Minimally Invasive Surgery Versus Conventional Neurosurgical Treatments for Patients with Subcortical Supratentorial Intracerebral Hemorrhage: A Nationwide Study of Real-World Data from 2016 to 2022
Abstract
1. Introduction
2. Methods
2.1. Database Characteristics
2.2. Patient Population
2.2.1. Study Outcomes
2.2.2. Statistical Methods
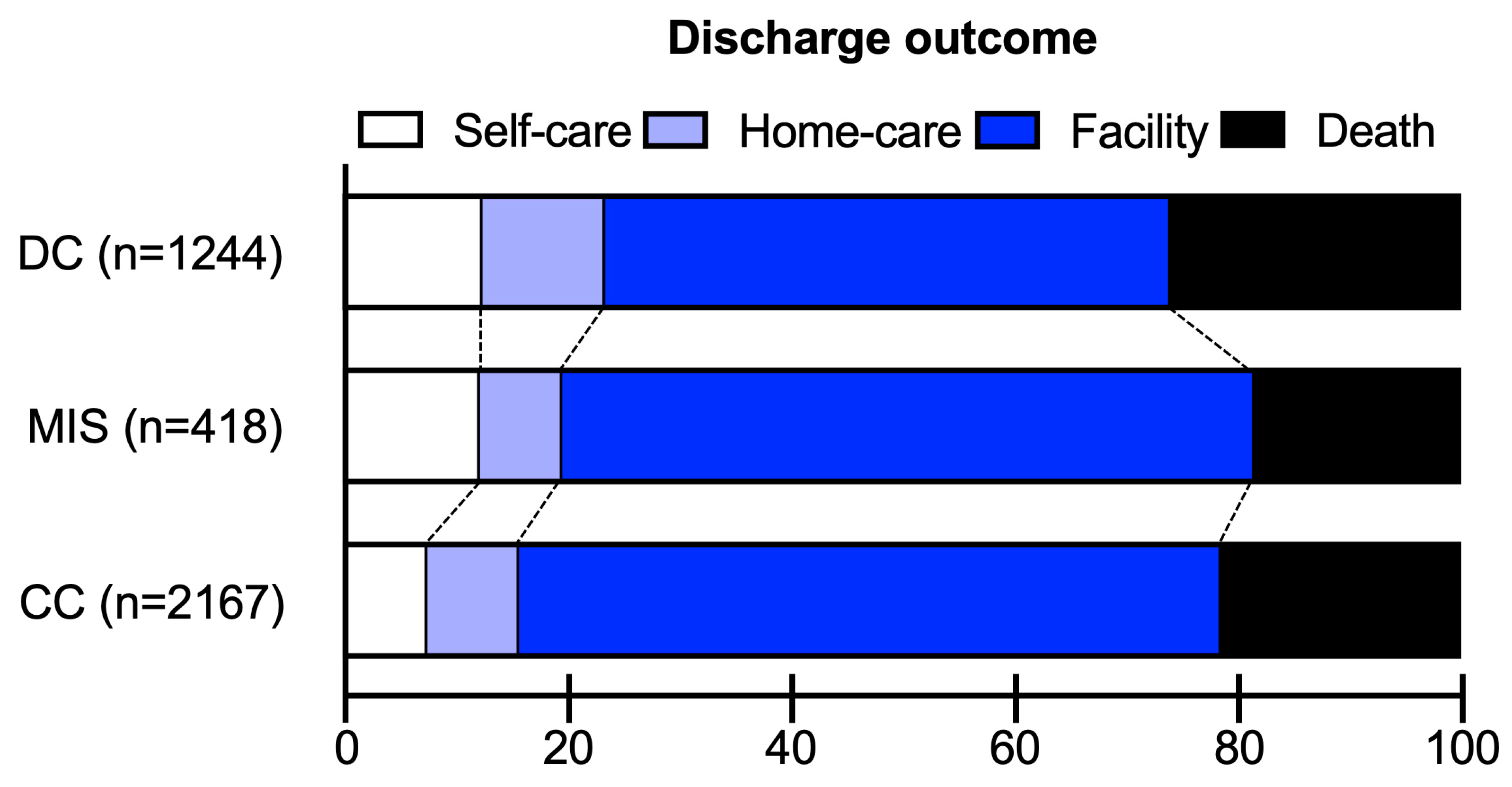
3. Results
3.1. Patient Characteristics
3.2. MIS vs. CC Outcomes
3.3. MIS vs. DC Outcomes
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Parry-Jones, A.R.; Krishnamurthi, R.; Ziai, W.C.; Shoamanesh, A.; Wu, S.; Martins, S.O.; Anderson, C.S. World Stroke Organization (WSO): Global intracerebral hemorrhage factsheet 2025. Int. J. Stroke 2025, 20, 145–150. [Google Scholar] [CrossRef] [PubMed]
- Mendelow, A.D.; Gregson, B.A.; Fernandes, H.M.; Murray, G.D.; Teasdale, G.M.; Hope, D.T.; Karimi, A.; Shaw, N.D.M.; Barer, D.H. Early surgery versus initial conservative treatment in patients with spontaneous supratentorial intracerebral haematomas in the International Surgical Trial in Intracerebral Haemorrhage (STICH): A randomised trial. Lancet 2005, 365, 387–397. [Google Scholar] [CrossRef] [PubMed]
- Beck, J.; Fung, C.; Strbian, D.; Bütikofer, L.; Z’Graggen, W.J.; Lang, M.F.; Beyeler, S.; Gralla, J.; Ringel, F.; Schaller, K.; et al. Decompressive craniectomy plus best medical treatment versus best medical treatment alone for spontaneous severe deep supratentorial intracerebral haemorrhage: A randomised controlled clinical trial. Lancet 2024, 403, 2395–2404. [Google Scholar] [CrossRef]
- Hannah, T.C.; Kellner, R.; Kellner, C.P. Minimally Invasive Intracerebral Hemorrhage Evacuation Techniques: A Review. Diagnostics 2021, 11, 576. [Google Scholar] [CrossRef]
- Hou, D.; Lu, Y.; Wu, D.; Tang, Y.; Dong, Q. Minimally Invasive Surgery in Patients With Intracerebral Hemorrhage: A Meta-Analysis of Randomized Controlled Trials. Front. Neurol. 2022, 12, 789757. [Google Scholar] [CrossRef]
- Scaggiante, J.; Zhang, X.; Mocco, J.; Kellner, C.P. Minimally Invasive Surgery for Intracerebral Hemorrhage. Stroke 2018, 49, 2612–2620. [Google Scholar] [CrossRef]
- Xu, X.; Zhang, H.; Zhang, J.; Luo, M.; Wang, Q.; Zhao, Y.; Gan, Z.; Xu, B.; Chen, X. Minimally invasive surgeries for spontaneous hypertensive intracerebral hemorrhage (MISICH): A multicenter randomized controlled trial. BMC Med. 2024, 22, 244. [Google Scholar] [CrossRef]
- Huan, J.; Yao, M.; Ma, Y.; Mei, F.; Liu, Y.; Ma, L.; Luo, X.; Liu, J.; Xu, J.; You, C.; et al. Surgical interventions for spontaneous supratentorial intracerebral haemorrhage: A systematic review and network meta-analysis. eClinicalMedicine 2025, 79, 102999. [Google Scholar] [CrossRef]
- Quan, H.; Sundararajan, V.; Halfon, P.; Fong, A.; Burnand, B.; Luthi, J.-C.; Saunders, L.D.; Beck, C.A.; Feasby, T.E.; Ghali, W.A. Coding Algorithms for Defining Comorbidities in ICD-9-CM and ICD-10 Administrative Data. Med. Care 2005, 43, 1130–1139. [Google Scholar] [CrossRef]
- Chen, H.; Khunte, M.; Colasurdo, M.; Malhotra, A.; Gandhi, D. Thrombectomy vs Medical Management for Posterior Cerebral Artery Stroke: Systematic Review, Meta-Analysis, and Real-World Data. Neurology 2024, 102, e209315. [Google Scholar] [CrossRef]
- Chen, H.; Khunte, M.; Malhotra, A.; Gandhi, D.; Colasurdo, M. Endovascular thrombectomy versus medical management for moderate-to-severe anterior cerebral artery occlusion stroke. J. Neurol. 2024, 271, 6247–6254. [Google Scholar] [CrossRef]
- Chen, H.; Colasurdo, M.; Khunte, M.; Malhotra, A.; Gandhi, D. Post-Thrombectomy Subarachnoid Hemorrhage: Incidence, Predictors, Clinical Relevance, and Effect Modulators. Diagnostics 2024, 14, 1856. [Google Scholar] [CrossRef]
- Chen, H.; Khunte, M.; Colasurdo, M.; Jindal, G.; Malhotra, A.; Gandhi, D.; Chaturvedi, S. Associations of Osteoarthritis With Thrombectomy Utilization and Outcomes for Large Vessel Acute Ischemic Stroke. Stroke 2023, 54, 518–526. [Google Scholar] [CrossRef]
- Chen, H.; Colasurdo, M.; Khunte, M.; Malhotra, A.; Gandhi, D. Endovascular thrombectomy versus medical management for acute basilar artery occlusion stroke in the elderly. Am. J. Neuroradiol. 2025, 46, 278–284. [Google Scholar] [CrossRef]
- Chen, H.; Khunte, M.; Colasurdo, M.; Malhotra, A.; Gandhi, D. Intravenous thrombolysis prior to endovascular thrombectomy in elderly stroke patients: An analysis of the National Inpatient Sample database. J. Neurol. Sci. 2023, 454, 120842. [Google Scholar] [CrossRef]
- Pradilla, G.; Ratcliff, J.J.; Hall, A.J.; Saville, B.R.; Allen, J.W.; Paulon, G.; McGlothlin, A.; Lewis, R.J.; Fitzgerald, M.; Caveney, A.F.; et al. Trial of Early Minimally Invasive Removal of Intracerebral Hemorrhage. N. Engl. J. Med. 2024, 390, 1277–1289. [Google Scholar] [CrossRef]
- Arthur, A.S.; Fiorella, D. Procedural, safety, and functional outcomes following minimally invasive surgery for deep and lobar intracranial hemorrhages: MIND study results. In Proceedings of the International Stroke Conference 2025, Los Angeles, CA, USA, 5–7 February 2025. [Google Scholar]
- Singh, R.; Parikh, P.P.; De La Peña, N.M.; Bhandarkar, A.R.; Doan, M.K.; Patel, N.P.; Meyer, F.B. Trends in the Neurosurgical Workforce and Implications in Providing for an Aging Population. World Neurosurg. 2022, 160, e261–e266. [Google Scholar] [CrossRef]
- Chen, H.; Marino, J.; Stemer, A.B.; Singh, I.P.; Froehler, M.T. Emerging Subspecialties in Neurology: Interventional Neurology. Neurology 2023, 101, e1939–e1942. [Google Scholar] [CrossRef]
- Kan, P.; Fiorella, D.; Dabus, G.; Samaniego, E.A.; Lanzino, G.; Siddiqui, A.H.; Chen, H.; Khalessi, A.A.; Pereira, V.M.; Fifi, J.T.; et al. ARISE I Consensus Statement on the Management of Chronic Subdural Hematoma. Stroke 2024, 55, 1438–1448. [Google Scholar] [CrossRef]
- Chen, H.; Colasurdo, M.; Kan, P. Middle Meningeal Artery Embolization for Subdural Hematoma. Neurosurg. Clin. N. Am. 2025, 36, 73–82. [Google Scholar] [CrossRef]
- Nguyen, T.N.; Abdalkader, M.; Fischer, U.; Qiu, Z.; Nagel, S.; Chen, H.-S.; Miao, Z.; Khatri, P. Endovascular management of acute stroke. Lancet 2024, 404, 1265–1278. [Google Scholar] [CrossRef] [PubMed]
- Steiger, K.; Singh, R.; Fox, W.C.; Koester, S.; Brown, N.; Shahrestani, S.; Miller, D.A.; Patel, N.P.; Catapano, J.S.; Srinivasan, V.M.; et al. Procedural, workforce, and reimbursement trends in neuroendovascular procedures. J. Neurointerv. Surg. 2023, 15, 909–913. [Google Scholar] [CrossRef]
- Tekle, W.; Benites, G.; Miller, S.; Betancourt, A.; Hassan, A.E. Minimally invasive surgery for evacuation of intracerebral hematoma by neurointerventionalists: Initial experience. J. Neurointerv. Surg. 2025. online ahead of print. [Google Scholar] [CrossRef]
- Teasdale, G.; Jennett, B. Assessment of Coma and Impaired Consciousness. Lancet 1974, 304, 81–84. [Google Scholar] [CrossRef]
- Hemphill, J.C.; Bonovich, D.C.; Besmertis, L.; Manley, G.T.; Johnston, S.C. The ICH Score. Stroke 2001, 32, 891–897. [Google Scholar] [CrossRef]
- Wada, R.; Aviv, R.I.; Fox, A.J.; Sahlas, D.J.; Gladstone, D.J.; Tomlinson, G.; Symons, S.P. CT Angiography “Spot Sign” Predicts Hematoma Expansion in Acute Intracerebral Hemorrhage. Stroke 2007, 38, 1257–1262. [Google Scholar] [CrossRef]
- van Swieten, J.C.; Koudstaal, P.J.; Visser, M.C.; Schouten, H.J.; van Gijn, J. Interobserver agreement for the assessment of handicap in stroke patients. Stroke 1988, 19, 604–607. [Google Scholar] [CrossRef]
- Lins, L.; Carvalho, F.M. SF-36 total score as a single measure of health-related quality of life: Scoping review. SAGE Open Med. 2016, 4. [Google Scholar] [CrossRef]
- Balestroni, G.; Bertolotti, G. EuroQol-5D (EQ-5D): An instrument for measuring quality of life. Monaldi Arch. Chest Dis. 2015, 78, 155–159. [Google Scholar] [CrossRef]

| Total | MIS | CC | DC | p-Values | ||
|---|---|---|---|---|---|---|
| Characteristic—Median (Q1–Q3) or % (n) | N = 3829 | N = 418 | N = 2167 | N = 1244 | MIS vs. CC | MIS vs. DC |
| Age (years) | 55 (45–64) | 58 (49–65) | 56 (47–65) | 52 (42–62) | 0.34 | <0.001 * |
| Female sex | 35.4% (1356) | 27.2% (114) | 36.1% (783) | 36.9% (459) | 0.004 * | 0.008 * |
| Intraventricular extension | 31.8% (1217) | 32.2% (135) | 31.2% (676) | 32.6% (406) | 0.79 | 0.92 |
| External ventricular drain | 28.5% (1093) | 25.1% (105) | 25.1% (543) | 35.7% (445) | 1.00 | 0.009 * |
| Antithrombotic medications | ||||||
| Anticoagulant use | 6.1% (233) | 4.0% (17) | 6.1% (133) | 6.7% (83) | 0.20 | 0.15 |
| Antiplatelet use | 2.0% (78) | 0.7% (3) | 2.4% (51) | 1.9% (24) | 0.087 | 0.15 |
| Comorbidities | ||||||
| Atrial fibrillation | 8.6% (328) | 7.1% (30) | 9.8% (211) | 7.0% (87) | 0.18 | 0.93 |
| Hypertension | 80.1% (3068) | 83.8% (350) | 83.8% (1817) | 72.4% (901) | 0.99 | <0.001 * |
| Hyperlipidemia | 26.4% (1010) | 29.7% (124) | 28.6% (620) | 21.4% (266) | 0.74 | 0.015 * |
| Diabetes | 23.2% (890) | 24.9% (104) | 25.8% (559) | 18.2% (227) | 0.78 | 0.013 * |
| Chronic liver disease | 5.3% (203) | 5.6% (23) | 4.8% (105) | 6.1% (75) | 0.61 | 0.75 |
| Chronic kidney disease | 17.0% (653) | 16.3% (68) | 17.7% (384) | 16.1% (200) | 0.60 | 0.94 |
| Coagulopathy | 15.0% (574) | 11.9% (50) | 14.4% (312) | 17.1% (212) | 0.31 | 0.039 * |
| Dementia | 1.7% (63) | 2.9% (12) | 2.2% (47) | 0.3% (4) | 0.57 | <0.001 * |
| Elixhauser comorbidity index | 16 (11–21) | 15 (11–21) | 16 (10–21) | 17 (10–23) | 0.71 | 0.41 |
| Treatment year | ||||||
| 2016 | 9.1% (349) | 11.3% (47) | 11.3% (245) | 4.6% (57) | 0.40 | 0.004 * |
| 2017 | 11.5% (440) | 13.5% (56) | 11.7% (254) | 10.5% (130) | ||
| 2018 | 13.1% (501) | 9.2% (38) | 14.7% (319) | 11.5% (143) | ||
| 2019 | 16.6% (636) | 17.4% (73) | 16.6% (360) | 16.3% (203) | ||
| 2020 | 17.1% (653) | 19.1% (80) | 14.7% (318) | 20.5% (255) | ||
| 2021 | 17.4% (667) | 12.4% (52) | 16.8% (364) | 20.2% (252) | ||
| 2022 | 15.2% (583) | 17.2% (72) | 14.1% (306) | 16.4% (205) | ||
| Unadjusted Comparisons | With Multivariable Adjustments | ||||
|---|---|---|---|---|---|
| Outcome | MIS (n = 418) | CC (n = 2167) | p-value | OR or B [95%CI] | p-Value |
| Routine discharge | 12.0% (50) | 7.2% (157) | 0.026 * | 1.99 [1.06 to 3.30] | 0.039 * |
| Home discharge | 19.3% (81) | 15.5% (336) | 0.16 | 1.35 [0.94 to 2.00] | 0.097 |
| In-hospital mortality | 18.5% (77) | 21.4% (464) | 0.30 | 0.81 [0.56 to 1.18] | 0.26 |
| Length of hospital stay (days) | 21 (13–37) | 19 (11–34) | 0.042 * | 0.43 [−2.91 to 3.77] | 0.80 |
| Cost of hospitalization (USD) | 89,866 (60,656–139,896) | 80,418 (52,437–123,765) | 0.003 * | 10,767 [702 to 20,831] | 0.036 * |
| Unadjusted Comparisons | With Multivariable Adjustments | ||||
|---|---|---|---|---|---|
| Outcome | MIS (n = 418) | DC (n = 1244) | p-Value | OR or B [95%CI] | p-Value |
| Routine discharge | 12.0% (50) | 12.2% (152) | 0.94 | 1.10 [0.66 to 1.86] | 0.73 |
| Home discharge | 19.3% (81) | 23.2% (289) | 0.23 | 0.82 [0.54 to 1.25] | 0.35 |
| In-hospital mortality | 18.5% (77) | 26.0% (323) | 0.026 * | 0.63 [0.41 to 0.96] | 0.032 * |
| Length of hospital stay (days) | 21 (13–37) | 19 (9–36) | 0.077 | 2.10 [−1.59 to 5.80] | 0.26 |
| Cost of hospitalization (USD) | 89,866 (60,656–139,896) | 88,000 (56,766–144,319) | 0.9 | 2984 [−10,045 to 16,014] | 0.65 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, H.; McIntyre, M.K.; Khunte, M.; Malhotra, A.; Labib, M.; Colasurdo, M.; Gandhi, D. Minimally Invasive Surgery Versus Conventional Neurosurgical Treatments for Patients with Subcortical Supratentorial Intracerebral Hemorrhage: A Nationwide Study of Real-World Data from 2016 to 2022. Diagnostics 2025, 15, 1308. https://doi.org/10.3390/diagnostics15111308
Chen H, McIntyre MK, Khunte M, Malhotra A, Labib M, Colasurdo M, Gandhi D. Minimally Invasive Surgery Versus Conventional Neurosurgical Treatments for Patients with Subcortical Supratentorial Intracerebral Hemorrhage: A Nationwide Study of Real-World Data from 2016 to 2022. Diagnostics. 2025; 15(11):1308. https://doi.org/10.3390/diagnostics15111308
Chicago/Turabian StyleChen, Huanwen, Matthew K. McIntyre, Mihir Khunte, Ajay Malhotra, Mohamed Labib, Marco Colasurdo, and Dheeraj Gandhi. 2025. "Minimally Invasive Surgery Versus Conventional Neurosurgical Treatments for Patients with Subcortical Supratentorial Intracerebral Hemorrhage: A Nationwide Study of Real-World Data from 2016 to 2022" Diagnostics 15, no. 11: 1308. https://doi.org/10.3390/diagnostics15111308
APA StyleChen, H., McIntyre, M. K., Khunte, M., Malhotra, A., Labib, M., Colasurdo, M., & Gandhi, D. (2025). Minimally Invasive Surgery Versus Conventional Neurosurgical Treatments for Patients with Subcortical Supratentorial Intracerebral Hemorrhage: A Nationwide Study of Real-World Data from 2016 to 2022. Diagnostics, 15(11), 1308. https://doi.org/10.3390/diagnostics15111308







