segmental instability’: Clinical presentation and specific stabilizing exercise management. Man. Ther. 2000, 5, 2–12. [Google Scholar] [CrossRef] [PubMed]
- Damasceno, L.H.F.; Catarin, S.R.G.; Campos, A.D.; Defino, H.L.A. Lumbar lordosis: A study of angle values and of vertebral bodies and intervertebral discs role. Acta Ortop. Bras. 2006, 14, 193–198. [Google Scholar] [CrossRef]
- Jun, J.Y.; Lee, J.S.; Lee, S.J.; Nam, J.H.; Lee, M.J.; Kim, K.W.; Lim, S.J.; Song, J.H.; Moon, J.Y.; Yeom, S.C.; et al. A relationship study of lumbar lordortic angle and herniation of intervertebral disc. J. Korean Soc. Chuna Man. Med. Spine Nerves 2012, 7, 83–90. [Google Scholar]
- Aylott, C.E.; Puna, R.; Robertson, P.A.; Walker, C. Spinous process morphology: The effect of ageing through adulthood on spinous process size and relationship to sagittal alignment. Eur. Spine J. 2012, 21, 1007–1012. [Google Scholar] [CrossRef]
- Mwakikunga, A.; Manjatika, A.; Mazengenya, P. Morphometric description of thoracic vertebral pedicles in adult Malawian cadavers and implications for transpedicular spine fixation. Int. J. Morphol. 2021, 39, 1575–1580. [Google Scholar] [CrossRef]
- Cao, Y.; Chen, R.C.; Katz, A.J. Why is a small sample size not enough. Oncologist 2024, 29, 761–763. [Google Scholar] [CrossRef]
- Bronfort, G.; Haas, M.; Evans, R.; Leininger, B.; Triano, J. Effectiveness of manual therapies: The UK evidence report. Chiropr. Osteopat. 2010, 18, 3. [Google Scholar] [CrossRef]
- Assendelft, W.J.; Morton, S.C.; Yu, E.I.; Suttorp, M.J.; Shekelle, P.G. Spinal manipulative therapy for low back pain. A meta-analysis of effectiveness relative to other therapies. Ann. Intern. Med. 2003, 138, 871–881. [Google Scholar] [CrossRef]
- Cook, C.; Hegedus, E. Diagnostic utility of clinical tests for spinal dysfunction. Man. Ther. 2011, 16, 21–25. [Google Scholar] [CrossRef]
- Wang, J.; Zhang, J.; Xu, R.; Chen, T.G.; Zhou, K.S.; Zhang, H.H. Measurement of scoliosis Cobb angle by end vertebra tilt angle method. J. Orthop. Surg. Res. 2018, 13, 223. [Google Scholar] [CrossRef]
|
Flexion
(n/2000) |
Extension
(n/2000) |
Rt. Lateral
Bending (n/2000) |
Lt. Lateral
Bending (n/2000) | Rt. Rotation (n/1600) * | Lt. Rotation (n/1600) * | |
|---|---|---|---|---|---|---|
| Rater 1 | 985 | 44 | 320 | 453 | 170 | 171 |
| Rater 2 | 451 | 102 | 147 | 195 | 60 | 253 |
| Rater 3 | 945 | 131 | 358 | 365 | 202 | 391 |
| Rater 4 | 52 | 34 | 188 | 216 | 101 | 210 |
| Rater 5 | 192 | 144 | 62 | 63 | 74 | 113 |
| Total | 2625 | 455 | 1075 | 1292 | 607 | 1138 |
| F1_W Score | ||||||
|---|---|---|---|---|---|---|
| Global Threshold | Local Threshold | |||||
| Flexion/Extension | Lateral Bending | Rotation | Flexion/Extension | Lateral Bending | Rotation | |
| Rater 1 | 0.81 | 0.93 | 0.72 | 0.89 | 0.94 | 0.73 |
| Rater 2 | 0.76 | 0.91 | 0.75 | 0.78 | 0.91 | 0.76 |
| Rater 3 | 0.72 | 0.67 | 0.52 | 0.79 | 0.70 | 0.55 |
| Rater 4 | 0.80 | 0.86 | 0.73 | 0.95 | 0.86 | 0.74 |
| Rater 5 | 0.70 | 0.88 | 0.82 | 0.81 | 0.94 | 0.84 |
| Average ±SD | 0.76 ±0.04 | 0.85 ±0.09 | 0.71 ±0.10 | 0.84 ±0.07 | 0.87 ±0.09 | 0.72 ±0.10 |
| Vertebral Body | |||||
|---|---|---|---|---|---|
| L1 | L2 | L3 | L4 | L5 | |
| Flexion (°) | 0.64 | 3.56 | 5.29 | 8.90 | 8.53 |
| Extension (°) | 10.46 | 14.95 | 17.61 | 20.76 | 24.47 |
| Lateral bending (°) | 2.21 | 2.10 | 1.92 | 2.06 | 2.31 |
| Rotation (°) | 9.49 | 5.19 | 4.59 | 5.87 | 7.13 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ju, M.-S.; Park, T.-Y.; Choi, M.; Ko, Y.; Na, Y.C.; Jeong, Y.H.; Jang, J.-S.; Lee, J.-H. A Study on the Diagnosis of Lumbar Spinal Malposition in Chuna Manual Therapy Using X-Ray Images Based on Digital Markers. Diagnostics 2025, 15, 1748. https://doi.org/10.3390/diagnostics15141748
Ju M-S, Park T-Y, Choi M, Ko Y, Na YC, Jeong YH, Jang J-S, Lee J-H. A Study on the Diagnosis of Lumbar Spinal Malposition in Chuna Manual Therapy Using X-Ray Images Based on Digital Markers. Diagnostics. 2025; 15(14):1748. https://doi.org/10.3390/diagnostics15141748
Chicago/Turabian StyleJu, Min-Su, Tae-Yong Park, Minho Choi, Younseok Ko, Young Cheol Na, Yeong Ha Jeong, Jun-Su Jang, and Jin-Hyun Lee. 2025. "A Study on the Diagnosis of Lumbar Spinal Malposition in Chuna Manual Therapy Using X-Ray Images Based on Digital Markers" Diagnostics 15, no. 14: 1748. https://doi.org/10.3390/diagnostics15141748
APA StyleJu, M.-S., Park, T.-Y., Choi, M., Ko, Y., Na, Y. C., Jeong, Y. H., Jang, J.-S., & Lee, J.-H. (2025). A Study on the Diagnosis of Lumbar Spinal Malposition in Chuna Manual Therapy Using X-Ray Images Based on Digital Markers. Diagnostics, 15(14), 1748. https://doi.org/10.3390/diagnostics15141748









