Abstract
Peripheral nerve injuries represent a significant challenge in legal medicine, and their proper management and evaluation are at the intersection of clinical medicine, anatomical science, and legal medicine. In this review, we aimed to integrate current knowledge about the anatomy, physiology, clinical management, and paraclinical assessment of peripheral nerve injuries, targeted explicitly for medical–legal practice. We conducted a comprehensive review of the medical–legal evaluation framework needed to evaluate peripheral nerve injuries, with particular emphasis on anatomical variations, imaging techniques, and methods to assess the timing of injury. Peripheral nerve injuries should be analyzed using a complex approach, which includes anatomical characteristics, variants, microanatomy, physiopathology, imaging, and other paraclinical evaluations. The analysis of causation and timing of injury should be heavily based on objective criteria and should be performed using a reproducible, objective, and scientifically based approach.
1. Introduction
Peripheral nerve injuries (PNIs) are often found in patients requiring medical–legal evaluation, and their proper management and expert analysis are usually lacking [1]. Their analysis sits at the intersection of clinical medicine, anatomical science, and legal medicine, often requiring a multidisciplinary approach for proper management.
PNIs are among the most prevalent, yet still understudied consequences of trauma, mainly affecting younger male patients. Aman et al., in an epidemiological analysis of more than 110,000 subjects from a European level 2 trauma center, found PNIs in around 5000 cases (4.5%), with 52.2% being acute PNIs, and the rest non-traumatic or posttraumatic—compression, neuroma formation, tumor, irritation, inflammation. In 46.6% of all cases, they found intact continuity of nerves despite perioperative loss of function; in 7.4%, they found an incomplete laceration, and in 44.8%, a complete nerve laceration. Most injuries were located in the upper extremity (88.3%), affected males (73.5%), and had a mean age of 43.2 [2]. In a larger cohort of 1,230,362 patients, Padovano et al. found a similar incidence of PNIs (2.6%), which included only traumatic cases [3]. Other studies have reported much lower values; for example, a registry-based research from Sweden found an overall incidence of 15.6 per 100,000 cases in men and 10.1 per 100,000 cases in women, with the most affected part being the hand [4]. PNIs are often associated with long-term consequences, extending far beyond acute disability, especially in younger groups [5], causing long-term disability, an increased number of sick days, and even permanent disability pension [6]. They also impose a significant socioeconomic burden, with the average direct medical cost exceeding EUR 4800 per case in Germany (with much higher values for cases with combined tendon or vascular injuries), not accounting for lost productivity and rehabilitation-related expenses [6].
The incidence of traumatic PNIs varies by location and depends on the type of traumatic event. For example, a study by Huckhagel et al. centered on lower limb TPNIs and found the highest overall incidence in motorcycle accidents, followed by car occupants, high falls, and pedestrians. In motorcycle accidents and among pedestrians, the most affected nerve was the peroneal nerve (35.5% and 12.7%, respectively). In car occupants, the tibial nerve was the most affected (32%), and in high falls, low falls (<3 m), and bicycle accidents, the femoral nerve was most affected (13.5%, 5.8%, and 4.8%, respectively) [7].
The clinical management and forensic evaluation of PNIs are based on anatomical principles. Peripheral nerves exhibit significant microarchitectural complexity, with a highly complex fascicular organization, layers of connective tissue, and vascular networks affecting injury patterns and regenerative potential [8,9]. For example, the tensile strength of the epineurium determines susceptibility to traction injuries, whereas fascicular topography has essential consequences for functional outcomes after partial nerve transection [10,11]. Anatomical variations represent a particular diagnostic and medical–legal challenge, especially as they are sometimes related to malpractice claims. About 15–20% of individuals have non-textbook nerve branching patterns or anomalous courses, potentially mimicking pathological findings, complicating surgical exploration, or causing an improper diagnosis.
The medicolegal evaluation of PNIs requires proper integration of anatomical knowledge, clinical expertise, and legal and forensic standards. Two main scenarios dominate medical–legal practice: the assessment of alleged medical malpractice in managing nerve injury and determining injury causation and severity in personal injury claims [8,12]. This review aims to integrate current knowledge about the anatomy, physiology, clinical management, and paraclinical assessment of PNIs for medical–legal practice.
2. Fundamental Anatomical Principles of the Peripheral Nerves: Clinical and Medical–Legal Consequences
Peripheral nerves are highly complex anatomical structures that transmit chemical messages between the central nervous system and peripheral effectors. Each nerve consists of three concentric connective tissue sheaths: epineurium, perineurium, and endoneurium, which provide structural integrity and controlled flexibility [13,14]. The epineurium (Henle’s sheet) encases each nerve fiber, creating the most intimate protective sheath for axons and their associated Schwann cells [15]. Schwann cells (mainly) secrete a continuous basal lamina, which has various roles, including Schwann cell proliferation, migration, myelination, and formation of Ranvier nodes, and provides mechanical support [16]. Individual fibers are then bundled together in fascicles, each surrounded by a stronger protective layer, the perineurium, which consists of 7–8 concentric layers of connective tissue, whose cellular component is mainly represented by myoepithelial cells [17]. The perineurium is a selective barrier, controlling molecular exchange between neural tissue and the surrounding environment [17,18]. Multiple fascicles are then bundled together with the associated blood supply and fatty tissue by the epineurium. Peripheral nerves usually contain 3–12 fascicles, depending on the anatomical location, with larger fascicle diameters found in motor nerves compared to sensory nerves (600–800 µm compared to 400–400 µm) [19]. The epineurium consists mainly of longitudinal type I and III collagen fibers, with a few elastic fibers to increase elastic support [20,21]. The epineurium consists of 30–75% of the nerves’ cross-sectional area [18,22], and it houses the vasa nervorum, a vascular network consisting mainly of arterioles with 50–150 µm [22]. See Figure 1.
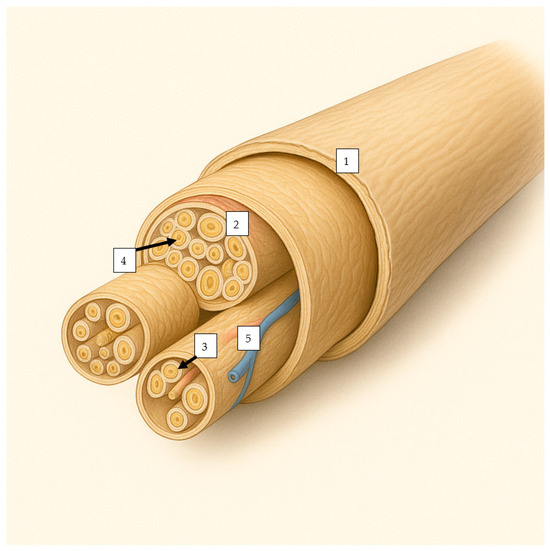
Figure 1.
The overall structure of a nerve, containing (1)—an outer layer (epineurium), encasing the nerve, (2)—an intermediary layer (perineurium), encasing multiple nerve fibers, and (3)—an inner layer (endoneurium), encasing each nerve fiber (4). Within the nerve fiber are present nutritional vessels (5).
This microanatomical organization of peripheral nerves ensures significant biomechanical resilience, enabling normal function during daily activities and protection against mechanical injuries [15]. The Schwann cell basal lamina ensures the biomechanical protection of individual fibers, which strengthens it in conjunction with specialized proteins such as PMP22 [15]. The perineurial layer further increases mechanical strength and protects from chemical byproducts associated with trauma [17]. Finally, the epineurium offers significant strength and security, accommodating the mechanical limb movement and positioning stresses [23].
Peripheral nerves have a dual vascular supply: extrinsic, represented by segmental arteries from adjacent vascular bundles (e.g., radial collateral artery for the radial nerve), and intrinsic, represented by longitudinal anastomoses within the epineurium. This redundant system allows the nerves to tolerate significant vascular compromise (up to 50%) before ischemic damage occurs [24,25,26]. However, there are areas where this vascular redundancy is minimized, such as the mid-humerus level for the radial nerve or the fibular neck segment for the common peroneal nerve [27,28,29].
Approximately 25% of individuals have significant peripheral nerve variations that deviate from classical anatomical descriptions. If they are not known, there is an increased risk of damage during the surgical procedure or improper management of the symptomatology associated with the injury. The most studied anatomical variations are those of the sciatic nerve, especially in relation to the piriformis muscle [30,31,32]. The most common variant of the sciatic nerve exits the pelvis through the greater sciatic foramen below the piriformis muscle. It descends between the greater trochanter and the ischiatic tuberosity [32], with an overall prevalence of approximately 90%, with high variability between individual studies. The common peroneal nerve is more susceptible to injury during total hip arthroplasty or other hip arthroscopic procedures, especially in patients with specific anatomical variants [31]. Another forensically relevant anatomical variation in the nerves of the lower limb is represented by the superficial course of the common peroneal nerve at the fibular neck (1.2–3.4 mm from the surface), which explains the very high prevalence of traction injuries at this level, especially during knee dislocations, fractures of the proximal fibula, or fractures of the tibial plateau [33].
The median nerve in the upper limb is known to have significant interindividual variation in its origin and course. An abnormal formation of the median nerve, from more than two roots, is seen in 11.5–52% of all cases, depending on the study [34,35,36,37], and is much more common in males than in females (81.8% vs. 18.2%, respectively) [36]. In a landmark study on the anatomical variations in the median nerve in carpal tunnel syndrome, Lanz found 29 variations in 246 hands, which he classified as type I, variations in the course of the thenar branch; type II, accessory branches at the distal portion of the carpal tunnel; type III, high divisions of the nerve; and type IV, accessory branches to the carpal canal [38]. Poisel classified the thenar branches as extra-, sub- (and trans-ligamentous in 46%), sub-ligamentous (31%), and 21% of cases, respectively [39]. All these variants have a significant impact on surgical outcomes and diagnostic accuracy. Clinicians should remain aware of these variants, as some require careful and specific preoperative planning and intraoperative awareness to optimize patient outcomes [36].
Anatomical variations in peripheral nerves have significant implications for surgical planning and execution, particularly in nerve reconstruction. Understanding intraneural topography is paramount while performing fascicular reconstruction, as the arrangement of motor and sensory fascicules varies between individuals and along the course of individual nerves [3,40,41]. The feasibility of distal nerve transfer is highly dependent on understanding both normal anatomy and anatomical variants [19]. Surgeons should consider the topographic organization of the target nerves when planning transfer procedures, as success is highly dependent on the appropriate matching of donor and recipient nerve fascicles [19]. Neurolysis also requires a detailed understanding of the anatomical variants and microanatomy of the nerve to achieve optimal outcomes [42,43]. Failure to account for anatomical variants during neurolysis could lead to incomplete symptom relief, inadvertent injury to unaffected neural components, and increased litigation risk.
Regional anesthesia and diagnostic procedures are another area in which peripheral nerve variations have significant consequences. The overall arrangement of the nerve fibers affects the overall effect of nerve blockade and the risk of nerve injury during the procedure [44]. To decrease this risk, various methods may be used, such as ultrasound, which may properly identify the nerve location, evaluate the relative position of blood vessels, nerves, and muscles around the puncture site, ultrasound aided by AI with medical image fusion, and neurostimulation [45].
The physiological processes involved when damaged neural structures lead to clinical symptoms are sometimes directly influenced or mimicked by those caused by anatomical variants [46]. Table 1 and Table 2 provide examples.

Table 1.
Anatomical variations leading to lower limb nerve compression (Based on [46,47,48,49,50,51,52,53,54,55,56,57]). Are detailed the nerve, common compression sites, and anatomical variations leading to compression.

Table 2.
Anatomical variations leading to upper limb nerve compression (based on [37,46,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77]. Are detailed the nerve, common compression sites, and anatomical variations leading to compression.
3. Diagnostic Challenges in Traumatic PNI
The diagnostic algorithm for traumatic PNI is complicated by the complex anatomy of the peripheral nerves, highly variable injury patterns associated with frequent anatomical variations, and significant limitations of mainstream assessment methods. Recent advances in microsurgical techniques, imaging technologies, electrophysiologic studies, and overall understanding of nerve microanatomy have increased diagnostic accuracy, but significant challenges still occur, especially in non-reference medical centers. The complexity of the evaluation in traumatic PNIs resides in the need to assess multiple components, such as motor function, sensory integrity, pain patterns, structural damage, while also taking into account the timing of injury, the age of the patient, associated complications, the type of medical intervention that was performed etc. [44,78].
For a proper forensic analysis, it is critical to classify the severity of the injury, a task that is difficult in traumatic PNIs. Traditional classification systems, such as those developed by Seddon and Sunderland (Table 3), provide an essential framework for understanding the nerve injuries the patient suffers, but often fail to capture the intricacies of complex trauma cases. Sedon defines three grades of PNI: neurapraxia, axonotmesis, and neurotmesis. Neurapraxia is caused by relatively minor injuries (usually compression in traumatic PNIs, causing neurotubules’ and neurofilaments’ fragmentation and axonal edema) [79], leading to a temporary loss of motor and sensory function, usually in up to eight weeks. Axonotmesis is caused by moderate trauma (a more severe compression injury, a stretch injury, or direct nerve contusion), causing damage to both the axon and the myelin sheath. It leads to motor and sensory dysfunction distally from the point of injury. It may be objectively assessed using imaging techniques, electromyography (which shows a denervation pattern, with fibrillation potential and positive sharp waves from 10 to 14 days after the traumatic event), or nerve conduction velocity studies (revealing loss of nerve conduction distally, from three to four days after the traumatic event). Neurotmesis is the most severe form of traumatic PNI, leading to an injury of both the nerve and the encasing fibrous tissue. It is usually caused by nerve lacerations (knives, shards of glass, saw blades) or severe stretch (as in severe dislocations) and, in the military, by explosions [80]. It has the worst prognosis, with a decreased chance of (even partial) recovery.

Table 3.
Seddon and Sunderland classifications for nerve injuries (based on [81,82,83,84], their main symptoms and MRN characteristics.
A proper distinction between different grades often requires a detailed understanding of the microanatomy and highly specialized and trained radiologists or other specialized techniques.
Compression injuries typically pertain to Grade I nerve injuries or neurapraxia and are common in the carpal tunnel or cubital tunnel, owing to nerves passing through confined anatomical openings. Crossing between rigid bony structures leads to compression of blood vessels, with subsequent ischemia and myelin displacement at the injury site. Both motor and sensory functions may be lost due to acute or chronic excessive pressure, even though the anatomy of the nerve is still intact and axonal damage is absent. Recovery is complete, and function is resumed relatively quickly (weeks to years) [85].
Axonotmesis generally occurs in injuries where the elastic nature of the nerve and its stretchability are defeated by a stronger traction force, commonly known as traction injuries [86]. This happens because of the nerve’s undulating characteristics loss when traction is applied for a long time or with extreme force. At this point, the perineurium takes on pressure with its tensile properties. If the traction force persists with the same intensity, the perineurium eventually tears [87].
Transection injuries are usually the cause of neurotmesis or grade V injuries and occur when the nerve is interrupted following severe trauma at that level. This is generally caused by the action of a sharp object (such as a knife) and can also be observed in patients with shrapnel injuries. In this case, the anatomical nerve structure is severed and requires surgical treatment to regain full functionality [81,88].
Clinical examination remains a cornerstone in the proper analysis of traumatic PNIs, despite its inherent limitations. The classical clinical approach consists of manual muscle testing, sensory collapse testing, and pain evaluation [89]. Details are provided in Table 4. Manual muscle testing has difficulties distinguishing between different causes of weakness or detecting more subtle motor deficits. It may also be compromised by a lack of cooperation, especially in acute trauma settings [89]. The challenges are even more complex in mixed nerve injuries, with motor and sensory components affected differently. Sensory testing has difficulty separating different types of sensory loss and correlating clinical findings with specific nerve territories (more pronounced in some specific anatomical variations) [83,90,91]. The Symptoms Categorization—History Taking-Examination—Diagnostic Evaluations Approach has been proposed to overcome some of these limitations as a more structured approach to manage these diagnostic challenges; however, proper implementation requires significant training and expertise to be effective [92].

Table 4.
Clinical examination in PNIs (based on [89,93]).
MR neurography (MRN) has emerged as a highly sensitive method for assessing traumatic PNIs in recent years [84]. It can not only correctly classify injuries but also correlate with functional outcomes. The diagnostic accuracy of MRN varies depending on the severity of the nerve injury and anatomical location. For example, in detecting root nerve avulsion in brachial plexus injuries, MRN has a high specificity (89%) but only a moderate sensitivity (68%) [94]. MRN is especially useful in differentiating Sunderland grade III from grade IV injuries through its ability to visualize fascicular architecture and perineurial integrity properly [84,95]. The sensitivity is especially high in detecting Sunderland IV-V injuries (reaching 83.3% for detecting inferior alveolar and lingual nerve injuries), and much lower for Sunderland I-III injuries (19.1%, for the same nerves) [96]. The high soft tissue contrast helps identify neuroma-in-continuity formation in neurotmetic injuries, a critical differentiator from lower-grade axonal injuries. This addressed a key limitation of electrophysiological studies, which often struggle to differentiate between intact but non-conducting fascicles and complete anatomical disruptions [97]. More advanced MRN protocols incorporate quantitative measures, including T2 hyperintensity, nerve cross-sectional areas, and diffusion tensor imaging parameters. These have shown significant promise in bridging the gap between structural assessment and functional prognosis. For example, persistent elevation of T2 hyperintensity beyond 6 months after trauma is associated with poor sensory recovery and the development of chronic neuropathic pain [98,99]. Diffusion tensor imaging-derived fractional anisotropy values below 0.3 at the injury site predict incomplete motor recovery [100,101]. The development of specialized sequences, such as 3D TSE STIR black-blood imaging, was shown to increase the visualization of PNI [96,102].
The main limitations of MRN are its high cost and limited availability, especially in resource-limited institutions [103]. A lower and variable sensitivity is also a highly relevant issue, especially in a medical–legal context where a near 100% diagnostic accuracy is needed. It has a poor reliability in detecting pseudomeningoceles as markers of nerve root avulsion, limiting its usefulness in specific types of PNIs [9,94]. It also has temporal limitations, as signal changes may persist after the initial traumatic injury, and it may not appear immediately after trauma [96].
High-resolution ultrasonography is increasingly used to evaluate traumatic PNIs, offering distinct advantages, such as real-time imaging, cost-effectiveness, and widespread availability [11]. It is beneficial for detecting injuries in superficial nerves (such as the superficial palmar nerves) [102]. Its novelty resides in its potential to visualize individual nerve fascicles and detect subtle architectural changes, which were previously only visible using histological examination [102,104]. It may also be used during reconstructive nerve surgeries, enabling direct contact imaging for enhanced structural resolution and real-time guidance during surgical procedures [105]. Numerous scientific articles have shown that ultrasound (US) can correctly identify patients with unfavorable surgical outcomes resulting from anatomical predisposition [54,106,107,108].
It may determine whether the nerves are compromised, tethered, or hypermobile in relation to neighboring structures. It allows for the easier identification of multi-segmental injuries because the entire longitudinal course of the nerve can be evaluated in a single examination. It may also detect neuropathic pain, locate the nerves causing the symptoms, and identify the exact anatomical area responsible for a specific symptom [11]. Despite its obvious advantages, this procedure has significant limitations. The procedure has decreased sensitivity and specificity in deeper-located nerves or patients with poorer acoustic windows due to obesity or edema [109]. It also has a reduced sensitivity for detecting mild nerve injuries, the diagnostic accuracy being highly dependent on the degree of neural damage [110]. Operator dependency is also a significant limitation, as the sensitivity and specificity vary according to the experience or skill of the personnel [110]. There is an incomplete correlation between ultrasound findings and functional outcomes, especially when structural abnormalities do not correspond to clinical disabilities. Also, sometimes there is a poor correlation between ultrasound abnormalities and electrodiagnostic studies [102].
Nerve biopsy may sometimes be useful as a diagnostic tool in forensic pathology, but its use is currently limited due to its increased invasiveness compared to other methods. Current indications include suspected inflammatory neuropathies (for a differential diagnosis with traumatic PNIs), cases involving toxic neuropathies with unknown etiology, or when a hereditary neuropathy must be confirmed or excluded, and genetic testing is unavailable or inconclusive [111,112]. The timing of nerve biopsy is essential for maximizing the diagnostic yield. Optimal timing is between two and six weeks after the injury, allowing enough time to develop characteristic histological changes while avoiding secondary changes that potentially obscure the primary pathology [111]. Post-mortem, nerve biopsies should be performed as early as possible to minimize post-mortem artifacts caused by autolysis or putrefaction [113].
Electrodiagnostic studies (such as nerve conduction studies or electromyography) have long been considered helpful for properly assessing PNI.
All patients with PNI must be evaluated using motor conduction studies (MCS), sensory conduction studies (SCS), and electromyography (EMG) of the involved muscle. The parameters measured during MCS and SCS are distal latency, amplitude, and velocity [114].
Although they are included in the standard protocol for evaluating PNIs, electroconduction studies have low sensitivity and specificity (30–65%) [115,116]. In addition, their value is time-constrained, as immediately after the injury, they may not reveal the full extent of nerve damage, potentially causing false-negative results in the acute phase [78]. This may lead to a delayed diagnosis, causing a miss of the optimal window for surgical intervention in complete nerve disruptions. They also have difficulties in properly evaluating mixed nerve injuries, providing a comprehensive assessment of muscular function, and precisely identifying the anatomical location of the injury [89].
4. Prognosis
The prognosis depends on the patient’s age, mechanism of injury, and associated vascular and soft tissue injuries [117]. Although peripheral nerve injuries are not life-threatening, they may lead to a considerable decline in the patient’s quality of life [118]. The main elements that altered the prognosis of the patients are presented in Table 5.

Table 5.
Prognostic factors in PNIs, useful for a proper evaluation of the medical-legal consequences of these injuries.
5. Medical Legal Framework for the Evaluation of PNIs
The medicolegal evaluation of PNIs should begin with a proper identification and characterization of the cause (either trauma or an iatrogenic injury), the prejudice, which in turn should be quantified appropriately, and end with a proper evaluation of the causation link between them [129]. Adequate establishment for causation in PNIs requires a deep understanding of multiple factors, including mechanisms of injury, anatomical vulnerability, anatomical variations, physiopathology of injury and recovery, and temporal relationships between the event of interest and the effect. PNIs may be caused by various mechanisms, including compression, penetrating trauma, stretch, and ischemia, each associated with distinct patterns of damage and recovery [10,130]. These mechanisms should be correlated with documented clinical, imaging, and electrophysiological findings. This task is exponentially more complex in cases involving preexisting conditions or multiple potential causes of a particular nerve dysfunction. A more structured approach to evaluation is preferable whenever available, such as the SHED approach [131]. An overview of the general framework for PNI evaluation in a forensic context is presented in Table 6.

Table 6.
Medical–legal framework for PNI evaluation (based on [8,129,132]).
6. Causation and Timeline Determination in Traumatic PNIs
To establish a causal link in PNIs, experts should have a comprehensive understanding of the mechanisms of injury and their relationship with different patterns of nerve damage. The expert should correlate the proposed mechanisms with the observer pattern of nerve alteration and determine whether the relationship is scientifically plausible.
Iatrogenic nerve injuries are especially challenging to determine because they occur during otherwise appropriate medical procedures, and their overall frequency is not low. For example, femoral nerve injuries have an iatrogenic etiology in up to 60% of all cases, occurring during different types of surgical interventions (abdominal, pelvic, orthopedic, urologic) [133]. They may be caused by mechanical damage due to stretching, compression due to incorrect surgical positioning, thermal injury due to the use of electrocautery, or chemical injury caused by local anesthesia. Each mechanism leads to a distinct pattern of nerve dysfunction, which can be identified using clinical, electrodiagnostic, and imaging evaluations. An example of an iatrogenic femoral injury is presented in Table 7. Postmortem, the temporal sequence of changes occurring in nerves may be established using histological, electron microscopy, and molecular biology techniques. Electron microscopy is especially useful for detecting early changes that can be used for timeline determination. A study by Pieri et al. found that, at 12 h after death, a relevant loss of osmium affinity, with persistent myelin sheath and internodal tract, and visible, symmetrical, Schmidt–Lanterman clefts. On transversal sections, there is an initial loss of the myelin structure and the formation of small vacuoles. At 24 h, the osmium loss in the paranodal tract was apparent, myelin being flocculent and granular at this level, and the Schmidt–Lanterman clefts still symmetrical, but broader and longer. On transverse sections, up to 36 h after death, small elliptical splits were present within the myelin sheath, and small, osmiophilic granules were present near these discontinuities. Between 37 and 48 h, they are identifiable, aggregating in the axon, and bulging splits, especially in larger fibers. At 48 h, the osmium loss at the paranodal tract was more significant, and the Schmidt–Lanterman clefts were significantly lengthened. On transverse sections, after 48 h, a complete collapse of the internal myelin layers, which are fragmented in lamellar configurations, is apparent [134]. Vacchiano et al. used postmortem cholesterol levels from the median nerve to evaluate the postmortem interval from 20 to 136 h postmortem [135], with initially promising results, but the technique is more challenging to fully implement in forensic practice. Some of these alterations also occur after trauma. To properly differentiate them, we should evaluate the pattern of damage—traumatic injuries show a more organized pattern, with specific histological hallmarks, while postmortem changes show a diffuse, unorganized, non-specific degradation. Traumatic injuries show characteristic hallmarks such as the presence of an organized inflammatory response, specific patterns of axonal injuries such as retraction balls, and localized hemorrhage, which are clearly distinct from autolytic changes [136]. The presence of organized scar tissue formation, or specific patterns of Wallerian degeneration, is also typical for antemortem injuries [134,137].

Table 7.
Patterns of femoral nerve dysfunction based on the mechanisms of injury (based on information from [133]. MRC—Medical Research Council muscle grading system [138], NCS—nerve conduction studies, EMG—electromyography.
The temporal relationship between traumatic/iatrogenic events and symptom onset provides highly relevant information for establishing causation. Although PNIs lead to immediate symptoms, the full extent of neurological dysfunction may not be clear until days or weeks later. Understanding the usual timeframe is necessary to differentiate these injuries from chronic degenerative conditions or other causes of nerve dysfunction. Preexisting conditions should also be carefully considered, as they may predispose patients to PNIs or mimic them. Anatomical variations should be considered, as they could make some individuals more prone to iatrogenic damage [139].
Regeneration timelines and recovery patterns are also essential for proper forensic analysis. Peripheral nerve regeneration is a slow process, typically requiring more than three months for axons to regenerate to distal target organs. During this time, the muscles undergo atrophy [140,141]. The usual regeneration rate is 1–2 mm daily, which helps assess recovery timelines based on the distance from the injury site to the target organ (s). In this regard, the classifications of Seddon and Sunderland can be used, even though they have some limitations, as mentioned above. Also, one must consider that recovery patterns differ based on the patient’s age, injury mechanism, anatomical location, and time to treatment [142]. Electrodiagnostic studies may provide objective measures of nerve regeneration, which may help track recovery times and predict functional outcomes. They may prove a progressive improvement, a plateau, or even a worsening case in which the causation nexus could be more complex, potentially involving medical malpractice [136,137,138,139].
Electromyographic temporal patterns may be used to assess the timeline. After PNI, Wallerian degeneration is initiated distal to the injury site, triggering electrophysiological changes detectable via EMG (Table 8).

Table 8.
Chronology of EMG changes in PNI (MUAP—Motor Unit Potential Evolution). Based on [143,144,145,146]. Are detailed the main EMG findings, and their clinical and forensic implications.
MRN may also be extremely useful in establishing a timeline for PNIs. Following axonal injury, the blood–nerve barrier breaks down, triggering endoneurial edema, which is detectable through increased T2 signal intensity within 6–48 h, preceding Wallerian degeneration, which is characterized by progressive distal nerve hyperintensity and volume loss. Details are presented in Table 9.

Table 9.
Chronology of MRN signal changes in PNI (DWI—diffusion weighted imaging; Ktrans—volume transfer constant; DTI—diffusion tensor imaging; ADC—apparent diffusion coefficient; 3D PSIF—Reversed Fast Imaging with Steady-State Free Precession; CSA—cross-sectional area).
7. Malingering in Traumatic PNIs
The American Psychiatric Association defines malingering as the intentional production of false or grossly exaggerated physical or physiological problems, usually externally motivated (avoiding military duty, work, obtaining financial compensation, avoiding/evading criminal prosecution, or obtaining controlled substances [147]. From both clinical and medico-legal perspectives, individuals who malinger often present symptomatology that is incongruent with the documented organic substrate, as confirmed by multidisciplinary evaluation, including neuropathic pain, unexplained muscular weakness, non-anatomical sensory deficits, allodynia, and hyperalgesia [148].
Malingering remains a challenging issue in medico-legal practice, mainly because there are sometimes significant difficulties in separating it from genuine psychological suffering. One of the most ethically and legally sensitive aspects of the medicolegal assessment is the potential misclassification of a genuine patient as a malingerer, which can seriously compromise both the quality of medical care and the integrity of legal proceedings [149].
Research has shown that current psychometric tools for detecting malingering have limited sensitivity and specificity, especially in psychiatric populations [150]. Therefore, a contextualized case-by-case analysis is essential, one that integrates the clinician’s experience with the available objective assessment tools to ensure accurate and ethically sound evaluations [151,152].
The differential diagnosis of posttraumatic neurological deficits often entails a multifaceted approach using both objective clinical methods and subjective evaluations. Quantifying neurological deficits is a critical aspect of forensic evaluations when assessing the severity of peripheral nerve injuries resulting from trauma [153].
This procedure mainly utilizes objective assessment methods, especially within medico-legal frameworks that depend exclusively on the objective evaluation of traumatic injuries and their effects, to create a definitive link between neurological harm and its influence on the claimant’s functional abilities [154].
Objective methods, such as electrodiagnostic tests and advanced neuroimaging, including high-resolution ultrasound and magnetic resonance neurography, provide quantifiable data regarding affected nerves’ anatomical and functional integrity, thus facilitating diagnosis, severity assessment, and prognosis [155,156,157]. Simultaneously, subjective methods, such as patient-reported outcome measures and standardized pain assessment tools, are essential for capturing nerve injury’s functional and psychosocial impact from the patient’s perspective, especially in chronic or neuropathic pain contexts [158,159,160].
A few approaches have been used to assess neuropathic pain, such as verbal rating scales, numeric rating scales, and visual analog scales, which are easy to use in clinical practice. More complex questionnaires are available that measure pain intensity and quality [161].
However, these questionnaires are usually complicated to include in practice because they are time-consuming and burdensome to analyze. The most frequently used and cited pain questionnaires are the McGill Pain Questionnaire, Self report-Leeds Assessment of Neuropathic Symptoms and Signs; RAND-36; Disability of Shoulder, Arm and Hand, designed to assess three components of pain (i.e., sensory, affective, and evaluative), but with little study evidence to support the benefit of their use [162,163].
Accurate techniques for assessing somatosensory function are essential in legal medicine scenarios concerning neuropathic pain, nerve injury from trauma, or complex regional pain syndrome. Quantitative Sensory Testing, along with electrophysiological assessments, are frequently employed methods that offer insights into the state of the sensory system [164]. Quantitative Sensory Testing is a psychophysical method used to assess sensory thresholds by examining reactions to controlled stimuli related to mechanical, thermal, and pain sensations, providing insights into the function of small-diameter myelinated (Aδ) and unmyelinated (C) fibers, which helps in the early detection of sensory deficits [165]. Quantitative Sensory Testing comprises static assessments that measure thresholds, identify hyperalgesia or hypoesthesia, and dynamic evaluations that indicate the central mechanisms of pain modulation [166,167]. Nonetheless, this method is subjective, reliant on patient cooperation and cognitive status, and does not permit precise localization of lesions [168].
8. Conclusions
The medical legal evaluation of PNIs needs a structured, interdisciplinary approach, integrating anatomical clinical, imaging and medical-legal principles and theories. This review aims to consolidate the foundational knowledge needed for an accurate diagnosis, the grading of the severity and the assessment of the timeline of the PNIs, which are often complex, and often further complicated by anatomical variations and limitations of diagnostic tools.
The tabulated data and tabulated framework provided here may be used as practical tools for medical-legal experts to increase consistency, reproducibility and objectivity in complex, expert analyses. Are emphasized the importance of recognizing anatomical variants, using appropriate imaging and electrodiagnostic methods, and understanding nerve regeneration patters associated with timeline markers, which are crucial for causation analysis and a proper differential diagnosis.
By promoting a systematic, scientifically grounded methodology, this review aims to further improve the activity of medical-legal experts by increasing the accuracy and defensibility of their opinions, therefore contributing to a more equitable, and evidence based judicial outcome.
Author Contributions
Conceptualization, S.H. and I.N.; methodology, S.H.; software, S.H.; investigation: all authors; writing—original draft preparation, S.H., O.-M.C. and E.P.; writing—review and editing, all authors; supervision, S.H. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Acknowledgments
During the preparation of this manuscript/study, the author(s) used Perplexity AI and Chat GPT for proofreading. The authors have reviewed and edited the output and take full responsibility for the content of this publication. Graphs were created with Biorender (https://www.biorender.com/) and ChatGPT 4-o.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Griffin, M.F.; Malahias, M.; Hindocha, S.; Wasim, S.K. Peripheral Nerve Injury: Principles for Repair and Regeneration. Open Orthop. J. 2014, 8, 199–203. [Google Scholar]
- Aman, M.; Zimmermann, K.S.; Thielen, M.; Thomas, B.; Daeschler, S.; Boecker, A.H.; Stolle, A.; Bigdeli, A.K.; Kneser, U.; Harhaus, L. An Epidemiological and Etiological Analysis of 5026 Peripheral Nerve Lesions from a European Level I Trauma Center. J. Pers. Med. 2022, 12, 1673. [Google Scholar] [CrossRef] [PubMed]
- Padovano, W.M.; Dengler, J.; Patterson, M.M.; Yee, A.; Snyder-Warwick, A.K.; Wood, M.D.; Moore, A.M.; Mackinnon, S.E. Incidence of Nerve Injury after Extremity Trauma in the United States. Hand 2022, 17, 615–623. [Google Scholar] [CrossRef] [PubMed]
- Magnéli, M.; Axenhus, M. Epidemiology and Regional Variance of Traumatic Peripheral Nerve Injuries in Sweden: A 15-Year Observational Study. PLoS ONE 2024, 19, e0310988. [Google Scholar] [CrossRef] [PubMed]
- Andrasfay, T.; Raymo, N.; Goldman, N.; Pebley, A.R. Physical Work Conditions and Disparities in Later Life Functioning: Potential Pathways. SSM Popul. Health 2021, 16, 100990. [Google Scholar] [CrossRef]
- Bergmeister, K.D.; Große-Hartlage, L.; Daeschler, S.C.; Rhodius, P.; Böcker, A.; Beyersdorff, M.; Kern, A.O.; Kneser, U.; Harhaus, L. Acute and Long-Term Costs of 268 Peripheral Nerve Injuries in the Upper Extremity. PLoS ONE 2020, 15, e0229530. [Google Scholar] [CrossRef]
- Huckhagel, T.; Nüchtern, J.; Regelsberger, J.; Gelderblom, M.; Lefering, R.; TraumaRegister DGU®. Nerve Trauma of the Lower Extremity: Evaluation of 60,422 Leg Injured Patients from the TraumaRegister DGU® between 2002 and 2015. Scand. J. Trauma Resusc. Emerg. Med. 2018, 26, 40. [Google Scholar] [CrossRef]
- Porzionato, A.; Macchi, V.; Stecco, C.; Boscolo-Berto, R.; Loukas, M.; Tubbs, R.S.; De Caro, R. Clinical Anatomy and Medical Malpractice-A Narrative Review with Methodological Implications. Healthcare 2022, 10, 1915. [Google Scholar] [CrossRef]
- Ku, V.; Cox, C.; Mikeska, A.; MacKay, B. Magnetic Resonance Neurography for Evaluation of Peripheral Nerves. J. Brachial Plex. Peripher. Nerve Inj. 2021, 16, e17–e23. [Google Scholar] [CrossRef]
- Dong, Y.; Alhaskawi, A.; Zhou, H.; Zou, X.; Liu, Z.; Ezzi, S.H.A.; Kota, V.G.; Abdulla, M.H.A.H.; Olga, A.; Abdalbary, S.A.; et al. Imaging Diagnosis in Peripheral Nerve Injury. Front. Neurol. 2023, 14, 1250808. [Google Scholar] [CrossRef]
- Elshewi, I.E.; Fatouh, M.M.; Mohamed, R.N.E.S.; Basheer, M.A.; El Liethy, N.E.; Abbas, H.M. Value of Ultrasound Assessment for Traumatic Nerve Injury of the Upper Limb. J. Ultrasound 2023, 26, 409–421. [Google Scholar] [CrossRef] [PubMed]
- Stark, M.M. Clinical Forensic Medicine: A Physician’s Guide, 3rd ed.; Humana Press: New York, NY, USA, 2011; ISBN 9781617792571. [Google Scholar]
- Orebaugh, S.L.; Bigeleisen, P.E.; McFadden, K. Connective Tissue and Peripheral Nerves. Reg. Anesth. Pain Med. 2013, 38, 70–71. [Google Scholar] [CrossRef] [PubMed]
- McMonagle, B.A. Peripheral Nerve Repair Using Olfactory Ensheathing and Stem Cells within a Vein Graft. In Connective Tissue Research; Taylor & Francis: Oxford, UK, 2025; pp. 1–12. [Google Scholar]
- Rosso, G.; Liashkovich, I.; Gess, B.; Young, P.; Kun, A.; Shahin, V. Unravelling Crucial Biomechanical Resilience of Myelinated Peripheral Nerve Fibres Provided by the Schwann Cell Basal Lamina and PMP22. Sci. Rep. 2014, 4, 7286. [Google Scholar] [CrossRef] [PubMed]
- Suter, U.; Scherer, S.S. Disease Mechanisms in Inherited Neuropathies. Nat. Rev. Neurosci. 2003, 4, 714–726. [Google Scholar] [CrossRef]
- Liu, Q.; Wang, X.; Yi, S. Pathophysiological Changes of Physical Barriers of Peripheral Nerves after Injury. Front. Neurosci. 2018, 12, 597. [Google Scholar] [CrossRef]
- Peltonen, S.; Alanne, M.; Peltonen, J. Barriers of the Peripheral Nerve. Tissue Barriers 2013, 1, e24956. [Google Scholar] [CrossRef]
- Le, E.L.H.; Allenby, T.H.; Fisher, M.; Constantine, R.S.; McNamara, C.T.; Barnhill, C.; Engemann, A.; Merced-O’Neill, O.; Iorio, M.L. Intraneural Topography and Branching Patterns of the Common Peroneal Nerve: Studying the Feasibility of Distal Nerve Transfers. Plast. Reconstr. Surg. Glob. Open 2024, 12, e6258. [Google Scholar] [CrossRef]
- Kerns, J.M. The Microstructure of Peripheral Nerves. Tech. Reg. Anesth. Pain Manag. 2008, 12, 127–133. [Google Scholar] [CrossRef]
- Koppaka, S.; Hess-Dunning, A.; Tyler, D.J. Biomechanical Characterization of Isolated Epineurial and Perineurial Membranes of Rabbit Sciatic Nerve. J. Biomech. 2022, 136, 111058. [Google Scholar] [CrossRef]
- Palladino, S.P.; Helton, E.S.; Jain, P.; Dong, C.; Crowley, M.R.; Crossman, D.K.; Ubogu, E.E. The Human Blood-Nerve Barrier Transcriptome. Sci. Rep. 2017, 7, 17477. [Google Scholar] [CrossRef]
- De Stefano, V.; Za, T.; Ciminello, A.; Betti, S.; Rossi, E. Causes of Adult Splanchnic Vein Thrombosis in the Mediterranean Area. Mediterr. J. Hematol. Infect. Dis. 2011, 3, e2011063. [Google Scholar] [CrossRef] [PubMed]
- Brull, R.; Hadzic, A.; Reina, M.A.; Barrington, M.J. Pathophysiology and Etiology of Nerve Injury Following Peripheral Nerve Blockade. Reg. Anesth. Pain Med. 2015, 40, 479–490. [Google Scholar] [CrossRef] [PubMed]
- Prahm, C.; Heinzel, J.; Kolbenschlag, J. Blood Supply and Microcirculation of the Peripheral Nerve. In Peripheral Nerve Tissue Engineering and Regeneration; Springer International Publishing: Cham, Switzerland, 2022; pp. 35–79. ISBN 9783030210519. [Google Scholar]
- Peng, T.-H.; Ding, H.-M.; Chen, S.-H.; Tang, M.-L.; Hong, L.; Tan, J.-G.; Wang, A.-P.; Xu, D.-C. Demonstration of Three Injection Methods for the Analysis of Extrinsic and Intrinsic Blood Supply of the Peripheral Nerve. Surg. Radiol. Anat. 2009, 31, 567–571. [Google Scholar] [CrossRef]
- Kamel, I.; Barnette, R. Positioning Patients for Spine Surgery: Avoiding Uncommon Position-Related Complications. World J. Orthop. 2014, 5, 425–443. [Google Scholar] [CrossRef]
- Boissaud-Cooke, M.; Pidgeon, T.; Tunstall, R. The Microcirculation of Peripheral Nerves: The Vasa Nervorum. In Nerves and Nerve Injuries; Academic Press: Cambridge, MA, USA, 2015; pp. 507–523. [Google Scholar]
- Kuo, F.; Park, J.; Chow, K.; Chen, A.; Walsworth, M.K. Avoiding Peripheral Nerve Injury in Arterial Interventions. Diagn. Interv. Radiol. 2019, 25, 380–391. [Google Scholar] [CrossRef]
- Branca, J.J.V.; Guarnieri, G.; Morelli, A.; Benedini, C.; Fagni, N.; Gulisano, M.; Pacini, A.; Paternostro, F. Sciatic Nerve and Its Anatomical Variations: In-Depth Understanding Acquired during Dissection Classes. Cureus 2024, 16, e60083. [Google Scholar] [CrossRef]
- Poutoglidou, F.; Piagkou, M.; Totlis, T.; Tzika, M.; Natsis, K. Sciatic Nerve Variants and the Piriformis Muscle: A Systematic Review and Meta-Analysis. Cureus 2020, 12, e11531. [Google Scholar] [CrossRef]
- Reynoso, J.P.; De Jesus Encarnacion, M.; Nurmukhametov, R.; Melchenko, D.; Efe, I.E.; Goncharov, E.; Taveras, A.A.; Ramirez Pena, I.J.; Montemurro, N. Anatomical Variations of the Sciatic Nerve Exit from the Pelvis and Its Relationship with the Piriformis Muscle: A Cadaveric Study. Neurol. Int. 2022, 14, 894–902. [Google Scholar] [CrossRef]
- Lezak, B.; Massel, D.H.; Varacallo, M.A. Peroneal Nerve Injury. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2025. [Google Scholar]
- Hada, S.; Kadel, M.; Pandit, T.K.; Basnet, K.S. Variations in Formation of Median Nerve: A Cadaveric Study. J. Chitwan Med. Coll. 2020, 10, 66–68. [Google Scholar] [CrossRef]
- Agarwal, P.; Gupta, S.; Yadav, P.; Sharma, D. Cadaveric Study of Anatomical Variations of the Median Nerve and Persistent Median Artery at Wrist. Indian J. Plast. Surg. 2014, 47, 95–101. [Google Scholar] [CrossRef]
- Encarnacion, M.; Nurmukhametov, R.; Barrientos, R.E.; Melchenko, D.; Goncharov, E.; Bernard, E.; Huerta, J.M.; Uhl, J.F.; Efe, I.E.; Montemurro, N.; et al. Anatomical Variations of the Median Nerve: A Cadaveric Study. Neurol. Int. 2022, 14, 664–672. [Google Scholar] [CrossRef] [PubMed]
- Henry, B.M.; Zwinczewska, H.; Roy, J.; Vikse, J.; Ramakrishnan, P.K.; Walocha, J.A.; Tomaszewski, K.A. The Prevalence of Anatomical Variations of the Median Nerve in the Carpal Tunnel: A Systematic Review and Meta-Analysis. PLoS ONE 2015, 10, e0136477. [Google Scholar] [CrossRef] [PubMed]
- Lanz, U. Anatomical Variations of the Median Nerve in the Carpal Tunnel. J. Hand Surg. Am. 1977, 2, 44–53. [Google Scholar] [CrossRef] [PubMed]
- Poisel, S. Ursprung Und Verlauf Des Ramus Muscularis Des Nervus Digitalis Palmaris Communis I (N. Medianus). Chir Praxis 1974, 18, 471–474. [Google Scholar]
- Delgado-Martínez, I.; Badia, J.; Pascual-Font, A.; Rodríguez-Baeza, A.; Navarro, X. Fascicular Topography of the Human Median Nerve for Neuroprosthetic Surgery. Front. Neurosci. 2016, 10, 286. [Google Scholar] [CrossRef]
- Jo, G.; Mf, G. Intraneural Topography of the Extratemporal Facial Nerve: Microsurgical Nerve Reconstruction. J. Craniofacial Surg. 2007, 18, 578–585. [Google Scholar]
- Millesi, H.; Rath, T.; Reihsner, R.; Zoch, G. Microsurgical Neurolysis: Its Anatomical and Physiological Basis and Its Classification. Microsurgery 1993, 14, 430–439. [Google Scholar] [CrossRef]
- Golarz, S.R.; White, J.M. Anatomic Variation of the Phrenic Nerve and Brachial Plexus Encountered during 100 Supraclavicular Decompressions for Neurogenic Thoracic Outlet Syndrome with Associated Postoperative Neurologic Complications. Ann. Vasc. Surg. 2020, 62, 70–75. [Google Scholar] [CrossRef]
- Sonawane, K.; Dixit, H.; Jayaraj, A.; Thota, N.; Sekar, C. “Knowing It before Blocking It,” the ABCD of the Peripheral Nerves: Part A (Nerve Anatomy and Physiology). Cureus 2023, 15, e41771. [Google Scholar] [CrossRef]
- Wu, Z.; Wang, Y. Development of Guidance Techniques for Regional Anesthesia: Past, Present and Future. J. Pain Res. 2021, 14, 1631–1641. [Google Scholar] [CrossRef]
- Orellana-Donoso, M.; Valenzuela-Fuenzalida, J.J.; Gold-Semmler, M.; Guernica-Garcia-Gorigoitia; Shane-Tubbs, R.; Santana-Machuca, E. Neural Entrapments Associated with Musculoskeletal Anatomical Variations of the Upper Limb: Literature Review. Transl. Res. Anat. 2021, 22, 100094. [Google Scholar] [CrossRef]
- Rydevik, B.; Brown, M.D.; Lundborg, G. Pathoanatomy and Pathophysiology of Nerve Root Compression. Spine 1984, 9, 7–15. [Google Scholar] [CrossRef] [PubMed]
- Rempel, D.; Dahlin, L.; Lundborg, G. Pathophysiology of Nerve Compression Syndromes: Response of Peripheral Nerves to Loading. J. Bone Jt. Surg. Am. 1999, 81, 1600–1610. [Google Scholar] [CrossRef] [PubMed]
- Khan, I.A.; Mahabadi, N.; D’Abarno, A.; Varacallo, M. Anatomy, Bony Pelvis and Lower Limb, Leg Lateral Compartment. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2018. [Google Scholar]
- Martinoli, C.; Perez, M.M.; Padua, L.; Valle, M.; Capaccio, E.; Altafini, L.; Michaud, J.; Tagliafico, A. Muscle Variants of the Upper and Lower Limb (with Anatomical Correlation). Semin. Musculoskelet. Radiol. 2010, 14, 106–121. [Google Scholar] [CrossRef]
- de Ridder, V.D.; de Lange, S.; Popta, J.V. Anatomical Variations of the Lateral Femoral Cutaneous Nerve and the Consequences for Surgery. J. Orthop. Trauma 1999, 13, 207–211. [Google Scholar] [CrossRef]
- De Maeseneer, M.; Madani, H.; Lenchik, L.; Kalume Brigido, M.; Shahabpour, M.; Marcelis, S.; de Mey, J.; Scafoglieri, A. Normal Anatomy and Compression Areas of Nerves of the Foot and Ankle: US and MR Imaging with Anatomic Correlation. Radiographics 2015, 35, 1469–1482. [Google Scholar] [CrossRef]
- Valenzuela-Fuenzalida, J.; Inostroza-Wegner, A.; Osorio-Muñoz, F.; Milos-Brandenberg, D.; Santana-Machuca, A.; Baeza, P.N.; Donoso, M.O.; Bruna-Mejías, A.; Iwanaga, J.; Sanchis-Gimeno, J.; et al. The Association between Anatomical Variants of Musculoskeletal Structures and Nerve Compressions of the Lower Limb: A Systematic Review and Meta-Analysis. Diagnostics 2024, 14, 695. [Google Scholar] [CrossRef]
- Martinoli, C.; Bianchi, S.; Gandolfo, N.; Valle, M.; Simonetti, S.; Derchi, L.E. US of Nerve Entrapments in Osteofibrous Tunnels of the Upper and Lower Limbs. Radiographics 2000, 20, S199–S213; discussion S213–S217. [Google Scholar] [CrossRef]
- Ochoa, J.; Fowler, T.J.; Gilliatt, R.W. Anatomical Changes in Peripheral Nerves Compressed by a Pneumatic Tourniquet. J. Anat. 1972, 113, 433–455. [Google Scholar]
- Ghosh, S.K.; Raheja, S.; Tuli, A. Potential Sites of Compression of Tibial Nerve Branches in Foot: A Cadaveric and Imaging Study: Abductor Hallucis Muscle and Tibial Nerve Compression. Clin. Anat. 2013, 26, 768–779. [Google Scholar] [CrossRef]
- Adibatti, M.; Sangeetha, V. Study on Variant Anatomy of Sciatic Nerve. J. Clin. Diagn. Res. 2014, 8, AC07–AC09. [Google Scholar] [CrossRef] [PubMed]
- Raza, K.; Singh, S.; Rani, N.; Mishra, R.; Mehta, K.; Kaler, S. Anomalous Innervation of the Median Nerve in the Arm in the Absence of the Musculocutaneous Nerve. Sultan Qaboos Univ. Med. J. 2017, 17, e106–e108. [Google Scholar] [CrossRef] [PubMed]
- Zdilla, M.J.; Pacurari, P.; Celuck, T.J.; Andrews, R.C.; Lambert, H.W. A Gantzer Muscle Arising from the Brachialis and Flexor Digitorum Superficialis: Embryological Considerations and Implications for Median Nerve Entrapment. Anat. Sci. Int. 2019, 94, 150–153. [Google Scholar] [CrossRef]
- Afshar, A. Ulnar Tunnel Syndrome Due to an Aberrant Muscle. Arch. Iran. Med. 2015, 18, 58–59. [Google Scholar]
- Ardouin, L.; Lecoq, F.-A.; Le Nen, D.; Herrou, P. An Ultrasound Diagnostic Aid in Hand Surgery: Observation on a Supernumerary Muscle in the Wrist. Chir. Main 2014, 33, 401–403. [Google Scholar] [CrossRef]
- Bladt, L.; Vankan, Y.; Demeyere, A.; Perdieus, D. Bilateral Ulnar Nerve Compression by Anconeus Epitrochlearis Muscle. JBR-BTR 2009, 92, 120. [Google Scholar]
- Erdem Bagatur, A.; Yalcin, M.B.; Ozer, U.E. Anconeus Epitrochlearis Muscle Causing Ulnar Neuropathy at the Elbow: Clinical and Neurophysiological Differential Diagnosis. Orthopedics 2016, 39, e988–e991. [Google Scholar] [CrossRef]
- Kumar, P.; John, R.; Sharma, G.K.; Aggarwal, S. Aberrant Course of Superficial Radial Nerve in the Forearm: An Anatomical Variation and Its Clinical Implications. BMJ Case Rep. 2017, 2017, bcr-2017. [Google Scholar] [CrossRef]
- Moore, C.W.; Rice, C.L. Rare Muscular Variations Identified in a Single Cadaveric Upper Limb: A Four-Headed Biceps Brachii and Muscular Elevator of the Latissimus Dorsi Tendon. Anat. Sci. Int. 2018, 93, 311–316. [Google Scholar] [CrossRef]
- Dostal, G.H.; Lister, G.D.; Hutchinson, D.; Mogan, J.V.; Davis, P.H. Extensor Digitorum Brevis Manus Associated with a Dorsal Wrist Ganglion: A Reivew of Five Cases. J. Hand Surg. Am. 1995, 20, 35–37. [Google Scholar] [CrossRef]
- Shereen, R.; Loukas, M.; Tubbs, R.S. Extensor Digitorum Brevis Manus: A Comprehensive Review of This Variant Muscle of the Dorsal Hand. Cureus 2017, 9, e1568. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Niedenführ, M.; Vázquez, T.; Golanó, P.; Parkin, I.; Sañudo, J.R. Extensor Digitorum Brevis Manus: Anatomical, Radiological and Clinical Relevance. A Review. Clin. Anat. 2002, 15, 286–292. [Google Scholar] [CrossRef]
- Pirola, E.; Hébert-Blouin, M.-N.; Amador, N.; Amrami, K.K.; Spinner, R.J. Palmaris Profundus: One Name, Several Subtypes, and a Shared Potential for Nerve Compression. Clin. Anat. 2009, 22, 643–648. [Google Scholar] [CrossRef] [PubMed]
- Elias, L.S.; Schulter-Ellis, F.P. Anomalous Flexor Superficialis Indicis: Two Case Reports and Literature Review. J. Hand Surg. Am. 1985, 10, 296–299. [Google Scholar] [CrossRef] [PubMed]
- Al-Qattan, M.M. Ulnar Nerve Compression at the Wrist by the Accessory Abductor Digiti Minimi Muscle: Wrist Trauma as a Precipitating Factor. Hand Surg. 2004, 9, 79–82. [Google Scholar] [CrossRef]
- Ayik, G.; Kolac, U.C.; Kaymakoglu, M.; McFarland, E.; Huri, G. Dark Side of the Shoulder: Suprascapular and Axillary Nerve Compressions. Int. Orthop. 2025, 49, 1153–1165. [Google Scholar] [CrossRef]
- Olewnik, Ł.; Paulsen, F.; Tubbs, R.S.; Zielińska, N.; Szewczyk, B.; Karauda, P.; Polguj, M. Potential Compression of the Musculocutaneous, Median and Ulnar Nerves by a Very Rare Variant of the Coracobrachialis Longus Muscle. Folia Morphol. 2021, 80, 707–713. [Google Scholar] [CrossRef]
- Pećina, M.; Bojanić, I. Musculocutaneous Nerve Entrapment in the Upper Arm. Int. Orthop. 1993, 17, 232–234. [Google Scholar] [CrossRef]
- Swain, R. Musculocutaneous Nerve Entrapment: A Case Report. Clin. J. Sport Med. 1995, 5, 196–198. [Google Scholar] [CrossRef]
- Schwabl, C.; Hörmann, R.; Strolz, C.J.; Drakonaki, E.; Zimmermann, R.; Klauser, A.S. Anatomical Variants of the Upper Limb Nerves: Clinical and Preoperative Relevance. Semin. Musculoskelet. Radiol. 2023, 27, 129–135. [Google Scholar] [CrossRef]
- Kaushal, P.; Jessy, J.P.; Ganapathy, A. Median Nerve Entrapment by Superficial Brachioulnar Artery: Anatomical Insights and Clinical Perspective. Cureus 2024, 16, e66228. [Google Scholar] [CrossRef] [PubMed]
- Bateman, E.A.; Pripotnev, S.; Larocerie-Salgado, J.; Ross, D.C.; Miller, T.A. Assessment, Management, and Rehabilitation of Traumatic Peripheral Nerve Injuries for Non-Surgeons. Muscle Nerve 2025, 71, 696–714. [Google Scholar] [CrossRef] [PubMed]
- Rowland, L.P. Merritt’s Neurology Textbook 10/E & Handbook Package, 10th ed.; Lippincott Williams and Wilkins: Philadelphia, PA, USA, 2001; ISBN 9780781737814. [Google Scholar]
- Campbell, W.W. Evaluation and Management of Peripheral Nerve Injury. Clin. Neurophysiol. 2008, 119, 1951–1965. [Google Scholar] [CrossRef]
- Magee, D.J.; Manske, R.C. Orthopedic Physical Assessment, 7th ed.; Saunders: Philadelphia, PA, USA, 2021; ISBN 9780323749510. [Google Scholar]
- Seddon, H.J. Three Types of Nerve Injury. Brain 1943, 66, 237–288. [Google Scholar] [CrossRef]
- Sunderland, S. A Classification of Peripheral Nerve Injuries Producing Loss of Function. Brain 1951, 74, 491–516. [Google Scholar] [CrossRef]
- Chhabra, A.; Ahlawat, S.; Belzberg, A.; Andreseik, G. Peripheral Nerve Injury Grading Simplified on MR Neurography: As Referenced to Seddon and Sunderland Classifications. Indian J. Radiol. Imaging 2014, 24, 217–224. [Google Scholar] [CrossRef]
- Netscher, D.; Murphy, K.; Fiore, N.A. Hand Surgery: Ch. 70 Nerve Compression Syndrome. In Townsend: Sabiston Textbook Surgery; Townsend, C.M., Beauchamp, R.D., Evers, B.M., Mattox, K.L., Eds.; Elsevier: Amsterdam, The Netherlands, 2012; pp. 1982–1984. [Google Scholar]
- Burnett, M.G.; Zager, E.L. Pathophysiology of Peripheral Nerve Injury: A Brief Review. Neurosurg. Focus 2004, 16, E1. [Google Scholar] [CrossRef]
- Sunderland, S. The Anatomy and Physiology of Nerve Injury. Muscle Nerve 1990, 13, 771–784. [Google Scholar] [CrossRef]
- Rochkind, S.; Strauss, I.; Shlitner, Z.; Alon, M.; Reider, E.; Graif, M. Clinical Aspects of Ballistic Peripheral Nerve Injury: Shrapnel versus Gunshot. Acta Neurochir. 2014, 156, 1567–1575. [Google Scholar] [CrossRef]
- Hagert, E. The Clinical Triad: A Structured Approach to Diagnosing Peripheral Nerve Compressions. Int. Orthop. 2025, 49, 899–909. [Google Scholar] [CrossRef]
- John, A.A.; Rossettie, S.; Rafael, J.; Cox, C.T.; Ducic, I.; Mackay, B.J. Clinical Assessment of Pain and Sensory Function in Peripheral Nerve Injury and Recovery: A Systematic Review of Literature. Arch. Plast. Surg. 2022, 49, 427–439. [Google Scholar] [CrossRef] [PubMed]
- Meyer, R.A.; Bagheri, S.C. Clinical Evaluation of Nerve Injuries. In Trigeminal Nerve Injuries; Springer Berlin Heidelberg: Berlin/Heidelberg, Germany, 2013; pp. 167–198. ISBN 9783642355387. [Google Scholar]
- Sonawane, K.; Rao, P.; Haripriya, T.; Mistry, T.; Sekar, C. Shedding Light on Perioperative Nerve Injury: An Investigation Using the SHED (Symptoms Categorization-History Taking-Examination-Diagnostic Evaluations) Approach. Cureus 2024, 16, e54133. [Google Scholar] [CrossRef] [PubMed]
- Hagert, E. Clinical Diagnosis and Wide-Awake Surgical Treatment of Proximal Median Nerve Entrapment at the Elbow: A Prospective Study. Hand 2013, 8, 41–46. [Google Scholar] [CrossRef] [PubMed]
- Brooks, J.; Hardie, C.; Wade, R.; Teh, I.; Bourke, G. Diagnostic Accuracy of MRI for Detecting Nerve Injury in Brachial Plexus Birth Injury. Br. J. Radiol. 2025, 98, 36–44. [Google Scholar] [CrossRef]
- Kollmer, J.; Bendszus, M. Magnetic Resonance Neurography: Improved Diagnosis of Peripheral Neuropathies. Neurotherapeutics 2021, 18, 2368–2383. [Google Scholar] [CrossRef]
- Bangia, M.; Ahmadzai, I.; Casselman, J.; Politis, C.; Jacobs, R.; Van der Cruyssen, F. Accuracy of MR Neurography as a Diagnostic Tool in Detecting Injuries to the Lingual and Inferior Alveolar Nerve in Patients with Iatrogenic Post-Traumatic Trigeminal Neuropathy. Eur. Radiol. 2024, 34, 4619–4627. [Google Scholar] [CrossRef]
- Lee, S.K.; Serhal, A.M.; Serhal, M.; Michalek, J.; Omar, I.M. The Role of High-Resolution Ultrasound and MRI in the Evaluation of Peripheral Nerves in the Lower Extremity. J. Ultrason. 2023, 23, e328–e346. [Google Scholar] [CrossRef]
- Feng, Y.; Su, X.; Zheng, C.; Lu, Z. The Noninvasive Diagnostic Value of MRN for CIDP: A Research from Qualitative to Quantitative. Spine 2020, 45, 1506–1512. [Google Scholar] [CrossRef]
- Van der Cruyssen, F.; Peeters, F.; Croonenborghs, T.-M.; Fransen, J.; Renton, T.; Politis, C.; Casselman, J.; Jacobs, R. A Systematic Review on Diagnostic Test Accuracy of Magnetic Resonance Neurography versus Clinical Neurosensory Assessment for Post-Traumatic Trigeminal Neuropathy in Patients Reporting Neurosensory Disturbance. Dentomaxillofac. Radiol. 2021, 50, 20200103. [Google Scholar] [CrossRef]
- Voser, T.; Martin, M.; Muriset, I.; Winkler, M.; Ledoux, J.-B.; Alemán-Gómez, Y.; Durand, S. Outcome Prediction by Diffusion Tensor Imaging (DTI) in Patients with Traumatic Injuries of the Median Nerve. Neurol. Int. 2024, 16, 1026–1038. [Google Scholar] [CrossRef]
- Pridmore, M.D.; Glassman, G.E.; Pollins, A.C.; Manzanera Esteve, I.V.; Drolet, B.C.; Weikert, D.R.; Does, M.D.; Perdikis, G.; Thayer, W.P.; Dortch, R.D. Initial Findings in Traumatic Peripheral Nerve Injury and Repair with Diffusion Tensor Imaging. Ann. Clin. Transl. Neurol. 2021, 8, 332–347. [Google Scholar] [CrossRef] [PubMed]
- Yang, H.; Son, N.-H.; Kim, D.; Chun, J.-H.; Kim, J.S.; Oh, T.K.; Lee, M.; Kim, H.J. Assessment of Traumatic Mandibular Nerve Using MR Neurography Sequence: A Preliminary Study. BMC Oral Health 2024, 24, 750. [Google Scholar] [CrossRef] [PubMed]
- Bourke, G.; Wade, R.G.; van Alfen, N. Updates in Diagnostic Tools for Diagnosing Nerve Injury and Compressions. J. Hand Surg. Eur. Vol. 2024, 49, 668–680. [Google Scholar] [CrossRef]
- Deka, J.B.; Shah, R.; Jiménez, M.; Bhatnagar, N.; Bravo-Sánchez, A.; Piñas-Bonilla, I.; Abián-Vicén, J.; Jiménez, F. A Retrospective Analysis of High Resolution Ultrasound Evaluation of the “Split Fat Sign” in Peripheral Nerve Sheath Tumors. Healthcare 2023, 11, 3147. [Google Scholar] [CrossRef]
- Pedro, M.T.; Antoniadis, G.; Scheuerle, A.; Pham, M.; Wirtz, C.R.; Koenig, R.W. Intraoperative High-Resolution Ultrasound and Contrast-Enhanced Ultrasound of Peripheral Nerve Tumors and Tumorlike Lesions. Neurosurg. Focus 2015, 39, E5. [Google Scholar] [CrossRef]
- Miwa, T.; Miwa, H. Ultrasonography of Carpal Tunnel Syndrome: Clinical Significance and Limitations in Elderly Patients. Intern. Med. 2011, 50, 2157–2161. [Google Scholar] [CrossRef]
- Eroğlu, A.; Sarı, E.; Topuz, A.K.; Şimşek, H.; Pusat, S. Recurrent Carpal Tunnel Syndrome: Evaluation and Treatment of the Possible Causes. World J. Clin. Cases 2018, 6, 365–372. [Google Scholar] [CrossRef]
- Gervasio, A.; Stelitano, C.; Bollani, P.; Giardini, A.; Vanzetti, E.; Ferrari, M. Carpal Tunnel Sonography. J. Ultrasound 2020, 23, 337–347. [Google Scholar] [CrossRef]
- Agarwal, A.; Chandra, A.; Jaipal, U.; Bagarhatta, M.; Mendiratta, K.; Goyal, A.; Kumar, R.; Mangalhara, N. Can Imaging Be the New Yardstick for Diagnosing Peripheral Neuropathy?—A Comparison between High Resolution Ultrasound and MR Neurography with an Approach to Diagnosis. Insights Imaging 2019, 10, 104. [Google Scholar] [CrossRef]
- Jackson, L.J.; Serhal, M.; Omar, I.M.; Garg, A.; Michalek, J.; Serhal, A. Sural Nerve: Imaging Anatomy and Pathology. Br. J. Radiol. 2023, 96, 20220336. [Google Scholar] [CrossRef]
- Weis, J.; Brandner, S.; Lammens, M.; Sommer, C.; Vallat, J.-M. Processing of Nerve Biopsies: A Practical Guide for Neuropathologists. Clin. Neuropathol. 2012, 31, 7–23. [Google Scholar] [CrossRef] [PubMed]
- Nathani, D.; Spies, J.; Barnett, M.H.; Pollard, J.; Wang, M.-X.; Sommer, C.; Kiernan, M.C. Nerve Biopsy: Current Indications and Decision Tools. Muscle Nerve 2021, 64, 125–139. [Google Scholar] [CrossRef] [PubMed]
- Hostiuc, S.; Rusu, M.C.; Mănoiu, V.S.; Vrapciu, A.D.; Negoi, I.; Popescu, M.V. Usefulness of ultrastructure studies for the estimation of the postmortem interval. A systematic review. Rom. J. Morphol. Embryol. 2017, 58, 377–384. [Google Scholar] [PubMed]
- Kamble, N.; Shukla, D.; Bhat, D. Peripheral Nerve Injuries: Electrophysiology for the Neurosurgeon. Neurol. India 2019, 67, 1419–1422. [Google Scholar] [CrossRef]
- Bridgeman, C.; Naidu, S.; Kothari, M.J. Clinical and Electrophysiological Presentation of Pronator Syndrome. Electromyogr. Clin. Neurophysiol. 2007, 47, 89–92. [Google Scholar]
- Campbell, W.W.; Carroll, C.; Landau, M.E. Ulnar Neuropathy at the Elbow: Five New Things. Neurol. Clin. Pract. 2015, 5, 35–41. [Google Scholar] [CrossRef]
- Kleggetveit, I.P.; Jørum, E. Large and Small Fiber Dysfunction in Peripheral Nerve Injuries with or without Spontaneous Pain. J. Pain 2010, 11, 1305–1310. [Google Scholar] [CrossRef]
- Stassart, R.M.; Fledrich, R.; Velanac, V.; Brinkmann, B.G.; Schwab, M.H.; Meijer, D.; Sereda, M.W.; Nave, K.-A. A Role for Schwann Cell-Derived Neuregulin-1 in Remyelination. Nat. Neurosci. 2013, 16, 48–54. [Google Scholar] [CrossRef]
- Seddon, H. Surgical Disorders of the Peripheral Nerves; Churchill Livingstone: London, UK, 1975. [Google Scholar]
- Sunderland, S.; Smith, J.W. Nerves and Nerve Injuries. Plast. Reconstr. Surg. 1969, 44, 601. [Google Scholar] [CrossRef]
- Robinson, L.R. Predicting Recovery from Peripheral Nerve Trauma. Phys. Med. Rehabil. Clin. N. Am. 2018, 29, 721–733. [Google Scholar] [CrossRef]
- Kim, Y.; 편성범. Evaluation of Recovery and Prognosis after Peripheral Nerve Injury. J. Korean Assoc. EMG Electrodiagn. Med. 2017, 19, 52–60. [Google Scholar]
- Haase, J.; Bjerre, P.; Simesen, K. Median and Ulnar Nerve Transections Treated with Microsurgical Interfascicular Cable Grafting with Autogenous Sural Nerve. J. Neurosurg. 1980, 53, 73–84. [Google Scholar] [CrossRef] [PubMed]
- Secer, H.I.; Daneyemez, M.; Tehli, O.; Gonul, E.; Izci, Y. The Clinical, Electrophysiologic, and Surgical Characteristics of Peripheral Nerve Injuries Caused by Gunshot Wounds in Adults: A 40-Year Experience. Surg. Neurol. 2008, 69, 143–152. [Google Scholar] [CrossRef] [PubMed]
- Kabak, S.; Halici, M.; Baktir, A.; Türk, C.Y.; Avşarogullari, L. Results of Treatment of the Extensive Volar Wrist Lacerations: “The Spaghetti Wrist”. Eur. J. Emerg. Med. 2002, 9, 71–76. [Google Scholar] [CrossRef]
- Gu, Y.D. To Improve the Diagnosis and Treatment of Peripheral Nerve Injuries. J. Chin. Orthop. Trauma 2003, 5. Available online: http://en.cnki.com.cn/Article_en/CJFDTOTAL-ZCGK200301000.htm (accessed on 18 May 2025).
- Meek, M.F.; Coert, J.H. Clinical Use of Nerve Conduits in Peripheral-Nerve Repair: Review of the Literature. J. Reconstr. Microsurg. 2002, 18, 97–109. [Google Scholar] [CrossRef]
- Bell, J.H.A.; Haycock, J.W. Next Generation Nerve Guides: Materials, Fabrication, Growth Factors, and Cell Delivery. Tissue Eng. Part B Rev. 2012, 18, 116–128. [Google Scholar] [CrossRef]
- Hostiuc, S.; Teodoru, D.; Isailă, O.; Buda, O.; Costescu, M. Tratat de Medicină Legală Odontostomatologică; Hostiuc, S., Ed.; All: București, Romania, 2020. [Google Scholar]
- Menorca, R.M.G.; Fussell, T.S.; Elfar, J.C. Nerve Physiology: Mechanisms of Injury and Recovery. Hand Clin. 2013, 29, 317–330. [Google Scholar] [CrossRef]
- Sonawane, K.; Dixit, H.; Thota, N.; Jayaraj, A.; Balavenkatasubramanian, J. “knowing It before Blocking It,” the ABCD of the Peripheral Nerves: Part D (Approach to the Patient with Nerve Injuries). Cureus 2023, 15, e41782. [Google Scholar] [CrossRef]
- Ferrara, S.D.; Baccino, E.; Bajanowski, T.; Boscolo-Berto, R.; Castellano, M.; De Angel, R.; Pauliukevičius, A.; Ricci, P.; Vanezis, P.; Vieira, D.N.; et al. Malpractice and Medical Liability. European Guidelines on Methods of Ascertainment and Criteria of Evaluation. Int. J. Legal Med. 2013, 127, 545–557. [Google Scholar] [CrossRef]
- Gibelli, F.; Ricci, G.; Sirignano, A.; Bailo, P.; De Leo, D. Iatrogenic Femoral Nerve Injuries: Analysis of Medico-Legal Issues through a Scoping Review Approach. Ann. Med. Surg. 2021, 72, 103055. [Google Scholar] [CrossRef] [PubMed]
- Pieri, M.; Maldonado, A.L.; Ros, M.M.; Massoni, F.; Ricci, S.; Vacchiano, G. Post-Mortem Morphological Alterations of Human Peripheral Nerve. Aust. J. Forensic Sci. 2019, 51, 340–347. [Google Scholar] [CrossRef]
- Vacchiano, G.; Maldonado, A.L.; Ros, M.M.; Di Lorenzo, P.; Pieri, M. The Cholesterol Levels in Median Nerve and Post-Mortem Interval Evaluation. Forensic Sci. Int. 2016, 265, 29–33. [Google Scholar] [CrossRef] [PubMed]
- Hostiuc, S.; Pirici, D.; Negoi, I.; Ion, D.A.; Ceausu, M. Detection of Diffuse Axonal Injury in Forensic Pathology. Rom. J. Leg. Med. 2014, 22, 145–152. [Google Scholar] [CrossRef]
- Rotshenker, S. Wallerian Degeneration: The Innate-Immune Response to Traumatic Nerve Injury. J. Neuroinflammation 2011, 8, 109. [Google Scholar] [CrossRef]
- Compston, A. Aids to the Investigation of Peripheral Nerve Injuries. Saunders Elsevier: 2010; pp. [8] 64 and 94 Figures. Brain 2010, 133, 2838–2844. [Google Scholar] [CrossRef]
- Przywara, S. Importance of Medial Antebrachial Cutaneous Nerve Anatomical Variations in Upper Arm Surgery. J. Neurosci. Rural Pract. 2016, 7, 337–338. [Google Scholar] [CrossRef]
- van Gelein Vitringa, V.M.; van Kooten, E.O.; Jaspers, R.T.; Mullender, M.G.; van Doorn-Loogman, M.H.; van der Sluijs, J.A. An MRI Study on the Relations between Muscle Atrophy, Shoulder Function and Glenohumeral Deformity in Shoulders of Children with Obstetric Brachial Plexus Injury. J. Brachial Plex. Peripher. Nerve Inj. 2009, 4, 9. [Google Scholar]
- Kraft, G.H. Fibrillation Potential Amplitude and Muscle Atrophy Following Peripheral Nerve Injury. Muscle Nerve 1990, 13, 814–821. [Google Scholar] [CrossRef]
- Grinsell, D.; Keating, C.P. Peripheral Nerve Reconstruction after Injury: A Review of Clinical and Experimental Therapies. Biomed. Res. Int. 2014, 2014, 698256. [Google Scholar] [CrossRef]
- Kramer, C.; Jordan, D.; Kretschmer, A.; Lehmeyer, V.; Kellermann, K.; Schaller, S.J.; Blobner, M.; Kochs, E.F.; Fink, H. Electromyographic Permutation Entropy Quantifies Diaphragmatic Denervation and Reinnervation. PLoS ONE 2014, 9, e115754. [Google Scholar] [CrossRef] [PubMed]
- Pond, A.; Marcante, A.; Zanato, R.; Martino, L.; Stramare, R.; Vindigni, V.; Zampieri, S.; Hofer, C.; Kern, H.; Masiero, S.; et al. History, Mechanisms and Clinical Value of Fibrillation Analyses in Muscle Denervation and Reinnervation by Single Fiber Electromyography and Dynamic Echomyography. Eur. J. Transl. Myol. 2014, 24, 3297. [Google Scholar] [CrossRef] [PubMed]
- Wu, P.; Chawla, A.; Spinner, R.J.; Yu, C.; Yaszemski, M.J.; Windebank, A.J.; Wang, H. Key Changes in Denervated Muscles and Their Impact on Regeneration and Reinnervation. Neural Regen. Res. 2014, 9, 1796–1809. [Google Scholar] [PubMed]
- Partanen, J.V. A Rare Type of Fibrillation-like EMG Activity. Clin. Neurophysiol. Pract. 2017, 2, 65–66. [Google Scholar] [CrossRef]
- James, G. Dsm-5-Tr; Independently Published: Chicago, IL, USA, 2023; ISBN 9798854066068. [Google Scholar]
- Greve, K.W.; Ord, J.S.; Bianchini, K.J.; Curtis, K.L. Prevalence of Malingering in Patients with Chronic Pain Referred for Psychologic Evaluation in a Medico-Legal Context. Arch. Phys. Med. Rehabil. 2009, 90, 1117–1126. [Google Scholar] [CrossRef]
- Thompson, C.R.; Heffernan, T.M.; Hamilton, C. False Positives in the Detection of Malingering: A Review. Clin. Neuropsychol. 2020, 34, 1325–1343. [Google Scholar]
- Young, G. Detecting Malingering and Deception: Forensic Distortion Analysis (FDA) and the Structured Inventory of Malingered Symptomatology (SIMS). Psychol. Inj. Law. 2014, 7, 145–155. [Google Scholar]
- Sweet, J.J.; Heilbronner, R.L.; Morgan, J.E.; Larrabee, G.J.; Rohling, M.L.; Boone, K.B.; Kirkwood, M.W.; Schroeder, R.W.; Suhr, J.A.; Conference Participants. American Academy of Clinical Neuropsychology (AACN) 2021 Consensus Statement on Validity Assessment: Update of the 2009 AACN Consensus Conference Statement on Neuropsychological Assessment of Effort, Response Bias, and Malingering. Clin. Neuropsychol. 2021, 35, 1053–1106. [Google Scholar] [CrossRef]
- Girometti, N.; Magliacano, A.; Ricci, G.; Ferrara, S.D. Malingering and Forensic Neuropsychology: An Update on Assessment Tools and Ethical Implications. Int. J. Legal Med. 2020, 134, 1017–1028. [Google Scholar]
- Zhang, X.-Y.; Liu, J.-H.; Cui, Y.; Tang, P. Electrophysiological examination of peripheral nerve injury and its significance in forensic medicine. Fa Yi Xue Za Zhi 2008, 24, 280–283. [Google Scholar]
- Kafadar, K. The Need for Objective Measures in Forensic Evidence. Significance 2019, 16, 16–20. [Google Scholar] [CrossRef]
- Preston, D.C.; Shapiro, B.E. Electromyography and Neuromuscular Disorders: Clinical-Electrophysiologic Correlations; Elsevier: Amsterdam, The Netherlands, 2020. [Google Scholar]
- Chhabra, A.; Andreisek, G.; Soldatos, T.; Wang, K.C.; Flammang, A.J.; Belzberg, A.J.; Carrino, J.A. MR Neurography: Past, Present, and Future. AJR Am. J. Roentgenol. 2011, 197, 583–591. [Google Scholar] [CrossRef] [PubMed]
- Zaidman, C.M.; Seelig, M.J.; Baker, J.C.; Mackinnon, S.E.; Pestronk, A. Detection of Peripheral Nerve Pathology: Comparison of Ultrasound and MRI. Neurology 2013, 80, 1634–1640. [Google Scholar] [CrossRef] [PubMed]
- Hudak, P.L.; Amadio, P.C.; Bombardier, C. Development of an Upper Extremity Outcome Measure: The DASH (Disabilities of the Arm, Shoulder and Hand) [Corrected]. The Upper Extremity Collaborative Group (UECG). Am. J. Ind. Med. 1996, 29, 602–608. [Google Scholar] [CrossRef]
- Freynhagen, R.; Baron, R.; Gockel, U.; Tölle, T.R. PainDETECT: A New Screening Questionnaire to Identify Neuropathic Components in Patients with Back Pain. Curr. Med. Res. Opin. 2006, 22, 1911–1920. [Google Scholar] [CrossRef]
- Bouhassira, D.; Attal, N.; Alchaar, H.; Boureau, F.; Brochet, B.; Bruxelle, J.; Cunin, G.; Fermanian, J.; Ginies, P.; Grun-Overdyking, A.; et al. Comparison of Pain Syndromes Associated with Nervous or Somatic Lesions and Development of a New Neuropathic Pain Diagnostic Questionnaire (DN4). Pain 2005, 114, 29–36. [Google Scholar] [CrossRef]
- Novak, C.B.; Katz, J. Neuropathic Pain in Patients with Upper-Extremity Nerve Injury. Physiother. Can. 2010, 62, 190–201. [Google Scholar] [CrossRef]
- Miclescu, A.; Straatmann, A.; Gkatziani, P.; Butler, S.; Karlsten, R.; Gordh, T. Chronic Neuropathic Pain after Traumatic Peripheral Nerve Injuries in the Upper Extremity: Prevalence, Demographic and Surgical Determinants, Impact on Health and on Pain Medication. Scand. J. Pain 2019, 20, 95–108. [Google Scholar] [CrossRef]
- Melzack, R. The McGill Pain Questionnaire: Major Properties and Scoring Methods. Pain 1975, 1, 277–299. [Google Scholar] [CrossRef]
- van Driel, M.E.C.; Huygen, F.J.P.M.; Rijsdijk, M. Quantitative Sensory Testing: A Practical Guide and Clinical Applications. BJA Educ. 2024, 24, 326–334. [Google Scholar] [CrossRef]
- Vollert, J.; Attal, N.; Baron, R.; Freynhagen, R.; Haanpää, M.; Hansson, P.; Jensen, T.S.; Rice, A.S.; Segerdahl, M.; Serra, J.; et al. Quantitative Sensory Testing Using the DFNS Protocol in Europe: An Updated Consensus. Pain 2022, 157, 750–758. [Google Scholar] [CrossRef] [PubMed]
- Yarnitsky, D.; Granot, M.; Granovsky, Y. Pain Modulation Profile and Pain Therapy: Between pro- and Antinociception. Pain 2014, 155, 663–665. [Google Scholar] [CrossRef] [PubMed]
- Backonja, M.M.; Attal, N.; Baron, R.; Bouhassira, D.; Drangholt, M.; Dyck, P.J.; Edwards, R.R.; Freeman, R.; Gracely, R.; Haanpaa, M.H.; et al. Value of Quantitative Sensory Testing in Neurological and Pain Disorders: NeuPSIG Consensus. Pain 2013, 154, 1807–1819. [Google Scholar] [CrossRef] [PubMed]
- Hansson, P. Translating Diagnostic Criteria and Assessment Tools for Neuropathic Pain. Pain 2018, 159, 1–2. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).


