Analysis of Factors Influencing Corrective Power of Akin’s Osteotomy in 2D Plain Radiographs: What to Consider to Obtain Good Correction in Hallux Valgus Surgery
Abstract
1. Introduction
2. Material and Methods
2.1. Statistical Report
2.2. Ethics Statement
3. Results
4. Discussion
Limitations
5. Conclusions
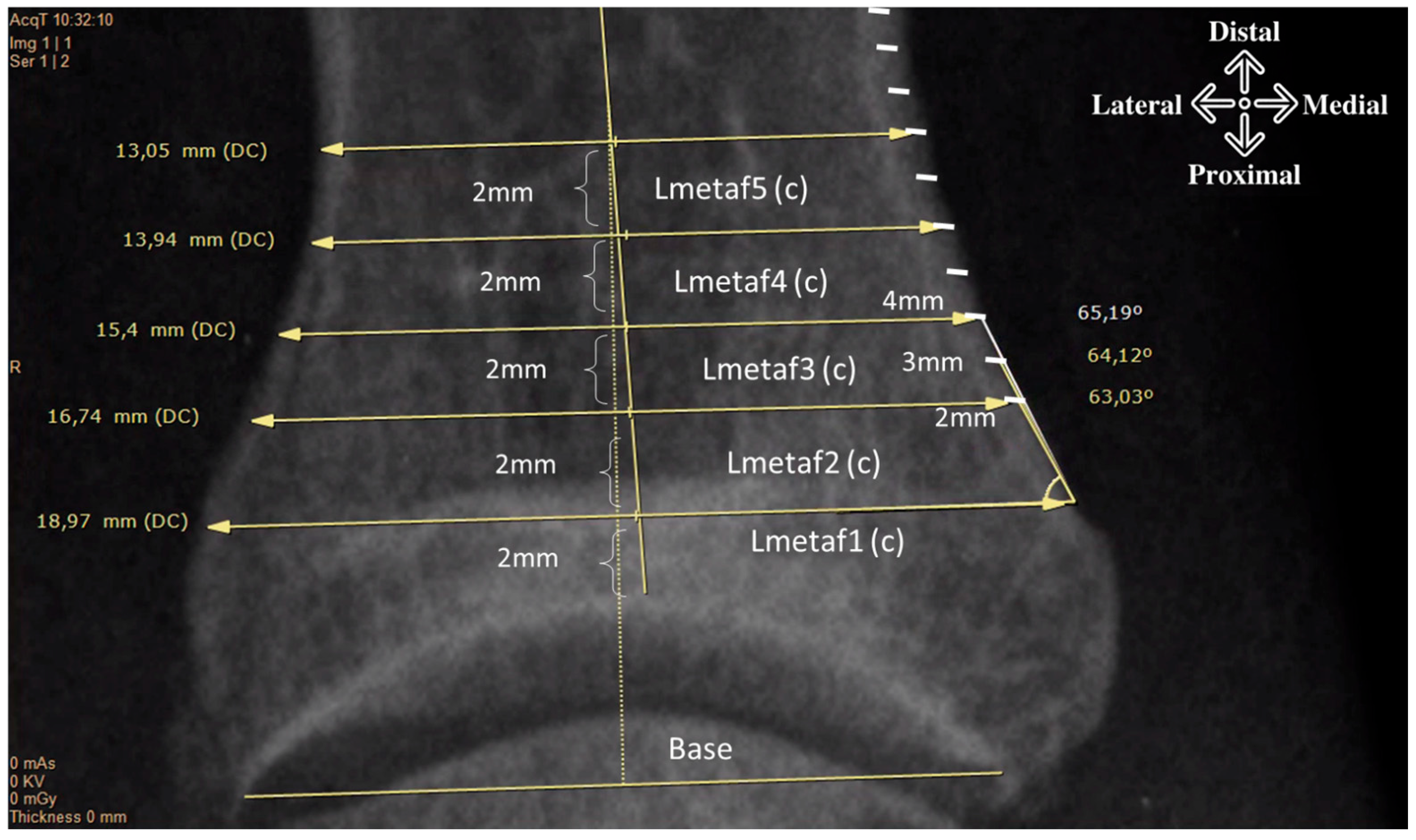
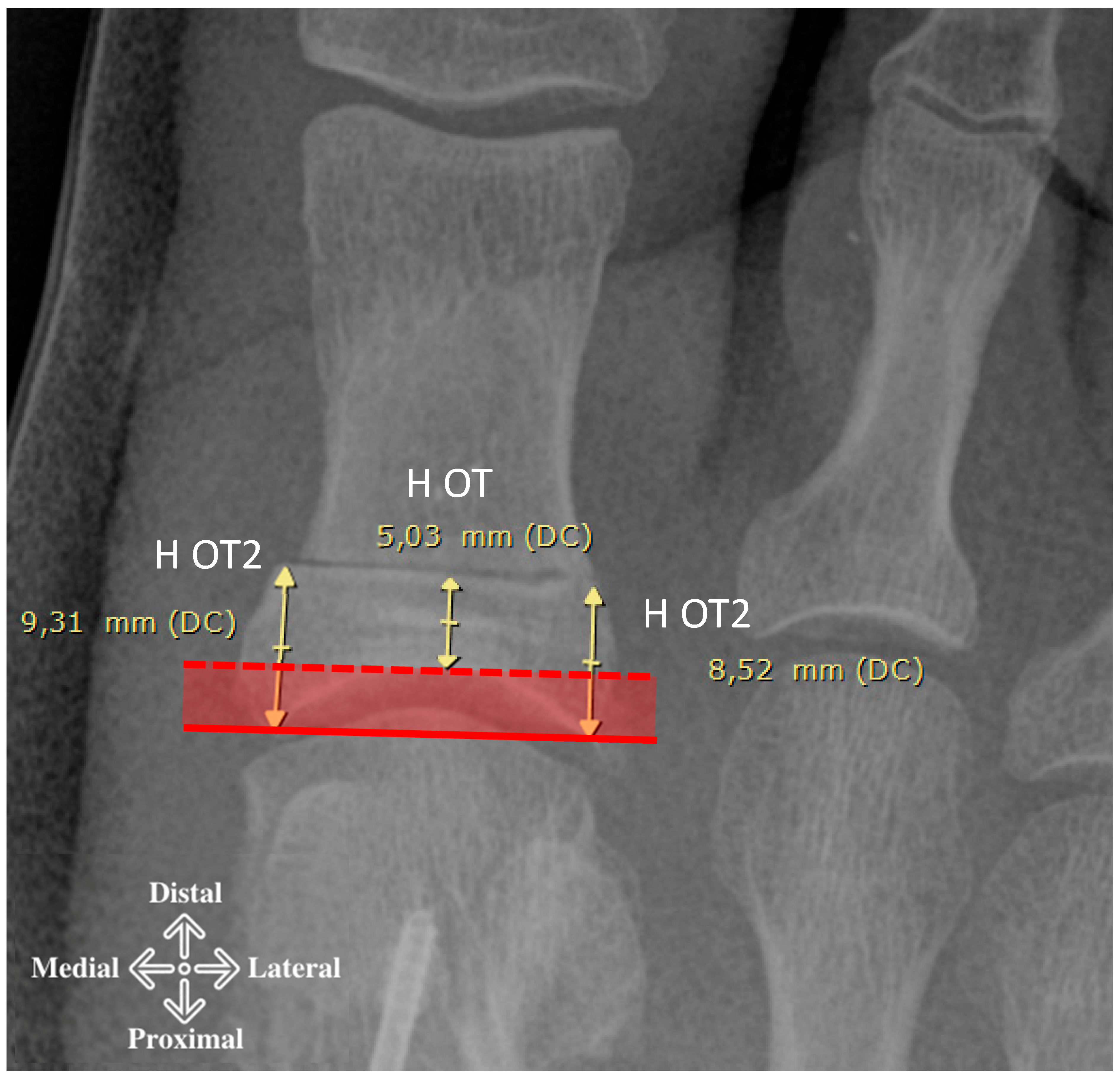
- The presented study provides an approximation of the corrective power of Akin’s osteotomy. This power depends on several factors including the width of the base, the inclination of the medial cortical, the height at which the osteotomy is performed and the width of the base of the subtraction wedge (Figure 5).
- The data suggest not performing the osteotomy within 10 mm of the joint line to avoid intra-articular extension.
- Greater angle correction is achieved if the cut is more diaphyseal versus metaphyseal and if the subtraction wedge inclination has a less acute versus more acute angle.
- The DASA and IPOA calculated on 2D plain radiographs would appear to be unreliable factors for planning purposes.
- Finally, the greater the width of the subtraction wedge, the greater the correction. It is important to consider all factors together, and this explains why different magnitudes of correction can be achieved, as observed in this study.
- Between 5.9 and 9.3 degrees with 2 mm base wedges.
- Between 9.0 and 14 degrees with 3 mm wedges.
- Between 12.1 and 18.4 degrees with 4 mm wedges, depending on the starting position of the osteotomy (metaphyseal or diaphyseal area) and the inclination of the medial cortical wall.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Akin, O. The Treatment of Hallux Valgus: A New Operative Procedure and Its Results. Med. Sentin. 1925, 33, 678–679. [Google Scholar]
- Bonk, J.H. Chapter 8. Phalangeal Osteotomy for Hallux Valgus. In Hallux Valgus and Forefoot Surgery, Medicine; Hetherington, V., Ed.; Churchill Livingstone: New York, NY, USA, 1994; pp. 137–146. [Google Scholar]
- Brahms, M. Hallux valgus: The Akin procedure. Clin. Orthop. Relat. Res. 1981, 157, 47–49. [Google Scholar] [CrossRef]
- Makwana, N.K. Osteotomy of the hallux proximal phalanx. Foot Ankle Clin. 2001, 6, 455–471. [Google Scholar] [CrossRef] [PubMed]
- Cohen, M.M. The oblique proximal phalangeal osteotomy in the correction of hallux valgus. J. Foot Ankle Surg. 2003, 42, 282–289. [Google Scholar] [CrossRef]
- Dellonder-Frigolé, J.; Matas-Pareja, M.; Calle-García, J.A.; Bowen, J.; Fatjó-Rios, J.; Albertí-Fitó, G. Revisiting the original Akin technique: A comparative analysis of radiographic outcome. Foot Ankle Surg. 2022, 28, 394–401. [Google Scholar] [CrossRef] [PubMed]
- Frey, C.; Jahss, M.; Kummer, F.J. The Akin procedure: An analysis of results. Foot Ankle Int. 1991, 12, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Montiel, V.; Suárez, Á.; Riera, L.; Villas, C.; Alfonso, M. Akin osteotomy: Is the type of staple fixation relevant? Int. Orthop. 2020, 44, 1435–1439. [Google Scholar] [CrossRef] [PubMed]
- Coughlin, M.J.; Shurnas, P.S. Hallux rigidus, Grading and long-term results of operative treatment. J. Bone Jt. Surg. Am. 2003, 85, 2072–2088. [Google Scholar] [CrossRef]
- Butterworth, R.D. Description of a simple bunion operation. J. Bone Jt. Surg. Am. 1964, 46, 461. [Google Scholar]
- Cwikla, P.S.; Hetherington, J.V.; Petek, J.M. Morphological consideration of the first metatarsophalangeal joint. J. Foot Surg. 1992, 31, 3–9. [Google Scholar] [PubMed]
- Yoshioka, Y.; Siu, D.W.; Cooke, T.D.V.; Bryant, J.T.; Wyss, U. Geometry of the first metatarsophalangeal joint. J. Orthop. Res. 1988, 6, 878–885. [Google Scholar] [CrossRef] [PubMed]
- Paley, D. Osteotomy Concepts and Frontal Plane Realignment. In Principles of Deformity Correction, 1st ed.; Paley, D., Ed.; Springer: Berlin/Heidelberg, Germany, 2002; pp. 99–154. [Google Scholar] [CrossRef]
- Filho, E.L.R.; Torres, M.R.; Silva, M.R.; Lima, F.R.; Aguiar, J.L. Simplified Calculation for Corrective Osteotomies of Long Bones. Acta Ortop. Bras. 2016, 24, 253–258. [Google Scholar] [CrossRef] [PubMed]
- Ho, N.T.; Rhodes, B.R.; Kominsky, S. A Closer Look at an Emerging Fixation Option for the Akin Osteotomy. Podiatry Today 2010, 23, 1–3. [Google Scholar]



| Variables (N = 186) | Mean | SD | Min | Max | |
|---|---|---|---|---|---|
| DASA, ° | 1.11 | 3.96 | −12.00 | 12.00 | Measured angles |
| IPOA, ° | 8.66 | 5.00 | −4.00 | 25.00 | |
| HOT, mm | 5.14 | 1.45 | 1.57 | 8.08 | Osteotomy Height |
| H2OT, mm | 8.91 | 1.50 | 5.38 | 12.85 | |
| Lbase, mm | 16.71 | 1.48 | 12.66 | 23.23 | Width of the base (c) |
| LMetaf1, (c), mm | 18.75 | 1.45 | 15.13 | 23.91 | |
| LMetaf2, (c), mm | 17.43 | 1.62 | 13.57 | 23.95 | |
| LMetaf3, (c), mm | 15.22 | 1.69 | 11.59 | 21.43 | |
| LMetaf4, (c), mm | 13.41 | 1.56 | 9.98 | 17.96 | |
| LMetaf5, (c), mm | 12.27 | 1.43 | 8.99 | 15.96 | |
| M2mm-L1, (d), ° | 71.54 | 9.68 | 49.98 | 94.06 | Cortical angle measured (relative to the joint line) using short side (shear width over cortical) and increasing from 2 to 3 and 4 mm (d) |
| M3mm-L1, (d), ° | 69.46 | 7.65 | 48.29 | 87.57 | |
| M4mm-L1, (d), ° | 67.38 | 6.89 | 44.28 | 87.06 | |
| M2mm-L2, (d), ° | 65.36 | 8.16 | 40.95 | 91.07 | |
| M3mm-L2, (d), ° | 66.31 | 7.50 | 43.26 | 90.92 | |
| M4mm-L2, (d), ° | 67.26 | 7.67 | 45.57 | 90.76 | |
| M2mm-L3, (d), ° | 71.41 | 8.68 | 51.83 | 92.94 | |
| M3mm-L3, (d), ° | 72.93 | 8.20 | 56.25 | 95.53 | |
| M4mm-L3, (d), ° | 74.45 | 8.08 | 57.65 | 98.11 | |
| M2mm-L4, (d), ° | 78.66 | 7.98 | 56.89 | 105.57 | |
| M3mm-L4, (d), ° | 80.07 | 7.56 | 63.35 | 103.69 | |
| M4mm-L4, (d), ° | 81.47 | 7.37 | 64.08 | 101.81 | |
| M2mm-L5, (d), ° | 84.40 | 7.26 | 67.36 | 102.18 | |
| M3mm-L5, (d), ° | 85.49 | 6.90 | 69.82 | 102.66 | |
| M4mm-L5, (d), ° | 86.59 | 6.82 | 70.68 | 103.74 | |
| e2mm-L1, (e), ° | 5.92 | 0.53 | 4.40 | 7.38 | Akin’s correction angle (with respect to joint line and cortical tilt) (e) |
| e3mm-L1, (e), ° | 8.99 | 0.77 | 6.82 | 11.29 | |
| e4mm-L1, (e), ° | 12.09 | 1.02 | 9.38 | 15.30 | |
| e2mm-L2, (e), ° | 6.24 | 0.71 | 4.12 | 8.47 | |
| e3mm-L2, (e), ° | 9.61 | 1.05 | 6.70 | 12.73 | |
| e4mm-L2, (e), ° | 13.06 | 1.38 | 9.60 | 16.86 | |
| e2mm-L3, (e), ° | 7.41 | 0.93 | 5.07 | 9.94 | |
| e3mm-L3, (e), ° | 11.31 | 1.31 | 7.99 | 14.85 | |
| e4mm-L3, (e), ° | 15.24 | 1.65 | 10.76 | 19.49 | |
| e2mm-L4, (e), ° | 8.59 | 1.01 | 5.93 | 11.55 | |
| e3mm-L4, (e), ° | 12.95 | 1.44 | 9.20 | 17.28 | |
| e4mm-L4, (e), ° | 17.20 | 1.82 | 12.60 | 22.73 | |
| e2mm-L5, (e), ° | 9.40 | 1.05 | 7.06 | 12.84 | |
| e3mm-L5, (e), ° | 14.01 | 1.50 | 10.77 | 19.02 | |
| e4mm-L5, (e), ° | 18.42 | 1.90 | 14.12 | 24.49 |
| Variables | Female | Male | p-Value |
|---|---|---|---|
| N = 166 | N = 20 | ||
| DASA, ° | 1.00 [0.00;3.00] | 1.00 [1.00;3.25] | 0.272 |
| IPOA, ° | 9.00 [6.00;12.0] | 6.50 [5.00;11.0] | 0.277 |
| Lbase, mm | 16.4 [15.7;17.4] | 17.0 [16.8;17.7] | 0.002 |
| LMetaf1 (c), mm | 18.4 [17.7;19.4] | 20.4 [18.9;21.9] | <0.001 |
| LMetaf2 (c), mm | 17.2 [16.3;18.1] | 19.5 [17.7;20.7] | <0.001 |
| LMetaf3 (c), mm | 15.0 [14.0;15.8] | 16.7 [15.3;19.1] | <0.001 |
| LMetaf4 (c), mm | 13.2 [12.3;14.1] | 15.1 [13.7;16.9] | <0.001 |
| LMetaf5 (c), mm | 12.1 [11.2;12.9] | 13.9 [12.5;15.2] | <0.001 |
| DASA | IPOA | DASA | IPOA | ||
|---|---|---|---|---|---|
| IPOA | 0.458 *** | IPOA | 0.458 *** | ||
| e2mm-L1 (e) | −0.123 | −0.011 | M2mm-L1 (d) | −0.016 | 0.036 |
| e3mm-L1 (e) | −0.159 * | −0.028 | M3mm-L1 (d) | −0.112 | −0.031 |
| e4mm-L1 (e) | −0.189 ** | −0.048 | M4mm-L1 (d) | −0.226 ** | −0.120 |
| e2mm-L2 (e) | −0.252 *** | −0.197 ** | M2mm-L2 (d) | −0.326 *** | −0.262 *** |
| e3mm-L2 (e) | −0.244 *** | −0.177 * | M3mm-L2 (d) | −0.426 *** | −0.302 *** |
| e4mm-L2 (e) | −0.218 ** | −0.149 * | M4mm-L2 (d) | −0.487 *** | −0.312 *** |
| e2mm-L3 (e) | −0.244 *** | −0.122 | M2mm-L3 (d) | −0.521 *** | −0.286 *** |
| e3mm-L3 (e) | −0.195 ** | −0.102 | M3mm-L3 (d) | −0.563 *** | −0.305 *** |
| e4mm-L3 (e) | −0.134 | −0.075 | M4mm-L3 (d) | −0.581 *** | −0.312 *** |
| e2mm-L4 (e) | −0.176 * | −0.062 | M2mm-L4 (d) | −0.581 *** | −0.283 *** |
| e3mm-L4 (e) | −0.115 | −0.034 | M3mm-L4 (d) | −0.596 *** | −0.293 *** |
| e4mm-L4 (e) | −0.053 | −0.003 | M4mm-L4 (d) | −0.593 *** | −0.294 *** |
| e2mm-L5 (e) | −0.145 * | −0.022 | M2mm-L5 (d) | −0.566 *** | −0.265 *** |
| e3mm-L5 (e) | −0.083 | 0.006 | M3mm-L5 (d) | −0.588 *** | −0.272 *** |
| e4mm-L5 (e) | −0.020 | 0.034 | M4mm-L5 (d) | −0.589 *** | −0.269 *** |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Testa, E.A.; Ruiz Nasarre, A.; Alvarez Goenaga, F.; Poggio Cano, D.; Porreca, A.; Baduell, A.; Garcia Elvira, R.; Dalmau-Pastor, M.; Ruiz Riquelme, P. Analysis of Factors Influencing Corrective Power of Akin’s Osteotomy in 2D Plain Radiographs: What to Consider to Obtain Good Correction in Hallux Valgus Surgery. Diagnostics 2025, 15, 1618. https://doi.org/10.3390/diagnostics15131618
Testa EA, Ruiz Nasarre A, Alvarez Goenaga F, Poggio Cano D, Porreca A, Baduell A, Garcia Elvira R, Dalmau-Pastor M, Ruiz Riquelme P. Analysis of Factors Influencing Corrective Power of Akin’s Osteotomy in 2D Plain Radiographs: What to Consider to Obtain Good Correction in Hallux Valgus Surgery. Diagnostics. 2025; 15(13):1618. https://doi.org/10.3390/diagnostics15131618
Chicago/Turabian StyleTesta, Enrique Adrian, Alberto Ruiz Nasarre, Fernando Alvarez Goenaga, Daniel Poggio Cano, Annamaria Porreca, Albert Baduell, Ruben Garcia Elvira, Miki Dalmau-Pastor, and Pablo Ruiz Riquelme. 2025. "Analysis of Factors Influencing Corrective Power of Akin’s Osteotomy in 2D Plain Radiographs: What to Consider to Obtain Good Correction in Hallux Valgus Surgery" Diagnostics 15, no. 13: 1618. https://doi.org/10.3390/diagnostics15131618
APA StyleTesta, E. A., Ruiz Nasarre, A., Alvarez Goenaga, F., Poggio Cano, D., Porreca, A., Baduell, A., Garcia Elvira, R., Dalmau-Pastor, M., & Ruiz Riquelme, P. (2025). Analysis of Factors Influencing Corrective Power of Akin’s Osteotomy in 2D Plain Radiographs: What to Consider to Obtain Good Correction in Hallux Valgus Surgery. Diagnostics, 15(13), 1618. https://doi.org/10.3390/diagnostics15131618






