Computed Tomography and Magnetic Resonance Enterography: From Protocols to Diagnosis
Abstract
1. Introduction
2. CTE or MRE?
3. Patient Preparation
3.1. Intraluminal Contrast Agents
3.2. Antiperistalsis Drugs
3.3. Patients’ Positioning
4. Technical Considerations
4.1. CTE
4.2. MRE
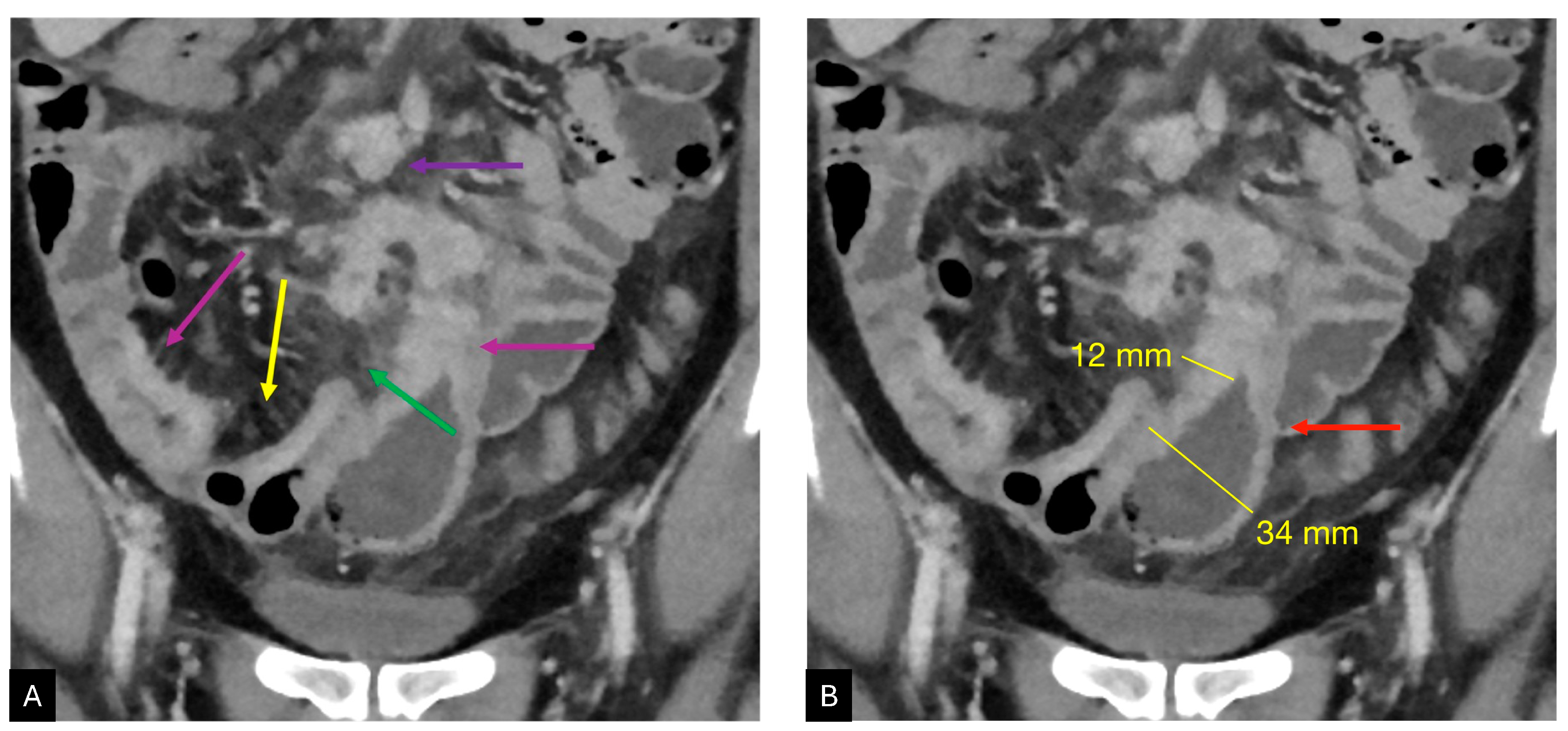
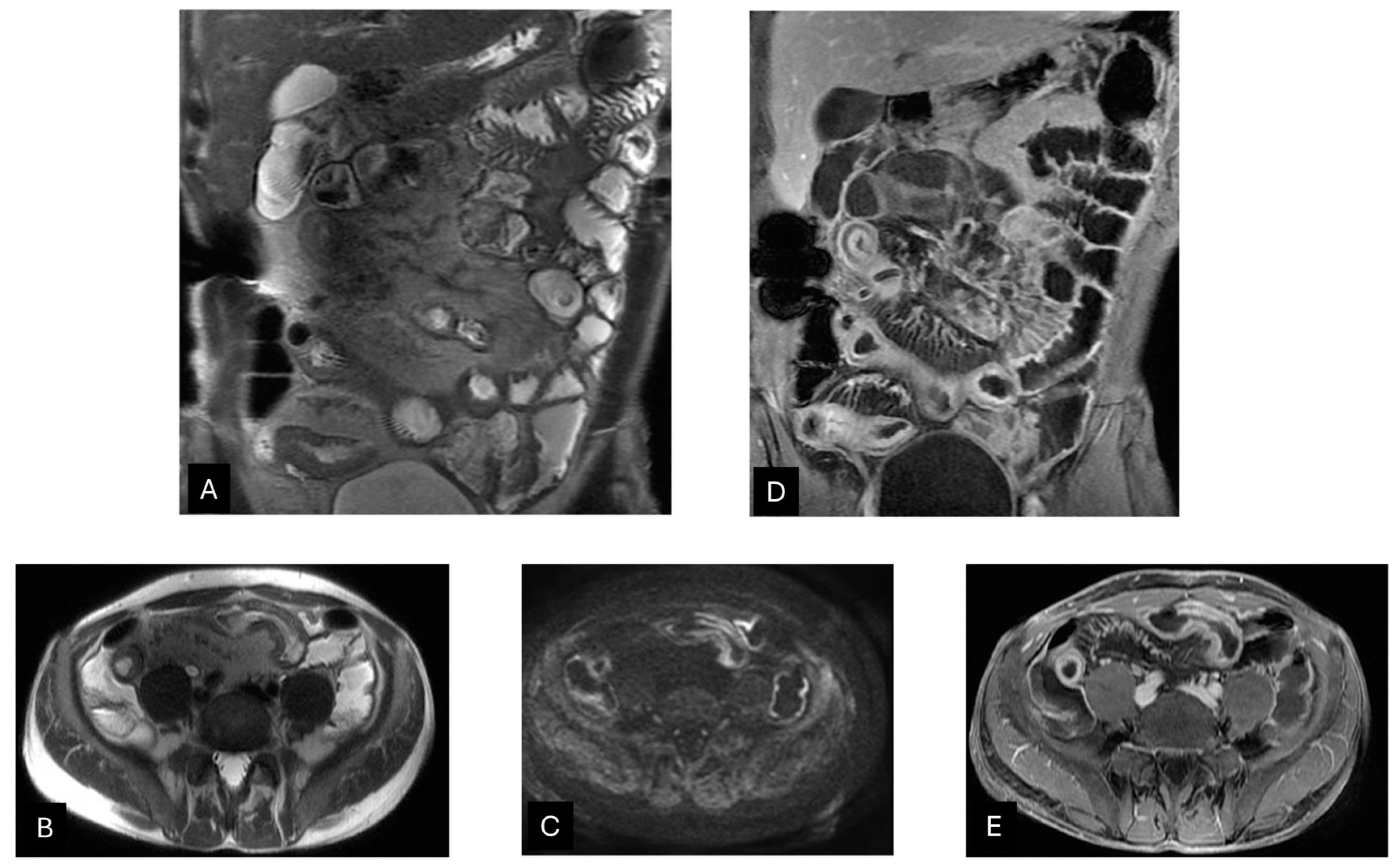
5. Imaging Features: What to Focus on
6. Disease Grading
7. Cross-Sectional Imaging Limitations
8. Conclusions
Author Contributions
Funding
Informed Consent Statement
Conflicts of Interest
References
- Gomollón, F.; Dignass, A.; Annese, V.; Tilg, H.; Van Assche, G.; Lindsay, J.O.; Peyrin-Biroulet, L.; Cullen, G.J.; Daperno, M.; Kucharzik, T.; et al. 3rd European Evidence-Based Consensus on the Diagnosis and Management of Crohn’s Disease 2016: Part 1: Diagnosis and Medical Management. J. Crohns Colitis 2017, 11, 3–25. [Google Scholar] [CrossRef] [PubMed]
- Grand, D.J.; Guglielmo, F.F.; Al-Hawary, M.M. MR Enterography in Crohn’s Disease: Current Consensus on Optimal Imaging Technique and Future Advances from the SAR Crohn’s Disease-Focused Panel. Abdom. Imaging 2015, 40, 953–964. [Google Scholar] [CrossRef] [PubMed]
- Gandhi, N.S.; Dillman, J.R.; Grand, D.J.; Huang, C.; Fletcher, J.G.; Al-Hawary, M.M.; Anupindi, S.A.; Baker, M.E.; Bruining, D.H.; Chatterji, M.; et al. Computed Tomography and Magnetic Resonance Enterography Protocols and Techniques: Survey of the Society of Abdominal Radiology Crohn’s Disease Disease-Focused Panel. Abdom. Radiol. 2020, 45, 1011–1017. [Google Scholar] [CrossRef] [PubMed]
- Bruining, D.H.; Zimmermann, E.M.; Loftus, E.V.; Sandborn, W.J.; Sauer, C.G.; Strong, S.A. Society of Abdominal Radiology Crohn’s Disease-Focused Panel Consensus Recommendations for Evaluation, Interpretation, and Utilization of Computed Tomography and Magnetic Resonance Enterography in Patients With Small Bowel Crohn’s Disease. Radiology 2018, 286, 776–799. [Google Scholar] [CrossRef] [PubMed]
- Lamb, C.A.; Kennedy, N.A.; Raine, T.; Hendy, P.A.; Smith, P.J.; Limdi, J.K.; Hayee, B.; Lomer, M.C.E.; Parkes, G.C.; Selinger, C.; et al. British Society of Gastroenterology Consensus Guidelines on the Management of Inflammatory Bowel Disease in Adults. Gut 2019, 68, s1–s106. [Google Scholar] [CrossRef]
- Panizza, P.S.B.; Viana, P.C.C.; Horvat, N.; Dos Santos, V.R.; de Araújo, D.A.P.; Yamanari, T.R.; Leite, C.d.C.; Cerri, G.G. Inflammatory Bowel Disease: Current Role of Imaging in Diagnosis and Detection of Complications: Gastrointestinal Imaging. Radiographics 2017, 37, 701–702. [Google Scholar] [CrossRef]
- Rees, M.A.; Dillman, J.R.; Anton, C.G.; Rattan, M.S.; Smith, E.A.; Towbin, A.J.; Zhang, B.; Trout, A.T. Inter-Radiologist Agreement Using Society of Abdominal Radiology-American Gastroenterological Association (SAR-AGA) Consensus Nomenclature for Reporting CT and MR Enterography in Children and Young Adults with Small Bowel Crohn Disease. Abdom. Radiol. 2019, 44, 391–397. [Google Scholar] [CrossRef]
- Taylor, S.A.; Rieder, F.; Fletcher, J.G. Differences in the Imaging of Crohn’s Disease Patients between North America and Europe: Are We Ready to Bridge the Divide? Abdom. Radiol. 2019, 44, 1637–1643. [Google Scholar] [CrossRef]
- Expert Panel on Gastrointestinal Imaging; Kim, D.H.; Chang, K.J.; Fowler, K.J.; Cash, B.D.; Garcia, E.M.; Kambadakone, A.R.; Levy, A.D.; Liu, P.S.; Mace, S.E.; et al. ACR Appropriateness Criteria® Crohn Disease. J. Am. Coll. Radiol. 2020, 17, S81–S99. [Google Scholar] [CrossRef]
- Barber, J.L.; Shah, N.; Watson, T.A. Early Onset Inflammatory Bowel Disease—What the Radiologist Needs to Know. Eur. J. Radiol. 2018, 106, 173–182. [Google Scholar] [CrossRef]
- Anupindi, S.A.; Terreblanche, O.; Courtier, J. Magnetic Resonance Enterography: Inflammatory Bowel Disease and Beyond. Magn. Reson. Imaging Clin. N. Am. 2013, 21, 731–750. [Google Scholar] [CrossRef] [PubMed]
- Judit Machnitz, A.; Reid, J.R.; Acord, M.R.; Khwaja, A.B.; Biko, D.M.; Ayyala, R.S.; Anupindi, S.A. MRI of the Bowel—beyond Inflammatory Bowel Disease. Pediatr. Radiol. 2018, 48, 1280–1290. [Google Scholar] [CrossRef] [PubMed]
- Romano, S.; Russo, A.; Daniele, S.; Tortora, G.; Maisto, F.; Romano, L. Acute Inflammatory Bowel Disease of the Small Intestine in Adult: MDCT Findings and Criteria for Differential Diagnosis. Eur. J. Radiol. 2009, 69, 381–387. [Google Scholar] [CrossRef]
- Qiu, Y.; Mao, R.; Chen, B.-L.; Li, X.-H.; He, Y.; Zeng, Z.-R.; Li, Z.-P.; Chen, M.-H. Systematic Review with Meta-Analysis: Magnetic Resonance Enterography vs. Computed Tomography Enterography for Evaluating Disease Activity in Small Bowel Crohn’s Disease. Aliment. Pharmacol. Ther. 2014, 40, 134–146. [Google Scholar] [CrossRef] [PubMed]
- Maaser, C.; Sturm, A.; Vavricka, S.R.; Kucharzik, T.; Fiorino, G.; Annese, V.; Calabrese, E.; Baumgart, D.C.; Bettenworth, D.; Borralho Nunes, P.; et al. ECCO-ESGAR Guideline for Diagnostic Assessment in IBD Part 1: Initial Diagnosis, Monitoring of Known IBD, Detection of Complications. J. Crohns Colitis 2019, 13, 144–164. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, G.C.; Low, D.; Chong, R.Y.; Diong, C.; Chawla, T. Utilization of Diagnostic Imaging and Ionization Radiation Exposure Among an Inflammatory Bowel Disease Inception Cohort. Inflamm. Bowel Dis. 2020, 26, 898–906. [Google Scholar] [CrossRef]
- Zakeri, N.; Pollok, R.C.G. Diagnostic Imaging and Radiation Exposure in Inflammatory Bowel Disease. World J. Gastroenterol. 2016, 22, 2165–2178. [Google Scholar] [CrossRef]
- Barlow, J.M.; Goss, B.C.; Hansel, S.L.; Kolbe, A.B.; Rackham, J.L.; Bruining, D.H.; Fletcher, J.G. CT Enterography: Technical and Interpretive Pitfalls. Abdom. Imaging 2015, 40, 1081–1096. [Google Scholar] [CrossRef]
- Baker, M.E.; Hara, A.K.; Platt, J.F.; Maglinte, D.D.T.; Fletcher, J.G. CT Enterography for Crohn’s Disease: Optimal Technique and Imaging Issues. Abdom. Imaging 2015, 40, 938–952. [Google Scholar] [CrossRef]
- Kerner, C.; Carey, K.; Mills, A.M.; Yang, W.; Synnestvedt, M.B.; Hilton, S.; Weiner, M.G.; Lewis, J.D. Use of Abdominopelvic Computed Tomography in Emergency Departments and Rates of Urgent Diagnoses in Crohn’s Disease. Clin. Gastroenterol. Hepatol. 2012, 10, 52–57. [Google Scholar] [CrossRef]
- Ha, J.; Park, S.H.; Son, J.H.; Kang, J.H.; Ye, B.D.; Park, S.H.; Kim, B.; Choi, S.H.; Park, S.H.; Yang, S.-K. Is the Mixed Use of Magnetic Resonance Enterography and Computed Tomography Enterography Adequate for Routine Periodic Follow-Up of Bowel Inflammation in Patients with Crohn’s Disease? Korean J. Radiol. 2022, 23, 30–41. [Google Scholar] [CrossRef] [PubMed]
- Stoddard, P.B.; Ghazi, L.J.; Wong-You-Cheong, J.; Cross, R.K.; Vandermeer, F.Q. Magnetic Resonance Enterography: State of the Art. Inflamm. Bowel Dis. 2015, 21, 229–239. [Google Scholar] [CrossRef] [PubMed]
- Greenup, A.-J.; Bressler, B.; Rosenfeld, G. Medical Imaging in Small Bowel Crohn’s Disease-Computer Tomography Enterography, Magnetic Resonance Enterography, and Ultrasound: “Which One Is the Best for What?”. Inflamm. Bowel Dis. 2016, 22, 1246–1261. [Google Scholar] [CrossRef]
- Ippolito, D.; Lombardi, S.; Talei Franzesi, C.; Drago, S.G.; Querques, G.; Casiraghi, A.; Pecorelli, A.; Riva, L.; Sironi, S. Dynamic Contrast-Enhanced MR with Quantitative Perfusion Analysis of Small Bowel in Vascular Assessment between Inflammatory and Fibrotic Lesions in Crohn’s Disease: A Feasibility Study. Contrast Media Mol. Imaging 2019, 2019, 1767620. [Google Scholar] [CrossRef] [PubMed]
- Rao, N.; Kumar, S.; Taylor, S.; Plumb, A. Diagnostic Pathways in Crohn’s Disease. Clin. Radiol. 2019, 74, 578–591. [Google Scholar] [CrossRef]
- Wnorowski, A.M.; Guglielmo, F.F.; Mitchell, D.G. How to Perform and Interpret Cine MR Enterography. J. Magn. Reson. Imaging 2015, 42, 1180–1189. [Google Scholar] [CrossRef]
- Minordi, L.M.; Bevere, A.; Papa, A.; Larosa, L.; Manfredi, R. CT and MRI Evaluations in Crohn’s Complications: A Guide for the Radiologist. Acad. Radiol. 2022, 29, 1206–1227. [Google Scholar] [CrossRef]
- Duigenan, S.; Gee, M.S. Imaging of Pediatric Patients With Inflammatory Bowel Disease. Am. J. Roentgenol. 2012, 199. [Google Scholar] [CrossRef]
- Liu, W.; Liu, J.; Xiao, W.; Luo, G. A diagnostic accuracy meta-analysis of CT and MRI for the evaluation of small bowel Crohn disease. Acad. Radiol. 2017, 24, 1216–1225. [Google Scholar] [CrossRef]
- Horsthuis, K.; Ziech, M.L.; Bipat, S.; Spijkerboer, A.M.; de Bruine-Dobben, A.C.; Hommes, D.W.; Stoker, J. Evaluation of an MRI-based score of disease activity in perianal fistulizing Crohn’s disease. Clin. Imaging 2011, 35, 360–365. [Google Scholar] [CrossRef]
- Fiorino, G.; Bonifacio, C.; Peyrin-Biroulet, L.; Minuti, F.; Repici, A.; Spinelli, A.; Fries, W.; Balzarini, L.; Montorsi, M.; Malesci, A.; et al. Prospective Comparison of Computed Tomography Enterography and Magnetic Resonance Enterography for Assessment of Disease Activity and Complications in Ileocolonic Crohn’s Disease. Inflamm. Bowel Dis. 2011, 17, 1073–1080. [Google Scholar] [CrossRef] [PubMed]
- Panes, J.; Bouhnik, Y.; Reinisch, W.; Stoker, J.; Taylor, S.A.; Baumgart, D.C.; Danese, S.; Halligan, S.; Marincek, B.; Matos, C.; et al. Imaging Techniques for Assessment of Inflammatory Bowel Disease: Joint ECCO and ESGAR Evidence-Based Consensus Guidelines. J. Crohns Colitis 2013, 7, 556–585. [Google Scholar] [CrossRef] [PubMed]
- Dave-Verma, H.; Moore, S.; Singh, A.; Martins, N.; Zawacki, J. Computed Tomographic Enterography and Enteroclysis: Pearls and Pitfalls. Curr. Probl. Diagn. Radiol. 2008, 37, 279–287. [Google Scholar] [CrossRef] [PubMed]
- Ilangovan, R.; Burling, D.; George, A.; Gupta, A.; Marshall, M.; Taylor, S.A. CT Enterography: Review of Technique and Practical Tips. Br. J. Radiol. 2012, 85, 876–886. [Google Scholar] [CrossRef]
- Taylor, S.A.; Avni, F.; Cronin, C.G.; Hoeffel, C.; Kim, S.H.; Laghi, A.; Napolitano, M.; Petit, P.; Rimola, J.; Tolan, D.J.; et al. The First Joint ESGAR/ ESPR Consensus Statement on the Technical Performance of Cross-Sectional Small Bowel and Colonic Imaging. Eur. Radiol. 2017, 27, 2570–2582. [Google Scholar] [CrossRef]
- Levine, A.; Koletzko, S.; Turner, D.; Escher, J.C.; Cucchiara, S.; de Ridder, L.; Kolho, K.-L.; Veres, G.; Russell, R.K.; Paerregaard, A.; et al. ESPGHAN Revised Porto Criteria for the Diagnosis of Inflammatory Bowel Disease in Children and Adolescents. J. Pediatr. Gastroenterol. Nutr. 2014, 58, 795–806. [Google Scholar] [CrossRef]
- Schooler, G.R.; Hull, N.C.; Mavis, A.; Lee, E.Y. MR Imaging Evaluation of Inflammatory Bowel Disease in Children:: Where Are We Now in 2019. Magn Reson Imaging Clin N Am 2019, 27, 291–300. [Google Scholar] [CrossRef]
- Morris, M.S.; Chu, D.I. Imaging for Inflammatory Bowel Disease. Surg. Clin. N. Am. 2015, 95, 1143–1158. [Google Scholar] [CrossRef]
- Khatri, G.; Coleman, J.; Leyendecker, J.R. Magnetic Resonance Enterography for Inflammatory and Noninflammatory Conditions of the Small Bowel. Radiol. Clin. N. Am. 2018, 56, 671–689. [Google Scholar] [CrossRef]
- Sturm, A.; Maaser, C.; Calabrese, E.; Annese, V.; Fiorino, G.; Kucharzik, T.; Vavricka, S.R.; Verstockt, B.; van Rheenen, P.; Tolan, D.; et al. ECCO-ESGAR Guideline for Diagnostic Assessment in IBD Part 2: IBD Scores and General Principles and Technical Aspects. J. Crohns Colitis 2019, 13, 273–284. [Google Scholar] [CrossRef]
- Wold, P.B.; Fletcher, J.G.; Johnson, C.D.; Sandborn, W.J. Assessment of Small Bowel Crohn Disease: Noninvasive Peroral CT Enterography Compared with Other Imaging Methods and Endoscopy--Feasibility Study. Radiology 2003, 229, 275–281. [Google Scholar] [CrossRef] [PubMed]
- Tkalčić, L.; Matana Kaštelan, Z.; Grubešić, T.; Mijandrušić Sinčić, B.; Milić, S.; Miletić, D. MR Enterocolonography in Patients with Crohn’s Disease and Healthy Volunteers - Do We Achieve Diagnostic Bowel Distension? Eur. J. Radiol. 2020, 129, 109100. [Google Scholar] [CrossRef] [PubMed]
- Schindera, S.T.; Nelson, R.C.; DeLong, D.M.; Jaffe, T.A.; Merkle, E.M.; Paulson, E.K.; Thomas, J. Multi-Detector Row CT of the Small Bowel: Peak Enhancement Temporal Window—Initial Experience. Radiology 2007, 243, 438–444. [Google Scholar] [CrossRef] [PubMed]
- Mollard, B.J.; Smith, E.A.; Dillman, J.R. Pediatric MR Enterography: Technique and Approach to Interpretation-How We Do It. Radiology 2015, 274, 29–43. [Google Scholar] [CrossRef]
- Dane, B.; Qian, K.; Gauvin, S.; Ji, H.; Karajgikar, J.; Kim, N.; Chang, S.; Chandarana, H.; Kim, S. Inter-Reader Agreement of the Society of Abdominal Radiology-American Gastroenterological Association (SAR-AGA) Consensus Reporting for Key Phenotypes at MR Enterography in Adults with Crohn Disease: Impact of Radiologist Experience. Abdom. Radiol. 2021, 46, 5095–5104. [Google Scholar] [CrossRef]
- Schmid-Tannwald, C.; Schmid-Tannwald, C.M.; Morelli, J.N.; Albert, N.L.; Braunagel, M.; Trumm, C.; Reiser, M.F.; Ertl-Wagner, B.; Rist, C. The Role of Diffusion-Weighted MRI in Assessment of Inflammatory Bowel Disease. Abdom. Radiol. 2016, 41, 1484–1494. [Google Scholar] [CrossRef]
- Guglielmo, F.F.; Anupindi, S.A.; Fletcher, J.G.; Al-Hawary, M.M.; Dillman, J.R.; Grand, D.J.; Bruining, D.H.; Chatterji, M.; Darge, K.; Fidler, J.L.; et al. Small Bowel Crohn Disease at CT and MR Enterography: Imaging Atlas and Glossary of Terms. Radiographics 2020, 40, 354–375. [Google Scholar] [CrossRef]
- Panés, J.; Bouzas, R.; Chaparro, M.; García-Sánchez, V.; Gisbert, J.P.; Martínez De Guereñu, B.; Mendoza, J.L.; Paredes, J.M.; Quiroga, S.; Ripollés, T.; et al. Systematic Review: The Use of Ultrasonography, Computed Tomography and Magnetic Resonance Imaging for the Diagnosis, Assessment of Activity and Abdominal Complications of Crohn’s Disease: Systematic Review: Cross-Sectional Imaging in Crohn’s Disease. Aliment. Ther. 2011, 34, 125–145. [Google Scholar] [CrossRef]
- Puylaert, C.a.J.; Tielbeek, J.a.W.; Bipat, S.; Stoker, J. Grading of Crohn’s Disease Activity Using CT, MRI, US and Scintigraphy: A Meta-Analysis. Eur. Radiol. 2015, 25, 3295–3313. [Google Scholar] [CrossRef]
- Church, P.C.; Turner, D.; Feldman, B.M.; Walters, T.D.; Greer, M.-L.; Amitai, M.M.; Griffiths, A.M.; the ImageKids Study Group. Systematic Review with Meta-analysis: Magnetic Resonance Enterography Signs for the Detection of Inflammation and Intestinal Damage in Crohn’s Disease. Aliment. Pharmacol. Ther. 2015, 41, 153–166. [Google Scholar] [CrossRef]
- Baker, M.E.; Walter, J.; Obuchowski, N.A.; Achkar, J.-P.; Einstein, D.; Veniero, J.C.; Vogel, J.; Stocchi, L. Mural Attenuation in Normal Small Bowel and Active Inflammatory Crohn’s Disease on CT Enterography: Location, Absolute Attenuation, Relative Attenuation, and the Effect of Wall Thickness. Am. J. Roentgenol. 2009, 192, 417–423. [Google Scholar] [CrossRef] [PubMed]
- Bodily, K.D.; Fletcher, J.G.; Solem, C.A.; Johnson, C.D.; Fidler, J.L.; Barlow, J.M.; Bruesewitz, M.R.; McCollough, C.H.; Sandborn, W.J.; Loftus, E.V.; et al. Crohn Disease: Mural Attenuation and Thickness at Contrast-Enhanced CT Enterography—Correlation with Endoscopic and Histologic Findings of Inflammation. Radiology 2006, 238, 505–516. [Google Scholar] [CrossRef]
- Rimola, J.; Ordás, I.; Rodriguez, S.; García-Bosch, O.; Aceituno, M.; Llach, J.; Ayuso, C.; Ricart, E.; Panés, J. Magnetic Resonance Imaging for Evaluation of Crohnʼs Disease: Validation of Parameters of Severity and Quantitative Index of Activity. Inflamm. Bowel Dis. 2011, 17, 1759–1768. [Google Scholar] [CrossRef]
- Zappa, M.; Stefanescu, C.; Cazals-Hatem, D.; Bretagnol, F.; Deschamps, L.; Attar, A.; Larroque, B.; Tréton, X.; Panis, Y.; Vilgrain, V.; et al. Which Magnetic Resonance Imaging Findings Accurately Evaluate Inflammation in Small Bowel Crohn’s Disease? A Retrospective Comparison with Surgical Pathologic Analysis. Inflamm. Bowel Dis. 2011, 17, 984–993. [Google Scholar] [CrossRef] [PubMed]
- Park, S.H. DWI at MR Enterography for Evaluating Bowel Inflammation in Crohn Disease. AJR Am. J. Roentgenol. 2016, 207, 40–48. [Google Scholar] [CrossRef] [PubMed]
- Morani, A.C.; Smith, E.A.; Ganeshan, D.; Dillman, J.R. Diffusion-Weighted MRI in Pediatric Inflammatory Bowel Disease. AJR Am. J. Roentgenol. 2015, 204, 1269–1277. [Google Scholar] [CrossRef]
- Vogel, J.; Da Luz Moreira, A.; Baker, M.; Hammel, J.; Einstein, D.; Stocchi, L.; Fazio, V. CT Enterography for Crohn’s Disease: Accurate Preoperative Diagnostic Imaging. Dis. Colon. Rectum 2007, 50, 1761–1769. [Google Scholar] [CrossRef]
- Barkmeier, D.T.; Dillman, J.R.; Al-Hawary, M.; Heider, A.; Davenport, M.S.; Smith, E.A.; Adler, J. MR Enterography–Histology Comparison in Resected Pediatric Small Bowel Crohn Disease Strictures: Can Imaging Predict Fibrosis? Pediatr. Radiol. 2016, 46, 498–507. [Google Scholar] [CrossRef]
- Oberhuber, G.; Stangl, P.C.; Vogelsang, H.; Schober, E.; Herbst, F.; Gasche, C. Significant Association of Strictures and Internal Fistula Formation in Crohn’s Disease. Virchows Archiv 2000, 437, 293–297. [Google Scholar] [CrossRef]
- Orscheln, E.S.; Dillman, J.R.; Towbin, A.J.; Denson, L.A.; Trout, A.T. Penetrating Crohn Disease: Does It Occur in the Absence of Stricturing Disease? Abdom. Radiol. 2018, 43, 1583–1589. [Google Scholar] [CrossRef]
- Rimola, J.; Rodriguez, S.; García-Bosch, O.; Ordás, I.; Ayala, E.; Aceituno, M.; Pellisé, M.; Ayuso, C.; Ricart, E.; Donoso, L.; et al. Magnetic Resonance for Assessment of Disease Activity and Severity in Ileocolonic Crohn’s Disease. Gut 2009, 58, 1113–1120. [Google Scholar] [CrossRef]
- Sinha, R.; Murphy, P.; Sanders, S.; Ramachandran, I.; Hawker, P.; Rawat, S.; Roberts, S. Diagnostic Accuracy of High-Resolution MR Enterography in Crohn’s Disease: Comparison with Surgical and Pathological Specimen. Clin. Radiol. 2013, 68, 917–927. [Google Scholar] [CrossRef]
- Kelly, J.K.; Preshaw, R.M. Origin of Fistulas in Crohn’s Disease. J. Clin. Gastroenterol. 1989, 11, 193–196. [Google Scholar] [CrossRef]
- Bruining, D.H.; Siddiki, H.A.; Fletcher, J.G.; Tremaine, W.J.; Sandborn, W.J.; Loftus, E.V. Prevalence of Penetrating Disease and Extra-intestinal Manifestations of Crohnʼs Disease Detected with CT Enterography. Inflamm. Bowel Dis. 2008, 14, 1701–1706. [Google Scholar] [CrossRef]
- Baker, M.E.; Fletcher, J.G.; Al-Hawary, M.; Bruining, D. Interdisciplinary Updates in Crohn’s Disease Reporting Nomenclature, and Cross-Sectional Disease Monitoring. Radiol. Clin. N. Am. 2018, 56, 691–707. [Google Scholar] [CrossRef]
- Tao, Y.; Li, H.; Xu, H.; Tang, W.; Fan, G.; Yang, X. Can the Simplified Magnetic Resonance Index of Activity Be Used to Evaluate the Degree of Activity in Crohn’s Disease? BMC Gastroenterol. 2021, 21, 409. [Google Scholar] [CrossRef]
- D’Amico, F.; Chateau, T.; Laurent, V.; Danese, S.; Peyrin-Biroulet, L. Which MRI Score and Technique Should Be Used for Assessing Crohn’s Disease Activity? J. Clin. Med. 2020, 9, 1691. [Google Scholar] [CrossRef]
- González-Suárez, B.; Rodriguez, S.; Ricart, E.; Ordás, I.; Rimola, J.; Díaz-González, Á.; Romero, C.; de Miguel, C.R.; Jáuregui, A.; Araujo, I.K.; et al. Comparison of Capsule Endoscopy and Magnetic Resonance Enterography for the Assessment of Small Bowel Lesions in Crohn’s Disease. Inflamm. Bowel Dis. 2018, 24, 775–780. [Google Scholar] [CrossRef]
- Buisson, A.; Joubert, A.; Montoriol, P.-F.; Da Ines, D.; Hordonneau, C.; Pereira, B.; Garcier, J.-M.; Bommelaer, G.; Petitcolin, V. Diffusion-Weighted Magnetic Resonance Imaging for Detecting and Assessing Ileal Inflammation in Crohn’s Disease. Aliment. Pharmacol. Ther. 2013, 37, 537–545. [Google Scholar] [CrossRef]
- Hordonneau, C.; Buisson, A.; Scanzi, J.; Goutorbe, F.; Pereira, B.; Borderon, C.; Da Ines, D.; Montoriol, P.F.; Garcier, J.M.; Boyer, L.; et al. Diffusion-Weighted Magnetic Resonance Imaging in Ileocolonic Crohn’s Disease: Validation of Quantitative Index of Activity. Am. J. Gastroenterol. 2014, 109, 89–98. [Google Scholar] [CrossRef]
- Thierry, M.-L.; Rousseau, H.; Pouillon, L.; Girard-Gavanier, M.; Baumann, C.; Lopez, A.; Danese, S.; Laurent, V.; Peyrin-Biroulet, L. Accuracy of Diffusion-Weighted Magnetic Resonance Imaging in Detecting Mucosal Healing and Treatment Response, and in Predicting Surgery, in Crohn’s Disease. J. Crohns Colitis 2018, 12, 1180–1190. [Google Scholar] [CrossRef]
- Choi, S.H.; Kim, K.W.; Lee, J.Y.; Kim, K.-J.; Park, S.H. Diffusion-Weighted Magnetic Resonance Enterography for Evaluating Bowel Inflammation in Crohnʼs Disease: A Systematic Review and Meta-Analysis. Inflamm. Bowel Dis. 2016, 22, 669–679. [Google Scholar] [CrossRef]
- Steward, M.J.; Punwani, S.; Proctor, I.; Adjei-Gyamfi, Y.; Chatterjee, F.; Bloom, S.; Novelli, M.; Halligan, S.; Rodriguez-Justo, M.; Taylor, S.A. Non-Perforating Small Bowel Crohn’s Disease Assessed by MRI Enterography: Derivation and Histopathological Validation of an MR-Based Activity Index. Eur. J. Radiol. 2012, 81, 2080–2088. [Google Scholar] [CrossRef]
- Spada, C.; Hassan, C.; Bellini, D.; Burling, D.; Cappello, G.; Carretero, C.; Dekker, E.; Eliakim, R.; De Haan, M.; Kaminski, M.F.; et al. Imaging Alternatives to Colonoscopy: CT Colonography and Colon Capsule. European Society of Gastrointestinal Endoscopy (ESGE) and European Society of Gastrointestinal and Abdominal Radiology (ESGAR) Guideline—Update 2020. Endoscopy 2020, 52, 1127–1141. [Google Scholar] [CrossRef]
- Rozendorn, N.; Klang, E.; Lahat, A.; Yablecovitch, D.; Kopylov, U.; Eliakim, A.; Ben-Horin, S.; Amitai, M.M. Prediction of Patency Capsule Retention in Known Crohn’s Disease Patients by Using Magnetic Resonance Imaging. Gastrointest. Endosc. 2016, 83, 182–187. [Google Scholar] [CrossRef]
- Yung, D.E.; Har-Noy, O.; Tham, Y.S.; Ben-Horin, S.; Eliakim, R.; Koulaouzidis, A.; Kopylov, U. Capsule Endoscopy, Magnetic Resonance Enterography, and Small Bowel Ultrasound for Evaluation of Postoperative Recurrence in Crohn’s Disease: Systematic Review and Meta-Analysis. Inflamm. Bowel Dis. 2018, 24, 93–100. [Google Scholar] [CrossRef]


| CTE | MRE | ||
|---|---|---|---|
| Advantages | Disadvantages | Advantages | Disadvantages |
|
|
|
|
| Authors | CTE | MRE | ||
|---|---|---|---|---|
| Sensitivity (%) | Specificity (%) | Sensitivity (%) | Specificity (%) | |
| Duigenan et al. [28] | n/a | n/a | 81–91 | 67–89 |
| Liu et al. [29] | 87 (95% CI, 78–92%) | 91 (95% CI, 84–95%) | 86 (95% CI, 79–91%) | 93 (95% CI, 84–97%) |
| Greenup et al. [23] | 67–95 | 70–90 | 66–100 | 72–100 |
| Horsthuis et al. [30] | 84.3 per patient analysis67.4 per segment analysis | 95.1 per patient analysis90.2 per segment analysis | 93 per patient analysis70.4 per segment analysis | 92.6 per patient analysis94 per segment analysis |
| Gomollòn et al. [1] | 84 per patient analysis | n/a | 93 per patient analysis | n/a |
| Fiorino et al. [31] | Strictures’ detection: 85Per-segment analysis: 81Rectal disease: 81 | Strictures’ detection: 51Per-segment analysis: 81Rectal disease: 50.9 | Strictures’ detection: 92Per-segment analysis: 93Rectal disease: 72 | Strictures’ detection: 90Per-segment analysis: 72Rectal disease: 100 |
| Maaser et al. [15] | 92 | 100 | 89 | 94 |
| MaRIA | Simplified MaRIA | London | Nancy | Clermont | |
|---|---|---|---|---|---|
| Fasting | Yes | Yes | Yes | No | Yes |
| Bowel preparation | Yes | Yes | Yes | No | No |
| Oral contrast administration | Yes | Yes | Yes | Yes | Yes |
| Gadolinium-based i.v. | Yes | No | Yes | Yes | No |
| Motility assessment | No | No | No | No | Yes |
| Bowel wall thickness | Yes | Yes | Yes | Yes | Yes |
| Wall enhancement | Yes | No | Yes | No | No |
| Edema | Yes | Yes | Yes | Yes | Yes |
| Ulceration | Yes | Yes | No | Yes | Yes |
| Mesenteric node enlargement (>1 cm) | Yes | No | Yes | No | Yes |
| Cut-off values for endoscopy correlation | ≥7 for active disease ≥11 for severe ulcerative disease | >1 for active disease >2 for severe lesions | ≥4.1 for the presence of histopathological acute inflammation | Mucosal healing: ≤6 total Nancy score ≤2 segmental Nancy score | >8.4 for ileal activity ≥12.5 for severe ileal disease |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Maino, C.; Mariani, I.; Drago, S.G.; Franco, P.N.; Giandola, T.P.; Donati, F.; Boraschi, P.; Ippolito, D. Computed Tomography and Magnetic Resonance Enterography: From Protocols to Diagnosis. Diagnostics 2024, 14, 2584. https://doi.org/10.3390/diagnostics14222584
Maino C, Mariani I, Drago SG, Franco PN, Giandola TP, Donati F, Boraschi P, Ippolito D. Computed Tomography and Magnetic Resonance Enterography: From Protocols to Diagnosis. Diagnostics. 2024; 14(22):2584. https://doi.org/10.3390/diagnostics14222584
Chicago/Turabian StyleMaino, Cesare, Ilaria Mariani, Silvia Girolama Drago, Paolo Niccolò Franco, Teresa Paola Giandola, Francescamaria Donati, Piero Boraschi, and Davide Ippolito. 2024. "Computed Tomography and Magnetic Resonance Enterography: From Protocols to Diagnosis" Diagnostics 14, no. 22: 2584. https://doi.org/10.3390/diagnostics14222584
APA StyleMaino, C., Mariani, I., Drago, S. G., Franco, P. N., Giandola, T. P., Donati, F., Boraschi, P., & Ippolito, D. (2024). Computed Tomography and Magnetic Resonance Enterography: From Protocols to Diagnosis. Diagnostics, 14(22), 2584. https://doi.org/10.3390/diagnostics14222584







