Retention of Asymptomatic Impacted Third Molars: Effects on Alveolar Bone at the Distal Surface of Second Molars over Time
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Ethics
2.3. Study Subjects
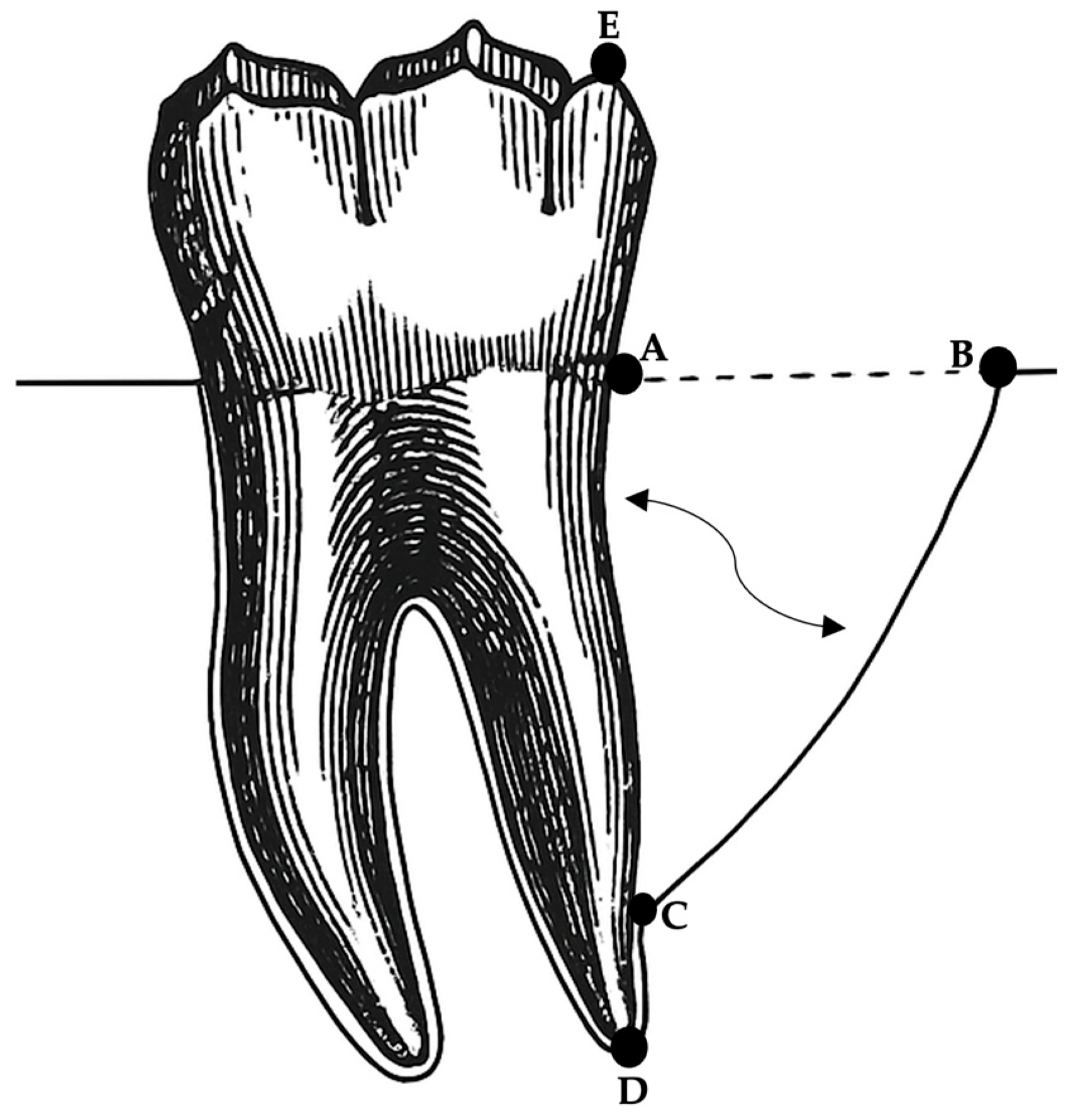
2.4. Radiographic Examination
2.5. Radiograph Standardization
- Equation one for correction factor: DC to RA (T0) ÷ DC to RA (T1) = correction factor.
- Equation two for adjusted T1 (DC to RA): DC to RA (T0) − [DC to RA (T1) × correction factor] = adjusted T1 (DC to RA)
- Equation three for adjusted T1 (CEJ to BD): CEJ to BD (T0) − [CEJ to BD (T1) × correction factor] = adjusted T1 (CEJ to BD)
- Equation four for adjusted T1 (BD to CB): BD to CB (T0) − [BD to CB (T1) × correction factor] = adjusted T1 (BD to CB).
2.6. Calibration of Radiographic Analysis
2.7. Data Management and Statistical Analysis
3. Results
4. Discussion
4.1. Study Limitations
4.2. Clinical Implications
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- McArdle, L.W.; Renton, T. The effects of NICE guidelines on the management of third molar teeth. Br. Dent. J. 2012, 213, E8. [Google Scholar] [CrossRef] [PubMed]
- Anjrini, A.A.; Kruger, E.; Tennant, M. Cost effectiveness modelling of a “watchful monitoring strategy” for impacted third molars vs prophylactic removal under GA: An Australian perspective. Br. Dent. J. 2015, 219, 19–23. [Google Scholar] [CrossRef]
- Carter, K.; Worthington, S. Predictors of third molar impaction. J. Dent. Res. 2016, 95, 267–276. [Google Scholar] [CrossRef] [PubMed]
- McArdle, L.W.; Andiappan, M.; Khan, I.; Jones, J.; McDonald, F. Diseases associated with mandibular third molar teeth. Br. Dent. J. 2018, 224, 434–440. [Google Scholar] [CrossRef] [PubMed]
- National Institute for Health and Care Excellence (NICE). Guidance on the Extraction of Wisdom Teeth. TA1. 2000. Available online: https://www.nice.org.uk/guidance/ta1 (accessed on 26 January 2022).
- Faculty of Dental Surgery. Parameters of Care for Patients Undergoing Mandibular Third Molar Surgery; The Royal College of Surgeons of England: London, UK, 2021; Available online: https://www.rcseng.ac.uk/-/media/files/rcs/fds/guidelines/3rd-molar-guidelines--april-2021.pdf (accessed on 26 January 2022).
- Ghaeminia, H.; Nienhuijs, M.E.; Toedtling, V.; Perry, J.; Tummers, M.; Hoppenreijs, T.J.; van der Sanden, W.J.; Mettes, T.G. Surgical removal versus retention for the management of asymptomatic disease-free impacted wisdom teeth. Cochrane Database Syst. Rev. 2020, 5, CD003879. [Google Scholar] [CrossRef] [PubMed]
- Schei, O.; Waerhaug, J.; Lovdal, A.; Arno, A. Alveolar bone loss as related to oral hygiene and age. J. Periodontol. 1959, 30, 7–16. [Google Scholar] [CrossRef]
- Bjorn, H.; Halling, A.; Thyberg, H. Radiographic assessment of marginal bone loss. Odontol. Revy 1969, 20, 165–179. [Google Scholar] [PubMed]
- Nibali, L.; Pometti, D.; Tu, Y.K.; Donos, N. Clinical and radiographic outcomes following non-surgical therapy of periodontal infrabony defects: A retrospective study. J. Clin. Periodontol. 2011, 38, 50–57. [Google Scholar] [CrossRef]
- Steffensen, B.; Webert, H.P. Relationship between the radiographic periodontal defect angle and healing after treatment. J. Periodontol. 1989, 60, 248–254. [Google Scholar] [CrossRef]
- Tonetti, M.S.; Pini Prato, G.; Williams, R.C.; Cortellini, P. Periodontal regeneration of human infrabony defects. III. Diagnostic strategies to detect bone gain. J. Periodontol. 1993, 64, 269–277. [Google Scholar] [CrossRef]
- Tsitoura, E.; Tucker, R.; Suvan, J.; Laurell, L.; Cortellini, P.; Tonetti, M. Baseline radiographic defect angle of the intrabony defect as a prognostic indicator in regenerative periodontal surgery with enamel matrix derivative. J. Clin. Periodontol. 2004, 31, 643–647. [Google Scholar] [CrossRef]
- Liñares, A.; Cortellini, P.; Lang, N.P.; Suvan, J.; Tonetti, M.S.; European Research Group on Periodontology (ErgoPerio). Guided tissue regeneration/deproteinized bovine bone mineral or papilla preservation flaps alone for treatment of intrabony defects. II: Radiographic predictors and outcomes. J. Clin. Periodontol. 2006, 33, 351–358. [Google Scholar] [CrossRef]
- Nunn, M.E.; Fish, M.D.; Garcia, R.I.; Kaye, E.K.; Figueroa, R.; Gohel, A.; Ito, M.; Lee, H.J.; Williams, D.E.; Miyamoto, T. Retained asymptomatic third molars and risk for second molar pathology. J. Dent. Res. 2013, 92, 1095–1099. [Google Scholar] [CrossRef] [PubMed]
- Krausz, A.A.; Machtei, E.E.; Peled, M. Effects of lower third molar extraction on attachment level and alveolar bone height of the adjacent second molar. Int. J. Oral Maxillofac. Surg. 2005, 34, 756–760. [Google Scholar] [CrossRef] [PubMed]
- Kugelberg, C.F.; Ahlström, U.; Ericson, S.; Hugoson, A. Periodontal healing after impacted lower third molar surgery. A retrospective study. Int. J. Oral Surg. 1985, 14, 29–40. [Google Scholar] [CrossRef]
- Helmi, M.F.; Huang, H.; Goodson, J.M.; Hasturk, H.; Tavares, M.; Natto, Z.S. Prevalence of periodontitis and alveolar bone loss in a patient population at Harvard School of Dental Medicine. BMC Oral Health 2019, 19, 254. [Google Scholar] [CrossRef] [PubMed]
- Wong, B.K.; Leichter, J.W.; Chandler, N.P.; Cullinan, M.P.; Holborow, D.W. Radiographic study of ethnic variation in alveolar bone height among New Zealand dental students. J. Periodontol. 2007, 78, 1070–1074. [Google Scholar] [CrossRef]
- Bergström, J.; Floderus-Myrhed, B. Cotwin control study of the relationship between smoking and some periodontal disease factors. Community Dent. Oral Epidemiol. 1983, 11, 113–116. [Google Scholar] [CrossRef]
- Bergström, J.; Eliasson, S. Cigarette smoking and alveolar bone height in subjects with a high standard of oral hygiene. J. Clin. Periodontol. 1987, 14, 466–469. [Google Scholar] [CrossRef]
- Kugelberg, C.F.; Ahlström, U.; Ericson, S.; Hugoson, A.; Kvint, S. Periodontal healing after impacted lower third molar surgery in adolescents and adults. A prospective study. Int. J. Oral Maxillofac. Surg. 1991, 20, 18–24. [Google Scholar] [CrossRef]
- Matzen, L.H.; Schropp, L.; Spin-Neto, R.; Wenzel, A. Radiographic signs of pathology determining removal of an impacted mandibular third molar assessed in a panoramic image or CBCT. Dentomaxillofacial Radiol. 2016, 46, 20160330. [Google Scholar] [CrossRef] [PubMed]
- Dias, M.J.; Franco, A.; Junqueira, J.L.; Fayad, F.T.; Pereira, P.H.; Oenning, A.C. Marginal bone loss in the second molar related to impacted mandibular third molars: Comparison between panoramic images and cone beam computed tomography. Med. Oral. Patol. Oral. Cir. Bucal. 2020, 25, e395–e402. [Google Scholar] [CrossRef] [PubMed]
- Yesiltepe, S.; Kılcı, G. Evaluation of the relationship between the position and impaction level of the impacted maxillary third molar teeth and marginal bone loss, caries, and resorption findings of the second molar teeth with CBCT scans. Oral. Radiol. 2022, 38, 269–277. [Google Scholar] [CrossRef] [PubMed]



| Measurement | p-Values | Decision |
|---|---|---|
| CEJ to BD at T0 and adjusted T1 | 0.377 | Retain the null hypothesis. |
| BD to CB at T0 and adjusted T1 | 0.275 | Retain the null hypothesis. |
| Intrabony defect angle at T0 and T1 | 0.366 | Retain the null hypothesis. |
| Measurement | Test | Variable | T0 Significance | T1 Significance | Decision |
|---|---|---|---|---|---|
| CEJ to BD | Mann–Whitney U Test | Gender | 0.022 | 0.027 | Significant |
| Mann–Whitney U Test | Systemic Health | 0.784 | 0.994 | Not significant | |
| Chi-Square Test | Ethnicity | 0.192 | 0.376 | Not significant | |
| Chi-Square Test | Smoking Status | 0.841 | 0.423 | Not significant | |
| Chi-Square | ITMs Angulation | 0.408 | 0.292 | Not significant | |
| BD to CB | Mann–Whitney U Test | Gender | 0.347 | 0.342 | Not significant |
| Mann–Whitney U Test | Systemic Health | 0.950 | 0.688 | Not significant | |
| Chi-Square Test | Ethnicity | 0.175 | 0.218 | Not significant | |
| Chi-Square Test | Smoking Status | 0.313 | 0.294 | Not significant | |
| Chi-Square Test | ITMs Angulation | 0.995 | 0.992 | Not significant | |
| Intrabony Defect Angle | Mann–Whitney U Test | Gender | 0.048 | 0.292 | Significant at T0 only |
| Mann–Whitney U Test | Systemic Health | 0.539 | 0.684 | Not significant | |
| Chi-Square Test | Ethnicity | 0.391 | 0.443 | Not significant | |
| Chi-Square Test | Smoking Status | 0.157 | 0.264 | Not significant | |
| Chi-Square Test | ITMs Angulation | 0.963 | 0.962 | Not significant |
| Correlation of the Linear Measurements with Age | R-Value (R) | R-Squared (R2) | Sig. |
|---|---|---|---|
| CEJ to BD at T0 and adjusted T1 | 0.056 | 0.003 | 0.413 |
| BD to CB at T0 and adjusted T1 | 0.012 | 0.000 | 0.858 |
| Intrabony defect angle at T0 at T1 | 0.146 | 0.021 | 0.047 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alfurhud, A.A.; Alouthah, H. Retention of Asymptomatic Impacted Third Molars: Effects on Alveolar Bone at the Distal Surface of Second Molars over Time. Diagnostics 2025, 15, 1643. https://doi.org/10.3390/diagnostics15131643
Alfurhud AA, Alouthah H. Retention of Asymptomatic Impacted Third Molars: Effects on Alveolar Bone at the Distal Surface of Second Molars over Time. Diagnostics. 2025; 15(13):1643. https://doi.org/10.3390/diagnostics15131643
Chicago/Turabian StyleAlfurhud, Ahmed Ata, and Hesham Alouthah. 2025. "Retention of Asymptomatic Impacted Third Molars: Effects on Alveolar Bone at the Distal Surface of Second Molars over Time" Diagnostics 15, no. 13: 1643. https://doi.org/10.3390/diagnostics15131643
APA StyleAlfurhud, A. A., & Alouthah, H. (2025). Retention of Asymptomatic Impacted Third Molars: Effects on Alveolar Bone at the Distal Surface of Second Molars over Time. Diagnostics, 15(13), 1643. https://doi.org/10.3390/diagnostics15131643






