Artificial Intelligence in Rotator Cuff Tear Detection: A Systematic Review of MRI-Based Models
Abstract
1. Introduction
2. Materials and Methods
2.1. Eligibility Criteria
2.2. Information Sources
2.3. Search Strategy and Data Collection Process
2.4. Data Items
2.5. Study Risk of Bias Assessment
2.6. Synthesis Method
3. Results
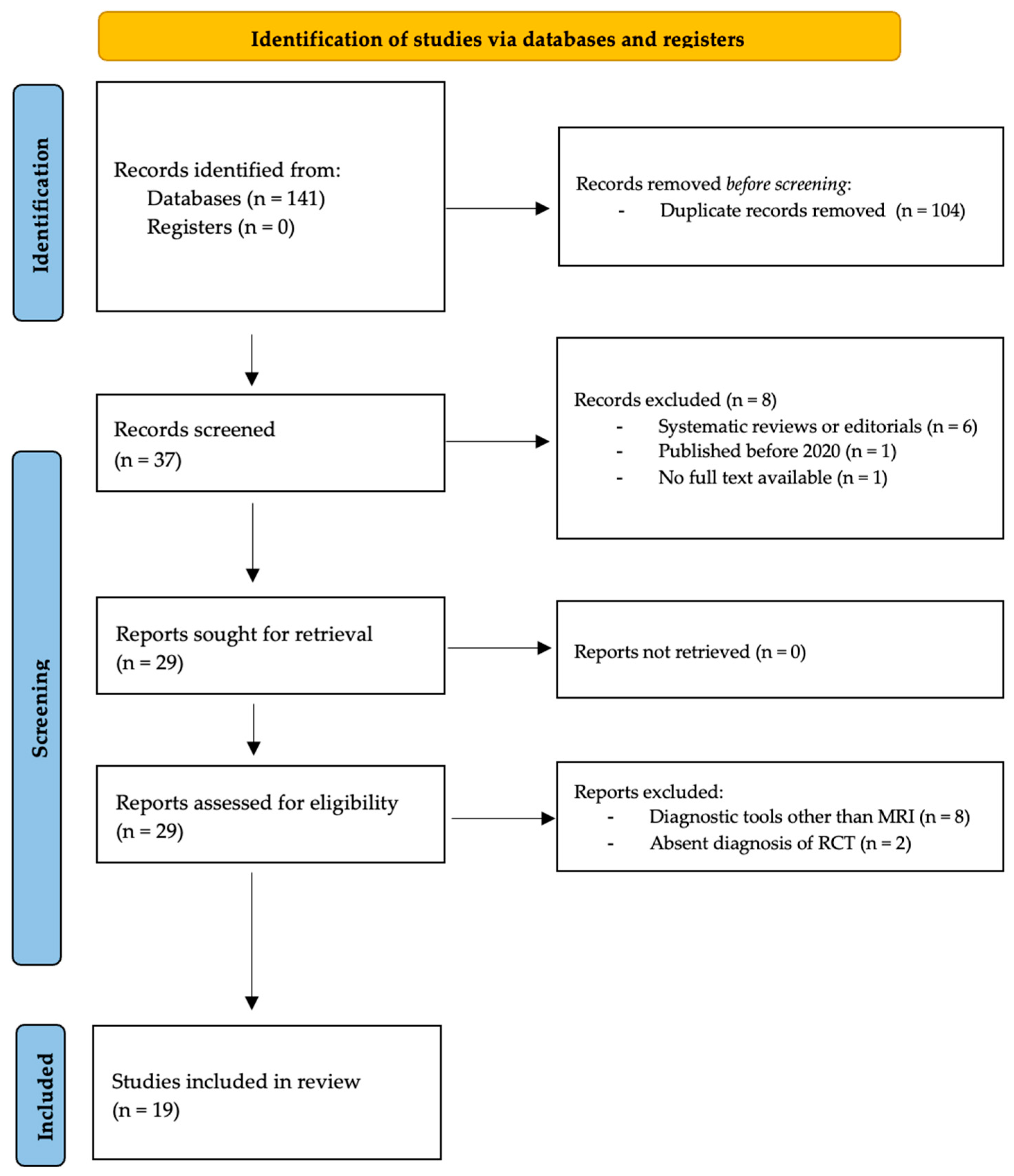
3.1. Study Selection
3.2. Quality of Evidence
3.3. Cohort Characteristics
3.4. Individual Study Objectives
3.5. MRI Acquisition Parameters
3.6. AI Models and Learning Data
3.7. AI Model Performance Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hill, J.R.; Olson, J.J.; Sefko, J.A.; Steger-May, K.; Teefey, S.A.; Middleton, W.D.; Keener, J.D. Does surgical intervention alter the natural history of degenerative rotator cuff tears? Comparative analysis from a prospective longitudinal study. J. Shoulder Elb. Surg. 2024, 34, 430–440. [Google Scholar] [CrossRef] [PubMed]
- Via, A.G.; De Cupis, M.; Spoliti, M.; Oliva, F. Clinical and biological aspects of rotator cuff tears. Muscles Ligaments Tendons J. 2013, 3, 70–79. [Google Scholar] [CrossRef] [PubMed]
- Redondo-Alonso, L.; Chamorro-Moriana, G.; Jiménez-Rejano, J.J.; López-Tarrida, P.; Ridao-Fernández, C. Relationship between chronic pathologies of the supraspinatus tendon and the long head of the biceps tendon: Systematic review. BMC Musculoskelet. Disord. 2014, 15, 377. [Google Scholar] [CrossRef]
- Calvo, E.; Guardado, C.R.; Morcillo, D.; Arce, G. Diagnosis and Classification of Rotator Cuff Tears. In Rotator Cuff Across the Life Span; Springer: Berlin/Heidelberg, Germany, 2019; pp. 3–10. [Google Scholar]
- Loew, M.; Magosch, P.; Lichtenberg, S.; Habermeyer, P.; Porschke, F. How to discriminate between acute traumatic and chronic degenerative rotator cuff lesions: An analysis of specific criteria on radiography and magnetic resonance imaging. J. Shoulder Elb. Surg. 2015, 24, 1685–1693. [Google Scholar] [CrossRef] [PubMed]
- Furrer, P.R.; Borbas, P.; Egli, R.J.; Zindel, C.; Wieser, K.; Bouaicha, S. MRI findings of traumatic and degenerative rotator cuff tears and introduction of the “cobra sign”. JSES Int. 2023, 7, 550–554. [Google Scholar] [CrossRef]
- Zhan, H.; Teng, F.; Liu, Z.; Yi, Z.; He, J.; Chen, Y.; Geng, B.; Xia, Y.; Wu, M.; Jiang, J. Artificial Intelligence Aids Detection of Rotator Cuff Pathology: A Systematic Review. Arthroscopy 2024, 40, 567–578. [Google Scholar] [CrossRef]
- Liu, F.; Guan, B.; Zhou, Z.; Samsonov, A.; Rosas, H.; Lian, K.; Sharma, R.; Kanarek, A.; Kim, J.; Guermazi, A.; et al. Fully Automated Diagnosis of Anterior Cruciate Ligament Tears on Knee MR Images by Using Deep Learning. Radiol. Artif. Intell. 2019, 1, 180091. [Google Scholar] [CrossRef]
- Gitto, S.; Serpi, F.; Albano, D.; Risoleo, G.; Fusco, S.; Messina, C.; Sconfienza, L.M. AI applications in musculoskeletal imaging: A narrative review. Eur. Radiol. Exp. 2024, 8, 22. [Google Scholar] [CrossRef]
- Lalehzarian, S.P.; Gowd, A.K.; Liu, J.N. Machine learning in orthopaedic surgery. World J. Orthop. 2021, 12, 685–699. [Google Scholar] [CrossRef]
- Lisacek-Kiosoglous, A.B.; Powling, A.S.; Fontalis, A.; Gabr, A.; Mazomenos, E.; Haddad, F.S. Artificial intelligence in orthopaedic surgery. Bone Jt. Res. 2023, 12, 447–454. [Google Scholar] [CrossRef]
- van Timmeren, J.E.; Cester, D.; Tanadini-Lang, S.; Alkadhi, H.; Baessler, B. Radiomics in medical imaging-”how-to” guide and critical reflection. Insights Imaging 2020, 11, 91. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez, H.C.; Rust, B.; Hansen, P.Y.; Maffulli, N.; Gupta, M.; Potty, A.G.; Gupta, A. Artificial Intelligence and Machine Learning in Rotator Cuff Tears. Sports Med. Arthrosc. Rev. 2023, 31, 67–72. [Google Scholar] [CrossRef] [PubMed]
- Velasquez Garcia, A.; Hsu, K.L.; Marinakis, K. Advancements in the diagnosis and management of rotator cuff tears. The role of artificial intelligence. J. Orthop. 2024, 47, 87–93. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA Statement. Open Med. 2009, 3, e123–e130. [Google Scholar]
- Cui, J.; Xia, X.; Wang, J.; Li, X.; Huang, M.; Miao, S.; Hao, D.; Li, J. Fully Automated Approach for Diagnosis of Supraspinatus Tendon Tear on Shoulder MRI by Using Deep Learning. Acad. Radiol. 2023, 31, 994–1002. [Google Scholar] [CrossRef]
- Esfandiari, M.A.; Fallah Tafti, M.; Jafarnia Dabanloo, N.; Yousefirizi, F. Detection of the rotator cuff tears using a novel convolutional neural network from magnetic resonance image (MRI). Heliyon 2023, 9, e15804. [Google Scholar] [CrossRef]
- Guo, D.; Liu, X.; Wang, D.; Tang, X.; Qin, Y. Development and clinical validation of deep learning for auto-diagnosis of supraspinatus tears. J. Orthop. Surg. Res. 2023, 18, 426. [Google Scholar] [CrossRef]
- Hahn, S.; Yi, J.; Lee, H.J.; Lee, Y.; Lim, Y.J.; Bang, J.Y.; Kim, H.; Lee, J. Image Quality and Diagnostic Performance of Accelerated Shoulder MRI With Deep Learning-Based Reconstruction. AJR Am. J. Roentgenol. 2022, 218, 506–516. [Google Scholar] [CrossRef]
- Hess, H.; Ruckli, A.C.; Bürki, F.; Gerber, N.; Menzemer, J.; Burger, J.; Schär, M.; Zumstein, M.A.; Gerber, K. Deep-Learning-Based Segmentation of the Shoulder from MRI with Inference Accuracy Prediction. Diagnostics 2023, 13, 1668. [Google Scholar] [CrossRef]
- Key, S.; Demir, S.; Gurger, M.; Yilmaz, E.; Barua, P.D.; Dogan, S.; Tuncer, T.; Arunkumar, N.; Tan, R.S.; Acharya, U.R. ViVGG19: Novel exemplar deep feature extraction-based shoulder rotator cuff tear and biceps tendinosis detection using magnetic resonance images. Med. Eng. Phys. 2022, 110, 103864. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.; Shin, K.; Lee, E.S.; Chung, S.W.; Koh, K.H.; Kim, N. Can deep learning reduce the time and effort required for manual segmentation in 3D reconstruction of MRI in rotator cuff tears? PLoS ONE 2022, 17, e0274075. [Google Scholar] [CrossRef]
- Kim, S.H.; Yoo, H.J.; Yoon, S.H.; Kim, Y.T.; Park, S.J.; Chai, J.W.; Oh, J.; Chae, H.D. Development of a deep learning-based fully automated segmentation of rotator cuff muscles from clinical MR scans. Acta Radiol. 2024, 65, 1126–1132. [Google Scholar] [CrossRef]
- Lee, K.C.; Cho, Y.; Ahn, K.S.; Park, H.J.; Kang, Y.S.; Lee, S.; Kim, D.; Kang, C.H. Deep-Learning-Based Automated Rotator Cuff Tear Screening in Three Planes of Shoulder MRI. Diagnostics 2023, 13, 3254. [Google Scholar] [CrossRef]
- Lee, S.H.; Lee, J.; Oh, K.S.; Yoon, J.P.; Seo, A.; Jeong, Y.; Chung, S.W. Automated 3-dimensional MRI segmentation for the posterosuperior rotator cuff tear lesion using deep learning algorithm. PLoS ONE 2023, 18, e0284111. [Google Scholar] [CrossRef]
- Lin, D.J.; Schwier, M.; Geiger, B.; Raithel, E.; von Busch, H.; Fritz, J.; Kline, M.; Brooks, M.; Dunham, K.; Shukla, M.; et al. Deep Learning Diagnosis and Classification of Rotator Cuff Tears on Shoulder MRI. Investig. Radiol. 2023, 58, 405–412. [Google Scholar] [CrossRef]
- Ni, M.; Zhao, Y.; Zhang, L.; Chen, W.; Wang, Q.; Tian, C.; Yuan, H. MRI-based automated multitask deep learning system to evaluate supraspinatus tendon injuries. Eur. Radiol. 2024, 34, 3538–3551. [Google Scholar] [CrossRef]
- Riem, L.; Feng, X.; Cousins, M.; DuCharme, O.; Leitch, E.B.; Werner, B.C.; Sheean, A.J.; Hart, J.; Antosh, I.J.; Blemker, S.S. A Deep Learning Algorithm for Automatic 3D Segmentation of Rotator Cuff Muscle and Fat from Clinical MRI Scans. Radiol. Artif. Intell. 2023, 5, e220132. [Google Scholar] [CrossRef]
- Ro, K.; Kim, J.Y.; Park, H.; Cho, B.H.; Kim, I.Y.; Shim, S.B.; Choi, I.Y.; Yoo, J.C. Deep-learning framework and computer assisted fatty infiltration analysis for the supraspinatus muscle in MRI. Sci. Rep. 2021, 11, 15065. [Google Scholar] [CrossRef] [PubMed]
- Aysun Sezer and Hasan Basri, S. Capsule network-based classification of rotator cuff pathologies from MRI. Comput. Electr. Eng. 2019, 80, 106480. [Google Scholar] [CrossRef]
- Shim, E.; Kim, J.Y.; Yoon, J.P.; Ki, S.Y.; Lho, T.; Kim, Y.; Chung, S.W. Automated rotator cuff tear classification using 3D convolutional neural network. Sci. Rep. 2020, 10, 15632. [Google Scholar] [CrossRef] [PubMed]
- Wang, P.; Liu, Y.; Zhou, Z. Supraspinatus extraction from MRI based on attention-dense spatial pyramid UNet network. J. Orthop. Surg. Res. 2024, 19, 60. [Google Scholar] [CrossRef]
- Yao, J.; Chepelev, L.; Nisha, Y.; Sathiadoss, P.; Rybicki, F.J.; Sheikh, A.M. Evaluation of a deep learning method for the automated detection of supraspinatus tears on MRI. Skelet. Radiol. 2022, 51, 1765–1775. [Google Scholar] [CrossRef] [PubMed]
- Zhan, J.; Liu, S.; Dong, C.; Ge, Y.; Xia, X.; Tian, N.; Xu, Q.; Jiang, G.; Xu, W.; Cui, J. Shoulder MRI-based radiomics for diagnosis and severity staging assessment of surgically treated supraspinatus tendon tears. Eur. Radiol. 2023, 33, 5587–5593. [Google Scholar] [CrossRef]
- Whiting, P.F.; Rutjes, A.W.; Westwood, M.E.; Mallett, S.; Deeks, J.J.; Reitsma, J.B.; Leeflang, M.M.; Sterne, J.A.; Bossuyt, P.M.; QUADAS-2 Group. QUADAS-2: A revised tool for the quality assessment of diagnostic accuracy studies. Ann. Intern. Med. 2011, 155, 529–536. [Google Scholar] [CrossRef]
- Saavedra, J.P.; Droppelmann, G.; García, N.; Jorquera, C.; Feijoo, F. High-accuracy detection of supraspinatus fatty infiltration in shoulder MRI using convolutional neural network algorithms. Front. Med. 2023, 10, 1070499. [Google Scholar] [CrossRef]
- Fazal Gafoor, H.; Jose, G.A.; Mampalli Narayanan, B. Role of Magnetic Resonance Imaging (MRI) in the Diagnosis of Rotator Cuff Injuries and Correlation With Arthroscopy Findings. Cureus 2023, 15, e50103. [Google Scholar] [CrossRef]
- Dickinson, R.N.; Kuhn, J.E. Nonoperative Treatment of Rotator Cuff Tears. Phys. Med. Rehabil. Clin. N. Am. 2023, 34, 335–355. [Google Scholar] [CrossRef]
- Ganal, E.; Ho, C.P.; Wilson, K.J.; Surowiec, R.K.; Smith, W.S.; Dornan, G.J.; Millett, P.J. Quantitative MRI characterization of arthroscopically verified supraspinatus pathology: Comparison of tendon tears, tendinosis and asymptomatic supraspinatus tendons with T2 mapping. Knee Surg. Sports Traumatol. Arthrosc. 2016, 24, 2216–2224. [Google Scholar] [CrossRef] [PubMed]
| Author and Year | Objective | Pathology | Cohort (n) | Mean Age | Gender | |
|---|---|---|---|---|---|---|
| F | M | |||||
| Cui et al., 2023 [17] | Diagnosis | SST | 431 | 47.6 ± 15.1 | 251 | 180 |
| Esfandiari et al., 2023 [18] | Diagnosis | RCT | 150 | NA | NA | NA |
| Guo et al., 2023 [19] | Classification | SST | 69 | NA | 37 | 32 |
| Hahn et al., 2022 [20] | Diagnosis | BT | 110 | 57.6 ± 10.9 | 60 | 45 |
| Hess et al., 2023 [21] | Segmentation | RCT | 76 | NA | 29 | 47 |
| Key et al., 2022 [22] | Diagnosis | BT | 295 | NA | NA | NA |
| Kim H. et al., 2022 [23] | Classification | SST | 56 | 63.7 ± 9.3 | 32 | 24 |
| Kim S.H. et al., 2024 [24] | Diagnosis | RCT | 94 | 62.3 ± 7.5 | 67 | 27 |
| Lee K.C. et al., 2023 [25] | Diagnosis | RCT | 794 | 59.0 ± 11 | 420 | 374 |
| Lee S.H. et al., 2023 [26] | Segmentation | RCT | 303 | 64.5 ± 8.2 | 157 | 146 |
| Lin et al., 2023 [27] | Classification | SST | 518 | 59.4 ± 14.4 | 227 | 291 |
| Ni et al., 2024 [28] | Classification | SST | 3087 | NA | 1602 | 1485 |
| Riem et al., 2023 [29] | Classification | RCT | 232 | NA | 106 | 126 |
| Ro et al., 2021 [30] | Classification | SST | 240 | NA | NA | NA |
| Sezer et al., 2019 [31] | Classification | RCT | 1006 | NA | NA | NA |
| Shim et al., 2020 [32] | Classification | RCT | 2124 | NA | NA | NA |
| Wang et al., 2024 [33] | Segmentation | SST | 60 | NA | NA | NA |
| Yao et al., 2022 [34] | Diagnosis | SST | 200 | 47.8 ± 15.3 | 79 | 121 |
| Zhan et al., 2023 [35] | Classification | SST | 432 | 47.2 ± 10.0 | 251 | 181 |
| Author and Year | No Tear | Tears | ||||||
|---|---|---|---|---|---|---|---|---|
| Tot | PT | FT | S | M | L | Ms | ||
| Cui et al., 2023 [17] | 229 | 202 | - | - | - | - | - | - |
| Esfandiari et al., 2023 [18] | 75 | 75 | - | - | - | - | - | - |
| Guo et al., 2023 [19] | 26 | 43 | 3 | 20 | 8 | 6 | 6 | 0 |
| Hahn et al., 2022 [20] | 49 | 61 | - | - | - | - | - | - |
| Hess et al., 2023 [21] | NA | |||||||
| Key et al., 2022 [22] | 140 | 155 | - | - | - | - | - | - |
| Kim H. et al., 2022 [23] | 10 | 46 | 6 | 0 | 6 | 14 | 12 | 8 |
| Kim S.H. et al., 2024 [24] | 94 | 6 | - | - | - | - | - | - |
| Lee K.C. et al., 2023 [25] | 100 | 694 | - | - | - | - | - | - |
| Lee S.H. et al., 2023 [26] | NA | |||||||
| Lin et al., 2023 [27] | 133 | 385 | 231 | 154 | - | - | - | - |
| Ni et al., 2024 [28] | 456 | 2631 | 1012 | 1619 | - | - | - | - |
| Riem et al., 2023 [29] | 63 | 169 | - | - | - | - | - | - |
| Ro et al., 2021 [30] | 55 | 185 | - | - | - | - | - | - |
| Sezer et al., 2019 [31] | 627 | 379 | - | - | - | - | - | - |
| Shim et al., 2020 [32] | 764 | 1360 | 285 | 0 | 227 | 567 | 281 | 0 |
| Wang et al., 2024 [33] | NA | |||||||
| Yao et al., 2022 [34] | 100 | 100 | 50 | 50 | - | - | - | - |
| Zhan et al., 2023 [35] | 202 | 230 | 100 | 130 | - | - | - | - |
| Author and Year | Plane | Sequence | Slices |
|---|---|---|---|
| Cui et al., 2023 [17] | C | T2 | 36 |
| Esfandiari et al., 2023 [18] | C, S, A | NA | NA |
| Guo et al., 2023 [19] | C | PD | 64 |
| Hahn et al., 2022 [20] | C, S, A | T2 | NA |
| Hess et al., 2023 [21] | C, S, A | T1 | NA |
| Key et al., 2022 [22] | A | T2 | 1169 |
| Kim H. et al., 2022 [23] | C | T2 | NA |
| Kim S.H. et al., 2024 [24] | C, S, A | PD, T1, T2 | 2820 |
| Lee K.C. et al., 2023 [25] | C, S, A | PD, T2 | NA |
| Lee S.H. et al., 2023 [26] | C, S, A | T1, T2 | 100 |
| Lin et al., 2023 [27] | C, S, A | PD, T2 | 32 |
| Ni et al., 2024 [28] | C, S | PD | NA |
| Riem et al., 2023 [29] | S | T1 | NA |
| Ro et al., 2021 [30] | C, A | T1 | NA |
| Sezer et al., 2019 [31] | C | PD | NA |
| Shim et al., 2020 [32] | C, S, A | T1, T2 | NA |
| Wang et al., 2024 [33] | C | PD | 200 |
| Yao et al., 2022 [34] | C | T2 | 4287 |
| Zhan et al., 2023 [35] | C | T2 | NA |
| Author and Year | AI Model | Slices | Training Set (n) | Test Set (n) | Ground Truth Reference |
|---|---|---|---|---|---|
| Cui et al., 2023 [17] | U-Net ResNet DensNet | 36 | 265 | 99 | Musculoskeletal radiologists |
| Esfandiari et al., 2023 [18] | MobileNet SqueezeNet | NA | NA | NA | Orthopaedic surgeon |
| Guo et al., 2023 [19] | Xception | 64 | 144 | 69 | Arthroscopic findings |
| Hahn et al., 2022 [20] | AIR Recon | NA | NA | NA | Arthroscopic findings |
| Hess et al., 2023 [21] | nnU-Net | NA | 111 | 60 | Musculoskeletal radiologists |
| Key et al., 2022 [22] | VGG INCA | 1169 | NA | NA | Arthroscopic findings |
| Kim H. et al., 2022 [23] | nnU-Net | NA | 34 | 11 | Orthopaedic surgeon |
| Kim S.H. et al., 2024 [24] | nnU-Net | 2820 | 84 | 20 | Musculoskeletal radiologists |
| Lee K.C. et al., 2023 [25] | YOLO | NA | 1511 | 391 | Musculoskeletal radiologists |
| Lee S.H. et al., 2023 [26] | U-Net | 100 | 182 | 61 | Orthopaedic surgeon |
| Lin et al., 2023 [27] | ResNet | 32 | 11,405 | 520 | Musculoskeletal radiologists |
| Ni et al., 2024 [28] | VGG RC-MTL | NA | 2470 | 309 | Arthroscopic findings |
| Riem et al., 2023 [29] | U-Net | NA | 202 | 30 | Orthopaedic surgeon |
| Ro et al., 2021 [30] | VGG | NA | 216 | 24 | Orthopaedic surgeon |
| Sezer et al., 2019 [31] | CapsNet | NA | NA | NA | Orthopaedic surgeon |
| Shim et al., 2020 [32] | VRN | NA | 1924 | 2000 | Arthroscopic findings |
| Wang et al., 2024 [33] | U-Net | 200 | NA | NA | Musculoskeletal radiologists |
| Yao et al., 2022 [34] | ResNet U-Net | 4287 | 160 | 40 | Musculoskeletal radiologists |
| Zhan et al., 2023 [35] | DenseNet VGG | NA | 332 | 100 | Musculoskeletal radiologists |
| Author and Year | Comparison | Accuracy (%) | Sensitivity (%) | Specificity (%) | Precision (%) | Dice |
|---|---|---|---|---|---|---|
| Cui et al., 2023 [17] | AI | 92.9 | 91.8 | 94.0 | NA | NA |
| H | 90.9 | 91.8 | 90.0 | NA | NA | |
| Esfandiari et al., 2023 [18] | - | 92.6 | 91.7 | 92.2 | 91.1 | NA |
| Guo et al., 2023 [19] | AI | 71.0 | 73.9 | 69.6 | 54.0 | NA |
| H | 86.2 | 93.5 | 82.6 | 72.9 | NA | |
| Hahn et al., 2022 [20] | - | 88.9 | 72.7 | 100 | NA | NA |
| Hess et al., 2023 [21] | - | NA | 100 | 94.0 | NA | 0.91 |
| Key et al., 2022 [22] | - | 100 | 100 | 100 | 100 | NA |
| Kim H. et al., 2022 [23] | - | NA | NA | NA | NA | 0.83 |
| Kim S.H. et al., 2024 [24] | - | NA | 93.3 | NA | 91.2 | 0.92 |
| Lee K.C. et al., 2023 [25] | - | 96.0 | 98.0 | 91.0 | 98.0 | NA |
| Lee S.H. et al., 2023 [26] | - | NA | 97.1 | 95.0 | 84.9 | 0.94 |
| Lin et al., 2023 [27] | AI | 81.0 | NA | NA | NA | NA |
| H | 79.0 | NA | NA | NA | NA | |
| Ni et al., 2024 [28] | - | 98.0 | 96.0 | 93.0 | NA | NA |
| Riem et al., 2023 [29] | - | NA | NA | NA | NA | 0.92 |
| Ro et al., 2021 [30] | - | 99.8 | 93.3 | 99.9 | NA | 0.94 |
| Sezer et al., 2019 [31] | - | 94.7 | NA | NA | NA | NA |
| Shim et al., 2020 [32] | AI | 87.5 | 92.0 | 86.0 | 94.0 | NA |
| H | 79.8 | 89.0 | 61.0 | 79.0 | NA | |
| Wang et al., 2024 [33] | - | NA | NA | NA | 99.2 | 0.90 |
| Yao et al., 2022 [34] | - | 81.4 | 85.0 | 85.0 | NA | 0.81 |
| Zhan et al., 2023 [35] | - | 76.4 | 79.2 | 74.3 | NA | NA |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Longo, U.G.; Bandini, B.; Mancini, L.; Merone, M.; Schena, E.; de Sire, A.; D’Hooghe, P.; Pecchia, L.; Carnevale, A. Artificial Intelligence in Rotator Cuff Tear Detection: A Systematic Review of MRI-Based Models. Diagnostics 2025, 15, 1315. https://doi.org/10.3390/diagnostics15111315
Longo UG, Bandini B, Mancini L, Merone M, Schena E, de Sire A, D’Hooghe P, Pecchia L, Carnevale A. Artificial Intelligence in Rotator Cuff Tear Detection: A Systematic Review of MRI-Based Models. Diagnostics. 2025; 15(11):1315. https://doi.org/10.3390/diagnostics15111315
Chicago/Turabian StyleLongo, Umile Giuseppe, Benedetta Bandini, Letizia Mancini, Mario Merone, Emiliano Schena, Alessandro de Sire, Pieter D’Hooghe, Leandro Pecchia, and Arianna Carnevale. 2025. "Artificial Intelligence in Rotator Cuff Tear Detection: A Systematic Review of MRI-Based Models" Diagnostics 15, no. 11: 1315. https://doi.org/10.3390/diagnostics15111315
APA StyleLongo, U. G., Bandini, B., Mancini, L., Merone, M., Schena, E., de Sire, A., D’Hooghe, P., Pecchia, L., & Carnevale, A. (2025). Artificial Intelligence in Rotator Cuff Tear Detection: A Systematic Review of MRI-Based Models. Diagnostics, 15(11), 1315. https://doi.org/10.3390/diagnostics15111315











