Cranial Vault Deformation and Its Association with Mandibular Deviation in Patients with Facial Asymmetry: A CT-Based Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Research Subjects and Materials
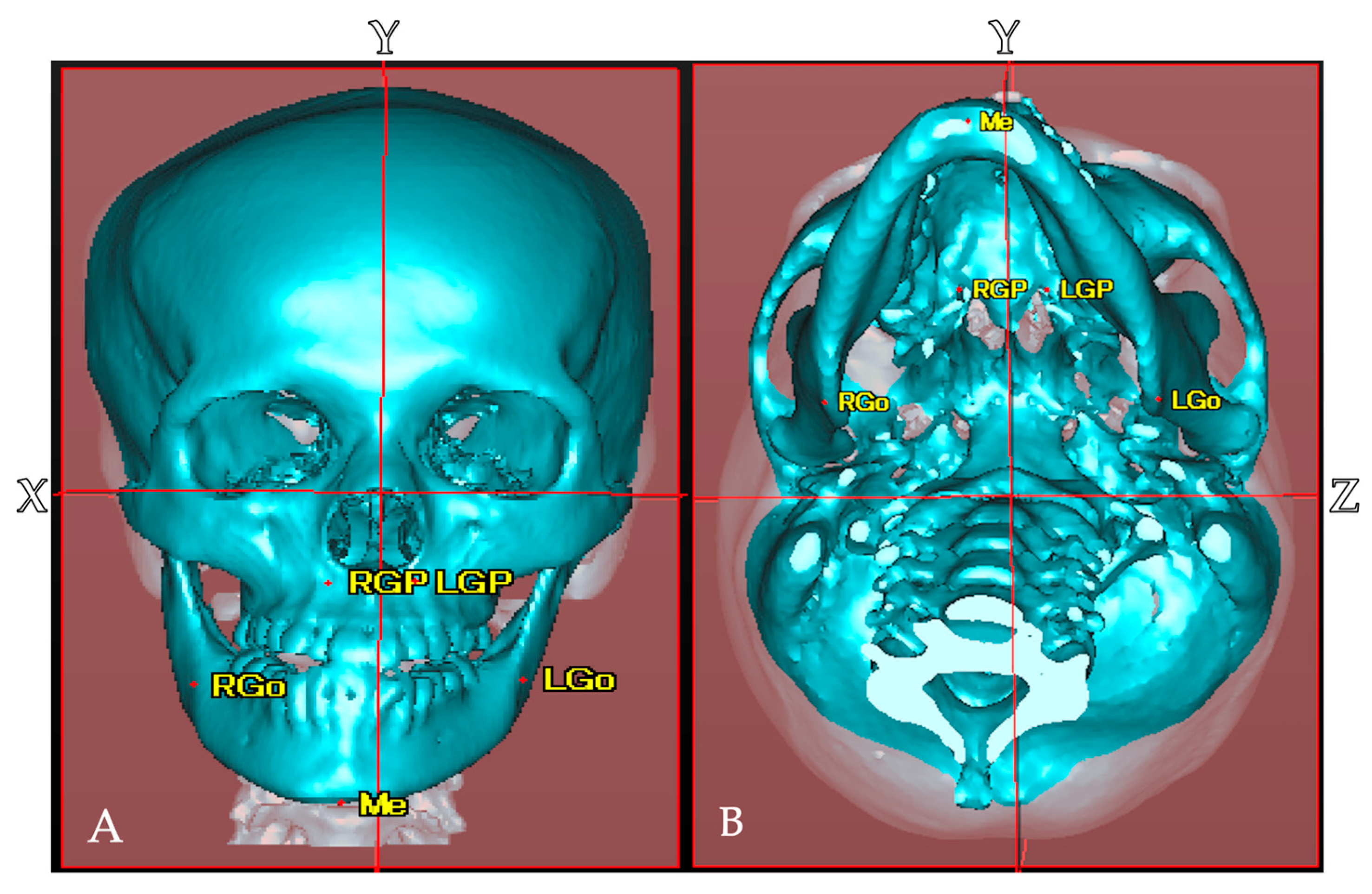
2.2. Establishment of Reference Points, Reference Planes, and Measurement Items in CT Images
2.3. Measurement and Evaluation
2.3.1. Comparison of Mandibular Deviation Between Asymmetric and Symmetric Groups
2.3.2. Comparison of Cranial Vault Volume Between Asymmetric and Symmetric Groups
2.3.3. Measurement of the Displacement Direction and Amount of Menton in Facial Asymmetry Groups
2.4. Statistical Analysis
3. Results
3.1. Comparison of Distance Measurements of Anatomical Structures in Maxilla and Mandible in Symmetric and Asymmetric Groups
3.2. Comparison of Left–Right Differences in Cranial Vault Volume Measurements Between Symmetric and Asymmetric Facial Groups
3.3. Relationship Between Posterior Cranial and Mandibular Deviation
4. Discussion
4.1. Deviation of the Maxilla and Mandible in Patients with Facial Asymmetry
4.2. Differences in the Volume of the Posterior Cranial Vault
4.3. Correlation Between Mandibular Deviation and Cranial Vault Volume
4.4. Research Methods
4.5. Positional Plagiocephaly
4.6. Limitations
4.7. Clinical Implication
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Katagiri, W.; Kobayashi, T.; Sasaki, A.; Susami, T.; Suda, N.; Tanaka, E.; Chikazu, D.; Tominaga, K.; Moriyama, K.; Yamashiro, T.; et al. Investigation of surgical orthodontic treatment in japan—A nationwide survey by Japanese society for jaw deformities in 2017. Jpn. J. Jaw Deform. 2020, 30, 213–225. [Google Scholar] [CrossRef]
- Tani, M.; Iketani, M.; Watanabe, M.; Suda, S.; Fujimura, N.; Miyazawa, M.; Nagura, H.; Enomoto, S. Posterior-anterior cephametric analysis in patients with dentofacial deformities. J. Jpn. Stomatol. Soc. 1989, 35, 1749–1759. [Google Scholar] [CrossRef]
- Severt, T.R.; Proffit, W.R. The prevalence of facial asymmetry in the dentofacial deformities population at the University of North Carolina. Int. J. Adult Orthod. Orthognath. Surg. 1997, 12, 171–176. [Google Scholar]
- Samman, N.; Tong, A.C.; Cheung, D.L.; Tideman, H. Analysis of 300 dentofacial deformities in Hong Kong. Int. J. Adult Orthod. Orthognath. Surg. 1992, 7, 181–185. [Google Scholar]
- Chew, M.T. Spectrum and management of dentofacial deformities in a multiethnic Asian population. Angle Orthod. 2006, 76, 806–809. [Google Scholar]
- You, K.H.; Lee, K.J.; Lee, S.H.; Baik, H.S. Three-dimensional computed tomography analysis of mandibular morphology in patients with facial asymmetry and mandibular prognathism. Am. J. Orthod. Dentofac. Orthop. 2010, 138, 540.e1–540.e8, discussion 541. [Google Scholar] [CrossRef] [PubMed]
- Kamata, H.; Higashihori, N.; Fukuoka, H.; Shiga, M.; Kawamoto, T.; Moriyama, K. Comprehending the three-dimensional mandibular morphology of facial asymmetry patients with mandibular prognathism. Prog. Orthod. 2017, 18, 43. [Google Scholar] [CrossRef]
- Lin, H.; Zhu, P.; Lin, Y.; Wan, S.; Shu, X.; Xu, Y.; Zheng, Y. Mandibular asymmetry: A three-dimensional quantification of bilateral condyles. Head Face Med. 2013, 9, 42. [Google Scholar] [CrossRef]
- Kim, K.A.; Lee, J.W.; Park, J.H.; Kim, B.H.; Ahn, H.W.; Kim, S.J. Targeted presurgical decompensation in patients with yaw-dependent facial asymmetry. Korean J. Orthod. 2017, 47, 195–206. [Google Scholar] [CrossRef]
- Yamaguchi, K.; Sasaki, A.; Kawajiri, A.; Fujimoto, K.; Uesato, T.; Toyota, A.; Suda, N. Three-dimentional analysis of cranial vault and position of mandibular fossa -Part 2. Analysis of asymmetry mandibular protrusion cases. Jpn. J. Jaw Deform. 2020, 30, 267–280. [Google Scholar] [CrossRef]
- Lisboa, C.O.; Borges, M.S.; Medeiros, P.J.D.; Motta, A.T.; Mucha, J.N. Orthodontic-surgical retreatment of facial asymmetry with occlusal cant and severe root resorption: A 3-year follow-up. Am. J. Orthod. Dentofac. Orthop. 2017, 152, 268–280. [Google Scholar] [CrossRef] [PubMed]
- Moon, I.Y.; Lim, S.Y.; Oh, K.S. Analysis of Facial Asymmetry in Deformational Plagiocephaly Using Three-Dimensional Computed Tomographic Review. Arch. Craniofac. Surg. 2014, 15, 109–116. [Google Scholar] [CrossRef] [PubMed]
- Hayashi, Y.; Tachiki, C.; Morikawa, T.; Aihara, Y.; Matsunaga, S.; Sugahara, K.; Watanabe, A.; Kawamata, T.; Nishii, Y. Three-Dimensional Analysis of the Cranial Base Structure in Patients with Facial Asymmetry. Diagnostics 2024, 14, 24. [Google Scholar] [CrossRef]
- Ono, S.; Tachiki, C.; Morikawa, T.; Aihara, Y.; Matsunaga, S.; Sugahara, K.; Watanabe, A.; Kawamata, T.; Nishii, Y. Morphological Evaluation of Cranium Facial Asymmetry in Class III Malocclusion Patients. Appl. Sci. 2023, 13, 6533. [Google Scholar] [CrossRef]
- Ajmera, D.H.; Zhang, C.; Ng, J.H.H.; Hsung, R.T.; Lam, W.Y.H.; Wang, W.; Leung, Y.Y.; Khambay, B.S.; Gu, M. Three-Dimensional Assessment of Facial Asymmetry in Class III Subjects, Part 2: Evaluating Asymmetry Index and Asymmetry Scores. Clin. Oral Investig. 2023, 27, 5813–5826. [Google Scholar] [CrossRef]
- Zhao, Q.; Chen, K.; Wang, X.; Wu, G. Assessment of Masseter Volume and Postoperative Stability After Orthognathic Surgery in Patients with Skeletal Class III Malocclusion with Facial Asymmetry. J. Craniofac. Surg. 2024, 35, 1249–1252. [Google Scholar] [CrossRef] [PubMed]
- Kwon, T.G.; Lee, K.H.; Park, H.S.; Ryoo, H.M.; Kim, H.J.; Lee, S.H. Relationship between the masticatory muscles and mandibular skeleton in mandibular prognathism with and without asymmetry. J. Oral Maxillofac. Surg. 2007, 65, 1538–1543. [Google Scholar] [CrossRef]
- Chou, S.T.; Wang, J.L.; Chen, S.C.; Pan, C.Y.; Chen, C.M.; Tseng, Y.C. Correlation between facial asymmetry of skeletal class III jaw relationship and morphology of the temporomandibular joint: A cone beam computed tomography study. J. Dent. Sci. 2023, 18, 1031–1041. [Google Scholar] [CrossRef]
- Noh, H.K.; Park, H.S. Does maxillary yaw exist in patients with skeletal Class III facial asymmetry? Am. J. Orthod. Dentofac. Orthop. 2021, 160, 573–587. [Google Scholar] [CrossRef]
- Goto, S.; Saito, I.; Nishii, Y.; Maki, K.; Moriyama, K.; Yamashiro, T. Shika Kyoseigaku (Orthodontics), 7th ed.; Ishiyaku Publishers: Tokyo, Japan, 2014; pp. 39–43. (In Japanese) [Google Scholar]
- Enlow, D.H. The Essentials of Facial Growth, 2nd.; W.B. Saunders: Philadelphia, PA, USA, 2008; pp. 91–113. [Google Scholar]
- Sugano, G.T.; Pauris, C.C.; Silva, Y.B.E.; Pandini, F.E.; Palermo, R.B.S.; Buchaim, D.V.; Buchaim, R.L.; Chacon, E.L.; Aparecida, C.C.; Pagani, B.T.; et al. Topographic and Morphometric Study of the Foramen Spinosum of the Skull and Its Clinical Correlation. Medicina 2022, 58, 1740. [Google Scholar] [CrossRef]
- Ide, Y. Tōkeibu no Kansetsu (Joints of the Head and Neck); Ishiyaku Publishers: Tokyo, Japan, 2009; pp. 84–87. (In Japanese) [Google Scholar]
- Kawamura, T.; Fukui, T.; Nishiyama, H.; Kobayashi, T.; Takagi, R.; Hayashi, T.; Saito, I. Three-dimensional analysis of the temporal bone and mandibular morphology in mandibular prognathism with facial asymmetry. Oral Sci. Int. 2022, 19, 44–51. [Google Scholar] [CrossRef]
- Shirakawa, T.; Fukumoto, S.; Iwamoto, T.; Morikawa, K. Shōni Shika (Pediatric Dentistry), 6th ed.; Ishiyaku Publishers: Tokyo, Japan, 2023; pp. 33–37. (In Japanese) [Google Scholar]
- The American Association of Oral and Maxillofacial Surgeons. Criteria for Orthognatic Surgery. Available online: https://aaoms.org/wp-content/uploads/2025/01/ortho_indications.pdf (accessed on 2 July 2025).
- Haraguchi, S.; Takada, K.; Yasuda, Y. Facial asymmetry in subjects with skeletal Class III deformity. Angle Orthod. 2002, 72, 28–35. [Google Scholar] [PubMed]
- Thiesen, G.; Kim, K.B. Criteria for determining facial asymmetries. Am. J. Orthod. Dentofac. Orthop. 2016, 50, 910. [Google Scholar] [CrossRef]
- Ohmura, E.; Ikawa, M.; Arai, K. Reliability of reference points in the submentovertex cephalogram. Jpn. J. Jaw Deform. 2003, 13, 1–11. [Google Scholar] [CrossRef]
- Zamora, N.; Llamas, J.M.; Cibrián, R.; Gandia, J.L.; Paredes, V. A study on the reproducibility of cephalometric landmarks when undertaking a three-dimensional (3D) cephalometric analysis. Med. Oral Patol. Oral Cir. Bucal 2012, 17, e678–e688. [Google Scholar] [CrossRef] [PubMed]
- Shibata, M.; Nawa, H.; Kise, Y.; Fuyamada, M.; Yoshida, K.; Katsumata, A.; Ariji, E.; Goto, S. Reproducibility of three-dimensional coordinate systems based on craniofacial landmarks: A tentative evaluation of four systems created on images obtained by cone-beam computed tomography with a large field of view. Angle Orthod. 2012, 82, 776–784. [Google Scholar] [CrossRef]
- Marmary, Y.; Zilberman, Y.; Mirsky, Y. Use of foramina spinosa to determine skull midlines. Angle Orthod. 1979, 49, 263–268. [Google Scholar]
- Turk, A.E.; McCarthy, J.G.; Thorne, C.H.; Wisoff, J.H. The “back to sleep campaign” and deformational plagiocephaly: Is there cause for concern? J. Craniofac. Surg. 1996, 7, 12–18. [Google Scholar] [CrossRef]
- Miyabayashi, H.; Nagano, N.; Kato, R.; Hashimoto, S.; Saito, K.; Noto, T.; Ohashi, S.; Masunaga, K.; Morioka, I. Creating reference values for cranial shape in early healthy Japanese infants using a three-dimensional scanner. J. Jpn. Soc. Perinat. Neonatal Med. 2023, 59, 166–173. [Google Scholar] [CrossRef]
- Miyabayashi, H.; Nagano, N.; Kato, R.; Hashimoto, S.; Saito, K.; Noto, T.; Ohashi, S.; Masunaga, K.; Morioka, I. Cranial shapes of Japanese preterm infants at one month of age using a three-dimensional scanner. Brain Dev. 2022, 44, 690–698. [Google Scholar] [CrossRef]
- Kim, D.H.; Kwon, D.R. Neurodevelopmental delay according to severity of deformational plagiocephaly in children. Medicine 2020, 99, e21194. [Google Scholar] [CrossRef] [PubMed]
- Roider, L.; Ungerer, G.; Shock, L.; Aldridge, K.; Al-Samarraie, M.; Tanaka, T.; Muzaffar, A. Increased Incidence of Ophthalmologic Findings in Children With Concurrent Isolated Nonsyndromic Metopic Suture Abnormalities and Deformational Cranial Vault Asymmetry. Cleft Palate Craniofac. J. 2021, 58, 497–504. [Google Scholar] [CrossRef] [PubMed]
- Purzycki, A.; Thompson, E.; Argenta, L.; David, L. Incidence of otitis media in children with deformational plagiocephaly. J. Craniofac. Surg. 2009, 20, 1407–1411. [Google Scholar] [CrossRef] [PubMed]
- Martiniuk, A.L.; Vujovich-Dunn, C.; Park, M.; Yu, W.; Lucas, B.R. Plagiocephaly and Developmental Delay: A Systematic Review. J. Dev. Behav. Pediatr. 2017, 38, 67–78. [Google Scholar] [CrossRef]
- Kajita, H.; Tanaka, I.; Komuro, H.; Nishimaki, S.; Kusakawa, I.; Sakamoto, K. Efficacy of Cranial Orthosis for Plagiocephaly Based on 2D and 3D Evaluation. Arch. Plast. Surg. 2024, 51, 169–181. [Google Scholar] [CrossRef]
- Noto, T.; Nagano, N.; Kato, R.; Hashimoto, S.; Saito, K.; Miyabayashi, H.; Sasano, M.; Sumi, K.; Yoshino, A.; Morioka, I. Natural-Course Evaluation of Infants with Positional Severe Plagiocephaly Using a Three-Dimensional Scanner in Japan: Comparison with Those Who Received Cranial Helmet Therapy. J. Clin. Med. 2021, 10, 3531. [Google Scholar] [CrossRef]





| Symmetry | Asymmetry | |
|---|---|---|
| n = 25 | n = 25 | |
| Sex | ||
| Male | 9 | 11 |
| Female | 16 | 14 |
| Age (y) | ||
| Mean | 25.7 ± 7.4 | 25.2 ± 8.6 |
| Range | 16.1–45.1 | 17.2–45.1 |
| Measurement values | ||
| Mean of ANB (°) | −2.8 ± 2.3 | −3.7 ± 2.8 |
| Mean of Difference in position of Menton (mm) | 1.5 ± 0.68 | 7.2 ± 3.8 |
| Range of Menton (mm) | 0.36–2.89 | 4.1–18.56 |
| Mean of FMA(°) | 28.2 ± 3.9 | 31.3 ± 3.6 |
| Mean of Wits appraisal (mm) | −8.7 ± 2.7 | −11.1 ± 3.5 |
| Abbreviation | Explanation | |
|---|---|---|
| Reference point | ||
| Glabella | G | Most prominent point between the eyebrows |
| Nasion | Na | Most anterior point of the frontal nasal suture |
| Orbirale | Or | Lowest point of the orbital bone margin |
| Porion | Po | Sublingual neural tube opening |
| Foramen spinosum | Fs | Foramen spinosum opening |
| Basion | Ba | Lowest point on the anterior margin of the foramen magnum |
| Menton | Me | Lowest point of the mandibular symphysis |
| Measurement point | ||
| Maxillary | ||
| Greater palatine foramen | GP | Opening in the posterior hard palate of the greater palatine canal |
| Mandible | ||
| Gonion | Go | Most posterior, inferior, and lateral point on the external point at the angle of the mandible |
| Maximum (mm) | Minimum (mm) | Mean (mm) | |
|---|---|---|---|
| Symmetry | |||
| maxillary | |||
| |X − GP| | 3.35 | 0 | 1.20 |
| |Y − GP| | 2.13 | 0.22 | 0.96 |
| |Z − GP| | 3.25 | 0.41 | 1.01 |
| mandible | |||
| |X − Go| | 4.25 | 0.02 | 1.62 |
| |Y − Go| | 1.26 | 0.42 | 1.99 |
| |Z − Go| | 3.84 | 0.61 | 2.04 |
| Asymmetry | |||
| maxillary | |||
| |X − GP| | 3.17 | 0.01 | 1.04 |
| |Y − GP| | 2.97 | 0.37 | 1.38 |
| |Z − GP| | 4.08 | 0.01 | 1.51 |
| mandible | |||
| |X − Go| | 8.15 | 0.06 | 1.47 |
| |Y − Go| | 9.09 | 0.41 | 3.53 |
| |Z − Go| | 9.84 | 1.43 | 4.02 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nishimura, M.; Tachiki, C.; Morikawa, T.; Ariizumi, D.; Matsunaga, S.; Sugahara, K.; Aihara, Y.; Watanabe, A.; Katakura, A.; Kawamata, T.; et al. Cranial Vault Deformation and Its Association with Mandibular Deviation in Patients with Facial Asymmetry: A CT-Based Study. Diagnostics 2025, 15, 1702. https://doi.org/10.3390/diagnostics15131702
Nishimura M, Tachiki C, Morikawa T, Ariizumi D, Matsunaga S, Sugahara K, Aihara Y, Watanabe A, Katakura A, Kawamata T, et al. Cranial Vault Deformation and Its Association with Mandibular Deviation in Patients with Facial Asymmetry: A CT-Based Study. Diagnostics. 2025; 15(13):1702. https://doi.org/10.3390/diagnostics15131702
Chicago/Turabian StyleNishimura, Mayuko, Chie Tachiki, Taiki Morikawa, Dai Ariizumi, Satoru Matsunaga, Keisuke Sugahara, Yasuo Aihara, Akira Watanabe, Akira Katakura, Takakazu Kawamata, and et al. 2025. "Cranial Vault Deformation and Its Association with Mandibular Deviation in Patients with Facial Asymmetry: A CT-Based Study" Diagnostics 15, no. 13: 1702. https://doi.org/10.3390/diagnostics15131702
APA StyleNishimura, M., Tachiki, C., Morikawa, T., Ariizumi, D., Matsunaga, S., Sugahara, K., Aihara, Y., Watanabe, A., Katakura, A., Kawamata, T., & Nishii, Y. (2025). Cranial Vault Deformation and Its Association with Mandibular Deviation in Patients with Facial Asymmetry: A CT-Based Study. Diagnostics, 15(13), 1702. https://doi.org/10.3390/diagnostics15131702










