Relationship between Volitional and Non-Volitional Quadriceps Muscle Endurance in Patients with Chronic Obstructive Pulmonary Disease
Abstract
1. Introduction
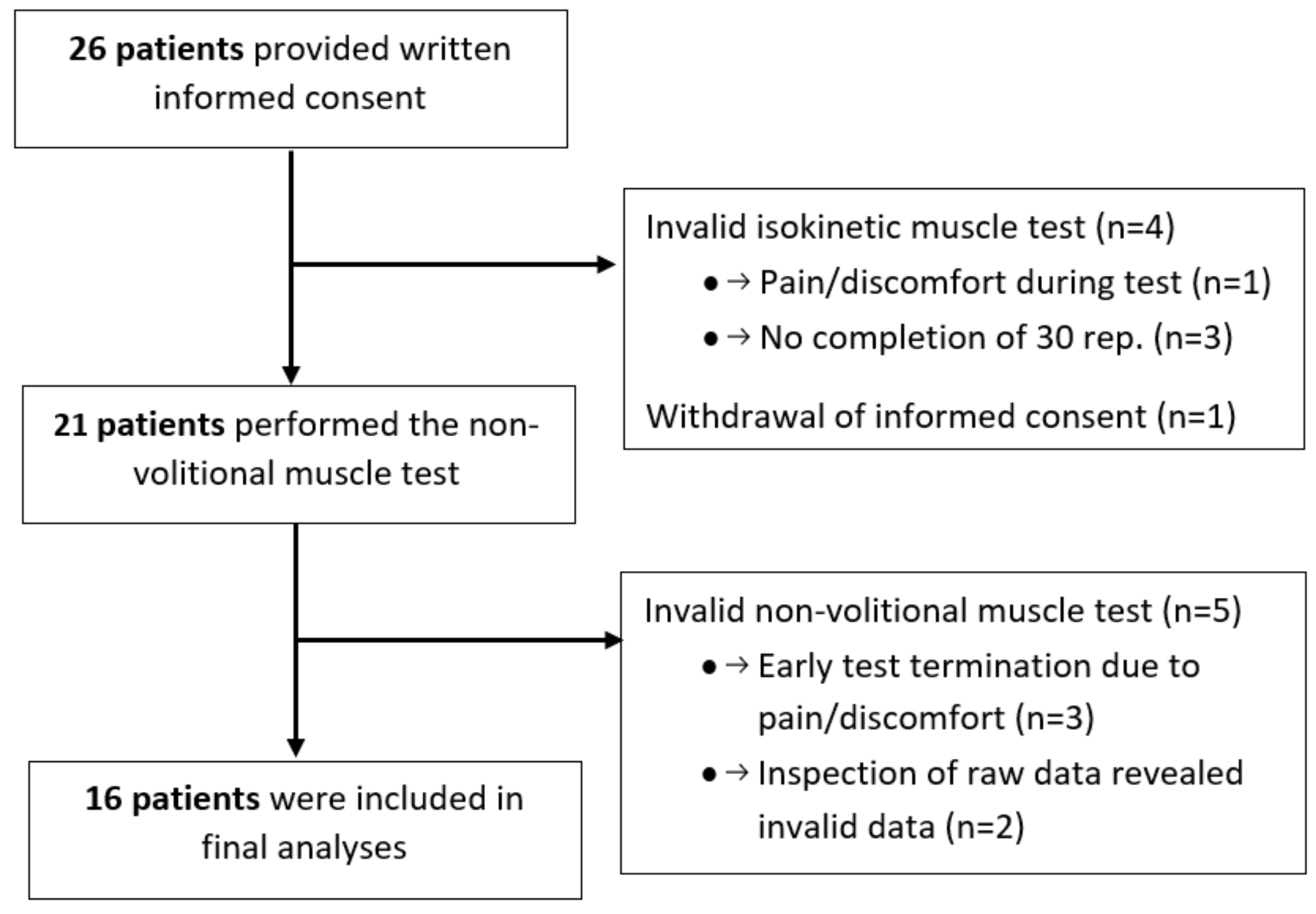
2. Materials and Methods
2.1. Assessment
2.1.1. Volitional Quadriceps Muscle Endurance
2.1.2. Non-Volitional Quadriceps Muscle Endurance
2.2. Statistical Analysis
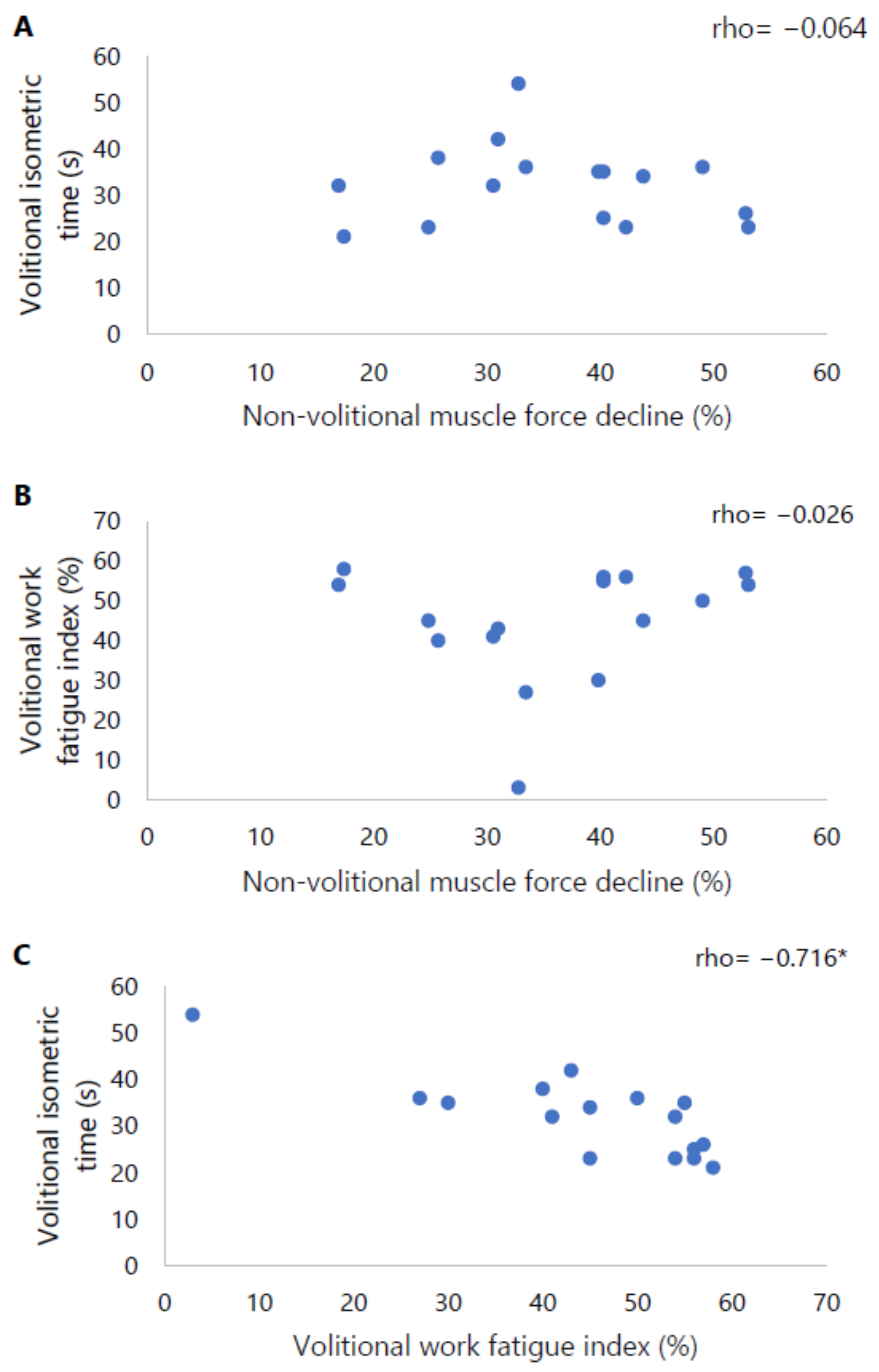
3. Results
3.1. Volitional and Non-Volitional Quadriceps Muscle Endurance
Borg Scores
4. Discussion
4.1. Strengths and Limitations
4.2. Clinical Implications and Future Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Celli, B.; Fabbri, L.; Criner, G.; Martinez, F.J.; Mannino, D.; Vogelmeier, C.; Montes de Oca, M.; Papi, A.; Sin, D.D.; Han, M.K.; et al. Definition and Nomenclature of Chronic Obstructive Pulmonary Disease: Time for its Revision. Am. J. Respir. Crit. Care Med. 2022, 206, 1317–1325. [Google Scholar] [CrossRef]
- GOLD. Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease, 2023 Report; GOLD: Deer Park, IL, USA, 2022. [Google Scholar]
- Maltais, F.; Decramer, M.; Casaburi, R.; Barreiro, E.; Burelle, Y.; Debigare, R.; Dekhuijzen, P.N.; Franssen, F.; Gayan-Ramirez, G.; Gea, J.; et al. An official American Thoracic Society/European Respiratory Society statement: Update on limb muscle dysfunction in chronic obstructive pulmonary disease. Am. J. Respir. Crit. Care Med. 2014, 189, e15–e62. [Google Scholar] [CrossRef] [PubMed]
- Whittom, F.; Jobin, J.; Simard, P.M.; Leblanc, P.; Simard, C.; Bernard, S.; Belleau, R.; Maltais, F. Histochemical and morphological characteristics of the vastus lateralis muscle in patients with chronic obstructive pulmonary disease. Med. Sci. Sports Exerc. 1998, 30, 1467–1474. [Google Scholar] [CrossRef] [PubMed]
- Gosker, H.R.; Zeegers, M.P.; Wouters, E.F.; Schols, A.M. Muscle fibre type shifting in the vastus lateralis of patients with COPD is associated with disease severity: A systematic review and meta-analysis. Thorax 2007, 62, 944–949. [Google Scholar] [CrossRef] [PubMed]
- Gosker, H.R.; Lencer, N.H.; Franssen, F.M.; van der Vusse, G.J.; Wouters, E.F.; Schols, A.M. Striking similarities in systemic factors contributing to decreased exercise capacity in patients with severe chronic heart failure or COPD. Chest 2003, 123, 1416–1424. [Google Scholar] [CrossRef] [PubMed]
- Gosker, H.R.; Engelen, M.P.; van Mameren, H.; van Dijk, P.J.; van der Vusse, G.J.; Wouters, E.F.; Schols, A.M. Muscle fiber type IIX atrophy is involved in the loss of fat-free mass in chronic obstructive pulmonary disease. Am. J. Clin. Nutr. 2002, 76, 113–119. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Li, P.; Cao, Y.; Liu, C.; Wang, J.; Wu, W. Skeletal Muscle Mitochondrial Dysfunction in Chronic Obstructive Pulmonary Disease: Underlying Mechanisms and Physical Therapy Perspectives. Aging Dis. 2023, 14, 33–45. [Google Scholar] [CrossRef]
- Marklund, S.; Bui, K.L.; Nyberg, A. Measuring and monitoring skeletal muscle function in COPD: Current perspectives. Int. J. COPD 2019, 14, 1825–1838. [Google Scholar] [CrossRef]
- Tanguay, S.; Saey, D.; Marklund, S.; Nyberg, A.; Gephine, S.; Frykholm, E.; De Brandt, J.; Burtin, C.; Maltais, F. Reference equations for quadriceps strength, endurance and power: A multicentre study. ERJ Open Res. 2023, in press. [Google Scholar] [CrossRef]
- Nyberg, A.; Saey, D.; Maltais, F. Why and How Limb Muscle Mass and Function Should Be Measured in Patients with Chronic Obstructive Pulmonary Disease. Ann. Am. Thorac. Soc. 2015, 12, 1269–1277. [Google Scholar] [CrossRef]
- Vaes, A.W.; Sillen, M.J.H.; Goertz, Y.M.J.; Machado, F.; Van Herck, M.; Burtin, C.; Franssen, F.M.E.; van’t Hul, A.J.; Spruit, M.A. The correlation between quadriceps muscle strength and endurance and exercise performance in patients with COPD. J. Appl. Physiol. 2021, 131, 589–600. [Google Scholar] [CrossRef]
- Frykholm, E.; Gephine, S.; Saey, D.; Lemson, A.; Klijn, P.; de Vaate, E.B.; Maltais, F.; van Hees, H.; Nyberg, A. Isotonic quadriceps endurance is better associated with daily physical activity than quadriceps strength and power in COPD: An international multicentre cross-sectional trial. Sci. Rep. 2021, 11, 11557. [Google Scholar] [CrossRef]
- Frykholm, E.; Gephine, S.; Saey, D.; van Hees, H.; Lemson, A.; Klijn, P.; Maltais, F.; Nyberg, A. Inter-day test-retest reliability and feasibility of isokinetic, isometric, and isotonic measurements to assess quadriceps endurance in people with chronic obstructive pulmonary disease: A multicenter study. Chron. Respir. Dis. 2019, 16, 1–9. [Google Scholar] [CrossRef]
- Allaire, J.; Maltais, F.; Doyon, J.F.; Noel, M.; LeBlanc, P.; Carrier, G.; Simard, C.; Jobin, J. Peripheral muscle endurance and the oxidative profile of the quadriceps in patients with COPD. Thorax 2004, 59, 673–678. [Google Scholar] [CrossRef] [PubMed]
- Van den Borst, B.; Slot, I.G.M.; Hellwig, V.A.C.V.; Vosse, B.A.H.; Kelders, M.C.J.M.; Barreiro, E.; Schols, A.M.W.J.; Gosker, H.R. Loss of quadriceps muscle oxidative phenotype and decreased endurance in patients with mild-to-moderate COPD. J. Appl. Physiol. 2012, 114, 1319–1328. [Google Scholar] [CrossRef]
- Degens, H.; Sanchez Horneros, J.M.; Heijdra, Y.F.; Dekhuijzen, P.N.; Hopman, M.T. Skeletal muscle contractility is preserved in COPD patients with normal fat-free mass. Acta Physiol. Scand. 2005, 184, 235–242. [Google Scholar] [CrossRef] [PubMed]
- Millet, G.Y.; Martin, V.; Martin, A.; Verges, S. Electrical stimulation for testing neuromuscular function: From sport to pathology. Eur. J. Appl. Physiol. 2011, 111, 2489–2500. [Google Scholar] [CrossRef] [PubMed]
- Swallow, E.B.; Gosker, H.R.; Ward, K.A.; Moore, A.J.; Dayer, M.J.; Hopkinson, N.S.; Schols, A.M.; Moxham, J.; Polkey, M.I. A novel technique for nonvolitional assessment of quadriceps muscle endurance in humans. J. Appl. Physiol. 2007, 103, 739–746. [Google Scholar] [CrossRef] [PubMed]
- Ju, C.R.; Chen, R.C. Quadriceps strength assessed by magnetic stimulation of femoral nerve in patients with chronic obstructive pulmonary disease. Chin. Med. J. 2011, 124, 2309–2315. [Google Scholar]
- Gerrits, H.L.; De Haan, A.; Hopman, M.T.; van Der Woude, L.H.; Jones, D.A.; Sargeant, A.J. Contractile properties of the quadriceps muscle in individuals with spinal cord injury. Muscle Nerve 1999, 22, 1249–1256. [Google Scholar] [CrossRef]
- Gerrits, H.L.; Hopman, M.T.; Sargeant, A.J.; de Haan, A. Reproducibility of contractile properties of the human paralysed and non-paralysed quadriceps muscle. Clin. Physiol. 2001, 21, 105–113. [Google Scholar] [CrossRef] [PubMed]
- Machado Rodrigues, F.; Demeyer, H.; Hornikx, M.; Camillo, C.A.; Calik-Kutukcu, E.; Burtin, C.; Janssens, W.; Troosters, T.; Osadnik, C. Validity and reliability of strain gauge measurement of volitional quadriceps force in patients with COPD. Chron. Respir. Dis. 2017, 14, 289–297. [Google Scholar] [CrossRef] [PubMed]
- Nyberg, A.; Saey, D.; Martin, M.; Maltais, F. Test-re-test reliability of quadriceps muscle strength measures in people with more severe chronic obstructive pulmonary disease. J. Rehabil. Med. 2018, 50, 759–764. [Google Scholar] [CrossRef] [PubMed]
- Saey, D.; Troosters, T. Measuring skeletal muscle strength and endurance, from bench to bedside. Clin. Investig. Med. 2008, 31, E307–E311. [Google Scholar] [CrossRef] [PubMed]
- Mahler, D.A.; Wells, C.K. Evaluation of clinical methods for rating dyspnea. Chest 1988, 93, 580–586. [Google Scholar] [CrossRef] [PubMed]
- Quanjer, P.H.; Tammeling, G.J.; Cotes, J.E.; Pedersen, O.F.; Peslin, R.; Yernault, J.C. Lung volumes and forced ventilatory flows. Report Working Party Standardization of Lung Function Tests, European Community for Steel and Coal. Official Statement of the European Respiratory Society. Eur. Respir. J. Suppl. 1993, 16, 5–40. [Google Scholar] [CrossRef] [PubMed]
- Quanjer, P.H.; Stanojevic, S.; Cole, T.J.; Baur, X.; Hall, G.L.; Culver, B.H.; Enright, P.L.; Hankinson, J.L.; Ip, M.S.; Zheng, J.; et al. Multi-ethnic reference values for spirometry for the 3-95-yr age range: The global lung function 2012 equations. Eur. Respir. J. 2012, 40, 1324–1343. [Google Scholar] [CrossRef]
- Koch, B.; Schaper, C.; Ittermann, T.; Spielhagen, T.; Dorr, M.; Volzke, H.; Opitz, C.F.; Ewert, R.; Glaser, S. Reference values for cardiopulmonary exercise testing in healthy volunteers: The SHIP study. Eur. Respir. J. 2009, 33, 389–397. [Google Scholar] [CrossRef]
- Radtke, T.; Crook, S.; Kaltsakas, G.; Louvaris, Z.; Berton, D.; Urquhart, D.S.; Kampouras, A.; Rabinovich, R.A.; Verges, S.; Kontopidis, D.; et al. ERS statement on standardisation of cardiopulmonary exercise testing in chronic lung diseases. Eur. Respir. Rev. 2019, 28, 180101. [Google Scholar] [CrossRef]
- De Groot, S.; Nieuwenhuizen, M.G. Validity and reliability of measuring activities, movement intensity and energy expenditure with the DynaPort MoveMonitor. Med. Eng. Phys. 2013, 35, 1499–1505. [Google Scholar] [CrossRef]
- Gore, S.; Blackwood, J.; Guyette, M.; Alsalaheen, B. Validity and Reliability of Accelerometers in Patients with COPD: A Systematic Review. J. Cardiopulm. Rehabil. Prev. 2018, 38, 147–158. [Google Scholar] [CrossRef] [PubMed]
- Harbo, T.; Brincks, J.; Andersen, H. Maximal isokinetic and isometric muscle strength of major muscle groups related to age, body mass, height, and sex in 178 healthy subjects. Eur. J. Appl. Physiol. 2011, 112, 267–275. [Google Scholar] [CrossRef]
- Borg’s, B.G. Perceived Exertion and Pain Scales; Human Kinetics: Champaign, IL, USA, 1998. [Google Scholar]
- Ribeiro, F.; Lépine, P.A.; Garceau-Bolduc, C.; Coats, V.; Allard, É.; Maltais, F.; Saey, D. Test-retest reliability of lower limb isokinetic endurance in COPD: A comparison of angular velocities. Int. J. Chron. Obstruct. Pulmon. Dis. 2015, 10, 1163–1172. [Google Scholar] [CrossRef]
- Stoffels, A.A.F.; Meys, R.; van Hees, H.W.H.; Franssen, F.M.E.; van den Borst, B.; van’t Hul, A.J.; Klijn, P.H.; Vaes, A.W.; De Brandt, J.; Burtin, C.; et al. Isokinetic testing of quadriceps function in COPD: Feasibility, responsiveness, and minimal important differences in patients undergoing pulmonary rehabilitation. Braz. J. Phys. Ther. 2022, 26, 100451. [Google Scholar] [CrossRef] [PubMed]
- Buller, A.J.; Lewis, D.M. The Rate of Tension Development in Isometric Tetanic Contractions of Mammalian Fast and Slow Skeletal Muscle. J. Physiol. 1965, 176, 337–354. [Google Scholar] [CrossRef]
- Edwards, R.H.; Hill, D.K.; Jones, D.A. Metabolic changes associated with the slowing of relaxation in fatigued mouse muscle. J. Physiol. 1975, 251, 287–301. [Google Scholar] [CrossRef] [PubMed]
- Sadri, K.; Khani, M.; Sadri, I. Role of Central Fatigue in Resistance and Endurance Exercises: An Emphasis on Mechanisms and Potential Sites. Sportlogia 2014, 10, 65–80. [Google Scholar] [CrossRef]
- Fitts, R.H.; McDonald, K.S.; Schluter, J.M. The determinants of skeletal muscle force and power: Their adaptability with changes in activity pattern. J. Biomech. 1991, 24, 111–122. [Google Scholar] [CrossRef]
- Suchomel, T.J.; Nimphius, S.; Bellon, C.R.; Stone, M.H. The Importance of Muscular Strength: Training Considerations. Sports Med. 2018, 48, 765–785. [Google Scholar] [CrossRef]
- Harridge, S.D.R.; Saltin, B. Neuromuscular System. In Encyclopedia of Gerontology, 2nd ed.; Birren, J.E., Ed.; Elsevier: New York, NY, USA, 2007; pp. 260–269. [Google Scholar] [CrossRef]
- Tornero-Aguilera, J.F.; Jimenez-Morcillo, J.; Rubio-Zarapuz, A.; Clemente-Suarez, V.J. Central and Peripheral Fatigue in Physical Exercise Explained: A Narrative Review. Int. J. Environ. Res. Public Health 2022, 19, 3909. [Google Scholar] [CrossRef]
- Beretta-Piccoli, M.; D’Antona, G.; Barbero, M.; Fisher, B.; Dieli-Conwright, C.M.; Clijsen, R.; Cescon, C. Evaluation of central and peripheral fatigue in the quadriceps using fractal dimension and conduction velocity in young females. PLoS ONE 2015, 10, e0123921. [Google Scholar] [CrossRef]
- Pageaux, B.; Lepers, R. Fatigue Induced by Physical and Mental Exertion Increases Perception of Effort and Impairs Subsequent Endurance Performance. Front. Physiol. 2016, 7, 587. [Google Scholar] [CrossRef]
- Martin, K.; Meeusen, R.; Thompson, K.G.; Keegan, R.; Rattray, B. Mental Fatigue Impairs Endurance Performance: A Physiological Explanation. Sports Med. 2018, 48, 2041–2051. [Google Scholar] [CrossRef]
- Aras, Y.G.; Aydemir, Y.; Güngen, B.D.; Güngen, A.C. Evaluation of central and peripheral neuropathy in patients with chronic obstructive pulmonary disease. Int. J. Chron. Obstruct. Pulmon. Dis. 2018, 13, 1857–1862. [Google Scholar] [CrossRef]
- Ribeiro, F.; Oueslati, F.; Saey, D.; Lepine, P.A.; Chambah, S.; Coats, V.; Maltais, F. Cardiorespiratory and Muscle Oxygenation Responses to Isokinetic Exercise in Chronic Obstructive Pulmonary Disease. Med. Sci. Sports Exerc. 2019, 51, 841–849. [Google Scholar] [CrossRef]

| Included Patients (n = 16) | |
|---|---|
| Age (years) | 61 ± 8 |
| Gender (male:female) | 6:10 |
| BMI (kg/m2) | 25.2 ± 5.3 |
| FFMI (kg/m2) | 16.6 ± 2.0 |
| GOLD A/B/E (n) | 0/8/8 |
| Lung function | |
| FEV1 (L) | 1.1 (1.0–1.6) |
| FEV1 (% pred) | 47 (32–53) |
| FEV1/FVC (%) | 37 (30–52) |
| RV (L) | 3.6 (2.8–4.5) |
| RV (% pred) | 176 ± 48 |
| TLC (L) | 6.7 (6.0–8.1) |
| TLC (% pred) | 120 ± 14 |
| DLco (mmol/(min·kPa)) * | 4.0 ± 1.4 |
| DLco (% pred) * | 50 ± 11 |
| mMRC dyspnoea grade | 2 (1–3) |
| Physical function | |
| VO2peak (mL/min/kg) | 14.4 (12.9–19.9) |
| VO2peak (% pred) | 63 (46–77) |
| Average steps/day | 4238 (2713–6811) |
| MVC (Nm) | 108 (98–153) |
| MVC (% pred) | 64 ± 12 |
| Volitional Isometric Test | Volitional Isokinetic Test | Non-Volitional Isometric Test | p-Value | |
|---|---|---|---|---|
| Borg score dyspnoea Start End Delta | 1 (0–3) | 1 (1–3) | 1 (1–2) | 0.218 |
| 4 (2–6) # | 5 (4–7) # | 2 (1–3) #,* | <0.001 a,b | |
| 1 (1–3) | 4 (2–5) | 1 (0–2) * | <0.001 a,b | |
| Borg score leg fatigue Start End Delta | 1 (0–3) | 2 (1–3) | 2 (1–3) | 0.223 |
| 5 (3–7) # | 6 (5–8) # | 4 (3–5) #,* | <0.001 a,b | |
| 3 (2–4) | 4 (3–5) | 2 (0–3) * | <0.001 b |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stoffels, A.A.F.; Allard, N.A.E.; Spruit, M.A.; Klijn, P.; Hopman, M.T.E.; Meys, R.; Franssen, F.M.E.; Timmers, S.; van den Borst, B.; van Hees, H.W.H. Relationship between Volitional and Non-Volitional Quadriceps Muscle Endurance in Patients with Chronic Obstructive Pulmonary Disease. Diagnostics 2024, 14, 190. https://doi.org/10.3390/diagnostics14020190
Stoffels AAF, Allard NAE, Spruit MA, Klijn P, Hopman MTE, Meys R, Franssen FME, Timmers S, van den Borst B, van Hees HWH. Relationship between Volitional and Non-Volitional Quadriceps Muscle Endurance in Patients with Chronic Obstructive Pulmonary Disease. Diagnostics. 2024; 14(2):190. https://doi.org/10.3390/diagnostics14020190
Chicago/Turabian StyleStoffels, Anouk A. F., Neeltje A. E. Allard, Martijn A. Spruit, Peter Klijn, Maria T. E. Hopman, Roy Meys, Frits M. E. Franssen, Silvie Timmers, Bram van den Borst, and Hieronymus W. H. van Hees. 2024. "Relationship between Volitional and Non-Volitional Quadriceps Muscle Endurance in Patients with Chronic Obstructive Pulmonary Disease" Diagnostics 14, no. 2: 190. https://doi.org/10.3390/diagnostics14020190
APA StyleStoffels, A. A. F., Allard, N. A. E., Spruit, M. A., Klijn, P., Hopman, M. T. E., Meys, R., Franssen, F. M. E., Timmers, S., van den Borst, B., & van Hees, H. W. H. (2024). Relationship between Volitional and Non-Volitional Quadriceps Muscle Endurance in Patients with Chronic Obstructive Pulmonary Disease. Diagnostics, 14(2), 190. https://doi.org/10.3390/diagnostics14020190






