1. Introduction
Over the past few decades, the goals of patients seeking orthodontic treatment have continuously evolved. In the 1980s and 1990s, patients primarily aimed to resolve malocclusion or restore normal occlusal function through orthodontic treatment. However, recent patients place a significant emphasis not only on functional occlusal recovery but also on aesthetic improvement [
1,
2,
3].
Orthodontic treatment can induce unwanted side effects on periodontal tissues, such as root resorption, bone dehiscence, gingival recession, and the formation of black triangles, which may reduce patient satisfaction with the treatment [
2,
4,
5]. A black triangle is an empty space beneath the contact area between teeth due to the loss of the interdental papilla [
6]. This issue not only affects aesthetics but can also lead to periodontal problems by chronically trapping food debris and making plaque control more difficult. Therefore, a thorough understanding of the etiology and pathogenesis of black triangles, as well as appropriate orthodontic diagnosis and treatment, is required [
7].
Previous studies have identified various factors contributing to the development of black triangles, including patient age, history of periodontitis, the distance between the interproximal contact and the alveolar crest, gingival biotype, and morphological characteristics of teeth [
8]. However, there is still a lack of consensus regarding the relationship between orthodontic treatment and black triangles. Some studies have reported a high incidence of black triangles in patients who have undergone orthodontic treatment [
9,
10,
11,
12,
13,
14,
15,
16], while others have suggested that orthodontic treatment can stimulate the formation of interdental papillae, thus reducing the incidence of black triangles [
17,
18,
19]. Consequently, a definitive conclusion about the relationship between orthodontic treatment and black triangles has yet to be reached. In addition, it should be distinguished from the case where black triangles occur when orthodontic treatment is performed on normal periodontal tissue with reduced periodontal support.
Risk factors associated with black triangle formation after orthodontic treatment include age, treatment duration, tooth shape, the amount of tooth movement, root angulation after treatment, the degree of crowding, the distance between the alveolar crest and the interproximal contact after treatment, traumatic brushing, the occurrence of periodontitis, and gingival biotype [
20,
21,
22,
23,
24,
25,
26]. However, most previous studies have evaluated the impact of risk factors on black triangle formation in a unidimensional manner, which limits the understanding of how these factors might interact during orthodontic treatment. Therefore, comprehensive investigation of associations among various risk factors is necessary.
The purpose of this study was to examine the association between the occurrence of black triangles during orthodontic treatment and factors such as age, gender, bracket type, and extraction status. The null hypothesis of this study is that there is no correlation between the occurrence of black triangles during orthodontic treatment and factors such as age, gender, bracket type, and extraction status.
2. Materials and Methods
2.1. Subjects
Patients who completed orthodontic treatment at the Department of Orthodontics, Korea University Guro Hospital were selected for this study. Among them, patients without a black triangle between the maxillary and mandibular central incisors, as assessed by a Jemt Index score of 3 from intraoral photographs taken before orthodontic treatment, were included. Patients with periodontitis, anterior tooth loss, a history of previous orthodontic treatment, prosthetic restorations of the maxillary or mandibular central incisors, or those who underwent interproximal reduction (stripping) during orthodontic treatment were excluded from the study. A total of 300 patients who underwent orthodontic treatment between January 2020 and March 2022 were evaluated, and after applying the exclusion criteria, 97 patients (58 adults and 39 adolescents, 47 extraction and 50 non-extraction) who had pre- and post-treatment intraoral photographs, lateral cephalograms, periapical radiographs, and study models were selected for this retrospective study.
For age classification, adolescents were defined as patients aged 9 to under 20 years, and adults were defined as those aged 20 to under 55 years based on pre-treatment age. The extraction group consisted of patients who underwent the extraction of the first premolars in both the maxilla and mandible. The orthodontic appliances used for treatment were the 0.022-inch slot metal ligating brackets (Formula-R, Tomy Inc, Fukushima, Japan), self-ligating brackets (Clippy-C, Tomy Inc, Fukushima, Japan), and lingual brackets (Fujita, Succeeding Co, Morioka, Japan).
2.2. Measurement Methods
2.2.1. Classification of Black Triangles According to Severity
Intraoral frontal photographs of the maxillary and mandibular central incisors were taken within one week after the completion of orthodontic treatment. Intraoral photographs were taken from the front using standardized camera settings (shutter speed 1/125, ISO 200, F22) after drying the area with air. A parallel line was drawn from the gingival zenith (the most cervical point of the crown) and the most cervical point of the interproximal contact area, followed by a bisecting line through the midpoint of these two parallel lines, dividing the interdental papilla area into four sections. Based on the Jemt Index, patients were classified into two groups: the non-occurrence group (Score 3, the papilla fills up the entire proximal space) and the occurrence group, which was further subdivided into Score 2 (mild, half or more of the height of the papilla is present), Score 1 (moderate, less than half of the height of the papilla is present), and Score 0 (severe, no papilla is present) (
Figure 1).
2.2.2. Measurements of Tooth Movement on Lateral Cephalograms
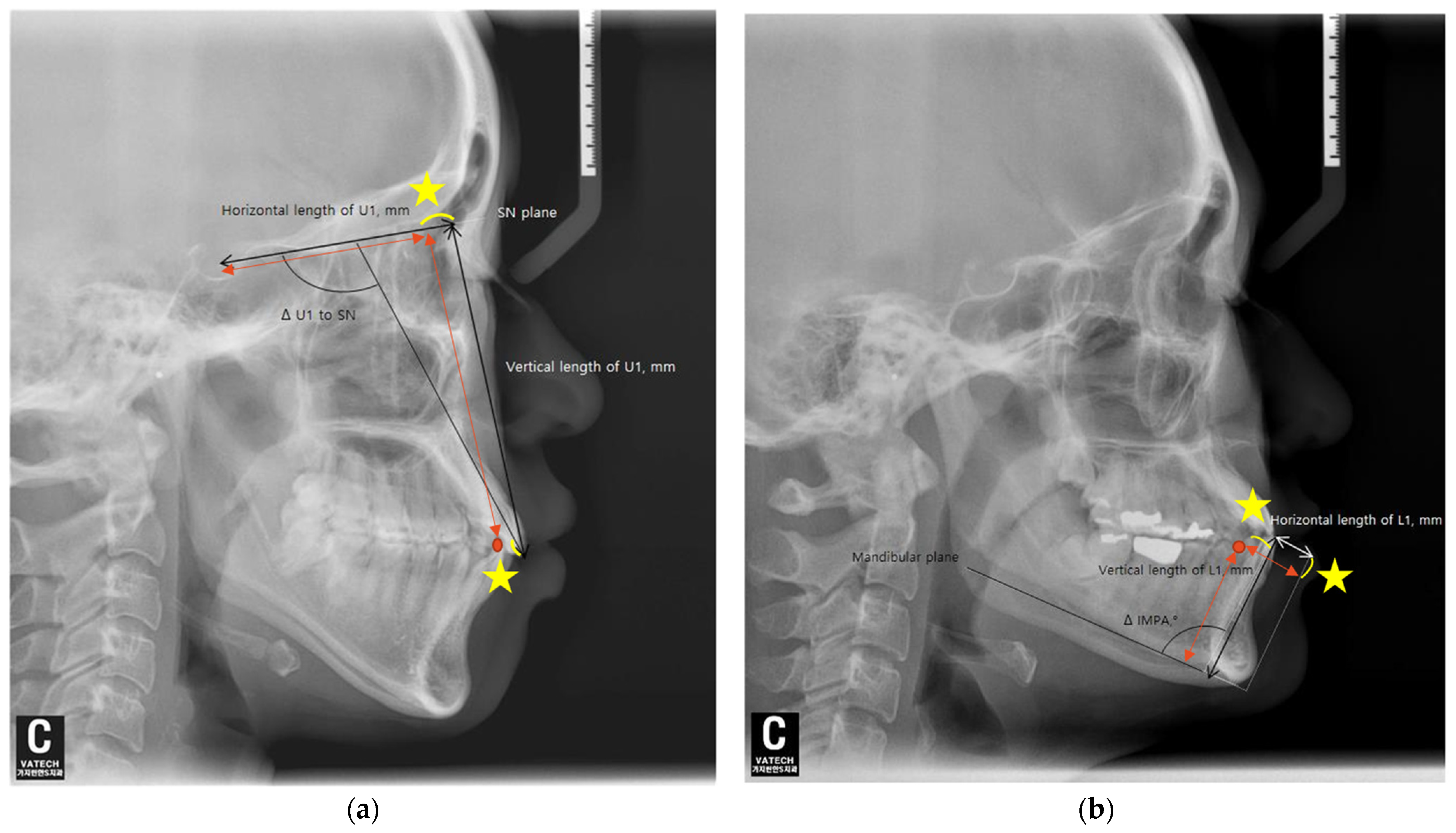
The angular and anteroposterior, as well as vertical, changes in the maxillary and mandibular central incisors before and after orthodontic treatment were measured using lateral cephalometric radiographs. Each radiograph was taken in a natural head position. Additionally, all subjects were instructed to stand still, hold their breath, swallow briefly before imaging, and refrain from swallowing while the radiographs were being taken. For the maxillary central incisors, the angular change was assessed by measuring the difference in the angle between the upper incisor and the SN plane (ΔU1 to SN), and for the mandibular central incisors, the difference in the incisor mandibular plane angle (ΔIMPA) was measured relative to the mandibular plane before and after orthodontic treatment.
The horizontal movement of the maxillary central incisors was measured as calculating the change in the distance between the perpendicular line drawn from the tip of the maxillary central incisor crown to the SN plane and the distance from this point to the Sella (S) (ΔTH = TH2 − TH1). The vertical movement of the maxillary central incisors was calculated by measuring the change in the perpendicular distance from the tip of the maxillary central incisor crown to the SN plane (ΔTV = TV2 − TV1) (
Figure 2a).
For the mandibular central incisors, the horizontal movement was assessed by measuring the change in the straight-line distance between the tip of the mandibular central incisor crown and the perpendicular line drawn from the mandibular plane to the Pogonion (ΔTH = TH2 − TH1). The vertical movement was calculated by measuring the change in the perpendicular distance from the tip of the mandibular central incisor crown to the mandibular plane (ΔTV = TV2 − TV1) (
Figure 2b).
2.2.3. The Tooth Shape and the Height of Alveolar Bone
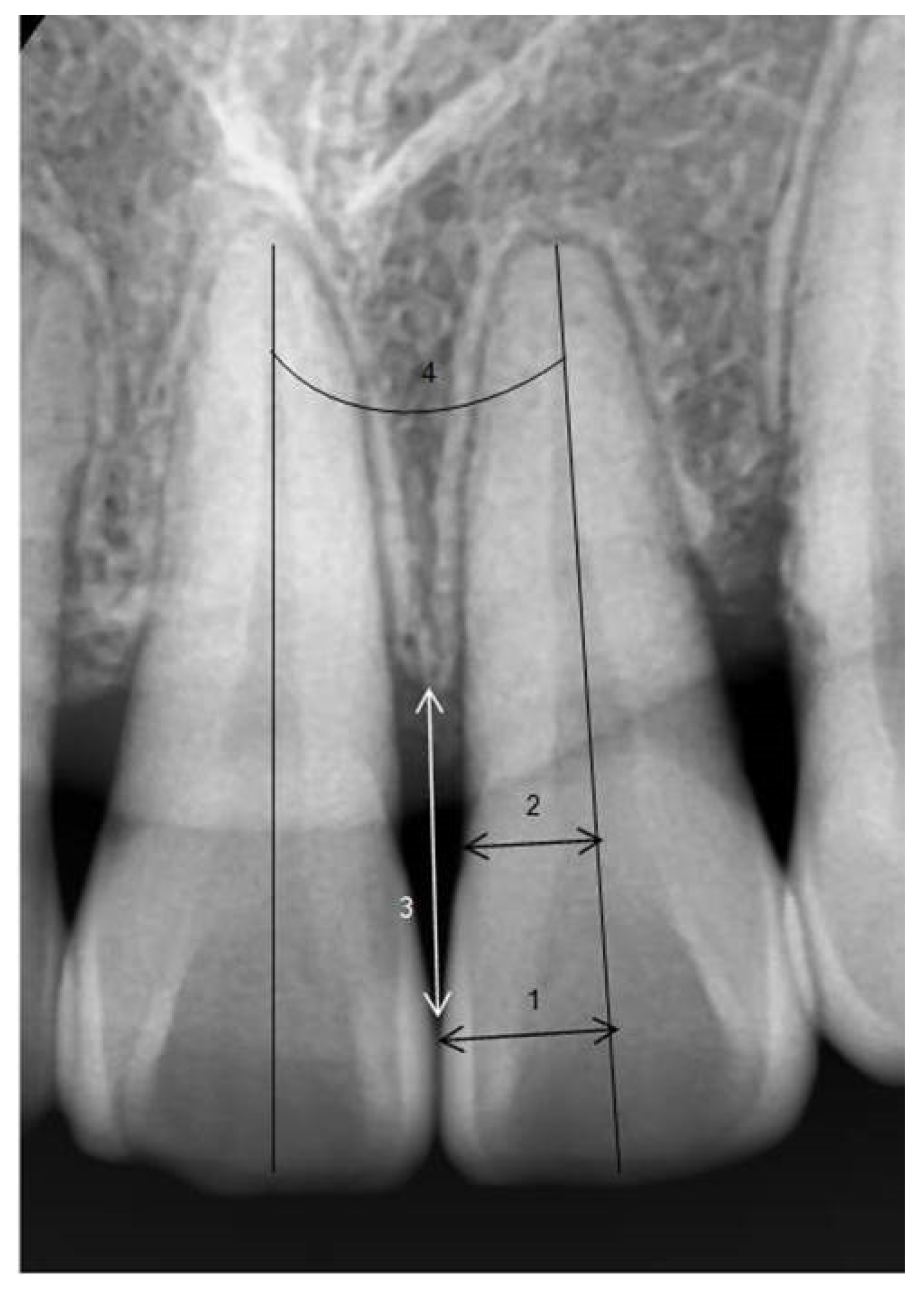
In periapical radiographs taken before orthodontic treatment, the long axis of the maxillary and mandibular central incisors was established. The ratio of the perpendicular distance from the long axis to the mesial contact point of the crown (1) to the perpendicular distance from the long axis to the mesial CEJ (cemento–enamel junction) (2) was calculated (crown ratio = (1)/(2)) [
27].
To minimize errors due to magnification or distortion in periapical radiographs, the clinical average crown lengths of the central incisors were used as reference values, and the amount of alveolar bone height change (ΔTA = TA2 − TA1) was measured [
28]. The distance from the contact point (or the most cervical point of the contact surface) of the maxillary and mandibular central incisors to the alveolar crest was measured, keeping the measurement parallel to the long axis of the left central incisor, and the difference in distance before and after orthodontic treatment was compared. If there was a space between the teeth without a contact point, the distance from the narrowest point between the mesial surfaces of both crowns and the alveolar crest was measured. The angle between the roots of the left and right maxillary and mandibular central incisors was measured in patients after completing orthodontic treatment (
Figure 3).
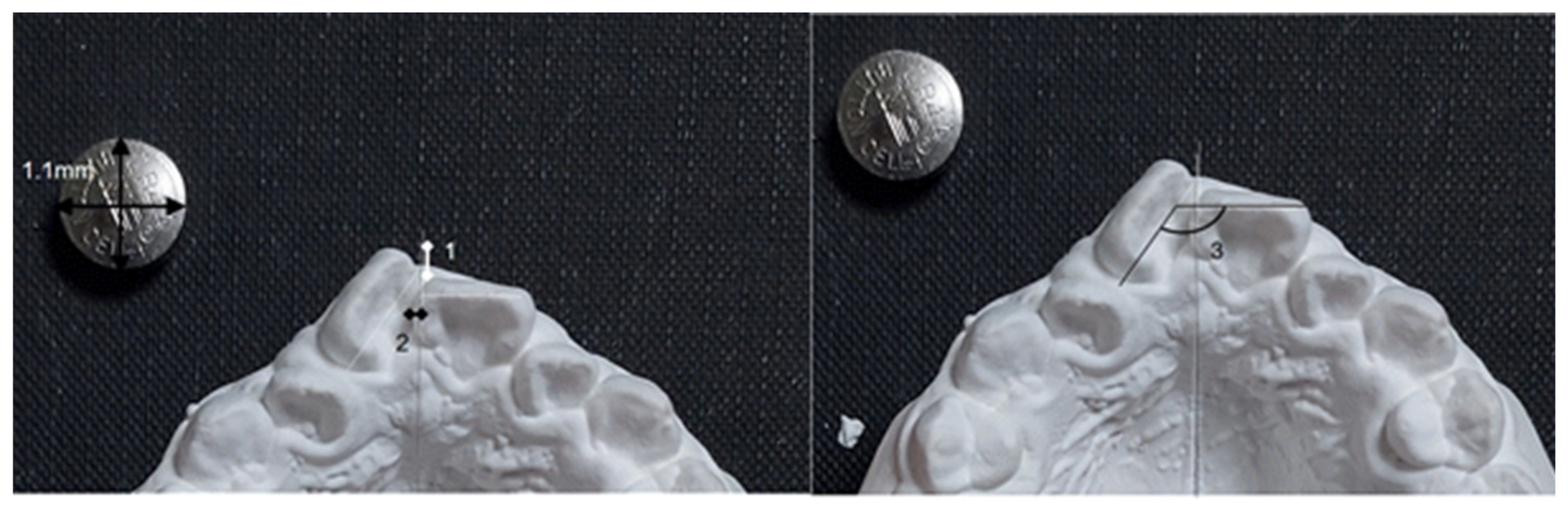
2.2.4. Measurements of Crowding on Study Models
In pre-treatment study model photographs, the anteroposterior and mesiodistal crowding of the maxillary and mandibular central incisors was measured. The plane connecting the central incisors and the first molars was set as the occlusal plane, and the photographs were taken perpendicular to this occlusal plane. The midpalatal raphe in the maxilla and a perpendicular line bisecting the line connecting the mesial surfaces of the first molars in the mandible were used as the reference lines. Anteroposterior overlap was measured by the length of the line connecting the most mesial points of the left and right central incisors, drawn parallel to the reference line. Mesiodistal overlap was measured by the length of the perpendicular line drawn from the most mesial points of the left and right central incisors to the reference line. The angle change between the crowns of the left and right central incisors (ΔTR = TR2 − TR1) was measured using occlusal surface photographs of the study models before and after orthodontic treatment. (
Figure 4).
2.3. Statistical Analysis
Statistical analysis was performed using PASW Statistics version 18.0.0 (SPSS Inc., Chicago, IL, USA). The target sample size was determined based on a review of existing literature and calculations using the G Power program version 3.1.9.7. To confirm the association between the incidence rates and contributing factors in the two groups, the statistically significant minimum sample size was calculated to be 40 participants per group based on age, requiring a total of at least 80 participants. All measurements were conducted by a single examiner, who randomly selected and reanalyzed 25 patients at one-week intervals. The degree of black triangle occurrence after orthodontic treatment was assessed, and the association between black triangle occurrence and variables such as age, gender, bracket type, and extraction versus non-extraction groups was examined using the Chi-square test and Fisher’s exact test.
For the occurrence and non-occurrence groups of black triangles, mean values and standard deviations were analyzed and compared using the independent t-test for variables such as treatment duration, age, tooth shape, pre- and post-treatment angle differences of the maxillary and mandibular incisors, horizontal and vertical movement changes of the maxillary and mandibular incisors, pre- and post-treatment differences in alveolar bone height, post-treatment angle between the roots of the left and right central incisors, anteroposterior and mesiodistal crowding of the maxillary and mandibular central incisors before treatment, and crown rotation changes before and after treatment.
Additionally, the independent t-test was performed to compare mean values for age (pediatric/adolescent versus adult) and extraction status (extraction versus non-extraction), which were identified as risk factors associated with black triangle occurrence in the Chi-square test. Simple logistic regression analysis was conducted to assess the association between risk factors and the occurrence of black triangles in the maxillary and mandibular central incisors during orthodontic treatment, followed by multiple logistic regression analysis to further analyze the combined risk factors and calculate the odds ratios. Statistical significance was set at a p-value of less than 0.05.
4. Discussion
In this study, the incidence of black triangles after orthodontic treatment was found to be between 51% and 64%. This is higher than the previously reported rates of 38% to 58%, which can be attributed to differences in study design, sample size, age distribution, and methods for assessing black triangles [
7,
9,
29]. The study confirmed a significant association between the occurrence of black triangles during orthodontic treatment and factors such as age and extraction status. Previous studies that highlighted the advantages of non-extraction treatment have reported that post-extraction orthodontic treatment leads to a significant reduction in the width of keratinized gingiva in the anterior region compared to non-extraction patients [
2]. This suggests that extraction treatment may have a negative impact on periodontal tissues. However, as with other studies analyzing the effects of bracket type and bonding location on microbial distribution and periodontal health [
30,
31,
32], this study found no significant association between the type of brackets or their bonding location and the occurrence of black triangles.
When comparing the mean values of various risk factors between patients with and without black triangles, the study found significant differences in the maxilla regarding treatment duration, age, and pre- and post-treatment incisor angulation changes. In the mandible, only age showed a significant difference. Previous studies have reported a significant increase in periodontal disease risk, such as inflammatory gingival hyperplasia, with longer orthodontic treatment durations due to increased plaque accumulation on appliances like brackets and power chains, as well as poor oral hygiene habits [
33,
34]. However, Ko-Kimura et al. [
22] reported no significant statistical correlation between the duration of orthodontic treatment and the occurrence of black triangles. In this study, the occurrence of black triangles in the maxillary anterior region was significantly higher in patients with longer treatment durations than those without black triangles.
The direction of tooth movement has also been identified in previous studies as a risk factor for the formation of black triangles during orthodontic treatment. Specifically, numerous studies have reported that labial horizontal or labial angular movements of the maxillary anterior teeth increase the likelihood of gingival recession or black triangle formation due to thin labial alveolar bone [
35,
36]. In this study, of the 97 patients, only 27 exhibited labial angular movement during orthodontic treatment, and only 8 of these patients developed mild black triangles, scoring 2 on the Jemt Index. The remaining 19 patients did not develop black triangles. Therefore, no significant association was found between labial angular movement and black triangle formation, contrary to previous studies. However, the results of the multiple regression analysis showed that the likelihood of black triangle formation increased as the maxillary incisors underwent lingual angulation relative to the SN plane. The odds ratio for changes in maxillary incisor angulation was 0.940, indicating that for each degree of lingual angulation, the risk of black triangle formation increased by a factor of 1.06. This finding aligns with An et al. [
7], who reported a significant association between black triangle formation and lingual horizontal movement of the maxillary incisors during orthodontic treatment.
The multiple regression analysis also revealed a significant association between age and the occurrence of black triangles during orthodontic treatment in both the maxilla and mandible. The odds ratios were 1.087 for the maxilla and 1.197 for the mandible, indicating that for each year of age, the risk of black triangle formation increased by 1.087 times in the maxilla and 1.197 times in the mandible. While age is commonly associated with an increased risk of periodontal disease, the occurrence of black triangles in older patients is not solely due to poor oral hygiene over time. As aging progresses, the reduction in oral epithelial keratinization, decreased interdental papilla height, and increased interdental space contribute to gingival recession and a higher likelihood of black triangles in adults [
22,
24]. These effects are particularly pronounced in adults over the age of 20 who undergo orthodontic treatment, as the ability of the papilla to regenerate and fill interdental spaces appears to diminish with age, exacerbating the condition during orthodontic interventions.
Tarnow et al. [
21] reported a correlation between the distance from the contact point to the alveolar crest and the occurrence of black triangles. When the distance exceeds 5 mm, the interdental papilla cannot fill the black triangle, but when the distance is less than 5 mm, the papilla can re-fill the space. This study measured only the relative distance changes between the contact point and the alveolar crest before and after orthodontic treatment, and no significant association with black triangle formation was found. However, it was observed that alveolar bone height generally decreased in patients, regardless of whether black triangles developed. This suggests that age-related changes, typically associated with aging, were evident during the course of orthodontic treatment.
Future studies should classify patients according to the type and severity of malocclusion and their ability to maintain oral hygiene to investigate black triangle occurrence rates. Additionally, selecting a control group of patients who did not undergo orthodontic treatment for comparative analysis would be beneficial. The relationship between black triangle formation and gingival biotype should also be examined, as gingival phenotype plays a crucial role in determining susceptibility to black triangles. Thin gingival phenotypes are particularly prone to gingival recession and papilla loss, which can exacerbate black triangle formation. Evaluating these factors in future studies could enhance clinical decision-making. Furthermore, while this study did not directly compare fixed and removable appliances, future investigations should explore their respective impacts on black triangle formation to develop clearer guidelines for appliance selection. The risk factors associated with black triangles after orthodontic treatment are diverse. Being aware of these factors and predicting potential risks during diagnosis and treatment planning can help prevent or minimize the occurrence of black triangles.
Once black triangles form, various approaches can be considered for correction depending on the severity and underlying cause. Orthodontic techniques, such as controlled tipping or closing interdental spaces, can help reduce black triangle visibility, while interproximal stripping can minimize interdental spacing by reducing tooth size. Restorative approaches, including composite resins or veneers, may also be employed to address aesthetic concerns. Interdisciplinary collaboration between orthodontics, periodontics, and prosthodontics is necessary to reduce or eliminate black triangles that develop after orthodontic treatment.