Utility of Biometric Measurements from Fetal Magnetic Resonance Imaging for Improved Antenatal Diagnosis of Dandy–Walker Spectrum Posterior Fossa Lesions
Abstract
1. Introduction
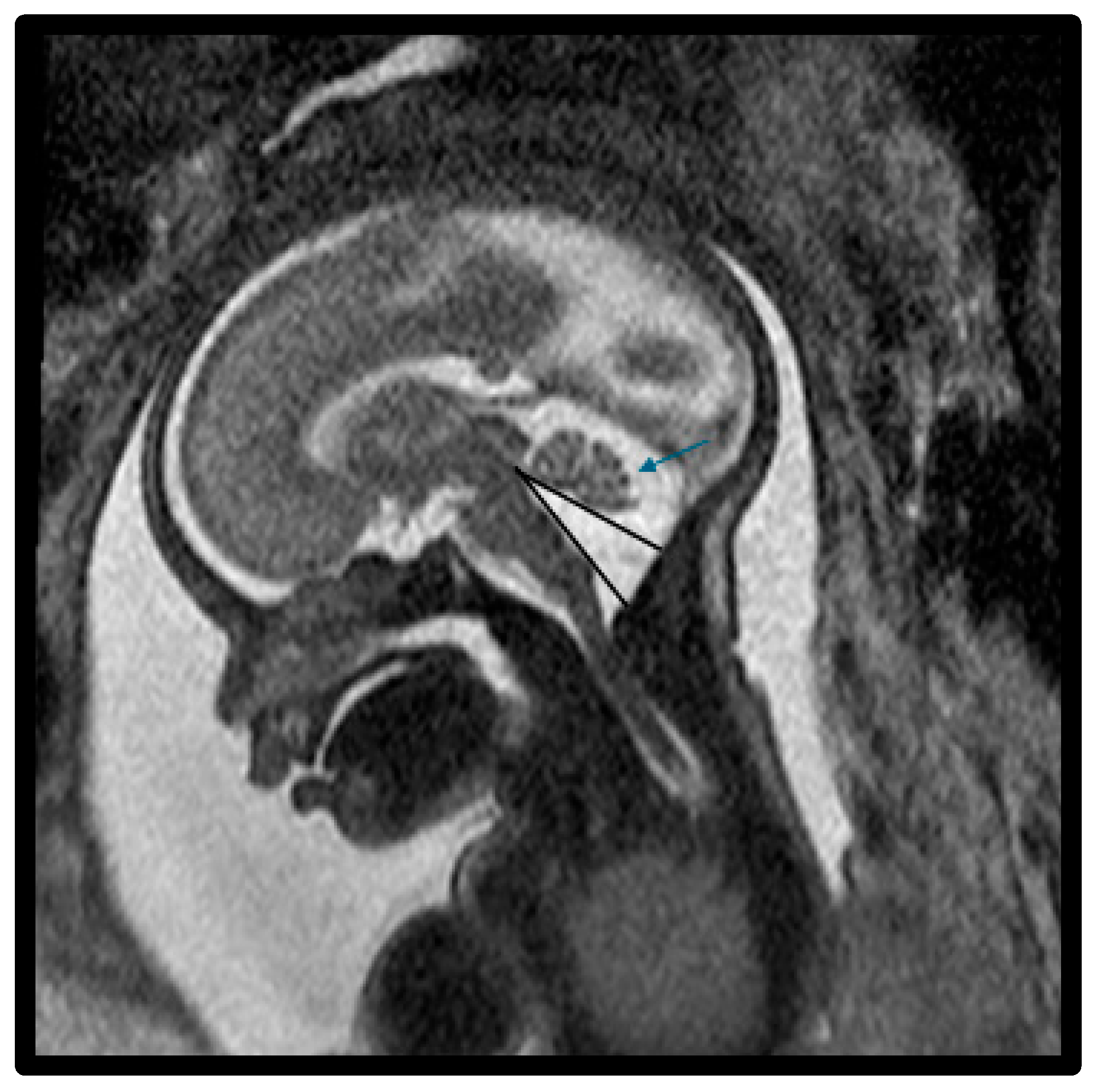
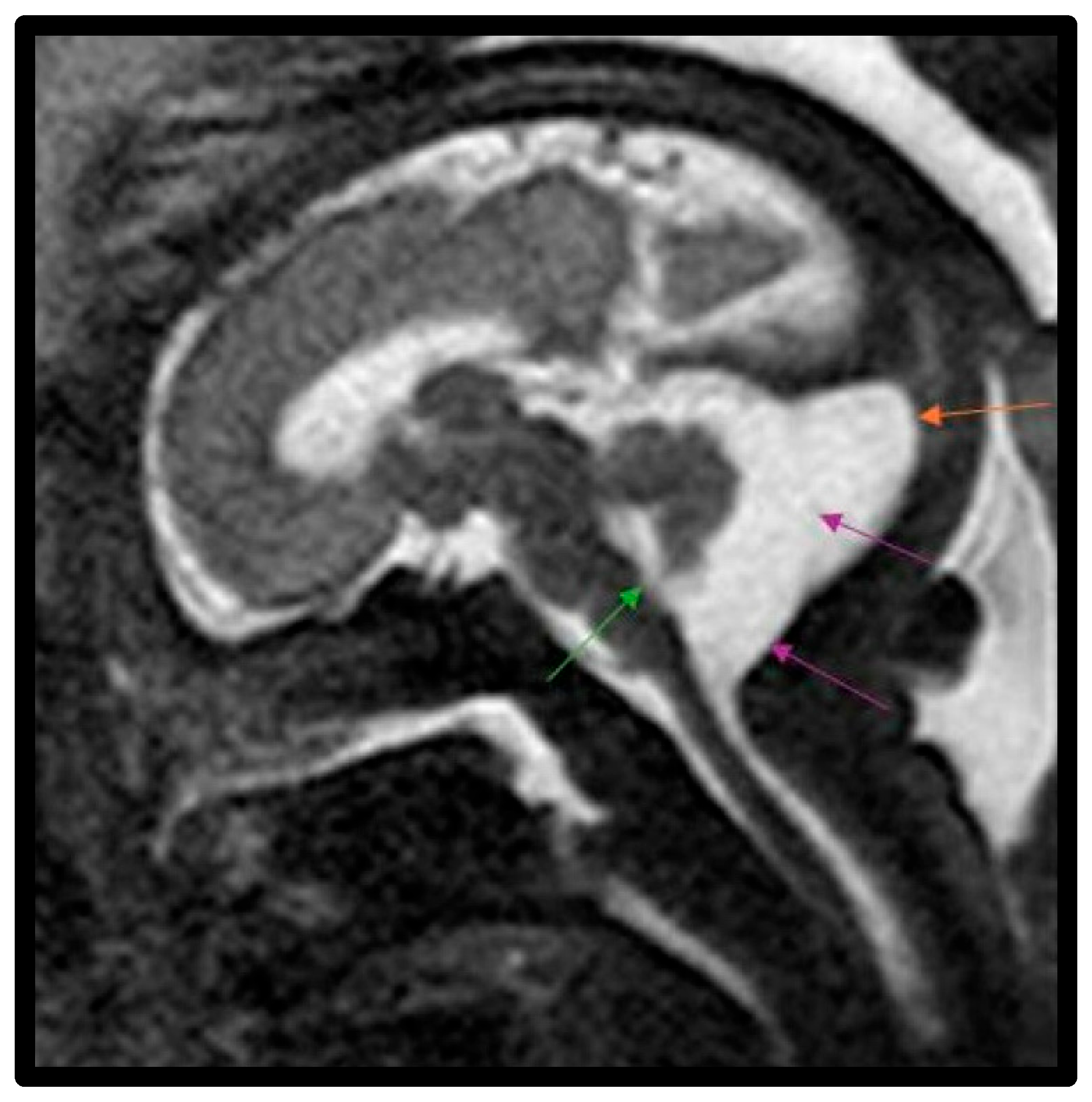
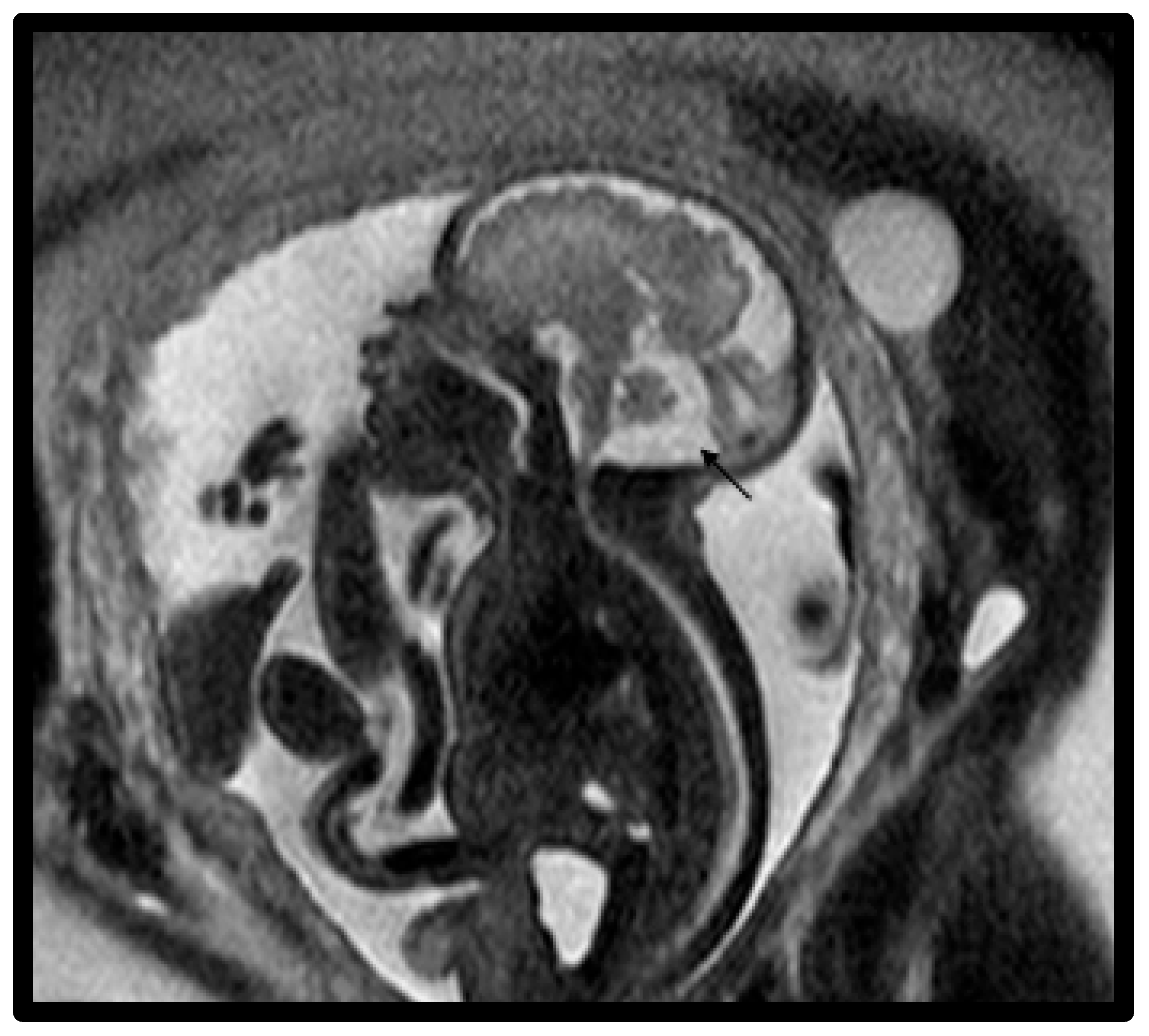
2. Materials and Methods
2.1. Study Population and Design
2.2. Data Collection and Management
2.3. Scanning Parameters for Fetal Magnetic Resonance Imaging
2.4. Classification of Posterior Fossa Malformations on Fetal MRI
2.5. Statistical Analysis
3. Results
- ❖
- Case 1 with DWM was noted to have hydrocephalus, markedly elevated CPK, bilateral talipes equinovarus deformity, overlapping fingers, a vertebral anomaly consisting of fusion of the second and third ribs, and retinal dysgenesis and was clinically diagnosed with Walker–Warburg syndrome.
- ❖
- Case 7 with DWM had a postnatal microarray, which identified a pathogenic 4.1 Mb loss at 3q24q25.1, including Z1C1 and Z1C4, which has been proposed as a critical region for brain anomalies. The entire deleted interval included 32 genes, of which 8 (Z1C1, RNF13, MED12L, HPS3, GYG1, CP, CRLN1, P2RY12) are associated with known clinical disorders.
- ❖
- Case 8 with DWM had one pathogenic change in ASPMc.7783_7786del, p.Lys2595Tyrfs 20 (AR primary microcephaly); a hetA VUS change in TUBGCP4 (AR) c.602G>A, p.Gluy201Asp; and a het A VUS change in MAPK8IP (AD) c.1057G>C, p.Asp353His, het identified.
- ❖
- Case 14 with VH was found to have a duplication of material on the long arm of chromosome X, including part of the FMR1 and AS1-FMR1 genes. In general, a loss of function of the FMR1 gene leads to Fragile X syndrome. It is not clear whether disruption of the gene would lead to a partial or complete loss of FMR1 function, especially since the disruption resulted in a duplication. In this patient, the CNS findings, including microcephaly, were explained by congenital CMV, as urine CMV testing on admission was positive with >3 million copies.
- ❖
- Case 19 with VH was diagnosed with Trisomy 13.
- ❖
- Case 31 with VH, cerebellar hypoplasia, moderate dilation of the lateral ventricles, and mild-to-moderate dilation of the 3rd ventricle was diagnosed with Smith–Lemli–Opitz Syndrome. Additional abnormalities for this infant included balanced AV canal Rastelli type 1 with no coarctation, posterior cleft palate, optic nerve dysplasia, infantile cataracts of both eyes, hearing loss, left talipes equinovarus, bilateral hand and foot polydactyly, a right hip dislocation, and restrictive lung disease due to scoliosis.
4. Discussion
Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Tan, A.G.; Sethi, N.; Sulaiman, S. Evaluation of prenatal central nervous system anomalies: Obstetric management, fetal outcomes and chromosomal abnormalities. BMC Pregnancy Childbirth 2022, 22, 210. [Google Scholar] [CrossRef] [PubMed]
- Garel, C.; Moutard, M.L. Main congenital cerebral anomalies: How prenatal imaging aids counseling. Fetal Diagn. Ther. 2014, 34, 229–239. [Google Scholar] [CrossRef] [PubMed]
- Gorayeb, R.P.; Gorayeb, R.; Berezowski, A.T.; Duarte, G. Effectiveness of psychological intervention for treating symptoms of anxiety and depression among pregnant women diagnosed with fetal malformation. Int. J. Gynaecol. Obstet. 2013, 121, 123–126. [Google Scholar] [CrossRef] [PubMed]
- D’Antonio, F.; Khalil, A.; Garel, C.; Pilu, G.; Rizzo, G.; Lerman-Sagie, T.; Bhide, A.; Thilaganathan, B.; Manzoli, L.; Papageorghiou, A.T. Systematic review and meta-analysis of isolated posterior fossa malformations on prenatal imaging (part 2): Neurodevelopmental outcome. Ultrasound Obstet. Gynecol. 2016, 48, 28–37. [Google Scholar] [CrossRef]
- Garg, N.; Kumar, M.; Rai, P.; Srivastava, S.S.; Gupta, A.; Roy, C.S. Relative prevalence and outcome of fetal posterior fossa abnormality. J. Pediatr. Child. Health. 2023, 59, 107–115. [Google Scholar] [CrossRef]
- Zamora, E.A.; Das, J.M.; Ahmad, T. Dandy-Walker Malformation. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2023. [Google Scholar] [PubMed]
- Barkovich, A.J.; Raybaud, C.A. Congenital malformations of the brain and skull. In Pediatric Neuroimaging, 6th ed.; Barkovich, A.J., Raybaud, C.A., Eds.; Wolters Kluwer: Philadelphia, PA, USA, 2019; p. 531. [Google Scholar]
- Wüest, A.; Surbek, D.; Wiest, R.; Bonel, H.; Steinlin, M.; Raio, L.; Tutschek, B. Enlarged posterior fossa on prenatal imaging: Differential diagnosis, associated anomalies and postnatal outcome. Acta Obstet. Gynecol. Scand. 2017, 96, 837–843. [Google Scholar] [CrossRef] [PubMed]
- Lerman-Sagie, T.; Prayer, D.; Stöcklein, S.; Malinger, G. Fetal cerebellar disorders. Handb. Clin. Neurol. 2018, 155, 3–23. [Google Scholar] [CrossRef] [PubMed]
- Nagaraj, U.D.; Kline-Faith, B.M.; Horn, P.S.; Venkatesan, C. Evaluation of posterior fossa biometric measurements on fetal MRI in the evaluation of Dandy-Walker spectrum. AJNR Am. J. Neuroradiol. 2021, 42, 1716–1721. [Google Scholar] [CrossRef] [PubMed]
- Alsehli, H.; Alshahrani, S.M.; Alzahrani, S.; Ababneh, F.; Alharbi, N.M.; Alarfaj, N.; Baarmah, D. Fetal and neonatal outcomes of posterior fossa anomalies: A retrospective cohort study. Sci. Rep. 2024, 14, 8411. [Google Scholar] [CrossRef]
- Zhang, J.; Guo, C.; Cui, Y.; Liu, Y.; Yao, L.; Zhang, T.; Wang, L.; Han, J.; Zhang, G.; Yan, Y.; et al. Optimal prenatal genetic diagnostic approach for posterior fossa malformation: Karyotyping, copy number variant testing, or whole-exome sequencing? Eur. J. Med. Res. 2024, 29, 397. [Google Scholar]
- Cotes, C.; Bonfante, E.; Lazor, J.; Jadhav, S.; Caldas, M.; Swischuk, L.; Riascos, R. Congenital basis of posterior fossa anomalies. Neuroradiol. J. 2015, 28, 238–253. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Şeker, E.; Aslan, B.; Aydın, E.; Koç, A. Long-term outcomes of fetal posterior fossa abnormalities diagnosed with fetal magnetic resonance imaging. J. Turk. Ger. Gynecol. Assoc. 2023, 24, 28–32. [Google Scholar] [CrossRef]
- Bernardo, S.; Vinci, V.; Saldari, M.; Servadei, F.; Silvestri, E.; Giancotti, A.; Aliberti, C.; Porpora, M.G.; Triulzi, F.; Rizzo, G.; et al. Dandy-Walker malformation: Is the ‘tail sign’ the key sign? Prenat. Diagn. 2015, 35, 1358–1364. [Google Scholar] [CrossRef] [PubMed]
- Whitehead, M.T.; Vezina, G.; Schlatterer, S.D.; Mulkey, S.B.; Plessis, A.J. Taenia-tela choroidea complex and choroid plexus location help distinguish Dandy-Walker malformation and Blake pouch cysts. Pediatr. Radiol. 2021, 51, 1457–1470. [Google Scholar] [CrossRef] [PubMed]
- Paladini, D.; Donarini, G.; Parodi, S.; Volpe, G.; Fulcheri, E. Hindbrain morphometry and choroid plexus position in differential diagnosis of posterior fossa cystic malformations. Ultrasound Obstet. Gynecol. 2019, 54, 207–214. [Google Scholar] [CrossRef] [PubMed]
- Haldipur, P.; Bernardo, S.; Aldinger, K.A.; Sivakumar, T.; Millman, J.; Sjoboen, A.H.; Dang, D.; Dubocanin, D.; Deng, M.; Timms, A.E.; et al. Evidence of disrupted rhombic lip development in the pathology of Dandy-Walker malformation. Acta Neuropathol. 2021, 142, 761–776. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, T.; O’Keane, A.; Vande Perre, S.; Chanclud, J.; Pointe, H.D.; Garel, C.; Blondiaux, E. Fetal imaging of posterior fossa malformations. Pediatr. Radiol. 2025, 55, 747–764. [Google Scholar] [CrossRef]
- Robinson, A.J. Inferior vermian hypoplasia--preconception, misconception. Ultrasound Obstet. Gynecol. 2014, 43, 123–136. [Google Scholar] [CrossRef] [PubMed]
- Robinson, A.J.; Ederies, M.A. Diagnostic imaging of posterior fossa anomalies in the fetus. Semin. Fetal Neonatal Med. 2016, 21, 312–320. [Google Scholar] [CrossRef] [PubMed]
- Barkovich, A.J.; Kjos, B.O.; Norman, D.; Edwards, M.S. Revised classification of posterior fossa cysts and cystlike malfor-mations based on the results of multiplanar MR imaging. AJNR Am. J. Neuroradiol. 1989, 10, 977–988. [Google Scholar] [CrossRef] [PubMed]
- Klein, O.; Pierre-Kahn, A.; Boddaert, N.; Parisot, D.; Brunelle, F. Dandy-Walker malformation: Prenatal diagnosis and prognosis. Childs Nerv. Syst. 2003, 19, 484–489. [Google Scholar] [CrossRef] [PubMed]
- Di Nora, A.; Costanza, G.; Pizzo, F.; Di Mari, A.; Sapuppo, A.; Basile, A.; Fiumara, A.; Pavone, P. Dandy-Walker malformation and variants: Clinical features and associated anomalies in 28 affected children-a single retrospective study and a review of the literature. Acta Neurol. Belg. 2023, 123, 903–909. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Garel, C. Fetal cerebral biometry: Normal parenchymal findings and ventricular size. Eur. Radiol. 2005, 15, 809–813. [Google Scholar] [CrossRef] [PubMed]
- Tilea, B.; Alberti, C.; Adamsbaum, C.; Armoogum, P.; Oury, J.F.; Cabrol, D.; Sebag, G.; Kalifa, G.; Garel, C. Cerebral biometry in fetal magnetic resonance imaging. Ultrasound Obstet. Gynecol. 2009, 33, 173–181. [Google Scholar] [CrossRef] [PubMed]
- Chapman, T.; Menashe, S.J.; Zare, M.; Alessio, A.M.; Ishak, G.E. Establishment of normative values for the fetal posterior fossa by magnetic resonance imaging. Prenat. Diagn. 2018, 38, 1035–1041. [Google Scholar] [CrossRef] [PubMed]
- Kline-Fath, B.; Bulas, D.I.; Lee, W. Fundamental and Advanced Fetal Imaging, 2nd ed.; Wolters Kluwer: Philadelphia, PA, USA, 2020. [Google Scholar]
- Chapman, T.; Mahalingam, S.; Ishak, G.E.; Nixon, J.N.; Siebert, J.; Dighe, M.K. Diagnostic imaging of posterior fossa anomalies in the fetus and neonate: Part 2, Posterior Fossa Disorders. Clin. Imaging 2015, 39, 167–175. [Google Scholar] [CrossRef] [PubMed]
- Saleem, S.N. Fetal MRI: An approach to practice: A review. J. Adv. Res. 2014, 5, 507–523. [Google Scholar] [CrossRef] [PubMed]
- Snyder, E.; Baschat, A.; Huisman, T.A.G.M.; Tekes, A. Value of Fetal MRI in the Era of Fetal Therapy for Management of Abnormalities Involving the Chest, Abdomen, or Pelvis. Am. J. Roentgenol. 2018, 210, 998–1009. [Google Scholar] [CrossRef] [PubMed]
- De Catte, L.; De Keersmaeker, B.; Claus, F. Prenatal neurologic anomalies: Sonographic diagnosis and treatment. Paediatr. Drugs. 2012, 14, 143–155. [Google Scholar] [CrossRef] [PubMed]
- Griffiths, P.D.; Bradburn, M.; Campbell, M.J.; Cooper, C.L.; Graham, R.; Jarvis, D.; Kilby, D.M.; Mason, G.; Mooney, C.; Robson, S.C.; et al. Use of MRI in the diagnosis of fetal brain abnormalities in utero (MERIDIAN): A multicentre, prospective cohort study. Lancet 2017, 389, 538–546. [Google Scholar] [CrossRef] [PubMed]
- Griffiths, P.D.; Bradburn, M.; Campbell, M.J.; Cooper, C.L.; Embleton, N.; Graham, R.; Hart, A.R.; Jarvis, D.; Kilby, M.D.; Lie, M.; et al. MRI in the diagnosis of fetal developmental brain abnormalities: The MERIDIAN diagnostic accuracy study. Health Technol. Assess. 2019, 23, 1–144. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Gandolfi, C.G.; Contro, E.; Carletti, A.; Ghi, T.; Campobasso, G.; Rembouskos, G.; Volpe, G.; Pilu, G.; Volpe, P. Prenatal diagnosis and outcome of fetal posterior fossa fluid collections. Ultrasound Obstet. Gynecol. 2012, 39, 625–631. [Google Scholar] [CrossRef] [PubMed]
- Cornips, E.M.; Overvliet, G.M.; Weber, J.W.; Postma, A.A.; Hoeberigs, C.M.; Baldewijns, M.M.; Vles, J.S. The clinical spectrum of Blake’s pouch cyst: Report of six illustrative cases. Child’s Nerv. Syst. 2010, 26, 1057–1064. [Google Scholar] [CrossRef] [PubMed]
- Nagaraj, U.D.; Kline-Fath, B.M.; Calvo-Garcia, M.A.; Vadivelu, S.; Venkatesan, C. Fetal and postnatal MRI findings of Blake pouch remnant causing obstructive hydrocephalus. Radiol. Case Rep. 2020, 15, 2535–2539. [Google Scholar] [CrossRef]
- Murali, L.; Rangasami, R.; Priyanka, C.; Suresh, I.; Suresh, S. Assessment of fastigial angle in fetuses with Blake pouch cyst and vermian hypoplasia on magnetic resonance imaging. J. Pediatr. Neurosci. 2024, 19, 39–44. [Google Scholar] [CrossRef]
- Limperopoulos, C.; Robertson, R.L.; Estroff, J.A.; Barnewolt, C.; Levine, D.; Bassan, H.; Plessis, A.J. Diagnosis of inferior vermian hypoplasia by fetal magnetic resonance imaging: Potential pitfalls and neurodevelopmental outcome. Am. J. Obstet. Gynecol. 2006, 194, 1070–1076. [Google Scholar] [CrossRef] [PubMed]
- Tarui, T.; Limperopoulos, C.; Sullivan, N.R.; Robertson, R.L.; Plessis, A.J. Long-term developmental outcome of children with a fetal diagnosis of isolated inferior vermian hypoplasia. Arch. Dis. Child. Fetal Neonatal Ed. 2014, 99, F54–F58. [Google Scholar] [CrossRef] [PubMed]
- Patek, K.J.; Kline-Fath, B.M.; Hopkin, R.J.; Pilipenko, V.V.; Crombleholme, T.M.; Spaeth, C.G. Posterior fossa anomalies diagnosed with fetal MRI: Associated anomalies and neurodevelopmental outcomes. Prenat. Diagn. 2012, 32, 75–82. [Google Scholar] [CrossRef] [PubMed]
- D’Antonio, F.; Khalil, A.; Garel, C.; Pilu, G.; Rizzo, G.; Lerman-Sagie, T.; Bhide, A.; Thilaganathan, B.; Manzoli, L.; Papageorghiou, A.T. Systematic review and meta-analysis of isolated posterior fossa malformations on prenatal ultrasound imaging (Part 1): Nomenclature, diagnostic accuracy and associated anomalies. Ultrasound Obstet. Gynecol. 2016, 47, 690–697. [Google Scholar] [CrossRef] [PubMed]
- Vahedifard, F.; Adepoju, J.O.; Supanich, M.; Ai, H.A.; Liu, X.; Kocak, M.; Marathu, K.K.; Byrd, S.E. Review of deep learning and artificial intelligence models in fetal brain magnetic resonance imaging. World J. Clin. Cases 2023, 11, 3725–3735. [Google Scholar] [CrossRef]

| Fetuses with Suspected Posterior Fossa Lesions Referred for Fetal MRI | |
|---|---|
| Maternal and Birth Characteristics | |
| Maternal age at delivery (years), mean ± SD | 27 ± 6 |
| Gestational age (weeks) at fetal MRI, mean ± SD | 26.5 ± 5.8 |
| Maternal comorbid diagnoses, N (%) | |
| Preeclampsia | 1 (3%) |
| Gestational or chronic hypertension | 5 (15%) |
| Gestational diabetes | 3 (9%) |
| Teen pregnancy | 3 (9%) |
| Advanced maternal age | 4 (12%) |
| Race/ethnicity, N (%) | |
| White | 9 (26.5%) |
| Black | 16 (47%) |
| Hispanic | 9 (26.5%) |
| Other | 0 (0%) |
| Cesarean delivery, N (%) | 9 (26.5%) |
| Apgar score | |
| 1 min, median (25th, 75th) | 8 (4, 9) |
| 5 min, median (25th, 75th) | 9 (9, 9) |
| Birth order | |
| Singleton | 34 (100%) |
| Multiple gestation | 0 (0%) |
| Insurance | |
| Commercial | 16 (47%) |
| Medicaid | 17 (50%) |
| Unknown or no insurance | 1 (3%) |
| Teratogenic exposures during pregnancy | 4 (11.8%) |
| Amniocentesis | |
| Normal karyotype and microarray | 13 (38%) |
| Abnormal results | 1 (3%) |
| Birth weight (g), mean ± SD | 2892 ± 558 |
| Birth gestational age (weeks), mean ± SD | 37 ± 4 |
| Male sex, N (%) | 16 (47%) |
| Clinical Characteristics and Hospital Course | |
| Fetal MRI findings b | |
| Isolated prominent or enlarged cisterna magna | 5 (15%) |
| Blake’s pouch cyst | 6 (18%) |
| Classic Dandy–Walker cyst | 7 (21%) |
| Vermian hypoplasia | 13 (38%) |
| Arachnoid cyst | 1 (3%) |
| Encephalomalacia or schizencephaly | 1 (3%) |
| Dysgenesis of the corpus callosum with colpocephaly | 1 (3%) |
| Imaging characteristics | |
| Postnatal imaging confirmed fetal MRI findings a | 20 (87%) |
| Postnatal imaging findings disagreed with fetal MRI findings | 3 (13%) |
| VP shunt placement | |
| During NICU admission | 3 (9%) |
| After NICU discharge | 1 (3%) |
| Seizure disorder | 2 (6%) |
| Mode of feeding at NICU discharge (N = 18) | |
| PO ad lib on demand | 14 (78%) |
| Gastrotomy tube feedings | 3 (17%) |
| Parenteral nutrition | 1 (6%) |
| Congenital infection | |
| CMV | 1 (3%) |
| Coxsackie | 1 (3%) |
| Postnatal genetic testing | |
| Normal | 13 (38%) |
| Abnormal c | 6 (18%) |
| Not sent/unknown | 15 (44%) |
| Disposition | |
| Inborn live birth | 22 (65%) |
| Outborn | 12 (35%) |
| Interruption of pregnancy based on fetal MRI findings | 1 (3%) |
| IUFD | 2 (6%) |
| NICU LOS (day), median (25th, 75th) | 8 (3, 32) |
| Live birth with death before NICU discharge, N (%), n = 22 | 4 (18%) |
| DWM (n = 6) # | VH (n = 14) | BPC (n = 6) | p-Value | |
|---|---|---|---|---|
| Vermis height (mm) | 5.0 ± 2.6 (n = 6) | 6.9 ± 2.8 | 9.5 ± 2.7 | 0.09 (NS) |
| Vermis AP (mm) * | 10.8 ± 6.2 (n = 6) | 11.8 ± 3.0 | 14.8 (SD, 3.3) | 0.002 |
| TVA (°) * | 93.7° ± 18.1° (n = 6) | 50.9° ± 17.3° | 21.7° (SD, 15.5°) | <0.001 |
| Enlarged CM * | 7/7 (100%) | 7/14 (50%) | 3/6 (50%) | 0.002 |
| Case | Prenatal US Findings | Fetal MRI Findings | Postnatal Imaging |
|---|---|---|---|
| 1 | Suspected DWM | Classic DWM | Classic DWM |
| 2 | Suspected DWM | Classic DWM | Not available |
| 3 | Hydrocephalus, large DWM, large supratentorial cyst, very little brain tissue remaining, and no evidence of cerebellar tissue. | Classic DWM | Large DW cyst occupying posterior half of the intracranial cavity. In the supratentorial region, there was a large cystic structure that represented a combination of the lateral ventricles and third ventricle under pressure from massive hydrocephalus. Small rim of cortical cerebral tissue along interior and lateral aspect of the supratentorial region. Thin brainstem. |
| 4 | Hydrocephalus, CNS anomaly. | DWM, massive DW cyst, encephalomalacia vs. schizencephaly. | Not available |
| 5 | CNS anomaly | Classic DWM, colopocephaly, dysgenesis of the CC, nodular heterotopia, holoprosencephaly. | CNS malformations include ACC and cerebellar abnormalities. |
| 6 | DWM with retrocerebellar DW cyst, mild supratentorial hydrocephalus. | Classic DWM | DWM and thin CC |
| 7 | Macrocephaly and DWM | Classic DWM | Classic DWM |
| 8 | DWM, absent CC, clubfeet, and SUA. | Classic DWM with ACC | Classic DWM, ACC with colpocephaly and migrational abnormalities involving the bifrontal parietal regions, and diffusely gracile brainstem. |
| 9 | Hydrocephalus | DWM with no thalamus or spinal cord. | Not available due to IUFD |
| 10 | CNS anomaly | VH | VH |
| 11 | BPC vs. VH vs. DWM | VH | Not available |
| 12 | Suspected VH vs. DWM | VH | VH |
| 13 | Suspected DWM | VH | Not available due to IUFD |
| 14 | Congenital CMV and suspected DWM. | VH | VH and calcifications and diffuse marked brain parenchymal loss from congenital CMV. |
| 15 | FGR, enlarged CM, VH | VH | Not available |
| 16 | Suspected DWM with partial absence of inferior portion of the posterior lobe of the vermis with mild-to-moderate widening of the vallecula. | VH | VH |
| 17 | Suspected DWM | VH | Mild prominence of 4th ventricle and CM. Normal ventricles. Repeat HUS was normal. |
| 18 | Dilated posterior fossa, absent cerebellar vermis, micrognathia, absent nasal bone. | VH | VH, hypoplasia of inferior cerebellar vermis, mild prominence/enlargement of 4th ventricle, mild prominence/enlargement of the vallecula, absence of the inferior aspect of the vermis of the cerebellum, and a small retrocerebellar cyst vs. enlargement of the CM. Normal posterior fossa structures including normal cerebellum and brainstem. Normal spine. |
| 19 | Suspected common atrium, perimembraneous VSD (AVSD), and DW spectrum malformation. | VH | DCC and DW variant, mineralizing vasculopathy of the basal ganglia. |
| 20 | Absence of inferior vermis. Fourth ventricle slightly enlarged and opened into a retrocerebellar cyst vs. CM consistent with DW variant. Cerebellar hemispheres were small but appeared normal for gestational age. Normal supratentorial region, fetal spine, and spinal cord. | VH | Not available |
| 21 | DW variant with cerebellar hypoplasia vs. isolated cerebellar hypoplasia. | VH | Not available |
| 22 | Suspected CNS anomaly | VH | VH, brain MRI showed partial aplasia of the cerebellum and vermis consistent with a very mild DW variant. |
| 23 | Mild inferior VH, right renal agenesis vs. right ectopic kidney, absent nasal bone, small pericardial effusion and LV hypertrophy, possible VSD. | VH | VH with DWM, hypoplastic cerebellum |
| 24 | Enlarged CM | BPC | Not available |
| 25 | BPC vs. enlarged CM | BPC | BPC |
| 26 | BPC vs. enlarged CM | BPC | Enlarged CM |
| 27 | Suspected bilateral polymicrogyria with enlarged CM and BPC, ventricles on the upper limit of normal, brain appears dysmature for stated age, and progressive IUGR. | BPC with polymicrogyria | Not available |
| 28 | Bilateral CDH with liver up, IUGR, BPC with no associated mass effect of hydrocephalus, no cerebellar VH, and high likelihood of ECMO due to severe pulmonary hypoplasia and risk of pulmonary hypertension. | BPC | Postnatal imaging was not obtained due to the severity of CDH. |
| 29 | Arachnoid cyst | Arachnoid cyst | Large PF cyst with mild mass effect on the cerebellar hemispheres, normal-appearing vermis and vallecula, and elevation of torcula consistent with arachnoid cyst within the CM. Subcutaneous fluid collection in the occipital region, which measured 7 mm in maximal width. Bilateral closed lip schizencephaly with polymicrogyria. Increased cortical gray matter with small sulci along portions of the bilateral frontal lobes, consistent with polymicrogyria. No hydrocephalus. |
| 30 | Enlarged CM | Enlarged CM | Not available |
| 31 | Suspected DWM, left talipes equinovarus, and AVSD. | Enlarged CM | Postnatal imaging was not consistent with DWM, mild dilation of lateral ventricles and superior 3rd ventricle, and cerebellar hypoplasia with prominent inferior basal cisterns. |
| 32 | Enlarged CM | Enlarged CM | Not available |
| 33 | Enlarged CM | Enlarged CM | Normal brain MRI |
| 34 | Hydrocephalus, polycystic kidney, two-vessel umbilical cord. | Enlarged CM | Colpocephaly, absence of the septum pellucidum, mild fullness of the 3rd ventricle, posterior fossa fluid collection, and left occipital echogenicity. Brain MRI showed marked dilatation of the lateral ventricle, mild dilatation of the 3rd ventricle with no septum pellucidum and vein CC, mega CM, possible hypoplastic cerebellum, left-sided parietal occipital infarct. |
| Case | PFM Type on fMRI | Additional Imaging Findings | GA at fMRI | Genetic or Unifying Diagnosis | Pregnancy Outcome | Brief Narrative Summary of Newborn Clinical Course |
|---|---|---|---|---|---|---|
| 1 | Classic DWM | Moderate to severe hydrocephalus, thin CC, hypoplastic cerebellum, large PF. | 34 | Walker-Warburg syndrome | Live birth, discharged with home hospice. | Term male, C/S delivery, admitted to NICU for 34 days. Microcephalic, overlapping fingers, bilateral talipes equinovarus deformity, hypotonicity, absent suck/swallow, decreased reflexes, dysmorphic features, retinal dysgenesis, reduced life expectancy. Discharged with home hospice and TPN via Broviac due to feeding intolerance. VP shunt placed. |
| 2 | Classic DWM | No hydrocephalus, normal cerebellum, mild DW cyst. | 25 | ---- | Outborn | Postnatal course not available due to outborn status. |
| 3 | Classic DWM | Absent cerebellum, large PF, dilated 4th ventricle, enlarged CM, severe hydrocephalus, massive DW cyst, small and thin brainstem. | 31 | Normal karyotype and microarray | Live birth, died before discharge. | Preterm C/S delivery, intubated in DR due to poor tone, no respiratory effort, central cyanosis, bradycardia, and massive macrocephaly. EEG showed global neuronal dysfunction. Imaging showed hydranencephaly. Respiratory failure with apnea and respiratory acidosis. Infant was compassionately extubated and died on day of life 7. Autopsy showed macrocephaly, posterior fossa cyst, severe cerebellar hypoplasia and partial hypoplasia of the brainstem, severe hydrocephalus with severe atrophy of cerebellar cortices, and no deep gray matter structures identified. Abnormal heart congenital polyvalvular disease moderate type was diagnosed with stenosis of tricuspid, mitral and aortic valves, and atypical hypertrophic cardiomyopathy. Liver with islands of extramedullary erythropoiesis. |
| 4 | Classic DWM | Absent cerebellum, enlarged PF, dilated 4th ventricle, enlarged CM, severe hydrocephalus, massive DW cyst, encephalomalacia or schizencephaly, hypoplastic brainstem, thin cerebral hemispheres. | 33 | ---- | Outborn | Postnatal course not available due to outborn status. |
| 5 | Classic DWM | Normal cerebellum, enlarged PF, normal 4th ventricle, enlarged CM, normal torcula, mild-to-moderate hydrocephalus, DCC, colpocephaly, DW cyst, nodular heterotopia, holoprosencephaly. | 19 | Normal karyotype and microarray | Interruption of pregnancy with D&E at 20 weeks gestation. | Autopsy showed SUA, CNS malformations, as described prenatally, including ACC and cerebellar abnormalities, and postaxial polydactyly of the right hand and right foot. |
| 6 | Classic DWM | Hypoplastic vermis & cerebellum, enlarged PF, dilated 4th ventricle, enlarged CM, normal torcula, mild supratentorial hydrocephalus, DWM with retrocerebellar DW cyst, aqueductal stenosis, thinning of CC, absent CSP. | 21 | Normal karyotype and microarray | Live birth | Admitted to NICU with hydrocephalus in the setting of congenital DWM. No seizures during NICU admission. VP shunt placed for hydrocephalus. Discharged home on PO ad lib feedings. |
| 7 | Classic DWM | Severely hypoplastic cerebellum, enlarged PF, dilated 4th ventricle, enlarged CM, elevated torcula, moderate hydrocephalus. | 31 | Pathogenic 4.1 Mb loss at 3q24q25.1, including ZIC1 and ZIC4, a critical region for brain anomalies that explained infant’s clinical findings. Deleted interval included 32 genes, 8 of which (ZIC1, RNF13, MED12L, HPS3, GYG1, CP, CRLN1, P2RY12) are associated with known clinical disorders. | Live birth | C/S delivery, admitted to NICU. Postnatal imaging confirmed large posterior fossa DWM. VP shunt placed for hydrocephalus. Discharged home on PO ad lib feedings with anti-reflux formula. No seizures during NICU admission. |
| 8 | Classic DWM | Hypoplastic cerebellum, enlarged posterior fossa, enlarged 4th ventricle, enlarged CM, normal torcula, no hydrocephalus, DWM cyst, ACC. | 25 | Seizure panel identified 3 VUS changes in FASN, SLC12AS, and SLC6A. Brain malformation panel identified pathogenic change in ASPM c.7783_7786del, p.Lys2595Tyrfs 20 (AR primary microcephaly); het A VUS change in TUBGCP4 (AR) c.255C>A, p.Tyr85; het A VUS change in B9D1 (AR) c.602G>A, p.Gluy201Asp; het A VUS change in MAPK8IP (AD) c.1057G>C, p.Asp353His, het. | Live birth | C/S delivery. Infant with clubfeet and single umbilical artery. LOS was 36 days in the NICU. Seizures, inability to feed safely by mouth requiring GT placement, cardiomyopathy requiring heart failure medications. Postnatal imaging consistent with areas of heterotopia superimposed on DWM with ACC and mild left hydronephrosis. VP shunt placed for hydrocephalus. |
| 9 | Classic DWM | Hydrocephalus. | 16 | Normal karyotype | IUFD | Postnatal radiograph confirmed stillborn female with bell-shaped thorax and multiple congenital anomalies. |
| 10 | VH | Prominent CM. No cerebellar hypoplasia. Remote microhemorrhages in left cerebellar hemisphere. | 19 | No testing available | Live birth | NSVD with unremarkable newborn nursery course, discharged home with normal neurological exam at nursery discharge. |
| 11 | VH | Flattened globes. | 22 | No testing available | Live birth | Live birth at OSH per maternal records, postnatal course not available in EMR. |
| 12 | VH | No hydrocephalus. | 30 | Normal karyotype and microarray | Live birth | Prolonged NICU hospitalization with VH confirmed. Severe disabilities, including right facial deformity with malformed ear and facial droop, respiratory failure requiring tracheostomy and mechanical ventilation, gastrostomy tube dependence, hearing impairment, and vision impairment. |
| 13 | VH | --------------------------- | 22 | Normal karyotype and microarray | IUFD | IUFD in the setting of FGR with teratogenic maternal exposure to methimazole during pregnancy and maternal Graves’ disease. |
| 14 | VH | Calcifications in the basal ganglia, thalami, and diffuse grey matter, including parenchymal and lateral ventricular wall calcifications consistent with congenital CMV. Marked ventriculomegaly suggestive of brain volume loss. Abnormal cortical development and migration. Intraventricular hemorrhage with fluid levels within bilateral lateral ventricles and 4th ventricle and cystic lesions. | 30 | Congenital CMV. Genetic testing noted duplication of material on the long arm of chromosome X, including part of the FMR1 and AS1-FMR1 genes. | Live birth | Congenital CMV. Coagulopathic at birth with a diffuse rash, calcifications on head US, retinitis, and microcephaly (<1st %ile). Neurological exam notable for lower extremity spasticity. Passed newborn hearing screen. |
| 15 | VH | Hypoplastic vermis, enlarged CM without cerebral ventriculomegaly. Fetal imaging notable for echogenic bowel, globular and thickened placenta suggestive of fetal infection vs. chromosomal anomaly, fetal echo with normal cardiac structure. | 21 | No testing available | Outborn | Outborn infant, postnatal course not available in EMR. |
| 16 | VH | Partial absence of inferior portion of vermis with mild-to-moderate widening of vallecula. Normal 4th ventricle. Postnatal brain MRI confirmed mild inferior VH, mild superior rotation of vermis with a normal-sized PF. | 36 | Normal prenatal screening | Live birth | C/S delivery with benign postnatal course. Normal neurological exam. Discharged home with mother on day of life 3 from the general care nursery feeding PO ad lib. |
| 17 | VH | Postnatal HUS showed prominence of 4th ventricle and CM with normal lateral ventricles, cerebellar vermis not well visualized. | 20 | Normal prenatal screening, CMV and toxoplasmosis testing were negative. | Live birth | C/S delivery, admitted to the NICU. CONS bacteremia. Normal eye exam without chorioretinitis. Passed hearing screen. Infant had normal growth and development at routine well-child checks through 15 months of age. |
| 18 | VH | Fetal US with dilated PF, absent cerebellar vermis, absent nasal bone, micrognathia. Postnatal HUS showed hypoplasia of inferior cerebellar vermis, enlarged 4th ventricle. Postnatal brain MRI showed mild enlargement of 4th ventricle, absent inferior aspect of cerebellar vermis, and small retro-cerebellar cyst with enlargement of CM. Normal brainstem and cerebellum. | 25 | Normal karyotype and microarray | Live birth | C/S delivery, unremarkable newborn nursery course with normal neurological exam. Well-child exams through to age 11 years with normal neurological exam with normal strength, tone, and developmental milestones. |
| 19 | VH | Postnatal HUS showed mineralizing vasculopathy in basal ganglia (can be seen in aneuploidy). Possible dysgenesis of the CC and hypoplastic vermis. Rectangular fluid-filled space between the brainstem and cerebellum continuous with expected location of 4th ventricle. Incomplete anterior portion of the cerebellum at the midline. | 23 | Trisomy 13 | Live birth | C/S delivery. Severe PPHN that required high-frequency oscillatory ventilation. Significantly constricted distal pulmonary arteries with no surgical repair possible. Congenital heart deformity with common atrium, large VSD, bicuspid aortic valve, large PDA. Polydactyly of left foot with supernumerary digit at lateral foot attached at 5th toe near MTP joint that contained 2 hypoplastic phalanges. Chromosomes confirmed Trisomy 13. Infant died before NICU discharge after compassionate redirection of care. |
| 20 | VH | 19 | No testing available | Live birth | Liveborn female based on maternal records but infant’s postnatal records not available in EMR. | |
| 21 | VH | 21 | No testing available | Outborn | Postnatal course not available | |
| 22 | VH | Postnatal head US showed no IVH or ventricular dilation with possible deficiency of the cerebellar vermis. Brain MRI showed partial aplasia of cerebellum and vermis. | 22 | Normal male karyotype (46 XY) on amniocentesis, FISH was normal. | Live birth | NSVD due to maternal preterm labor at 31 weeks, 41-day NICU stay with benign course, room air, PO ad lib feedings, normal developmental exam, passed hearing screen. |
| 23 | VH | Prenatal imaging showed mild inferior VH, right renal agenesis vs. right ectopic kidney, absent nasal bone, small pericardial effusion and LV hypertrophy, possible VSD. Postnatal imaging showed VH and hypoplastic cerebellum. | 29 | Amniocentesis normal karyotype & microarray. Noonan panel with heterozygous variant of uncertain significance in BRAF gene identified, c.786A>G, pGln262=. Amniotic fluid with higher titer for Coxsackie virus (1:8) consistent with resolving infection. | Live birth | Term male C/S delivery at term, admitted to NICU for 18-day LOS, discharged in room air, PO ad lib feeding. Postnatal imaging confirmed VH, right ectopic kidney in the iliac fossa, two tiny VSDs, ventral hernia, multiple midline lesions including epulis of gum, cyst on lip, bifurcated gluteal folds, asymmetry of testes, supernumerary nipple, closed left clavicular fracture. Right-sided sensorineural hearing loss. |
| 24 | BPC | Fetal US concerning for enlarged CM, found to be BPC on fMRI. | 36 | No testing available | Outborn | Postnatal course not available |
| 25 | BPC | Fetal US with enlarged CM vs. BPC, found to be BPC on fMRI, postnatal HUS showed BPC. | 34 | cfDNA low risk for aneuploidy or sex chromosome disorders. | Live birth | C/S delivery, 4-day LOS, phototherapy for hyperbilirubinemia, discharged home with mother from GCN feeding PO ad lib in room air. Postnatal HUS showed BPC. |
| 26 | BPC | Fetal US with MCM vs. BPC. FMRI suggestive of BPC. Postnatal brain MRI most consistent with MCM. | 23 | cfDNA low risk for aneuploidy or sex chromosome disorders. | Live birth | C/S delivery, unremarkable newborn course, discharged home from GCN on DOL 2 feeding PO ad lib in room air. Postnatal imaging consistent with MCM. |
| 27 | BPC | Fetal US with FGR, suspected bilateral polymicrogyria with enlarged CM and BPC, ventricles upper limit of normal, brain dysmature for stated age. | 31 | Declined amniocentesis, low risk quad screen. | Live birth | Apgar scores 8 and 9, admitted to the NICU, details of hospital course unavailable in EMR. |
| 28 | BPC | Fetal US notable for FGR, BPC, bilateral CDH with pulmonary hypoplasia, estimated lung volumes ~20% of expected. | 25 | Amniocentesis with normal karyotype and microarray. | Live birth | C/S delivery, postnatal course complicated by severe CDH with pulmonary hypoplasia, death in NICU within 24 h of birth after redirection to comfort care. |
| 29 | CM | Enlarged CM on fetal US confirmed on fetal MRI. | 30 | No testing available. | Outborn | Postnatal course not available. |
| 30 | MCM + CNS anomalies | Prenatal US with MCM, arachnoid cyst, absent CSP, hydrocephalus, SUA, polycystic kidney. Postnatal HUS: absent CSP, colpocephaly, mild 3rd ventricle dilation, PF fluid collection, left occipital echogenicity. Postnatal brain MRI showed marked lateral ventricle dilation, mild 3rd ventricle dilatation, absent CSP, MCM, possible hypoplastic cerebellum, left parietal–occipital infarct. | 32 | Amniocentesis with normal karyotype and microarray. | Live birth | NSVD, LOS was 6 days in NICU, diagnosed with left MCDK, absent CSP, DCC, hypoplastic cerebellum, left partial occipital cerebrovascular accident, MCM, bilateral optic nerve hypoplasia, left T4 hemivertebrae with mild levoscoliosis. Treated with phototherapy for hyperbilirubinemia. VP shunt placed by NSGY at 2 months of age as an outpatient. VP shunt placed for hydrocephalus. |
| 31 | MCM | Prenatal US with left talipes equinovarus, AVSD, possible DW spectrum disorder. Postnatal head CT showed moderate dilatation lateral ventricles, moderate 3rd ventricle dilation, mild 4th ventricle enlargement. No obstructive hydrocephalus. Prominent cortical sulci of both cerebral hemispheres. Prominent CSF space but no mass effect. Cerebellar hypoplasia with prominent inferior basal cisterns. Cortical volume loss and atrophy in the setting of Smith–Lemli–Opitz syndrome. | 36 | Amniocentesis with 46XX, diagnosed with Smith–Lemli–Opitz syndrome in infant of a mother with gestational DM requiring insulin. | Live birth | NVSD with NICU LOS was 102 days. Smith–Lemli–Optiz syndrome. No seizures. Balanced AVSD Rastelli type 1, cleft palate, left talipes equinovarus, bilateral hand and foot polydactyly, and hyponatremia. Medical NEC. CPAP for poor aeration and respiratory acidosis. GT placed for feeding challenges. Intubated for heart failure, treated with Lasix, Digoxin, and Captopril with improvement. Hypertension due to autonomic instability. Global developmental delay (non-verbal and non-ambulatory). Failed hearing screen. Scoliosis, right hip dislocation, and wheelchair bound. Infantile cataracts of both eyes, post-bilateral cataract extraction with intraocular lens implantation. Slow photoreceptor recovery time, optic nerve demyelination, and optic nerve hypoplasia. Restrictive lung disease due to scoliosis. Death at age 9 years from sepsis. |
| 32 | Enlarged CM | Enlarged CM on fetal US, confirmed on fetal MRI. | 26 | No testing available | Outborn | Postnatal course not available |
| 33 | Enlarged CM | Postnatal brain MRI showed normal brain with marginal CM enlargement. | 32 | No testing available | Live birth | Normal postnatal brain imaging, normal neurological exam at birth, discharged home from GCN after uneventful newborn nursery course. |
| 34 | Arachnoid cyst | Postnatal brain MRI notable for arachnoid cyst and bilateral closed lip schizencephaly with polymicrogyria. | 33 | Low risk cfDNA, microarray showed: arr(122)x2, (XY)x1. Extended contiguous regions of allele homozygosity (ROH > 8 Mb) in multiple chromosomes consistent with common descent, 50.35 Mb total (1.89% of autosomal genome). No known consanguinity but from same village in Mexico. ROH Bp linear position: chr1:159775332-169090660. chr1:229984949-238623222. chr4:165411055-181814242. chr20:41192992-57181430. Congenital brain malformation panel with multiple VUS as follows: LAMB1 (AR) c.4156CA, p.Gln1386Lys, heterozygous VUS. RAB3GAP2 (AR) c.1609GA, p.Val537Ile, Heterozygous VUS. TMEM231 (AR) c.757GA, p.Gly253Arg, heterozygous VUS. PCLO (AR) c.13434GT, p.Glu4478Asp, heterozygous VUS.TMEM67 (AR) c.167510dup, intronic, heterozygous VUS. | Live birth | NVSD, briefly admitted to the NICU with transient tachypnea of the newborn requiring CPAP but was quickly weaned to room air and transferred to the GCN. Discharged home on DOL 3 in room air, feeding PO ad lib. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bowker, R.M.; Marathu, K.K.; Pharel, M.; Adepoju, J.O.; Vahedifard, F.; Adler, S.; Kocak, M.; Liu, X.; Byrd, S.E. Utility of Biometric Measurements from Fetal Magnetic Resonance Imaging for Improved Antenatal Diagnosis of Dandy–Walker Spectrum Posterior Fossa Lesions. Diagnostics 2025, 15, 1295. https://doi.org/10.3390/diagnostics15101295
Bowker RM, Marathu KK, Pharel M, Adepoju JO, Vahedifard F, Adler S, Kocak M, Liu X, Byrd SE. Utility of Biometric Measurements from Fetal Magnetic Resonance Imaging for Improved Antenatal Diagnosis of Dandy–Walker Spectrum Posterior Fossa Lesions. Diagnostics. 2025; 15(10):1295. https://doi.org/10.3390/diagnostics15101295
Chicago/Turabian StyleBowker, Rakhee M., Kranthi K. Marathu, Marissa Pharel, Jubril O. Adepoju, Farzan Vahedifard, Seth Adler, Mehmet Kocak, Xuchu Liu, and Sharon E. Byrd. 2025. "Utility of Biometric Measurements from Fetal Magnetic Resonance Imaging for Improved Antenatal Diagnosis of Dandy–Walker Spectrum Posterior Fossa Lesions" Diagnostics 15, no. 10: 1295. https://doi.org/10.3390/diagnostics15101295
APA StyleBowker, R. M., Marathu, K. K., Pharel, M., Adepoju, J. O., Vahedifard, F., Adler, S., Kocak, M., Liu, X., & Byrd, S. E. (2025). Utility of Biometric Measurements from Fetal Magnetic Resonance Imaging for Improved Antenatal Diagnosis of Dandy–Walker Spectrum Posterior Fossa Lesions. Diagnostics, 15(10), 1295. https://doi.org/10.3390/diagnostics15101295






