Diagnostic Value of Multimodal Lymphatic Imaging Techniques in Thoracic Duct Outlet Obstruction
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Non-Enhanced Magnetic Resonance Lymphangiography
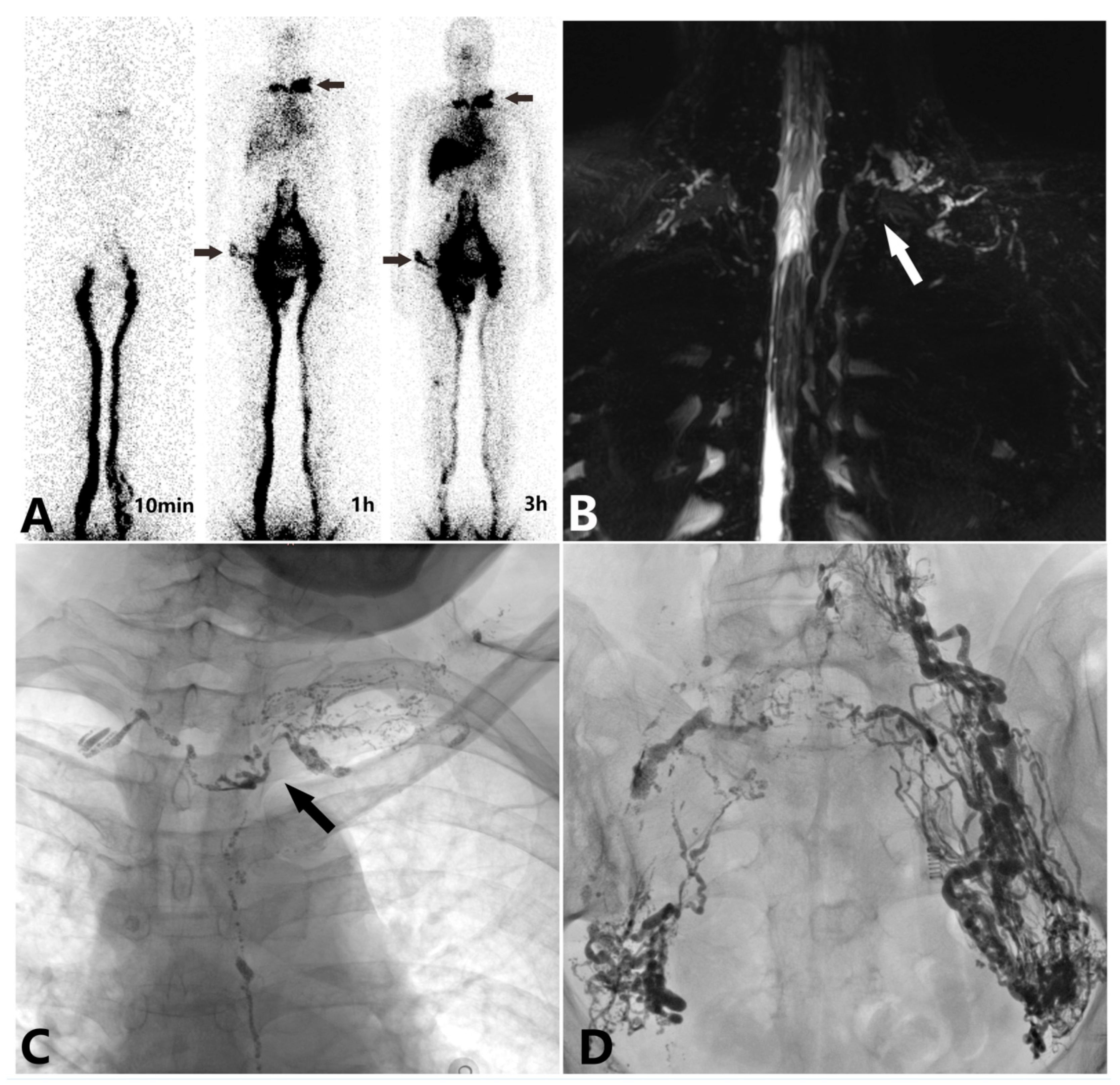
2.3. 99Tcm-DX Lymphoscintigraphy
2.4. Intranodal Lymphangiography
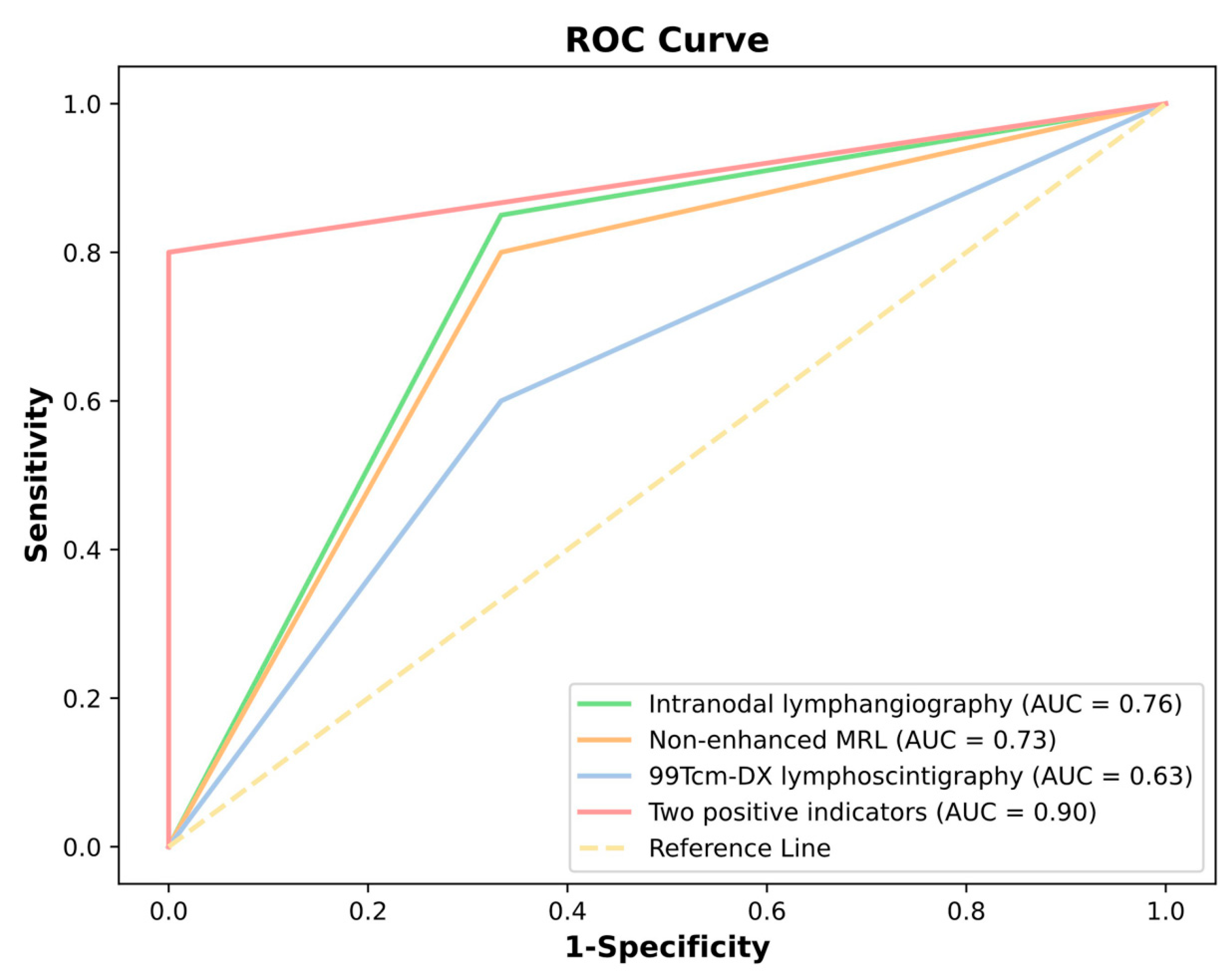
2.5. Statistical Analysis
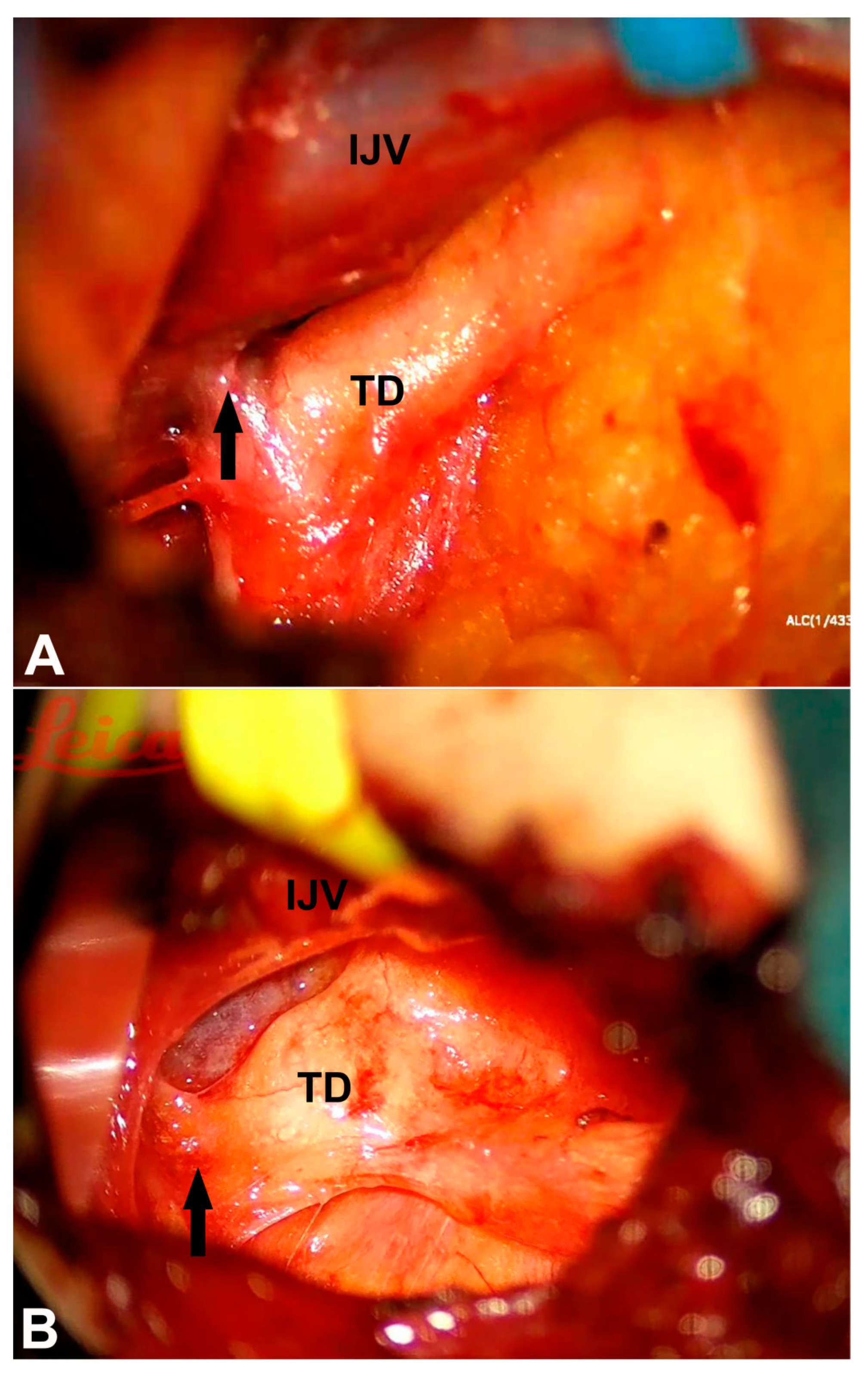
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Benjamin, J.; O’leary, C.; Hur, S.; Gurevich, A.; Klein, W.M.; Itkin, M. Imaging and Interventions for Lymphatic and Lymphatic-related Disorders. Radiology 2023, 307, e220231. [Google Scholar] [CrossRef] [PubMed]
- Bhatnagar, M.; Fisher, A.; Ramsaroop, S.; Carter, A.; Pippard, B. Chylothorax: Pathophysiology, diagnosis, and management—A comprehensive review. J. Thorac. Dis. 2024, 16, 1645–1661. [Google Scholar] [CrossRef]
- Oliver, G.; Kipnis, J.; Randolph, G.J.; Harvey, N.L. The lymphatic vasculature in the 21st century: Novel functional roles in homeostasis and disease. Cell 2020, 182, 270–296. [Google Scholar] [CrossRef]
- de Beer, H.G.; Mol, M.J.; Janssen, J.P. Chylothorax. Neth. J. Med. 2000, 56, 25–31. [Google Scholar] [CrossRef] [PubMed]
- Nadolski, G.J.; Itkin, M. Feasibility of ultrasound-guided intranodal lymphangiogram for thoracic duct embolization. J. Vasc. Interv. Radiol. 2012, 23, 613–616. [Google Scholar] [CrossRef]
- Kim, P.H.; Tsauo, J.; Shin, J.H. Lymphatic Interventions for Chylothorax: A Systematic Review and Meta-Analysis. J. Vasc. Interv. Radiol. 2018, 29, 194–202.e4. [Google Scholar] [CrossRef] [PubMed]
- Hur, S.; Shin, J.H.; Lee, I.J.; Min, S.-K.; Min, S.-I.; Ahn, S.; Kim, J.; Kim, S.Y.; Kim, M.; Lee, M.; et al. Early Experience in the Management of Postoperative Lymphatic Leakage Using Lipiodol Lymphangiography and Adjunctive Glue Embolization. J. Vasc. Interv. Radiol. 2016, 27, 1177–1186.e1. [Google Scholar] [CrossRef]
- An, R.; Xia, S.; Sun, Y.; Chang, K.; Li, Y.; Shen, W. New application of direct lymphangiography in the diagnosis and treatment of chylothorax after lung cancer surgery: A case series. Ann. Palliat. Med. 2021, 10, 4768–4776. [Google Scholar] [CrossRef]
- Kariya, S.; Nakatani, M.; Ono, Y.; Maruyama, T.; Ueno, Y.; Komemushi, A.; Tanigawa, N. Percutaneous Balloon Plasty for Thoracic Duct Occlusion in a Patient with Chylothorax and Chylous Ascites. Cardiovasc. Interv. Radiol. 2019, 42, 779–783. [Google Scholar] [CrossRef]
- Liu, X.; Liu, Z.; Shen, W.; Xia, S.; Sun, Y.; Chang, K.; Xin, J.; An, R.; Liang, C.; Zhou, C. Diagnostic imaging, therapeutic interventions and suggestions for thoracic duct congestion in postoperative hepatic lymphorrhea: A retrospective analysis of 20 cases. BMC Surg. 2024, 24, 352. [Google Scholar] [CrossRef]
- Othman, S.; Azoury, S.C.; Klifto, K.D.; Toyoda, Y.; Itkin, M.M.; Kovach, S.J. Microsurgical thoracic duct lymphovenous bypass in the adult population. Plast. Reconstr. Surg. Glob. Open 2021, 9, e3875. [Google Scholar] [CrossRef] [PubMed]
- Othman, S.; Azoury, S.C.; DiBardino, D.; Adams, D.M.; Itkin, M.; Kovach, S.J. Respiratory failure in Noonan syndrome treated by microsurgical thoracic duct-venous anastomosis. Ann. Thorac. Surg. 2022, 113, e219–e221. [Google Scholar] [CrossRef]
- Pan, F.; Loos, M.; Do, T.D.; Richter, G.M.; Kauczor, H.U.; Hackert, T.; Sommer, C.M. The roles of iodized oil-based lymphangiography and post-lymphangiographic computed tomography for specific lymphatic intervention planning in patients with postoperative lymphatic fistula: A literature review and case series. CVIR Endovasc. 2020, 3, 79. [Google Scholar] [CrossRef] [PubMed]
- Matsumoto, T.; Yamagami, T.; Kato, T.; Hirota, T.; Yoshimatsu, R.; Masunami, T.; Nishimura, T. The effectiveness of lymphangiography as a treatment method for various chyle leakages. Br. J. Radiol. 2009, 82, 286–290. [Google Scholar] [CrossRef]
- Zhang, Y.; Wen, Z.; Liu, M.; Li, X.; Zhang, M.; Wang, R. Diagnostic value of combined CT lymphangiography and 99Tcm-DX lymphoscintigraphy in primary chylopericardium. BMC Med. Imaging 2024, 24, 223. [Google Scholar] [CrossRef]
- Cholet, C.; Delalandre, C.; Monnier-Cholley, L.; Le Pimpec-Barthes, F.; El Mouhadi, S.; Arrivé, L. Nontraumatic Chylothorax: Nonenhanced MR Lymphography. RadioGraphics 2020, 40, 1554–1573. [Google Scholar] [CrossRef] [PubMed]
- Biko, D.M.; DeWitt, A.G.; Pinto, E.M.; Morrison, R.E.; Johnstone, J.A.; Griffis, H.; O’byrne, M.L.; Fogel, M.A.; Harris, M.A.; Partington, S.L.; et al. MRI Evaluation of Lymphatic Abnormalities in the Neck and Thorax after Fontan Surgery: Relationship with Outcome. Radiology 2019, 291, 774–780. [Google Scholar] [CrossRef]
- Zhang, Y.; Zhang, Y.; Sun, X.; Sun, X.; Liu, M.; Liu, M.; Li, X.; Li, X.; Zhang, M.; Zhang, M.; et al. Association between lymphatic abnormalities in the neck and thorax in primary chylopericardium and surgical outcomes evaluated by non-enhanced magnetic resonance (MR) lymphangiography. Quant. Imaging Med. Surg. 2024, 14, 5961–5972. [Google Scholar] [CrossRef]
- Kiyonaga, M.; Mori, H.; Matsumoto, S.; Yamada, Y.; Sai, M.; Okada, F. Thoracic duct and cisterna chyli: Evaluation with multidetector row CT. Br. J. Radiol. 2012, 85, 1052–1058. [Google Scholar] [CrossRef]
- Majdalany, B.S.; Murrey, D.A.; Kapoor, B.S.; Cain, T.R.; Ganguli, S.; Kent, M.S.; Maldonado, F.; McBride, J.J.; Minocha, J.; Reis, S.P.; et al. Expert Panel on Vascular Imaging and Interventional Radiology. ACR Appropriateness Criteria® Chylothorax Treatment Planning. J. Am. Coll. Radiol. 2017, 14, S118–S126. [Google Scholar] [CrossRef]
- Gray, M.; Kovatis, K.Z.; Stuart, T.; Enlow, E.; Itkin, M.; Keller, M.S.; French, H.M. Treatment of congenital pulmonary lymphangiectasia using ethiodized oil lymphangiography. J. Perinatol. 2014, 34, 720–722. [Google Scholar] [CrossRef] [PubMed]
- Kirschen, M.P.; Dori, Y.; Itkin, M.; Licht, D.J.; Ichord, R.; Vossough, A. Cerebral Lipiodol Embolism after Lymphatic Embolization for Plastic Bronchitis. J. Pediatr. 2016, 176, 200–203. [Google Scholar] [CrossRef] [PubMed]
- Hubrechts, J.; Wåhlander, H.; Kjellberg-Olofsson, C.; Maleux, G.; Gewillig, M. Case Report: Disseminated Systemic Embolism of Lipiodol After Lymphography for Plastic Bronchitis After Fontan Repair. Front. Pediatr. 2020, 8, 584185. [Google Scholar] [CrossRef] [PubMed]
- Dori, Y.; Keller, M.S.; Fogel, M.A.; Rome, J.J.; Whitehead, K.K.; Harris, M.A.; Itkin, M. MRI of lymphatic abnormalities after functional single-ventricle palliation surgery. AJR Am. J. Roentgenol. 2014, 203, 426–431. [Google Scholar] [CrossRef]
- Dori, Y.; Zviman, M.M.; Itkin, M. Dynamic contrast-enhanced MR lymphangiography: Feasibility study in swine. Radiology 2014, 273, 410–416. [Google Scholar] [CrossRef]
| Characteristics | Patient Numbers |
|---|---|
| Sex (M/F) | 15/8 |
| Age (Year) | 59.78 ± 13.08 |
| The etiology of chylous leakage | |
| Non-iatrogenic traumatic factor | 1 |
| Iatrogenic factors (post radical resection of malignant tumors) | 7 |
| Iatrogenic factors (postoperative complications of benign thoracic/abdominal diseases) | 2 |
| Spontaneous chylous leakage | 13 |
| Chylous leakage type | |
| Chylothorax | 7 |
| Chylous ascites | 4 |
| Chylopericardium | 2 |
| Chylothorax and chylous ascites | 2 |
| Lower limb or perineal chylous leak | 8 |
| The imaging technique indicates TD outlet obstruction | |
| 99Tcm-DX lymphoscintigraphy | 13 |
| Non-enhanced magnetic resonance lymphangiography | 17 |
| Intranodal lymphangiography | 18 |
| Characteristics | Patient Numbers |
|---|---|
| The imaging technique indicates TD outlet obstruction | |
| 99Tcm-DX lymphoscintigraphy | 13 |
| Non-enhanced magnetic resonance lymphangiography | 17 |
| Intranodal lymphangiography | 18 |
| 99Tcm-DX lymphoscintigraphy | |
| Type I | 8 |
| Type II | 5 |
| Type III | 10 |
| Non-enhanced magnetic resonance lymphangiography | |
| Type I | 5 |
| Type II | 8 |
| Type III | 1 |
| Type IV | 3 |
| Intranodal lymphangiography | |
| Reasons for imaging failure | Peripheral entry of lipiodol into the bloodstream (3) Cystic dilatation of the lymphatic vessels (2) |
| TD dilatation | 16 |
| Branch reflux | 18 |
| Difficulty in lipiodol penetration into bloodstream | 18 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fei, Y.; Lu, Y.; Yao, Z.; Yin, K.; Zhou, D.; Liu, Z. Diagnostic Value of Multimodal Lymphatic Imaging Techniques in Thoracic Duct Outlet Obstruction. Diagnostics 2025, 15, 1288. https://doi.org/10.3390/diagnostics15101288
Fei Y, Lu Y, Yao Z, Yin K, Zhou D, Liu Z. Diagnostic Value of Multimodal Lymphatic Imaging Techniques in Thoracic Duct Outlet Obstruction. Diagnostics. 2025; 15(10):1288. https://doi.org/10.3390/diagnostics15101288
Chicago/Turabian StyleFei, Ying, Yanli Lu, Zhichao Yao, Kongxiang Yin, Dayong Zhou, and Zhanao Liu. 2025. "Diagnostic Value of Multimodal Lymphatic Imaging Techniques in Thoracic Duct Outlet Obstruction" Diagnostics 15, no. 10: 1288. https://doi.org/10.3390/diagnostics15101288
APA StyleFei, Y., Lu, Y., Yao, Z., Yin, K., Zhou, D., & Liu, Z. (2025). Diagnostic Value of Multimodal Lymphatic Imaging Techniques in Thoracic Duct Outlet Obstruction. Diagnostics, 15(10), 1288. https://doi.org/10.3390/diagnostics15101288





