The Prognostic Significance of the Pan-Immune-Inflammation Value in Patients with Heart Failure with Reduced Ejection Fraction
Abstract
1. Introduction
2. Material and Methods
2.1. Study Design, Setting and Participants
2.2. Collection of Cardiac and Other Data
2.3. Statistical Analysis
3. Results
| Mortality | ||||
|---|---|---|---|---|
| Total (n = 419) | Yes (n = 96) | No (n = 323) | p | |
| Age, years | 55.09 ± 13.54 | 56.10 ± 12.48 | 54.79 ± 13.84 | 0.403 † |
| Sex | ||||
| Female | 89 (21.24%) | 20 (20.83%) | 69 (21.36%) | 1.000 # |
| Male | 330 (78.76%) | 76 (79.17%) | 254 (78.64%) | |
| Body mass index, kg/m2 | 27.05 ± 3.83 | 25.48 ± 3.42 | 27.51 ± 3.82 | <0.001 † |
| Smoking status | ||||
| Non-smoker | 279 (66.59%) | 69 (71.88%) | 210 (65.02%) | 0.445 # |
| Ex-smoker | 49 (11.69%) | 10 (10.42%) | 39 (12.07%) | |
| Active smoker | 91 (21.72%) | 17 (17.71%) | 74 (22.91%) | |
| Diabetes mellitus | 147 (35.08%) | 34 (35.42%) | 113 (34.98%) | 0.938 # |
| Hypertension | 173 (41.29%) | 27 (28.13%) | 146 (45.20%) | 0.003 # |
| Atrial fibrillation | 271 (64.68%) | 48 (50.00%) | 223 (69.04%) | 0.001 # |
| Ischemic cardiomyopathy | 206 (49.16%) | 46 (47.92%) | 160 (49.54%) | 0.781 # |
| Cardiac device | 314 (74.94%) | 75 (78.13%) | 239 (73.99%) | 0.493 # |
| ICD | 305 (72.79%) | 74 (77.08%) | 231 (71.52%) | 0.466 # |
| CRT | 9 (2.15%) | 1 (1.04%) | 8 (2.48%) | |
| End-diastolic diameter, mm | 65.13 ± 10.21 | 66.84 ± 11.74 | 64.62 ± 9.67 | 0.061 † |
| End-systolic diameter, mm | 54.87 ± 10.02 | 57.27 ± 10.31 | 54.15 ± 9.83 | 0.007 † |
| LVEF | 24.30 ± 6.60 | 21.42 ± 6.32 | 25.15 ± 6.45 | <0.001 † |
| NYHA classification | ||||
| Class I | 36 (8.59%) | 2 (2.08%) | 34 (10.53%) | <0.001 # |
| Class II | 250 (59.67%) | 44 (45.83%) | 206 (63.78%) | |
| Class III | 120 (28.64%) | 41 (42.71%) | 79 (24.46%) | |
| Class IV | 13 (3.10%) | 9 (9.38%) | 4 (1.24%) | |
| Device therapy | ||||
| None | 135 (61.09%) | 21 (46.67%) | 114 (64.77%) | 0.040 # |
| Therapy | 86 (38.91%) | 24 (53.33%) | 62 (35.23%) | |
| Medications | ||||
| MRA | 206 (49.16%) | 45 (46.88%) | 161 (49.85%) | 0.609 # |
| ACE inhibitors/ARB | 355 (84.73%) | 75 (78.13%) | 280 (86.69%) | 0.059 # |
| Beta blockers | 414 (98.81%) | 95 (98.96%) | 319 (98.76%) | 1.000 § |
| Digoxin | 95 (22.67%) | 25 (26.04%) | 70 (21.67%) | 0.369 # |
| Follow-up time, months | 29 (17–71) | 20 (11–64.5) | 38 (18–74) | 0.001 ‡ |
| NT-proBNP | 1126 (435–2310) | 1920.5 (1130–3373) | 967 (362–2037) | <0.001 ‡ |
| logNT-proBNP | 2.97 ± 0.56 | 3.24 ± 0.46 | 2.89 ± 0.57 | <0.001 † |
| Sodium, mEq/L | 136.97 ± 4.50 | 134.69 ± 5.64 | 137.65 ± 3.85 | <0.001 † |
| Glucose, mg/dL | 105 (90–131) | 102 (92–128.5) | 106 (89–131) | 0.543 ‡ |
| Urea, mg/dL | 34 (24–47) | 36 (24–54.5) | 34 (24–46) | 0.375 ‡ |
| Creatinine, mg/dL | 1.03 (0.86–1.23) | 1.04 (0.85–1.26) | 1.02 (0.86–1.23) | 0.544 ‡ |
| eGFR, mL/min/1.73 m2 | 79.85 ± 25.33 | 77.74 ± 26.76 | 80.48 ± 24.89 | 0.353 † |
| Albumin, g/dL | 3.81 ± 0.43 | 3.69 ± 0.44 | 3.85 ± 0.42 | 0.002 † |
| LDL-C, mg/dL | 100.72 ± 35.20 | 92.91 ± 32.35 | 103.04 ± 35.72 | 0.013 † |
| Triglyceride, mg/dL | 116 (89–158) | 102 (76–138.5) | 126 (92–178) | <0.001 ‡ |
| HDL-C, mg/dL | 37 (30–43) | 36 (26–41.5) | 38 (31–44) | 0.054 ‡ |
| Total cholesterol, mg/dL | 167.18 ± 45.06 | 153.61 ± 43.50 | 171.21 ± 44.79 | 0.001 † |
| Hemoglobin, g/dL | 13.38 ± 2.05 | 12.97 ± 1.94 | 13.51 ± 2.07 | 0.024 † |
| Neutrophil (×103) | 5.13 (4.00–6.30) | 5.30 (3.80–6.46) | 5.10 (4.06–6.27) | 0.600 ‡ |
| Lymphocyte (×103) | 1.95 ± 0.80 | 1.62 ± 0.73 | 2.05 ± 0.80 | <0.001 † |
| Monocyte (×103) | 0.65 ± 0.25 | 0.65 ± 0.24 | 0.65 ± 0.26 | 0.868 † |
| Platelet (×103) | 237.30 ± 74.16 | 233.49 ± 75.28 | 238.43 ± 73.91 | 0.567 † |
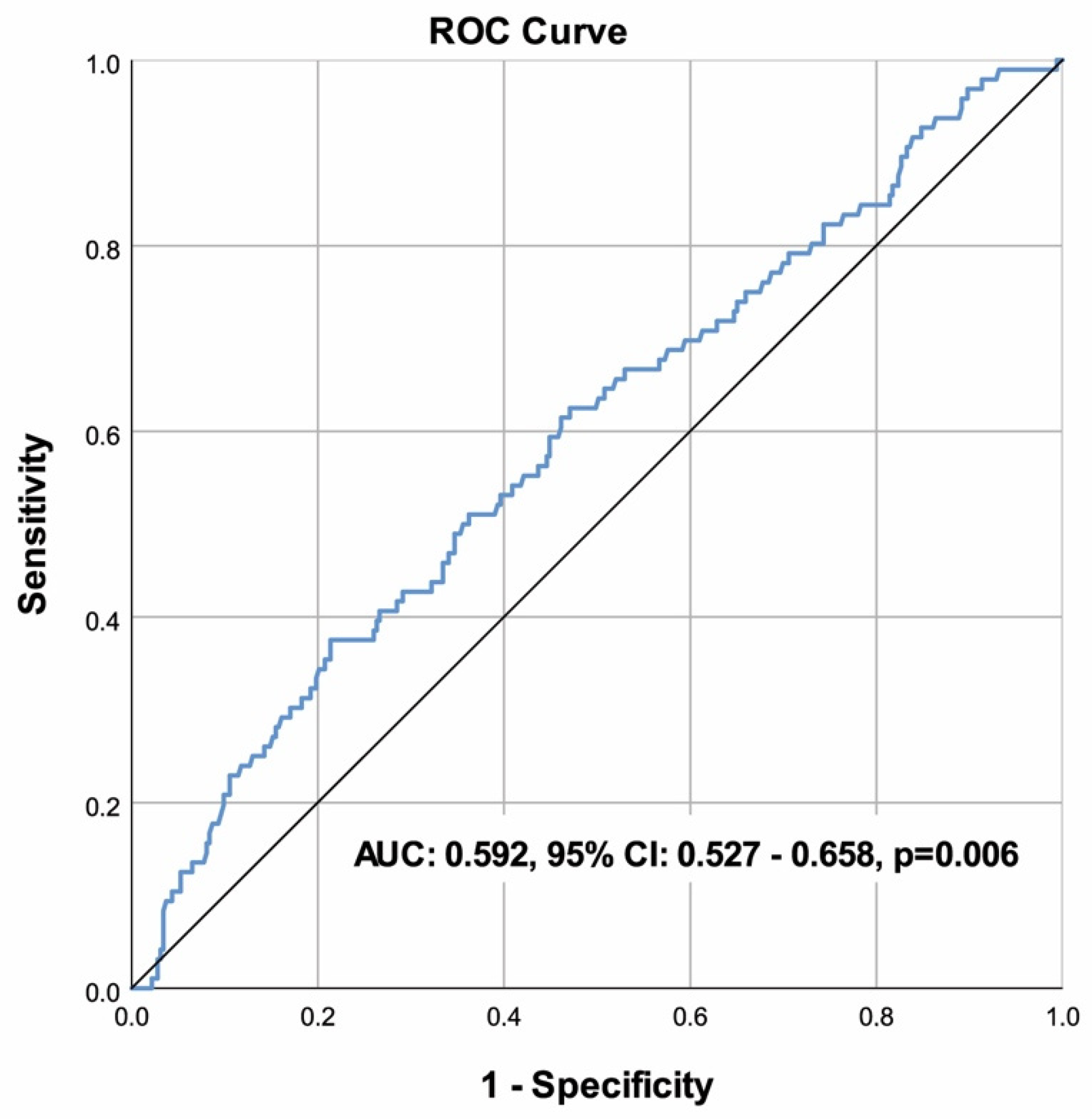
| PIV (×106) | 345.09 (227.50–697.92) | 441.97 (251.99–911.50) | 334.80 (219.37–632.46) | 0.006 ‡ |
| Cut-off | >696 |
| Sensitivity | 37.50% |
| Specificity | 78.64% |
| Accuracy | 69.21% |
| PPV | 34.29% |
| NPV | 80.89% |
| AUC (95% CI) | 0.592 (0.527–0.658) |
| p | 0.006 |
4. Discussion
Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| PIV | Pan-immune-inflammation value |
| HFrEF | Heart failure with reduced ejection fraction |
| NYHA | New York Heart Association |
| LVEF | Left ventricular ejection fraction |
| BMI | Body mass index |
| ICD | Implantable cardioverter defibrillator |
| CRT | Cardiac resynchronization therapy |
| NT-proBNP | N-terminal pro b-type natriuretic peptide |
| LDL-C | Low-density lipoprotein cholesterol |
| HDL-C | High-density lipoprotein cholesterol |
| SD | Standard deviation |
| ROC | Receiver operating characteristic |
| TNF-α | Tumor necrosis factor-alpha |
References
- Braunwald, E. Braunwald’s Heart Disease; WB Saunders Elsevier: Philadelphia, PA, USA, 2012. [Google Scholar]
- Alcaide, P.; Kallikourdis, M.; Emig, R.; Prabhu, S.D. Myocardial Inflammation in Heart Failure with Reduced and Preserved Ejection Fraction. Circ. Res. 2024, 134, 1752–1766. [Google Scholar] [CrossRef] [PubMed]
- Yancy, C.W.; Jessup, M.; Bozkurt, B.; Butler, J.; Casey, D.E., Jr.; Drazner, M.H.; Fonarow, G.C.; Geraci, S.A.; Horwich, T.; Januzzi, J.L.; et al. 2013 ACCF/AHA guideline for the management of heart failure: A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J. Am. Coll. Cardiol. 2013, 62, e147–e239. [Google Scholar] [CrossRef] [PubMed]
- McDonagh, T.A.; Metra, M.; Adamo, M.; Gardner, R.S.; Baumbach, A.; Böhm, M.; Burri, H.; Butler, J.; Čelutkienė, J.; Chioncel, O.; et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: Developed by the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur. Heart J. 2021, 42, 3599–3726. [Google Scholar]
- Tromp, J.; Westenbrink, B.D.; Ouwerkerk, W.; van Veldhuisen, D.J.; Samani, N.J.; Ponikowski, P.; Metra, M.; Anker, S.D.; Cleland, J.G.; Dickstein, K.; et al. Identifying Pathophysiological Mechanisms in Heart Failure with Reduced Versus Preserved Ejection Fraction. J. Am. Coll. Cardiol. 2018, 72, 1081–1090. [Google Scholar] [CrossRef] [PubMed]
- Soehnlein, O.; Steffens, S.; Hidalgo, A.; Weber, C. Neutrophils as protagonists and targets in chronic inflammation. Nat. Rev. Immunol. 2017, 17, 248–261. [Google Scholar] [CrossRef]
- Apostolakis, S.; Lip, G.Y.; Shantsila, E. Monocytes in heart failure: Relationship to a deteriorating immune overreaction or a desperate attempt for tissue repair? Cardiovasc. Res. 2010, 85, 649–660. [Google Scholar] [CrossRef]
- Vulesevic, B.; Sirois, M.G.; Allen, B.G.; de Denus, S.; White, M. Subclinical Inflammation in Heart Failure: A Neutrophil Perspective. Can. J. Cardiol. 2018, 34, 717–725. [Google Scholar] [CrossRef]
- Tang, Y.; Zeng, X.; Feng, Y.; Chen, Q.; Liu, Z.; Luo, H.; Zha, L.; Yu, Z. Association of Systemic Immune-Inflammation Index with Short-Term Mortality of Congestive Heart Failure: A Retrospective Cohort Study. Front. Cardiovasc. Med. 2021, 8, 753133. [Google Scholar] [CrossRef]
- Zhang, F.; Li, L.; Wu, X.; Wen, Y.; Zhan, X.; Peng, F.; Wang, X.; Zhou, Q.; Feng, X. Pan-immune-inflammation value is associated with poor prognosis in patients undergoing peritoneal dialysis. Ren. Fail. 2023, 45, 2158103. [Google Scholar] [CrossRef]
- Murat, B.; Murat, S.; Ozgeyik, M.; Bilgin, M. Comparison of pan-immune-inflammation value with other inflammation markers of long-term survival after ST-segment elevation myocardial infarction. Eur. J. Clin. Investig. 2023, 53, e13872. [Google Scholar] [CrossRef]
- Pérez-Martelo, M.; González-García, A.; Vidal-Ínsua, Y.; Blanco-Freire, C.; Brozos-Vázquez, E.M.; Abdulkader-Nallib, I.; Álvarez-Fernández, J.; Lázare-Iglesias, H.; García-Martínez, C.; Betancor, Y.Z.; et al. Clinical significance of baseline Pan-Immune-Inflammation Value and its dynamics in metastatic colorectal cancer patients under first-line chemotherapy. Sci. Rep. 2022, 12, 6893. [Google Scholar] [CrossRef] [PubMed]
- Fucà, G.; Beninato, T.; Bini, M.; Mazzeo, L.; Di Guardo, L.; Cimminiello, C.; Randon, G.; Apollonio, G.; Bisogno, I.; Del Vecchio, M.; et al. The Pan-Immune-Inflammation Value in Patients with Metastatic Melanoma Receiving First-Line Therapy. Target Oncol. 2021, 16, 529–536. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Hong, X.; Chen, G.; Xue, J.; Huang, J.; Wang, F.; Ali, W.; Li, J.; Zhang, L. The Pan-Immune-Inflammation Value predicts the survival of patients with anaplastic lymphoma kinase-positive non-small cell lung cancer treated with first-line ALK inhibitor. Transl. Oncol. 2022, 17, 101338. [Google Scholar] [CrossRef]
- Lee, L.E.; Ahn, S.S.; Pyo, J.Y.; Song, J.J.; Park, Y.B.; Lee, S.W. Pan-immune-inflammation value at diagnosis independently predicts all-cause mortality in patients with antineutrophil cytoplasmic antibody-associated vasculitis. Clin. Exp. Rheumatol. 2021, 39 (Suppl. 129), 88–93. [Google Scholar] [CrossRef]
- Gambichler, T.; Hessam, S.; Cramer, P.; Abu Rached, N.; Bechara, F.G. Complete blood collection-based systemic inflammation biomarkers for patients with hidradenitis suppurativa. J. Eur. Acad. Dermatol. Venereol. 2022, 36, 1593–1596. [Google Scholar] [CrossRef]
- Murat, B.; Murat, S.; Altınbas, M.E.; Yalvac, H.E.; Durmaz, F.E.; Mert, K.U.; Cavusoglu, Y. Association of Pan Immune-Inflammation Value with Long Term Outcomes of Acute Decompensated Heart Failure. Arq. Bras. Cardiol. 2024, 121, e20230817. [Google Scholar] [CrossRef]
- Kidney Disease: Improving Global Outcomes (KDIGO). CKD-EPI Creatinine Equation. 2021. Available online: https://www.kidney.org/ckd-epi-creatinine-equation-2021 (accessed on 14 July 2024).
- Groenewegen, A.; Rutten, F.H.; Mosterd, A.; Hoes, A.W. Epidemiology of heart failure. Eur. J. Heart Fail. 2020, 22, 1342–1356. [Google Scholar] [CrossRef]
- Inan, D.; Erdogan, A.; Pay, L.; Genc, D.; Demırtola, A.I.; Yıldız, U.; Guler, A.; Tekkesin, A.I.; Karagoz, A. The prognostic impact of inflammation in patients with decompensated acute heart failure, as assessed using the pan-immune inflammation value (PIV). Scand. J. Clin. Lab. Investig. 2023, 83, 371–378. [Google Scholar] [CrossRef]
- Villacorta, H.; Masetto, A.C.; Mesquita, E.T. C-reactive protein: An inflammatory marker with prognostic value in patients with decompensated heart failure. Arq. Bras. Cardiol. 2007, 88, 585–589. [Google Scholar] [CrossRef] [PubMed]
- Elster, S.K.; Braunwald, E.; Wood, H.F. A study of C-reactive protein in the serum of patients with congestive heart failure. Am. Heart J. 1956, 51, 533–541. [Google Scholar] [CrossRef]
- Markousis-Mavrogenis, G.; Tromp, J.; Ouwerkerk, W.; Devalaraja, M.; Anker, S.D.; Cleland, J.G.; Dickstein, K.; Filippatos, G.S.; van der Harst, P.; Lang, C.C.; et al. The clinical significance of interleukin-6 in heart failure: Results from the BIOSTAT-CHF study. Eur. J. Heart Fail. 2019, 21, 965–973. [Google Scholar] [CrossRef] [PubMed]
- Wu, B.; Zhang, C.; Lin, S.; Zhang, Y.; Ding, S.; Song, W. The relationship between the pan-immune-inflammation value and long-term prognoses in patients with hypertension: National Health and Nutrition Examination Study, 1999–2018. Front. Cardiovasc. Med. 2023, 10, 1099427. [Google Scholar] [CrossRef]
- Jin, C.; Li, X.; Luo, Y.; Zhang, C.; Zuo, D. Associations between pan-immune-inflammation value and abdominal aortic calcification: A cross-sectional study. Front. Immunol. 2024, 15, 1370516. [Google Scholar] [CrossRef]
- Kaplangoray, M.; Toprak, K.; Deveci, E.; Caglayan, C.; Şahin, E. Could Pan-Immune-Inflammation Value be a Marker for the Diagnosis of Coronary Slow Flow Phenomenon? Cardiovasc. Toxicol. 2024, 24, 519–526. [Google Scholar] [CrossRef] [PubMed]
- Aukrust, P.; Gullestad, L.; Ueland, T.; Damås, J.K.; Yndestad, A. Inflammatory and anti-inflammatory cytokines in chronic heart failure: Potential therapeutic implications. Ann. Med. 2005, 37, 74–85. [Google Scholar] [CrossRef] [PubMed]
- Yildirim, N.; Unal, S.; Yalcinkaya, A.; Karahan, F.; Oztas, Y. Evaluation of the relationship between intravascular hemolysis and clinical manifestations in sickle cell disease: Decreased hemopexin during vaso-occlusive crises and increased inflammation in acute chest syndrome. Ann. Hematol. 2022, 101, 35–41. [Google Scholar] [CrossRef]
- Kucuk, A.; Topkan, E.; Ozkan, E.E.; Ozturk, D.; Pehlivan, B.; Selek, U. A high pan-immune-inflammation value before chemoradiotherapy indicates poor outcomes in patients with small-cell lung cancer. Int. J. Immunopathol. Pharmacol. 2023, 37, 3946320231187759. [Google Scholar] [CrossRef]
- Nicholson, L.B. The immune system. Essays Biochem. 2016, 60, 275–301. [Google Scholar] [CrossRef]
- Zhang, K.; Qin, W.; Zheng, Y.; Pang, J.; Zhong, N.; Fei, J.; Li, Y.; Jian, X.; Hou, X.; Hu, Z.; et al. Malnutrition Contributes to Low Lymphocyte Count in Early-Stage Coronavirus Disease-2019. Front. Nutr. 2021, 8, 739216. [Google Scholar] [CrossRef]
- Hwang, I.C.; Choi, H.M.; Yoon, Y.E.; Park, J.J.; Park, J.B.; Park, J.H.; Lee, S.P.; Kim, H.K.; Kim, Y.J.; Cho, G.Y. Body Mass Index, Muscle Mass, and All-Cause Mortality in Patients with Acute Heart Failure: The Obesity Paradox Revisited. Int. J. Heart Fail. 2022, 4, 95–109. [Google Scholar] [CrossRef]
- Brener, M.I.; Uriel, N.; Burkhoff, D. Left Ventricular Volume Reduction and Reshaping as a Treatment Option for Heart Failure. Struct. Heart 2020, 4, 264–283. [Google Scholar] [CrossRef]
- Caraballo, C.; Desai, N.R.; Mulder, H.; Alhanti, B.; Wilson, F.P.; Fiuzat, M.; Felker, G.M.; Piña, I.L.; O’Connor, C.M.; Lindenfeld, J.; et al. Clinical Implications of the New York Heart Association Classification. J. Am. Heart Assoc. 2019, 8, e014240. [Google Scholar] [CrossRef] [PubMed]
- Brunner-La Rocca, H.P.; Sanders-van Wijk, S. Natriuretic Peptides in Chronic Heart Failure. Card. Fail. Rev. 2019, 5, 44–49. [Google Scholar] [CrossRef]
- Xu, Y.; Shi, Y.; Zhu, Z.; Cui, C.; Li, B.; Chen, F.; Li, D.; Chen, S.; Guo, Y. Prognosis of patients with heart failure and reduced ejection fraction in China. Exp. Ther. Med. 2013, 6, 1437–1442. [Google Scholar] [CrossRef]
- Lundorff, I.J.; Sengeløv, M.; Godsk Jørgensen, P.; Pedersen, S.; Modin, D.; Eske Bruun, N.; Fritz-Hansen, T.; Skov Jensen, J.; Biering-Sørensen, T. Echocardiographic Predictors of Mortality in Women with Heart Failure with Reduced Ejection Fraction. Circ. Cardiovasc. Imaging 2018, 11, e008031. [Google Scholar] [CrossRef]
- Kontogeorgos, S.; Thunström, E.; Johansson, M.C.; Fu, M. Heart failure with preserved ejection fraction has a better long-term prognosis than heart failure with reduced ejection fraction in old patients in a 5-year follow-up retrospective study. Int. J. Cardiol. 2017, 232, 86–92. [Google Scholar] [CrossRef]
- Kerzner, R.; Gage, B.F.; Freedland, K.E.; Rich, M.W. Predictors of mortality in younger and older patients with heart failure and preserved or reduced left ventricular ejection fraction. Am. Heart J. 2003, 146, 286–290. [Google Scholar] [CrossRef]
- Liu, X.; Yu, H.; Pei, J.; Chu, J.; Pu, J.; Zhang, S. Clinical characteristics and long-term prognosis in patients with chronic heart failure and reduced ejection fraction in China. Heart Lung Circ. 2014, 23, 818–826. [Google Scholar] [CrossRef] [PubMed]
- Mendez Fernandez, A.B.; Ferrero-Gregori, A.; Garcia-Osuna, A.; Mirabet-Perez, S.; Pirla-Buxo, M.J.; Cinca-Cuscullola, J.; Ordonez-Llanos, J.; Roig Minguell, E. Growth differentiation factor 15 as mortality predictor in heart failure patients with non-reduced ejection fraction. ESC Heart Fail. 2020, 7, 2223–2229. [Google Scholar] [CrossRef]
- O’Connor, C.; Fiuzat, M.; Mulder, H.; Coles, A.; Ahmad, T.; Ezekowitz, J.A.; Adams, K.F.; Piña, I.L.; Anstrom, K.J.; Cooper, L.S.; et al. Clinical factors related to morbidity and mortality in high-risk heart failure patients: The GUIDE-IT predictive model and risk score. Eur. J. Heart Fail. 2019, 21, 770–778. [Google Scholar] [CrossRef]
- Pérez de Isla, L.; Zamorano, J.; Hernández, N.; Contreras, L.; Rodrigo, J.L.; Almería, C.; Aubele, A.L.; Mataix, L.; Macaya, C. Prognostic factors and predictors of in-hospital mortality of patients with heart failure with preserved left ventricular ejection fraction. J. Cardiovasc. Med. 2008, 9, 1011–1015. [Google Scholar] [CrossRef] [PubMed]
- Koller, L.; Kleber, M.E.; Brandenburg, V.M.; Goliasch, G.; Richter, B.; Sulzgruber, P.; Scharnagl, H.; Silbernagel, G.; Grammer, T.B.; Delgado, G.; et al. Fibroblast Growth Factor 23 Is an Independent and Specific Predictor of Mortality in Patients with Heart Failure and Reduced Ejection Fraction. Circ. Heart Fail. 2015, 8, 1059–1067. [Google Scholar] [CrossRef] [PubMed]
- Tay, W.T.; Teng, T.K.; Simon, O.; Ouwerkerk, W.; Tromp, J.; Doughty, R.N.; Richards, A.M.; Hung, C.L.; Qin, Y.; Aung, T.; et al. Readmissions, Death and Its Associated Predictors in Heart Failure with Preserved Versus Reduced Ejection Fraction. J. Am. Heart Assoc. 2021, 10, e021414. [Google Scholar] [CrossRef]
- Wu, C.K.; Lee, J.K.; Chiang, F.T.; Lin, L.Y.; Lin, J.W.; Hwang, J.J.; Tseng, C.D.; Tsai, C.T. Prognostic factors of heart failure with preserved ejection fraction: A 12-year prospective cohort follow-up study. Int. J. Cardiol. 2014, 171, 331–337. [Google Scholar] [CrossRef] [PubMed]
| β Coefficient | Standard Error | p | Exp(β) | 95% CI for Exp(β) | ||
|---|---|---|---|---|---|---|
| Body mass index, kg/m2 | −0.156 | 0.042 | <0.001 | 0.856 | 0.788 | 0.930 |
| End-systolic diameter, mm | 0.029 | 0.014 | 0.035 | 1.029 | 1.002 | 1.057 |
| LVEF | −0.078 | 0.022 | <0.001 | 0.925 | 0.886 | 0.966 |
| NYHA classification, class III and IV | 0.667 | 0.282 | 0.018 | 1.948 | 1.121 | 3.385 |
| log NT-proBNP | 0.788 | 0.318 | 0.013 | 2.198 | 1.179 | 4.097 |
| Sodium, mEq/L | −0.109 | 0.028 | <0.001 | 0.896 | 0.848 | 0.947 |
| Lymphocyte (×103) | −0.464 | 0.191 | 0.015 | 0.629 | 0.432 | 0.915 |
| Constant | 16.199 | 4.261 | <0.001 | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dervis, E.; Yakut, I.; Inan, D. The Prognostic Significance of the Pan-Immune-Inflammation Value in Patients with Heart Failure with Reduced Ejection Fraction. Diagnostics 2025, 15, 1617. https://doi.org/10.3390/diagnostics15131617
Dervis E, Yakut I, Inan D. The Prognostic Significance of the Pan-Immune-Inflammation Value in Patients with Heart Failure with Reduced Ejection Fraction. Diagnostics. 2025; 15(13):1617. https://doi.org/10.3390/diagnostics15131617
Chicago/Turabian StyleDervis, Emir, Idris Yakut, and Duygu Inan. 2025. "The Prognostic Significance of the Pan-Immune-Inflammation Value in Patients with Heart Failure with Reduced Ejection Fraction" Diagnostics 15, no. 13: 1617. https://doi.org/10.3390/diagnostics15131617
APA StyleDervis, E., Yakut, I., & Inan, D. (2025). The Prognostic Significance of the Pan-Immune-Inflammation Value in Patients with Heart Failure with Reduced Ejection Fraction. Diagnostics, 15(13), 1617. https://doi.org/10.3390/diagnostics15131617






